Abstract
The aim of this study was to measure the prevalence of (infected) chronic wounds in Dutch nursing homes and to explore which signs and symptoms are used to diagnose infected chronic wounds. Moreover, it was to determine which structural quality indicators related to chronic wound care at ward and institutional levels were fulfilled. In April 2012, as part of the annual National Prevalence Measurement of Care Problems of Maastricht University [Landelijke Prevalentiemeting Zorgproblemen (LPZ)], a multi‐center cross‐sectional point‐prevalence measurement was carried out together with an assessment of relevant care quality indicators. The prevalence was 4·2%; 16 of 72 (22%) chronic wounds were considered to be infected. Increase of exudate (81·3%; n = 13), erythema (68·8%; n = 11), pain (56·3%; n = 9) and wound recalcitrance (56·3%; n = 9) were considered to be diagnostic signs and symptoms of a chronic wound infection. Although at institutional level most quality indicators were fulfilled, at ward level this was not the case. Despite the relatively low number of residents, we consider our population as representative for the nursing home population. It may be an advantage to appoint specific ward nurses and to provide them specifically with knowledge and skills concerning chronic wounds.
Keywords: Chronic wound, Infection, Prevalence, Quality indicators
Introduction
When wound healing does not proceed normally, and the anatomic and functional integrity of the skin is not reached within a few weeks, a wound is considered to be chronic 1, 2. Although a chronic wound is often defined by mentioning the wound type based on different underlying aetiology, as pressure ulcers, venous leg ulcers and diabetic foot, knowledge of intrinsic and extrinsic factors that contribute to wound recalcitrance is essential to provide successful wound care 3, 4. Vascular insufficiency and infection are important factors responsible for the non‐healing of wounds 5. Wound infection implies the multiplication of micro‐organisms resulting in a prolonged (and excessive) inflammatory response, a delay in collagen synthesis, retarded epithelialisation and finally in tissue damage 6, 7, 8, 9. In 1994, Cutting and Harding reviewed the literature and demonstrated the signs and symptoms on which to base the diagnosis of wound infection10. In 2008, the World Union of Wound Healing Societies published its guideline on diagnosing wound infection 11.
For improving the care for patients with chronic wounds, it is important to have insight in the prevalence of chronic wounds, the characteristics of patients vulnerable for chronic wounds and the signs and symptoms of chronic wound infection. Getting attention and being aware of a problem are the first steps in the process of improving care. With prevalence data about chronic wounds and the quality of care for patients with chronic wounds, awareness can be created in caregivers, managers, policymakers and politicians. Subsequently, interventions to improve the care for patients with chronic wounds can be initiated.
Since 1998, The Dutch National Prevalence Measurement of care problems [Landelijke Prevalentiemeting Zorgproblemen (LPZ)] measures yearly the prevalence and related quality indicators of different care problems including pressure ulcers, incontinence, malnutrition, falls, restraints and intertrigo. Since 2012, the LPZ focuses also on chronic wounds. This study describes the results of the first LPZ measurement of chronic (infected) wounds in Dutch nursing homes.
In the Netherlands, disabled persons with physical diseases or with progressive dementia, mainly the elderly who are not able to manage their daily activities, and suffer from many comorbidity and care problems and who need plural, more complex continuing care are often admitted to a nursing home. There are about 345 nursing homes with about 63 000 beds, 27 000 in somatic wards and 36 000 in psychogeriatric wards. Nursing homes employ their own multidisciplinary staffs, consisting of elderly care physicians, nurses, physiotherapists, occupational therapists, speech therapists, dieticians, psychologists, social workers, pastoral workers and recreational therapists 12. Until now, no data have been published on the prevalence of chronic wounds and wound care policy related to chronic wounds in Dutch nursing homes.
The aims of this study were to answer the following questions:
What is the prevalence of (infected) chronic wounds in Dutch nursing homes?
What are the most common types of chronic wounds, wound locations on body and actual duration of these wounds?
Which signs and symptoms are used to diagnose infected chronic wounds?
Which dressings are used for the management of chronic wounds?
Which structural quality indicators related to chronic wounds at ward and institutional level are fulfilled in Dutch nursing homes?
Method
Design
This study was part of the annual National Prevalence Measurement of care problems of Maastricht University [Landelijke Prevalentiemeting Zorgproblemen (LPZ), Van Nie et al.] 13. The design of the study involved a multi‐centre cross‐sectional point‐prevalence measurement and was carried out in April 2012.
Sample
For the LPZ study, all the 345 nursing home organisations in the Netherlands were invited by mail to participate voluntarily. Of the 158 participating elderly organisations, 21 nursing home organisations agreed to participate in the module on chronic wounds. Patients were included if they gave informed consent, and were ≥18 years old.
Data collection
This annual LPZ measurement took place on 3 April 2012. Each participating organisation appointed a coordinator, who was responsible for organising the measurement. The coordinators were trained collectively by the research group on how to manage the survey, and how to use the standardised questionnaires and the specially designed Internet data‐entry program (www.LPZ‐UM.eu). As a regular procedure, to achieve objective judgment for every patient, all patients were assessed by a rater pair of two health care professionals (nurses or physicians; one of whom worked on the patient's ward and one independent).The coordinators also received a protocol and training package to support them in training the health care professionals who would perform the measurement within their organisations. LPZ participants could find all the information needed for the measurement and data entry on a purpose‐built website. The LPZ measurement includes several care problems. Each institution can decide which care problems need to be measured.
Instrument
For the module on chronic wounds, a standardised questionnaire focusing on four levels being wound, patient, ward and nursing home, was used. At the wound level, a rater pair assessed whether a patient had a wound that had lasted more than 3 weeks. If so, an experienced wound care nurse, or when not available, the elderly care physician (ECP), filled in a questionnaire about each chronic wound. Besides questions related to the type of the chronic wound and whether the wound was infected, questions were also incorporated about the signs and symptoms [based on World Union of Wound Healing Societies (WUWHS) 2008] on which the diagnosis of a chronic wound infection relied on. Additionally, questions were asked about undertaken diagnostic assessments, the type of wound dressings used, and the use of anti‐microbials in relation to the existing wound, in the last 3 months. At the patient level, information was collected by the rater pair about demographic characteristics (sex, age, mobility and operation), diseases registered in the medical records and the degree of care dependency (as measured using the Care Dependency Scale) 14. At the ward level, the head of the department filled in an eight‐item questionnaire with dichotomous (yes/no) answer categories about specified quality indicators at the ward level related to the care of chronic wounds (Table 3). At the institutional level, the institutional coordinator filled in an eight‐item questionnaire with regard to specified structural quality indicators at the institutional level related to the care of chronic wounds. These quality indicators were derived from the original LPZ structural indicators for pressure ulcers and intertrigo 15.
Table 3.
Quality indicators related to chronic wound care at institutional level (n, %)
| Quality indicators | Nursing homes (n = 21) |
|---|---|
| Approved protocol/guideline for prevention and treatment | 14 (66) |
| Patients having a chronic wound for more than 3 weeks are reported to a central contact (e.g. an experienced nurse in wounds or pressure ulcers) | 17 (81) |
| Central registration of the number of patients suffering from chronic wounds | 21 (100) |
| In the last 2 years, a training and/or thematic meeting on the prevention and treatment of chronic wounds has been organised | 21 (100) |
| Information brochure on wounds for patients available | 14 (66) |
| Standard policy at admission or discharge, with regard to information transfer in the chain care | 20 (95) |
Data analysis
Descriptive analyses were performed with SPSS version 20.0 (SPSS Inc, Chicago, IL).
Results
Twenty‐one nursing homes with 61 wards agreed to participate in the prevalence measurement of chronic (infected) wounds (Table 1). In total 1514 patients were assessed, which is a response of 96·4% in the participating wards; 67% were female and the mean age was 82 years (SD 10·0).
Table 1.
Signs and symptoms of infected chronic wounds (n, %) as assessed by the wound care nurses or elderly care physicians (ECPs)
| Signs and symptoms of infected chronic wounds | Infected chronic wounds (n = 16) |
|---|---|
| Pain | 9 (56·3%) |
| Erythema | 11 (68·8%) |
| Local warmth | 1 (6·3%) |
| Swelling | 4 (25·0%) |
| Induration | 0 (0%) |
| Smell | 0 (0%) |
| Increase of (purulent) exudate | 13 (81·3%) |
| Delayed (or stalled) healing | 9 (56·3%) |
| Bleeding or friable (easily damaged) granulation tissue | 2 (12·5%) |
Chronic wounds
Sixty‐three of 1514 patients had one or more chronic wounds, which results in a prevalence of 4·2%. These patients had a total of 72 chronic wounds. Almost half (46%) of these wounds were pressure ulcers (Figure 1), followed by post‐surgical wounds (9·5%).
Figure 1.
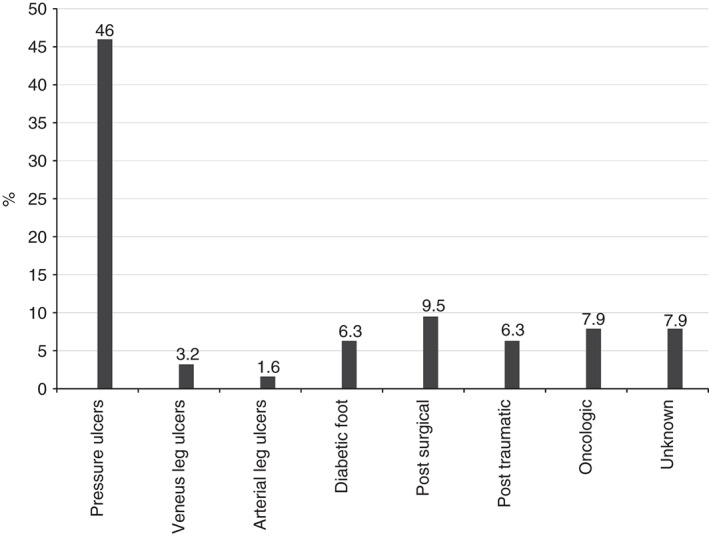
Prevalence of the different chronic wounds on the total number of chronic wounds.
The most frequently identified body locations of chronic wounds were the trunk (n = 16; 22·2%), hip or thigh (n = 11; 15·3%) and the legs of the patients (n = 9; 12·5%). Seven (10%) of the chronic wounds were located at the heel or foot. Other locations included 17% of all chronic wounds.
Most chronic wounds existed for a period shorter than 3 months (n = 45; 62·5%).
Sixteen of 72 (22%) chronic wounds were considered to be infected. In Table 1 the different signs and symptoms used to diagnose these chronic infected wounds are shown. The wound care nurses or elderly care physicians considered especially an increase of exudate (81·3%; n = 13), the existence of erythema (68·8%; n = 11), pain (56·3%; n = 9) and wound recalcitrance (56·3%; n = 9) as relevant clinical signs and symptoms to identify a chronic wound infection (Table 1).
In Table 2 the different dressings used for the management of chronic wounds are shown.
Table 2.
Dressings used for chronic wound management (n)
| Type of dressing | Non‐infected chronic wounds | Infected chronic wounds |
|---|---|---|
| Dry | 2 | 0 |
| Alginate | 4 | 1 |
| Film | 0 | 4 |
| Hydrocolloïd | 2 | 0 |
| Hydrogel | 2 | 1 |
| Foam | 6 | 0 |
| Impregnated fatty gauze | 2 | 2 |
| Negative pressure wound therapy (NPWT) | 0 | 0 |
| Anti‐bacterial | 1 | 5 |
| Hydrofiber | 6 | 0 |
| Other | 26 | 3 |
| None | 2 | 0 |
Of all 16 wounds considered to be infected, 5 were managed with an anti‐bacterial type of dressing, 4 with some kind of film dressing, 1 with hydrogel, 2 with impregnated fatty gauzes and 3 wounds were covered with other kind of dressings mentioned specifically (Table 2).
Quality indicators of chronic wound care
In Tables 3 and 4 the results of the structural quality indicators related to chronic wound care at institutional respective ward level are shown.
Table 4.
Quality indicators related to chronic wound care at ward level in 2012 (n; %)
| Quality indicators | Wards (n = 61) |
|---|---|
| Wound care nurse for chronic wounds | 7 (11) |
| Discussion of patients within multidisciplinary meetings | 4 (7) |
| Implementation of a protocol/guideline | 8 (13) |
| Cause of chronic wound is mentioned in the patient record | 1 (2) |
| Preventive measures are mentioned in the patient record | 20 (33) |
| Information brochure on chronic wounds | 0 |
| Standard information transfer at discharge | 60 (98) |
Institutional level
In all participating nursing homes, the number of patients with a chronic wound was centrally registered and every 2 years, a training on prevention and treatment was organised. In 20 nursing homes, a standard policy on admission or discharge was available with regard to information transfer to another care provider. However not every nursing home had a protocol/guideline dealing with chronic wounds and/or an information brochure for residents and family on chronic wounds (Table 2).
Ward level
In Table 4 the results of the answers with regard to the quality indicators at ward level are shown. Although at institutional level, most structural indicators were fulfilled, at ward level most indicators were not.
The transfer of wound related information was a normal procedure at the time of discharge of a patient in almost all wards. In 20 wards the preventive measures were mentioned in the patient records, and in only 8 wards a chronic wound protocol was implemented. In seven wards there was a wound care nurse, specifically taking care of chronic wounds, while discussing patients in a multidisciplinary setting was carried out in only four wards. The aetiology of chronic wounds was listed at one of the 61 wards. Although it was indicated that institutions had an information brochure on chronic wounds available, it has not been distributed to patients at the ward level.
Discussion
To the best of our knowledge, this study measured the prevalence of (infected) chronic wounds in Dutch nursing homes for the first time. The results showed a prevalence of chronic wounds of 4·2% in a Dutch nursing home population of 1514 residents. Nearly 50% of the wounds were located on the trunk, hip or thigh, whereas 46% of all chronic wounds were pressure ulcers; 62·5% of the chronic wounds existed for a period of less than 3 months. Experienced wound nurses and/or ECPs assessed that 22% (n = 16) of the 72 chronic wounds were infected. Erythema, exudate, pain and wound recalcitrance were the signs and symptoms they based this diagnosis on. At institutional level all of the measured structural quality indicators scored 66% or more. Except for the chronic wound related information at admission or discharge, all quality indicators scored much lower at ward level. A chronic wound protocol was implemented in only 8 of the participating 61 wards. In seven of these, a specific wound care nurse took care of chronic wounds, while discussing patients in a multidisciplinary meeting was carried out in only four wards.
Wounds tend to occur more in elderly patients and in those with a poor clinical condition, and are therefore common in nursing homes 16. Although the impact on the quality of life of patients suffering from a chronic wound has been well documented 17, 18, very little is known of the prevalence of chronic wounds. In an urban population (London, UK), Moffat et al. made a rough ascertainment of leg ulceration in 0.45/1000 population (113/252000), with more than 4 weeks duration and a mean age of 75 (range 31–94 years) 19. Except for the study by Moffat et al. there are none on the prevalence of (infected) chronic wounds 19. Identification of infection in acute and chronic wounds in daily clinical practice in general is merely based on clinical signs and symptoms 20. The signs and symptoms of infected chronic wounds are often subtle and a correct diagnosis of the infection is difficult to make 11, 21, 22, 23, 24, 25, 26. Using the WUWHS criteria, the experienced wound‐care nurses and/or ECPs assessed 16 chronic wounds as infected 11. Considering that the diagnosis of chronic wound infection in itself is difficult 10, 11, 23, 24 and that the nurses and ECPs were not specifically trained, it is possible that their assessment of 16 chronic wounds as being infected is just an estimation. The consensus document of the World Union of Wound Healing Society shows ‘increase of purulent exudate’ and ‘erythema’ as triggers for suspecting a localised infection in an acute wound 11. This study showed that the nurses and ECPs still used ‘traditional’ criteria of wound infection. These observations were already found for Dutch elderly‐care physicians in 2009 10, 24.
This study also shows that different dressings were used for the management of (infected) chronic wounds. It is rather striking that in only 30% (5/16) of the wounds, considered to be locally infected, anti‐bacterial dressings were used. It is even more striking that in these infected wounds, film dressings, hydrogels and impregnated fatty gauzes not having any anti‐microbial capacity were used. However, pre‐mature conclusions must not be drawn, because of the small numbers involved. In this study 21 nursing homes and 1514 patients participated. This is a small part of the 345 (in 2003) nursing homes with about 63 000 residents in the Netherlands' study. The measured prevalence of 2·4% for chronic pressure ulcers in this study was comparable with the prevalence of pressure ulcers existing for more than 2 weeks measured by Halfens et al., for a much larger population of care home residents in the Netherlands 15. Although this study sample is relatively small and the participating nursing homes were mostly located in two southern provinces of the Netherlands (Brabant and Limburg), the distribution between countryside and cities was even. The similarity in chronic pressure ulcer prevalence between this study and the one of Halfens, leads to the careful impression that the results of this study are representative for all 345 nursing homes in the Netherlands. Indeed, in this study, pressure ulcers were the most common chronic wounds and because the patient characteristics (gender, age and BMI) in both Halfens' 15 and our study were very similar, the representativeness of the results of this study for all nursing homes in the Netherlands is enforced.
The burden of chronic wounds is unknown in most health economics, owing to the wide variation in definition and management of chronic wounds 27. Therefore in 2010 Fletcher argued the necessity of a consistent methodology, and an on‐going surveillance system for the UK 27. In the Netherlands, from 2012, an on‐going surveillance has been set up by the LPZ, measuring the prevalence of (infected) chronic wounds and related quality indicators, twice a year and in a consistent manner. Prevalence data about chronic wounds and the quality of care for patients with chronic wounds will contribute to the awareness of caregivers, managers, policymakers and politicians. Subsequently, interventions to improve the care for patients with chronic wounds can be initiated. Taking into account the low scores of the structural quality indicators at the ward level, development of wound care policy should specifically focus on creating the possibility of conducting a multidisciplinary discussion on (infected) chronic wounds and their registration as part of the patients' treatment plan. For the implementation of adequate measures, appointment of specific ward nurses and ward physicians with knowledge and skills on chronic wounds is warranted.
References
- 1. Lazarus GS, Cooper DM, Knighton DR, Margolis DJ, Pacaro RE, Rodeheaver G, Robson MC. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch Dermatol 1994;130:489–93. [PubMed] [Google Scholar]
- 2. Robson MC. Wound infection. A Failure of wound healing caused by an imbalance of bacteria. Surg Clin North Am 1997;77:637–50. [DOI] [PubMed] [Google Scholar]
- 3. Bates‐Jenssen BM. Chronic wound assessment. Surg Clin North Am 1999;34:799–845. [PubMed] [Google Scholar]
- 4. Seaman S. Considerations for the global assessment and treatment of patients with recalcitrant wounds. Ostomy Wound Manage 2000;46(1A Suppl):10–29. [PubMed] [Google Scholar]
- 5. Mostow EN. Diagnosis and classification of chronic wounds. Clin Dermatol 1994;12:3–9. [DOI] [PubMed] [Google Scholar]
- 6. Robson MC, Stenberg BD, Hegger JP. Wound healing alterations caused by infections. Clin Plast Surg 1990;17:485–92. [PubMed] [Google Scholar]
- 7. Mast BA, Schultz GS. Interactions of cytokines, growth factors, and proteases in acute and chronic wounds. Wound Rep Reg 1996;4:411–20. [DOI] [PubMed] [Google Scholar]
- 8. Cooper RA. The contribution of microbial virulence to wound infection. Br J Nurs 2002;7(3 Suppl):10–14. [Google Scholar]
- 9. Ovington LG. Feature: bacterial toxins and wound Healing. Ostomy Wound Manage 2003;49(7A Suppl):8–12. [PubMed] [Google Scholar]
- 10. Cutting KF, Harding KG. Criteria for identifying wound infection. J Wound Care 1994;3:198–201. [DOI] [PubMed] [Google Scholar]
- 11. Special Issue: Wound Infection in Clinical Practice: an International Consensus. Int Wound J 2008;5(3 Suppl):iii–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schols JMGA, Crebolder HF, Weel C van. Nursing home and nursing home physician: the Dutch experience. J Am Med Dir Assoc 2004;5:207–12. [DOI] [PubMed] [Google Scholar]
- 13. Nie Van NC, Halfens RJG, Meijers JMM, Meesterberends E, Neyens JCL, Rondas AALM, Schols JMGA. Rapportage Resultaten: Landelijke Prevalentiemeting Zorgproblemen. Maastricht: Universitaire Pers Maastricht, 2013. [Google Scholar]
- 14. Dijkstra A, Tiesinga LJ, Plantinga L, Veltman G, Dassen TW. Diagnostic accuracy of the Care Dependency Scale. J Adv Nurs 2005;50:410–16. [DOI] [PubMed] [Google Scholar]
- 15. Halfens RJG, Meijers JMM, Meesterberends E, Nie NC van, Neyens JCL, ALM Rondas en JMGA Schols . Rapportage Resultaten: Landelijke Prevalentiemeting Zorgproblemen. Maastricht: Universitaire Pers Maastricht, 2012. [Google Scholar]
- 16. Posnett J, Franks PJ. The burden of chronic wounds in the UK. Nurs Times 2008;104:44–5. [PubMed] [Google Scholar]
- 17. Franks PJ, Morgan PA. Health‐related quality of life with chronic leg ulceration. Expert Rev Pharmacoecon Outcomes Res 2003;3:611–22. [DOI] [PubMed] [Google Scholar]
- 18.International consensus Optimizing wellbeing in people living with a wound. Wound International An expert working group review. London: Wounds International, 2012. URL http://www.woundsinternational.com[accessed on 7 September 2013].
- 19. Moffat CJ, Franks PJ, Doherty DC, Martin R, Blewett R, Ross F. Prevalence of leg ulceration in a London population. Q J Med 2004;97:431–7. [DOI] [PubMed] [Google Scholar]
- 20. Rondas AALM, Schols JMGA, Halfens RJG, Stobberingh EE. Swab versus biopsy for the diagnosis of chronic infected woundsa literature review. Adv Skin Wound Care 2013;26:211–9. [DOI] [PubMed] [Google Scholar]
- 21. Bowler PG, Duerden BI, Armstrong DG. Wound microbiology and associated approaches to wound management. Clin Microbiol Rev 2001;14:244–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dow G. Bacterial swabs and the chronic wound: when, how and what do they mean. Ostomy Wound Manage 2003;49(5A Suppl):8–13. [PubMed] [Google Scholar]
- 23. Cutting KG, White RJ, Mahoney P, Harding KF. Clinical identification of wound infectiona Delphi approach. In: Position document on identifying criteria for wound infection. London: Medical Education Partnership Ltd, 2005. [Google Scholar]
- 24. Rondas AALM, Schols JMGA, Stobberingh EE, Price PE. Definition of infection in chronic wounds by Dutch nursing home physicians. Int Wound J 2009;6:267–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Reddy M, Gill SS, Wu W, Kalkar SR, Rochon PA. Does this patient have an infection of a chronic wound? JAMA 2012;307:605–11. [DOI] [PubMed] [Google Scholar]
- 26. Cutting KF, White RJ, Mahoney P. Wound infection, dressings and pain, is there a relationship in the chronic wound? Int Wound J 2013;10:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fletcher J. NHS West Midlands guide for quality in the commissioning and delivery of chronic wound prevention and treatment services, 2010. URL http://www.scribd.com/doc/118444791/Nhs‐West‐Midlands‐Chronic‐Wounds‐Toolkit [accessed on 7 September 2013]


