Abstract
Whenever a new therapy enters the wound care arena it is mandatory to deliver the best evidence to clinicians, healthcare administrators and policy makers to support integration of the technology into clinical practice. While this can often be problematic when novel therapies lack a large body of supporting evidence, methods that incorporate the use of expert opinion do exist to evaluate existing evidence and create consensus statements that can help guide decisions. Topical pressurised oxygen therapy is a method of delivering pressurised and humidified oxygen directly to the wound bed to support the healing of chronic and hypoxic wounds. This article will present the process by which the evidence was identified and evaluated as well as present standards based on the evidence related to topical pressurised oxygen therapy. We will show, through the use of the evidence, how this therapy can be a non invasive safe approach for wound management for selected patients in all clinical care settings.
Keywords: Evidence‐based, Oxygen therapy, Pressurised
INTRODUCTION
Canada's aging population will soon become ‘an $850 billion ticking time bomb’(1) and the management of wounds will take‐up a large part of these rising healthcare costs.
An Ontario‐wide study has shown that wound care accounts for up to 50% of home care services provided at any given time. The project estimates that 31 000 people are admitted to home care for wound care each year, with an annual cost of $108·7 million in services with respect to wounds, excluding the cost of supplies and equipment (2).
In 2010, Ontario, a province in Canada, introduced Bill 46, which calls for ‘excellent care for all’ through legislation that puts the patient first. The foundation for this is a high‐quality healthcare system that is ‘accessible, appropriate, effective, efficient, equitable, integrated, patient‐centred, population health focused and safe’(3).
Reconciling the realities of a need for ‘excellent care for all’ and increasing healthcare costs is an issue facing every healthcare jurisdiction in Canada, and elsewhere around the world. How do decision‐makers decide on the most cost‐effective choices while continuing to provide excellent care, specifically in relation to wound care?
Innovative technologies for addressing wounds can sometimes answer the need, but must be carefully reviewed by wound care clinicians, researchers and decision‐makers to determine their level of evidence before implementation into practice. If warranted, they can be part of the solution by reducing wound healing times and decreasing wound recurrence rates – thereby meeting the standards identified by Bill 46.
New technologies rarely come with an abundance of evidence to back them. So how do decision‐makers evaluate innovations? What can the evidence of related but not identical technologies offer to the questions surrounding the new technology? How are gaps in the evidence that may exist, be identified and filled? How can decision‐makers and practitioners critically evaluate anecdotal evidence presented by eager proponents of the new technology? How can the manufacturers/distributors of the technology represent their product fairly, i.e. in the best light while conforming to best evidence standards?
These were exactly the questions that needed to be addressed regarding topical pressurised oxygen therapy, a relatively new wound treatment modality that has abundant anecdotal evidence that parallels other technologies but lacks a large body of specific evidence to support its use.
To answer these and other important questions, a process was implemented that addressed the following concerns:
-
1
Bias: It is essential to the integrity of the process that an individual with no stake in the outcome facilitates all activities regarding the evaluation of the evidence.
-
2
Method: To ensure that the outcomes have value to the field, the process used must be validated, transparent and well understood by all participants.
-
3
Experience: An interprofessional group of individuals with long experience in the area where the technology is used is ideal to provide a range of viewpoints and expertise during the process of evaluating the evidence.
-
4
Experience with the specific technology: The hands‐on experience of practitioners in the field can provide another essential viewpoint, particularly when there is a lack of research in the literature.
-
5
Range of evidence: Finding different levels and types of evidence is important when there is not a lot of evidence to evaluate. A variety of evidence often provides insight into strengths and weaknesses of the total body of evidence and can more easily lead to identification of where the gaps are.
-
6
Realistic presentation of findings: Once a process is in place to evaluate the evidence, the reporting of that evaluation must be presented in such a way that:
-
•
appropriate follow‐up questions can be asked,
-
•
useful future research can build on the information reported,
-
•
decision‐makers can be confident in any decisions they make to accept, reject or defer the use of the technology.
WHAT IS TOPICAL PRESSURISED OXYGEN THERAPY?
Topical pressurised oxygen therapy * is a therapeutic modality that delivers humidified, pressurised oxygen directly to a specific body part to achieve tissue penetration and increased oxygen levels to the open ischaemic wound. Although hyperbaric therapy has been used for a century, topical pressurised oxygen therapy is relatively new, having been developed in 1969 by Dr Fischer, an Austrian engineer, physician and faculty member of the Institute of Rehabilitation Medicine at New York University (4).
Studies have shown that topical pressurised oxygen therapy raises tissue O2 levels to a depth of 2 mm within the wound bed, stimulates new blood vessel formation, supports synthesis and maturation of collagen deposition, leading to increased tensile strength and decreased recurrence of the wound. Increased oxygen levels at the wound site have shown to lead to the timely closure of wounds.
According to the distributor, topical pressurised oxygen therapy is currently available in the US under national contract for all Veterans Affairs Medical Centers to be used in the hospitals or in the home care setting. It is currently approved in five states for medical assistance recipients, with three more states in the approval mode. There are hospitals in Ohio that use them in the inpatient setting. Currently in Canada, topical pressurised oxygen therapy has been used in British Columbia, Ontario and Quebec.
HOW DOES TOPICAL PRESSURISED OXYGEN THERAPY DIFFER FROM OTHER FORMS OF OXYGEN THERAPY?
Systemic hyperbaric oxygen therapy (HBOT) is a treatment modality in which the patient breathes 100% oxygen at a pressure greater than one atmosphere: the pressure of air at sea level. This therapy occurs while the patient is entirely enclosed in a stationary pressure chamber. This therapy increases the plasma oxygen levels and is systemic, therefore dependent on adequate blood‐flow to the wound. As HBOT is systemic and raises the pO2, there is a risk of complications such as seizures, damage to the tympanic membrane of the ear (barotraumas) and damage to the retinal nerve (retinopathy). If patients have diabetes their glucose levels could also be affected by an increased pO2.
Topical pressurised oxygen therapy is also considered hyperbaric in that it also delivers 100% oxygen at a pressure greater than one atmosphere. However, it is a non invasive, portable therapy that uses a reusable acrylic chamber, vinyl extremity boot or vinyl multipurpose bag to deliver humidified pressurised oxygen directly to the wound bed. This method of delivery achieves tissue penetration and increased oxygen levels in the open wound without risk of systemic oxygen toxicity. Topical pressurised oxygen therapy is not dependent on systemic circulation reaching the wound bed.
Topical continuous oxygen therapy is the delivery of non pressurised, non humidified oxygen to the open wound via a cannula placed over the wound with a dressing topper.
USING NEW TECHNOLOGIES
All new technologies must be approved for use by the Food and Drug Administration (FDA in the United States) and by the Therapeutic Products Directorate, Medical Product through Health Canada, Health Products and Food Branch (in Canada). Products must be approved for safety issues such as electrical configuration, electromechanical interference (EMI), pressure testing and also to verify that each product does what the manufacturer says it does. Case studies and the science supporting the product need to be approved for the specific use indicated. Upon submission of an application for approval, the approval organisation reviews the diagnosis such as diabetic foot ulcer, venous stasis ulcer, pressure ulcer and examines how and why the device works. Topical pressurised oxygen therapy* is a licensed microportable version of a hyperbaric chamber and Health Canada granted licensing based on its safety and treatment effectiveness of chronic problem wounds (including diabetic foot ulcers), which is one of the 13 recognised the Undersea Hyperbaric Medical Society (UHMS) indications for hyperbaric treatment that we use to license hyperbaric chambers.
Although topical pressurised oxygen therapy is approved for use and studies have showed its effectiveness, there are still many questions that clinicians need to ask in order to maintain a high standard of care. This is true for any new – or even existing – technology:
-
1
Is this therapy appropriate for my patient and his/her wound at this point in time, considering indications, contraindications, precautions and warnings?
-
2
Has the physician/advanced practice clinician ordered the therapy with appropriate duration and frequency?
-
3
Is the type of device appropriate for the wound type?
-
4
Are the members of the wound care team properly trained in the use of this therapy?
-
5
Has the patient and his/her caregivers been trained in how to apply and/or monitor the device and what to do and who to contact in case of problems or emergencies?
-
6
Are the appropriate wound dressing materials being used?
-
7
Is there a standard for wound re‐evaluation to determine the therapy's effectiveness and when it can be discontinued?
-
8
Have appropriate arrangements been made for use of this therapy across the continuum of care (acute care, long‐term care, home care, outpatient)? Adapted from reference 5.
In an effort to address these questions and others, an independent, interprofessional advisory group (AG) was assembled to aggregate and weigh the evidence, set a standard for the delivery of topical pressurised oxygen therapy and determine where there were gaps in the evidence. †
METHODOLOGY – THE DELPHI METHOD
The process chosen to develop the set of standards was the Delphi method. The Delphi method has been linked with the term ‘collective intelligence’ used to support the development of a knowledge base by structuring a group communication process to facilitate consensus building and group problem‐solving. The product from this approach can lead to the dissemination and implementation of findings such as the publication of consensus statements that can guide health policy, clinical practice and research (6).
The advisory group
A Canadian interprofessional AG was selected to participate in the Delphi process. This group was chosen based on discipline and geographic location. Each individual also needed to meet four ‘expertise’ requirements: (i) knowledge and experience with wound care and/or topical pressurised oxygen therapy, (ii) capacity and willingness to participate, (iii) sufficient time to participate and (iv) effective communication skills.
The interprofessional members of the AG are
-
1
Joseph Baum: MD, FRCS(C), Department of Surgery, Division of Plastic Surgery, Etobicoke General Hospital, Ontario. He is a plastic surgeon with over 30 years experience treating complex surgical wounds. He has a special interest in wound care, introducing clinical use of negative pressure wound therapy (NPWT) to Canada, and is physician leader of a committee organising wound care at Etobicoke General Hospital. He has used topical pressurised oxygen therapy on wounds therapeutically on both inpatient and outpatient bases.
-
2
Dawn Christensen: BScN, RN, MHSc(N), CETN(C), Clinical Nurse Specialist/ Advanced Practice Nurse, KDS Professional Consulting, Ontario. She has been an enterostomal therapy nurse (with expertise in advanced wound care) since 1989 and currently consults on wound care at 30 long‐term care facilities and two community acute care hospitals in the Ottawa area. She is currently a member of and was a board member for the Canadian Association for Enterostomal Therapy and is a member of the Canadian Association of Wound Care.
-
3
Marc Despatis: BSc, MSc, RVT, MD FRCS, Vascular Surgery, Centre Hospitalier Universitaire de Sherbrooke, Quebec. He has many years of experience in wound care. He has been part of specialised clinics (diabetic foot ulcer and venous leg ulcer) working in multidisciplinary care in a university hospital. He has been involved with the Canadian Association of Wound Care over the last 10 years. He has no clinical experience with topical pressurised oxygen therapy.
-
4
Kyle Goettl: RN, BScN, MEd, IIWCC, Nurse Clinician, Amputee Rehabilitation, Parkwood Hospital, London, Ontario. He is a member of the Canadian Association of Wound Care, the Canadian Diabetes Association and is a graduate of the International Interprofessional Wound Care Course through the University of Toronto. He is also an associate scientist at the Lawson Health Research Institute and sits on the Medical Advisory Council for the Amputee Coalition of Canada. He is a member of the Chronic Wound and Skin Healthcare team at Parkwood Hospital and has worked in many specialty areas and as a research study nurse on various projects. He has been involved in many initiatives to advance best practice wound care and prevention of wounds for a wide variety of patient populations. He has had direct involvement in the selection and trialing of topical pressurised oxygen therapy on several inpatients at Parkwood hospital.
-
5
David Haligowski: BSc, MD, Family physician, Lecturer and Sessional instructor, University of Manitoba, member of the Uniting Primary Care and Oncology and Medical Director of Middlechurch Home of Winnipeg and River East Personal Care Home, Manitoba. He is a former director of the Canadian Association of Wound Care.
-
6
Chester Ho: MD, Physiatrist, Associate Professor and Head, Division of Physical Medicine and Rehabilitation, Department of Clinical Neurosciences, University of Calgary, Alberta. He has over 10 years of advanced wound care experience and founded the interdisciplinary skin care team and was the cochair of Skin Care Committee at Louis Stokes Cleveland Department of Veterans Affairs Medical Center. He has presented nationally and internationally on pressure ulcer management and also has an active research program on pressure ulcer issues, with research funding from national agencies and multiple peer‐reviewed publications on this topic. He has written many chapters in major Physical Medicine and Rehabilitation textbooks on the topic of pressure ulcers. He has used topical pressurised oxygen therapy clinically in his previous practice in Cleveland and in his current practice in Calgary with spinal cord injury patients with non healing, stage IV pressure ulcers.
-
7
Keith Louis: MD, Fellowship in general and vascular surgery, in practice since 1985 with a special interest in diabetic wounds, Ontario. He is currently involved in the wound care clinic at Brampton Civic Hospital sharing coverage with two Infectious Disease specialists. He is frequently consulted on diabetic wounds that are seen in‐hospital. He is also on the Canadian board of advisory surgeons for NPWT therapy and its related products. He has been involved in approximately six cases using topical pressurised oxygen therapy.
-
8
Deirdre O’Sullivan‐Drombolis: BSc PT, MClSc (Wound Healing), Physical Therapist and Wound Care Team Lead, Riverside Health Care Facilities, Fort Frances, Ontario. She is the wound care team lead and resource for Riverside Health Care Facilities in Fort Frances, Ontario. Her role involves implementing best practices in wound care through the development of policies and procedures, education as well as clinical practice. She is also an adjunct faculty for the University of Western Ontario Clinical Masters in Wound Healing Program and chairs the Northwestern Ontario Wound Community of Practice.
-
9
Valerie Winberg: RN(EC), BScN, MN, NP‐PHC, ENC(c), IIWCC, Emergency department, Chatham‐Kent Health Alliance, Project lead for Twin Bridges NP‐Led Clinic, Sarnia, Ontario. She has been a nursing professional for 25 years with extensive experience in all sectors of the healthcare environment, working many years in the emergency department first as a RN then as an NP, practising in primary care in the community and long‐term care, with the last 10 as a primary healthcare nurse practitioner. She was a founding member and an executive for the Ontario Woundcare Interest Group, an interdisciplinary political action group. She participates in wound consultations and wound care education for groups and as an international speaker. She has had experience with topical pressurised oxygen therapy with a variety of patients including First Nations peoples and with DM, venous and lower limb ulcers.
-
10
Kevin Woo: RN, MSc, PhD(c), ACNP, GNC(C), Assistant Professor, School of Nursing Queen's University, Kingston, Ontario. In addition to being on faculty for wound care programs, Dr Woo is an advanced wound care consultant, advisory board member for multiple wound care companies, and international speaker. He has topical pressurised oxygen therapy experience, including both trials and regular/occasional use.
The objective was to bring this group of experts together to create a document that would support efficient and effective clinical decision‐making relating to topical pressurised oxygen therapy. The following criteria were followed to represent the characteristics of the Delphi method:
-
1
Anonymity of Delphi participants: allowed the participants to freely express their opinions without undue pressures to conform to others in the group. Decisions were evaluated on their merit, rather than who had proposed the idea.
-
2
Iteration: allowed the participants to refine their views in light of the progress of the group's work from round to round.
-
3
Controlled feedback: informed the participants of the other participant's perspectives, and provided the opportunity for Delphi participants to clarify or change their views.
-
4
Statistical aggregation of group response: allowed for a quantitative analysis and interpretation of data.
Delphi method
The following steps (Figure 1) were required to complete this process:
Figure 1.
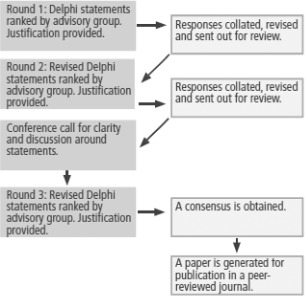
The Delphi method.
-
1
Step 1: Attended a conference call to introduce the AG members and discuss the process of the project.
-
2
Step 2: The AG members read the resource material provided to become familiar with the evidence supporting topical pressurised oxygen therapy technology.
-
3
Step 3: The AG members critically reviewed the draft Standards for Use of Topical Pressurised Oxygen Therapy document and appraised each statement, based on their experience/expert opinion and the supporting documents, by checking the appropriate responses: Agree, Somewhat agree or Disagree.
-
4
Step 4: If ‘Somewhat agree’ or ‘Disagree’ was checked, a comment was required stating why there was no agreement and identifying a recommendation to correct or improve the statement.
-
5
Step 5: The AG members returned the draft Standards for Use of Topical Pressurised Oxygen Therapy document for collation.
-
6
Step 6: Once all the reviews were received and collated a new document was created by the consultants based on the responses and sent for an additional round of reviews. Standards that did not achieve 80% endorsement were revised along with justification.
-
7
Step 7: Continued process (Steps 3 through 6) until consensus on the statements was obtained.
-
8
Step 8: A second conference call occurred for further discussion for clarification towards consensus building.
-
9
Step 9: Developed a consensus paper for peer‐reviewed publication.
-
10
Step 10: Set a revision plan for the document (recommended for 3–5 years).
THE RESOURCE MATERIAL
In January 2011, a literature search of PubMed was conducted by the manufacturer (AOTI Inc., West Galway, Ireland) to determine the level of evidence surrounding topical pressurised oxygen therapy. Twenty‐seven articles were identified using the following terms: oxygen therapy and wound healing. These articles were reviewed by the consultants from both the distributor and from eQuadra with six articles selected as being current and specific to topical pressurised oxygen therapy as well as having identified outcomes. Additionally, the manufacturer's website was considered as a resource because it contained recommendations for product use. Two other articles were identified to support a best practice approach to wound management as well as a standard for wound assessment. These nine resources were then used by the AG as the basis for their evaluations of the Standard statements to support the appropriate use of topical pressurised oxygen therapy (Table 1).
Table 1.
Advisory group resource material
| Resource material | Description |
|---|---|
| Topical wound oxygen therapy in the treatment of severe diabetic foot ulcers: a prospective controlled study: Blackman et al. (7) | Prospective controlled study |
| Improving accuracy of wound measurement in clinical practice: Flanagan (8) | Review of the literature |
| Dermal excisional wound healing in pigs following treatment with topically applied pure oxygen: Fries et al. (9) | Experimental study using a pre‐clinical model |
| Medical Director for AOTI: Frye (10) | Manufacturer's recommendations |
| Evidence‐based recommendations for the use of topical oxygen therapy in the treatment of lower extremity wounds: Gordillo et al. (11) | Summary of experimental, pre‐clinical and clinical findings |
| Topical oxygen therapy induces vascular endothelial growth factor expression and improves closure of clinically presented chronic wounds: Gordillo et al. (12) | Non randomised controlled study |
| New Therapeutic Angiogenesis Biomarkers for Chronic Diabetic Foot Ulcers Treated with Transdermal Hyperoxia/Topical Wound Oxygen (TWO2): Scott (13) | Experimental study |
| Best Practice Recommendations for preparing the wound bed: Update 2006: Sibbald et al. (14) | Summary of recommendations |
| Does topical wound oxygen (TWO2) offer an improved outcome over conventional compression dressings (CCD) in the management of refractory venous ulcers (RVU)? A Parallel Observational Study: Tawfick and Sultan (15) | Parallel group observational comparative study |
STANDARD STATEMENTS
Standard statements were developed from the resource material that best describes the use and usefulness of topical pressurised oxygen therapy and were agreed upon by the AG. The strength of the evidence for each standard was based on the Registered Nurses Association of Ontario (RNAO) Interpretation of the Evidence (Table 2).
Table 2.
Interpretation of the evidence
| Level | Description |
|---|---|
| Ia | Evidence obtained from meta‐analysis or systematic review of randomised controlled trials. |
| Ib | Evidence obtained from at least one randomised controlled trial. |
| IIa | Evidence obtained from at least one well‐designed controlled study without randomisation. |
| IIb | Evidence obtained from at least one other type of well‐designed quasi‐experimental study, without randomisation. |
| III | Evidence obtained from well‐designed non experimental descriptive studies, such as comparative studies, correlation studies and case studies. |
| IV | Evidence obtained from expert committee reports or opinions and/or clinical experiences from respected authorities. |
The standard statements and related discussion were placed into the following categories:
-
1
Product description
-
2
Patient selection
-
3
Patient preparation
-
4
Application principles
-
5
Evaluating therapy
-
6
Expected outcomes
-
7
Resources
-
8
Safety and precautions
The AG, using the Delphi method, finalised the statements and weighted the level of evidence as indicated in the Quick Reference Guide (Table 3).
Table 3.
Topical pressurised oxygen therapy: quick reference guide
| Category | Statement | Strength |
|---|---|---|
| Product description | Topical pressurised oxygen therapy is an adjunctive modality/device designed to support wound healing. | Level IIa |
| Topical pressurised oxygen therapy delivers humidified oxygen to the wound bed at cyclical pressures above atmospheric pressure. | Level IIa | |
| Topical pressurised oxygen therapy delivers oxygen into the wound bed, penetrating into the tissue approximately 2 mm deep. | Level IIb | |
| Patient selection | Topical pressurised oxygen therapy is indicated for the treatment of chronic wounds such as diabetic/neuropathic foot ulcers, venous stasis ulcers and pressure ulcers. | Level IIa |
| Topical pressurised oxygen therapy is contraindicated if the patient has an untreated acute DVT or acute thrombophlebitis. | Level IV | |
| Patient preparation | The presence of necrotic tissue must be minimised in the wound bed prior to the initiation of therapy. | Level III |
| The cause(s) of trauma and cofactors that may interfere with healing of the wound must be removed prior to the initiation of therapy. | Level IV | |
| Client and caregiver concerns must be addressed prior to the initiation of therapy. | Level IV | |
| Topical dressings post‐therapy must meet the needs of the wound in terms of debridement and bacterial and moisture balance. | Level IV | |
| Any dressings or preparations that create an oxygen‐impermeable barrier, such as any petrolatum‐based product or occlusive dressing, cannot be used in conjunction with topical pressurised oxygen therapy. | Level IV | |
| Application principles | The frequency and duration of therapy is dependent on wound aetiology, wound response and patient tolerance. | Level IV |
| Evaluating therapy | Patients being treated with topical pressurised oxygen therapy require assessment using standardised instruments and documentation on a regular basis according to agency healthcare setting practice and policy. | Level III |
| If wound closure is the goal and the wound is not reduced by 20–40% after 2–4 weeks of therapy despite efforts to address the underlying causes and cofactors, therapy should be discontinued and alternate methods sought. | Level IV | |
| Expected outcomes | Increased wound oxygenation, through the application of topical pressurised oxygen, results in increased collagen deposition and tensile strength. | Level IIa |
| Topically applied pressurised oxygen increases angiogenesis‐related growth factor expression in wound fluids from chronic diabetic foot ulcers that may be consistent with revascularisation and renewed healing. | Level IIa | |
| A lower recurrence rate may be expected in venous leg ulcers and diabetic foot ulcers following topical pressurised oxygen therapy. | Level III | |
| Topical pressurised oxygen therapy may reduce wound‐related pain in venous leg ulcers. | Level III | |
| Resources | Education needs to be provided to patients, caregivers and healthcare providers regarding the purpose and process of using topical pressurised oxygen therapy. | Level IV |
| Preliminary studies have shown that topical pressurised oxygen therapy has the potential for cost savings. | Level IV | |
| Safety and precautions | Protocols for oxygen safety must be followed when therapy is in use. | Level IV |
DVT, deep venous thrombosis.
DISCUSSION OF THE EVIDENCE
Product description
Topical pressurised oxygen therapy is an adjunctive modality/device designedto support wound healing, Level IIa.
Discussion: It is well established that oxygen is vital for wound healing through the synthesis of collagen, enhancement of fibroblasts, angiogenesis and leukocyte function. Oxygen also has key functions in energy metabolism and in the inhibition of microbial growth. Oxygen and reactive oxygen species are required and involved in all stages of wound healing: modulating cell migration, adhesion, proliferation, neovascularisation, remodelling and apoptosis 7, 9, 12, 15.
In acute and chronic wounds, a state of hypoxia frequently occurs during the inflammatory phase of wound healing and helps to ‘kick‐start' angiogenesis; however, increased O2 is necessary for continued wound healing (12) (Figure 2). Tissue hypoxia caused by disrupted or compromised vasculature can be a key factor that limits wound healing (11). This hypoxic state can occur because of capillary congestion, oedema, peripheral vascular disease (PVD) or peripheral arterial disease (PAD), where the wound does not get an adequate supply of oxygenated blood. Studies show that tissues must have a pO2 of at least 40 mm Hg in order to promote the production of FEGF, vascular endothelial growth factor (VEGF), collagen and most importantly restore angiogenesis and neovascularisation (12).
Figure 2.
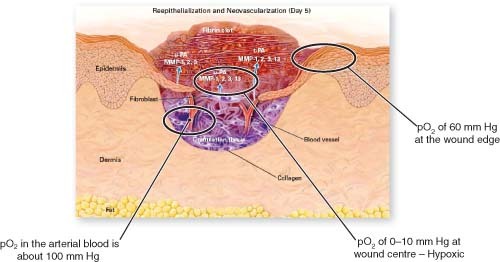
Oxygenation and trauma. Reprinted with permission from reference 10.
Topical pressurised oxygen therapy reduces hypoxia, promoting increases in FEGF for collagen formation and VEGF promoting neoangiogenesis (13). Topical pressurised oxygen therapy can generate a sustained increase in wound pO2, supporting angiogenesis; and in chronic human wounds it can induce a progressively increasing and sustained elevation of VEGF expression (11).
Topical pressurised oxygen therapy delivers humidified oxygen to the wound bed at cyclical pressures above atmospheric pressure, Level IIa.
Discussion: Topical pressurised oxygen therapy is a form of hyperbaric medicine in that it uses oxygen at a higher level than atmospheric pressure. The therapy consists of delivering pressurised, humidified 100% oxygen from 1·0 atmosphere absolute (ATA) to 1·03 atmospheres (ATA) topically to the wound bed and periwound skin. The atmospheric pressure increases in a sine‐wave amplitude (a smooth repetitive cycle) from baseline to plateau and then back to base line (7, 11, 12, 15).
Topical pressurised oxygen therapy delivers oxygen into the wound bed, penetrating into the tissue approximately 2 mm deep, Level IIb.
Discussion: Topical oxygen therapy increases the tissue pO2 of superficial wound tissue in pigs (9). Using a special probe designed to measure superficial pO2 at 2 mm depth at the centre of the wound bed, Fries et al. saw an increase of pO2 from less than 10 mm Hg to 40 mm Hg in as little as 4 minutes. Fries et al. showed by histology that wounds treated with oxygen that penetrated into the tissues showed signs of improved angiogenesis and tissue oxygenation in pigs (Figure 3).
Figure 3.

Oxygen penetrates to the cellular level supporting angiogenesis and enhancing collagen formation. Reprinted with permission from reference 10.
Patient selection
Topical pressurised oxygen therapy is indicated for the treatment of chronic wounds such as diabetic/neuropathic foot ulcers, venous stasis ulcers and pressure ulcers, Level IIa.
Discussion: Topical pressurised oxygen therapy has showed effectiveness as an adjunctive therapy to best practice for the management of acute and chronic diabetic/neuropathic foot ulcers, venous stasis ulcers, some mixed ulcers and pressure ulcers. It can also be an adjunctive therapy for treating wounds where hypoxia, oedema and increased bioburden are suspected to be key factors interfering with wound healing. In two studies with chronic wounds, topical pressurised oxygen therapy has shown to demonstrate no adverse responses (7, 11, 12, 15).
Topical pressurised oxygen therapy is contraindicated if the patient has an untreated acute deep venous thrombosis or untreated acute thrombophlebitis, Level IV.
Discussion: In the instance of acute untreated deep venous thrombosis (DVT) or thrombophlebitis, topical pressurised oxygen therapy is contraindicated. The cyclical positive pressure that is delivered by the hard chamber or extremity system may increase the risk that a clot may be dislodged and moved through the circulatory system, possibly promoting stroke, myocardial infarction or pulmonary emboli and risk of sudden death (10).
Patient preparation
The presence of necrotic tissue must be minimised in the wound bed prior to the initiation of therapy, Level III.
Discussion: Wounds should have at least 50% viable tissue exposed to allow for adequate oxygen to enter the tissues – therefore, it is imperative to remove as much eschar and slough from the wound bed as safely possible. Wounds can be debrided through surgical, sharp, autolytic, enzymatic, mechanical or larval methods. Topical pressurised oxygen therapy can then deliver pressurised oxygen directly to the surface of the wound, allowing oxygen penetration to achieve its maximum benefit (7, 11, 12, 14, 15).
The cause(s) of trauma and cofactors that may interfere with healing of the wound must be removed prior to the initiation of therapy, Level IV.
Discussion: The patient must be approached as a whole person. The clinician(s) need to address all the factors and cofactors that could interfere with healing before focus turns to the wound. The wound bed preparation model (Figure 4) promotes wound management through assessment, diagnosis and appropriate treatment of the cause, attention to patient‐centred concerns, and only then addresses local wound care. It is important to address factors that may interfere with wound healing through steps such as providing pressure‐relieving surfaces to reduce pressure and trauma, proper offloading to reduce trauma to diabetic foot ulcers and controlling oedema in the presence of venous leg ulcers. There are many cofactors, such as nutrition and hydration that should also be considered. Once these have been addressed, topical pressurised oxygen therapy can be adjunctive with the primary treatment strategies (11, 14).
Figure 4.
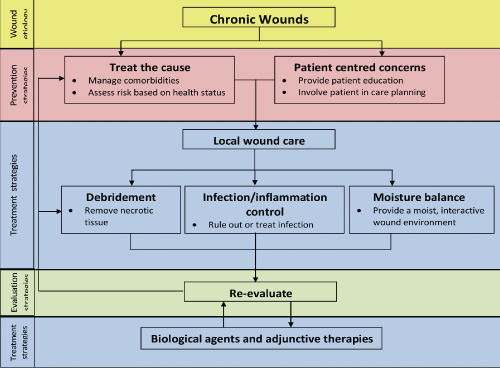
Wound bed preparation paradigm. Adapted with permission from reference 14.
Client and caregiver concerns must be addressed prior to the initiation of therapy, Level IV.
Discussion: The interdisciplinary team needs to work closely with patients, caregivers and their families to address the complex lifestyle, self‐care and multiple treatment demands of patients who have chronic wounds.
Patient concern is a key component of the wound bed preparation model (Figure 4) and supports patient adherence to therapy (14). Patient and caregiver concerns such as pain management, dressing removal and reapplication, signs and symptoms of infection, equipment usage – including proper application, troubleshooting, cleaning and maintenance – should all be considered and addressed with the patient and their caregivers (10).
Select a topical dressing post‐therapy that meets the needs of the wound in terms of debridement and bacterial and moisture balance, Level IV.
Discussion: Clinicians should base dressing selection on the patient history and assessment, the cause of the wound, and the evaluation of the wound bed and periwound skin. The dressing should address the needs of the wound with a focus on its ability to support debridement, bacterial and moisture balance (Figure 3). Because the dressing needs to be removed and reapplied once or twice a day the dressing should not cause trauma with frequent removal (14).
Any dressings or preparations that create an oxygen‐impermeable barrier, such as any petrolatum‐based product or occlusive dressing, cannot be used in conjunction with topical pressurised oxygen therapy, Level IV.
Discussion: Many wound care products have components that will prevent or restrict oxygen from penetrating the wound bed. Petrolatum is a semi‐solid mineral oil product that is often used in wound dressings and can create an occlusive wound covering that can interfere with topical oxygen delivery. Occlusive barriers, film dressings and any products that may restrict oxygen access to the wound bed should also be avoided during therapy (9, 10, 11).
Application principles
The frequency and duration of therapy is dependent on wound aetiology, wound response and patient tolerance, Level IV.
Discussion: The manufacturer has recommended protocols for topical pressurised oxygen therapy (Table 4) based on the hyperbaric protocols identified by the UHMS, to determine the frequency and duration of the therapy. However, these may need to be modified based on studies, clinician experience, wound aetiology and patient tolerance (10, 11, 15, 16).
Table 4.
Recommended protocols for topical pressurised oxygen therapy.
| Ulcer type | Diabetic foot ulcers | Venous leg ulcers | Pressure ulcers |
|---|---|---|---|
| Frequency | OD or BID | BID | OD or BID |
| Duration | 120 minutes | 180 minutes | 120–180 minutes |
| Device | Extremity system | Extremity system | Multipurpose bags |
OD, once a day; BID, twice a day.
For burns and post‐surgical wounds: frequency, duration and devices will be determined based on the location of the wound and orders.
Evaluating treatment
Patients being treated with topical pressurised oxygen therapy require assessment using standardised instruments and documentation on a regular basis according to agency healthcare setting practice and policy, Level III.
Discussion: Patients usually respond to therapy very quickly; within the first 3–5 days their wound bed and periwound skin should show noticeable changes. These changes will include reduced size (length, width and depth), diminished periwound oedema, increased granulation tissue, less drainage, less slough or eschar as well as less pain suffered by the patient. Consistent and reliable wound assessment remains a clinical challenge for wound care clinicians. A wound assessment standard needs to be identified, consistently done and documented in the patient record (9, 10, 14, 15).
If wound closure is the goal and the wound is not reduced by 20–40% after 2–4 weeks of therapy, despite efforts to address the underlying causes and cofactors, therapy should be discontinued and alternate methods sought, Level IV.
Discussion: Once the therapy has begun the wound should be assessed at regular intervals following institutional/agency policies and using a standardised method or tool to determine if the therapy is effective in wound closure. If sinus tracts are present these should be measured and documented as well (10, 15).
Wound closure is not always the only endpoint with therapy. The clinician has the option to take the wound to full closure and epithelialisation or until the identified goals or endpoints have been met. Topical pressurised oxygen therapy can improve the wound to a point that it can be treated with conventional methods. Topical pressurised oxygen therapy may be used to achieve goals such as:
-
•
Promoting a granulation wound bed.
-
•
Challenging a wound that is not responding to traditional closure methods.
Expected outcomes
Increased wound oxygenation, through the application of topical pressurised oxygen, results in increased collagen deposition and tensile strength, Level IIa.
Discussion: Although a level of hypoxia is normal during the inflammatory phase of wound healing, a chronic hypoxic state is not conducive to tissue healing and can lead to tissue necrosis (11). Adequate tissue oxygenation, as provided by topical pressurised oxygen therapy, promotes the formation of VEGF‐2 and FEGF which in turn increases the production of collagen 9, 11. Collagen synthesis is dependent on the hydroxylation of proline and lysine, and the increase of pO2 converts proline residues to hydroxyproline. This process allows the procollagen peptide chains to assume the triple helix configuration. Once the procollagen has assumed the triple helix conformation and has been excreted, the individual collagen fibres are arranged into linear fibrils via cross‐linking of lysyl hydroxylase and a final cross‐linking between large fibrils. These cross‐linkages are ultimately responsible for tensile strength in healed wounds (12).
Topically applied pressurised oxygen alters angiogenesis‐related growth factor expression in wound fluids from chronic diabetic foot ulcers that may be consistent with revascularisation and renewed healing, Level IIa.
Discussion: Topical pressurised oxygen therapy has shown a consistent and persistent elevation in the expression of biomarkers VEGF and fibroblast growth factor (FGF)‐2 throughout the therapy. Both VEGF and FGF‐2 promote epithelialisation and capillary neoangiogenesis. These biomarkers, as measured by Scott, quantify therapeutic angiogenesis, indicating evidence of renewed activation of dormant cells in chronic wounds and therefore promote healing (11, 12).
A low recurrence rate may be expected in venous leg ulcers and diabetic foot ulcers following topical pressurised oxygen therapy, Level III.
Discussion: Topical pressurised oxygen therapy promotes epithelialisation and capillary neoangiogenesis, leading to the formation of higher collagen tensile strength during wound healing. This in turn has shown to reduce scarring and risk of ulcer recurrence. Blackman et al. showed no recurrence after 24 months in either the control group or the group that received topical pressurised oxygen therapy. Tawfick et al. showed after 36 months, that 8 of the 13 healed ulcers in the control group recurred compared to none of the 37 healed ulcers in the group that received topical pressurised oxygen therapy (7, 15).
Topical pressurised oxygen therapy may reduce wound‐related pain in venous leg ulcers, Level III.
Discussion: The oscillating cyclical nature of the therapy is thought to assist in removing the interstitial oedema in the tissue, relieving the pain associated with venous stasis and the extreme tensions placed on the tissues. Patients indicated their pain levels fell from eight to three on the pain scale upon commencement of the therapy (15).
Resources
Education needs to be provided to patients, caregivers and healthcare providers regarding the purpose and process of using topical pressurised oxygen therapy, Level IV.
Discussion: Once an order is obtained for the therapy and its duration, healthcare professionals, personal support workers (PSWs) as well as patients and their family members can be instructed on how to set‐up and apply topical pressurised oxygen therapy. Selection for who may administer the therapy must be based on the healthcare policy and procedures. The identified individual(s) must receive training on the equipment and its use from a designated distributor employee or designate. Healthcare professionals need to be skilled in providing accurate follow‐up for wound assessment and documentation as well as post‐treatment dressing application and care (10).
In order to support patient and caregiver understanding and adherence to treatment regimens, several strategies can be used in combination:
-
1
Emphasise the value of the patient's regimen and the positive effects of adherence.
-
2
Create a patient regimen that is simple – with simple, clear instructions.
-
3
Listen to the patient and customise the regimen to his/her lifestyle.
-
4
Enlist support from the patient's family, friends and community services when needed.
Preliminary studies have shown that topical pressurised oxygen therapy has the potential for cost savings, Level IV.
Discussion: Tawfick and Sultan showed at 12 weeks that 80% of the venous leg ulcers were closed in the topical pressurised oxygen therapy group compared with 35% closure in control group. The median time to full closure for all ulcers was 45 days for topical pressurised oxygen therapy group versus 182 days in control group. Fourteen of 17 (82·4%) ulcers in the topical pressurised oxygen therapy group closed, with a median average of 56 days. 5 of 11 (45·45%) of the ulcers closed in the control group, with median average of 93 days (7, 15).
In contrasting the topical pressurised oxygen therapy group with the control group, cost savings are evident in the areas of physician visits, debridement, dressing, antibiotics and hospitalisations – and also in possible amputations.
According to Blackman et al.‘The significant differences in treatment outcomes confirm the potential in the benefits of topical pressurised oxygen therapy in the management of difficult to heal diabetic foot ulcers (DFUs). Clinical efficacy and cost‐effectiveness studies are warranted.’
Safety and precautions
Protocols for oxygen safety must be followed when topical pressurised oxygen therapy is in use.
Discussion: Because oxygen is a non flammable and non explosive gas it does not burn; however, it does support combustion. Any material that will burn in air will ignite more readily in an oxygen‐enriched environment. According to the Ontario Ministry of Health and Long‐Term Care, oxygen users must take precautions when using oxygen. Keep oxygen systems away from sources of heat or open flame. Patients, caregivers, family or visitors should not smoke or let anyone else smoke in the area where oxygen is in use. Patients need to be reminded that smoking is not only a health risk but it eliminates the benefits of oxygen therapy. A warning sign must be posted wherever oxygen is in use; as well the local fire department should be notified there is oxygen in the home. Oxygen needs to be stored in a well‐ventilated non confined area. Frost injuries to the skin can occur if filling is not done correctly, so the manufacturers' recommendations must be followed to ensure the safe and effective use of this therapy. Vaseline or other petroleum products containing grease or oils, petroleum jelly, alcohol or flammable liquids that can cause oxygen to be flammable should not be on or near an oxygen system (17).
FURTHER STUDIES
Further studies are required to determine if topical pressurised oxygen therapy is indicated for the treatment of acute post‐surgical wounds, skin grafts and flaps, and burns. Identified endpoints such as reduced peripheral oedema and decreased bacterial burden also require further research.
In addition, randomised controlled trials (RCTs) would be beneficial to increase the evidence around the use and effectiveness of topical pressurised oxygen therapy and to establish optimal parameters for use. Current studies show the efficacy of the therapy in DFUs and venous leg ulcers (VLUs). However, there is variation in protocols and dosing methods, and therefore RCTs are warranted to improve understanding of the parameters for use.
There have been no studies found that show improved quality of life for patients receiving topical pressurised oxygen therapy. It has been implied that if topical pressurised oxygen therapy can close wounds more quickly and efficiently, the patients can retain their limbs and remain ambulatory and can be a part of the contributing work force. However, endpoints identifying the patient's perspective are needed to show improved quality of life.
Although studies have suggested that topical pressurised oxygen therapy is cost effective there have been no specific cost effectiveness studies completed.
CONCLUSION
Clinicians addressing wound care concerns are often bombarded by therapies claiming to heal wounds. The review undertaken in this initiative used a recognised methodology for systematically exploring the evidence around topical pressurised oxygen therapy to identify statements that are not only evidence‐based but also agreed upon by experts in the field. The result is this document, which provides a standard by which clinicians and decision/policy makers can make an informed decision on the use of topical pressurised oxygen therapy regarding the appropriateness of implementation into practice. It also identifies where further research is required to provide a more complete picture regarding the effective use of topical pressurised oxygen therapy.
Footnotes
Topical pressurized oxygen therapy (TPOT) is approved by the Therapeutic Products Directorate as a Class 2 Medical Product through Health Canada, Health Products and Food Branch.
TSS, the Canadian distributors of topical pressurized oxygen therapy, engaged services of eQuadra Solutions Inc. (London, ON) to assemble an advisory group of 10 experts. Through the use of a modified Delphi method, eQuadra facilitated a process for arriving at consensus statements and identifying gaps in the evidence.
REFERENCES
- 1. The Leader‐Post. Regina. 6 October 2006.
- 2. Integrated Client Care Project. From the report to their steering committee, 11 September 2009.
- 3. Ontario Ministry of Health and Long‐Term Care. Bill 46, An Act respecting the care provided by health care organizations. Queen's Printer for Ontario, 2008 [WWW document]. URL http://www.health.gov.on.ca/en/legislation/excellent_care/ [accessed on 23 June 2010].
- 4. Fischer BH. Topical hyperbaric oxygen treatment of pressure sores and skin ulcers. Lancet 1969;23:405–9. [DOI] [PubMed] [Google Scholar]
- 5. Krasner D. NPWT standards of care: 9 questions to ask. WoundSource [WWW document].URL http://www.woundsource.com/blog/npwt‐standards‐care‐9‐questions‐ask [posted on 16 February 2011].
- 6. Jones J, Hunter D. Qualitative research: consensus methods for medical and health services research. BMJ 1995;311:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blackman E, Moore C, Hyatt J, Railton R, Frye C. Topical wound oxygen therapy in the treatment of severe diabetic foot ulcers: a prospective controlled study. Ostomy Wound Manage 2010;56:24–31. [PubMed] [Google Scholar]
- 8. Flanagan M. Improving accuracy of wound measurement in clinical practice. Ostomy Wound Manage 2003;49:28–40. [PubMed] [Google Scholar]
- 9. Fries RB, Wallace WA, Roy S. Dermal. Dermal excisional wound healing in pigs following treatment with topically applied pure oxygen. Mutat Res 2005;579:172–81. [DOI] [PubMed] [Google Scholar]
- 10. Frye C. Medical Director for AOTI. Advanced oxygen therapy (AOTI) [WWW document]. URL www.aotinc.net [accessed on 13 June 2011].
- 11. Gordillo GM, Sen CK. Evidence‐based recommendations for the use of topical oxygen therapy in the treatment of lower extremity wounds. Int J Low Extrem Wounds 2009;8:105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gordillo GM, Roy S, Khanna S, Schlanger R, Khandelwal S, Phillips G, Sen CK. Topical oxygen therapy induces vascular endothelial growth factor expression and improves closure of clinically presented chronic wounds. Clin Exp Pharmacol Physiol 2008;35:957–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Scott GF. New therapeutic angiogenesis biomarkers for chronic diabetic foot ulcers treated with transdermal hyperoxia/topical wound oxygen (TWO2). Fort Worth: Department of Cell Biology and Genetics, University of North Texas Health Science Center, 2005. [Google Scholar]
- 14. Sibbald RG, Orsted HL, Coutts P, Keast D. Best Practice Recommendations for preparing the wound bed. Update 2006. Advances in Skin & Wound Care 2007;20:368–415. [DOI] [PubMed] [Google Scholar]
- 15. Tawfick W, Sultan S. Does topical wound oxygen (TWO2) offer an improved outcome over conventional compression dressings (CCD) in the management of refractory venous ulcers (RVU)? A parallel observational study. Eur Soc Vasc Surg 2009;38:125–32. [DOI] [PubMed] [Google Scholar]
- 16. Undersea Hyperbaric Medical Society (UHMS). Treatment protocols [WWW document].URL http://membership.uhms.org/?page=Indications [accessed on February 2011].
- 17. Ontario Ministry of Health and Long‐Term Care. ADP: Home oxygen program. Queen's Printer for Ontario 2002. URL http://www.health.gov.on.ca/english/public/pub/adp/oxygen.html [accessed on 15 June 2009].


