Abstract
This study presents the results of a descriptive, cross‐sectional, online international survey in order to explore current practices in the assessment, prediction, prevention and treatment of skin tears (STs). A total of 1127 health care providers (HCP) from 16 countries completed the survey. The majority of the respondents (69·6%, n = 695) reported problems with the current methods for the assessment and documentation of STs with an overwhelming majority (89·5%, n = 891) favouring the development of a simplified method of assessment. Respondents ranked equipment injury during patient transfer and falls as the main causes of STs. The majority of the samples indicated that they used non‐adhesive dressings (35·89%, n = 322) to treat a ST, with the use of protective clothing being the most common method of prevention. The results of this study led to the establishment of a consensus document, classification system and a tool kit for use by practitioners. The authors believe that this survey was an important first step in raising the global awareness of STs and to stimulate discussion and research of these complex acute wounds.
Keywords: Assessment, Elderly, Prevention, Skin tears, Treatment
Background
Skin tears (STs), a condition of compromised skin integrity, are far more common than many believe, occurring even more frequently than pressure ulcers 1. Prevalence rates for STs have been reported to be as high as 41% 1, 2. STs, while beginning as acute wounds, can encounter complications and become chronic wounds 2. Individuals suffering from STs complain of increased pain that, in addition to other biopsychosocial factors associated with chronic wounds such as physical disability, social needs and mental anguish, can have a negative impact on an individual's quality of life. Populations at the highest risk for STs include those at extremes of age and the critically or chronically ill. These individuals are at a higher risk for developing secondary wound infections and have comorbidities 2, 3, 4. Health care professionals must become cognizant of which individuals are at risk for developing STs, how to prevent these wounds, and how to treat them once they occur. As most STs result from equipment or a fall, many should be preventable 5. Unfortunately, a dearth of literature existed on the appropriate prevention, assessment and management of STs, leaving it a continuing challenge for health care providers (HCP). Based on this knowledge, an international survey was conducted to solicit input from wound care professionals on their perceptions of the extent of the problem of STs in a variety of health care or community settings.
Introduction
When queried about their perceptions of STs, many health care individuals may respond ‘So what?’ Unfortunately there has been a perception among health care professionals that there are so many other conditions ‘more serious’ than STs, resulting in an inadequate amount of scientific study devoted to this condition. However, STs are acute wounds and have the potential of becoming a chronic, complex wounds in some instances 2. In order to begin establishing the extent to which health care professionals encounter STs and how they are managed, and to ultimately create a paradigm shift, a survey was designed to gather such data from a wide variety of international health care professionals as a means of documenting the problem.
Method
A descriptive, cross‐sectional, online international survey was undertaken between June 2010 and December 2010 to explore current practices in the assessment, prediction, prevention and treatment of STs. A convenience sampling method was used to disseminate the link to the online survey (http://www.surveymonkey.com/home/) to health care professionals known to the International Skin Tear Advisory Panel (ISTAP) members. Participants were also invited via online and print journals advertisement to participate in the study; hence it was difficult to determine an accurate estimate of the total number of individuals the survey reached. The data collection tool for the survey was designed specifically for this study. It consisted of 15 questions, six of which required a simple binary response (yes/no). The questions were designed to elicit responses about HCPs' experiences with STs. The data was analysed using the survey software, and frequencies and percentages were generated to provide information on the assessment and management of STs.
Ethics
Completing and submitting the survey implied consent. The research team at no time had access to the names and email contact lists of participants. Confidentiality and anominity were guaranteed. The surveys were completed online and directly downloaded to the Survey Monkey database. Survey Monkey has been awarded TRUSTe's Privacy Seal signifying that TRUSTe has reviewed Survey Monkey's privacy policy and practices for compliance with transparency, accountability and choice regarding the collection and use of personal information. Data was stored on a secure, password‐protected server. As this survey was an online International survey and anominity and confidentiality were guaranteed, the research team did not seek independent ethical approval.
Results
A total of 1127 HCP from 16 countries completed the survey (Table 1). Almost three‐quarters (73·4%, n = 843) of the respondents were from USA and the majority of the total sample worked in acute care (66·2%, n = 746). Registered nurses (RN) represented 77·4% (n = 872) of the sample.
Table 1.
International skin tear survey results (n = 1127)
| n | % | |
|---|---|---|
| What is your country of practice? | ||
| USA | 843 | 73·4 |
| Canada | 131 | 11·4 |
| Australia | 79 | 6·9 |
| UK | 55 | 4·8 |
| Mainland Europe | 16 | 1·4 |
| Japan | 3 | 0·3 |
| Total number of respondents | 1127 | |
| What is your primary area of practice? | ||
| Acute care | 746 | 66·2 |
| Long‐term care | 197 | 17·5 |
| Home care | 190 | 16·9 |
| Hospice/palliative care | 24 | 2·1 |
| Rehabilitation care | 62 | 5·5 |
| Paediatric care | 16 | 1·4 |
| Total number of respondents | 1127 | |
| What are your credentials? | ||
| RN | 872 | 77·4 |
| LPN/RPN | 36 | 3·2 |
| CNS | 118 | 10·5 |
| NP/APN | 109 | 9·7 |
| MD/DO/DPM | 37 | 3·3 |
| Total number of respondents | 1127 | |
| Wound care specific qualification | ||
| WOCN/CETN/ET/WCC/CWS | 295 | |
RN, registered nurses; WOCN, wound ostomy continence nurse; CETN, certified enterostomal therapy nurse; ET, enterosotmal therapists; WCC, wound care clinician; CWS, certified wound specialist; LPN, license practical nurse; RPN, registered practical nurse; CNS, Clinical nurse specialist; NP, nurse practitioner; APN, advanced practice nurse; MD, medical doctor; DO/ DPM, podiatrist.
A quarter of the sample indicated that they treated between 20 and 49 wounds in a typical week (25·6%, n = 259) with slightly fewer treating between 1 and 5 wounds/week (21·5%, n = 217). Of the number of wounds treated, 63·3% of the respondents indicated that approximately 1–5% were STs.
The majority of the respondents (69·6%, n = 695) reported a problem with current assessment and documentation of STs in their practice settings. Furthermore an overwhelming percentage of the sample (89·5%, n = 891) favoured a simplified method for documenting and assessing STs. A total of 80·9% (n = 790) of respondents reported that they did not use any tool or classification system for assessing and documenting STs but the majority did report completing a weekly wound assessment on all STs (62%, n = 619; Table 2).
Table 2.
Use of classification systems for skin tears and wound assessment
| n | % | |
|---|---|---|
| Does your facility/hospital/home care agency use any of the following scales for assessing and documenting skin tears? | ||
| Payne–Martin classification system for skin tears | 98 | 10·0 |
| CAWC best practice recommendations | 32 | 3·3 |
| STAR classification system | 57 | 5·8 |
| None | 790 | 80·9 |
| Missing data | 150 | |
| Total number of respondents | 977 | |
| Do you complete a weekly wound assessment on all skin tears? | ||
| Yes | 619 | 62 |
| No | 379 | 38 |
| Missing data | 129 | |
| Total number of respondents | 998 | |
CAWC, Canadian Association of Wound Care; STAR, Skin Tear Audit Research.
Respondents were also asked what terms they used to document STs. Subsequent to content analysis of the responses to this question the following common terms were identified (Table 3). The majority of the terminology relates to the definition of a ST.
Table 3.
Terms used to document a skin tear
| Terms used to document a skin tear | Total number of responses |
|---|---|
| Partial thickness {superficial} (n = 181) | 463 |
| Scrape or abrasion (n = 21) | |
| Loss of epidermis or stripping (n = 18) | |
| Flap (n = 91) | |
| Full thickness (n = 80) | |
| Linear (n = 18)/laceration (n = 24)/tear (n = 12)/slit (n = 1)/peel (n = 1) | |
| Avulsion (n = 8)/degloved (n = 1)/deroofed (n = 7) | |
| Skin tear | 303 |
| Category 1, 2, 3/I, II, III (n = 30) | 62 |
| Payne–Martin (n = 17) | |
| STAR (n = 15) | |
| Pressure ulcer‐related terminology (n = 16)/friction/burn/shear (n = 10) | 26 |
| Skin lesion (n = 4)/open wound (n = 16)/ecchymotic (n = 3)/tape stripping (n = 2) | 25 |
| No term used | 13 |
| Skipped question | 335 |
Respondents ranked equipment injury, patient transfer and falls as the top three causes of STs with blunt trauma being ranked the least frequent (Table 4 and Figure 1). With regards to location the arms and legs were the most commonly reported areas prone to STs (Table 5 and Figure 2).
Table 4.
Most commonly reported causes of skin tears (n = 1012)
| Rank the top three causes of skin tears | ||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | Rating average | n | ||
| 1 | Equipment injury | 280 | 231 | 227 | 1·93 | 738 |
| 2 | During patient transfer | 202 | 248 | 149 | 1·91 | 599 |
| 3 | Dressing/treatment related | 130 | 139 | 166 | 2·08 | 435 |
| 4 | While performing ADLs | 127 | 162 | 162 | 2·08 | 451 |
| 5 | Falls | 214 | 150 | 180 | 1·94 | 544 |
| 6 | Blunt trauma | 46 | 46 | 77 | 2·18 | 169 |
| 7 | Missing data | 115 | ||||
| Total number of respondents | 1012 | |||||
ADL, Activities of daily Living.
Figure 1.
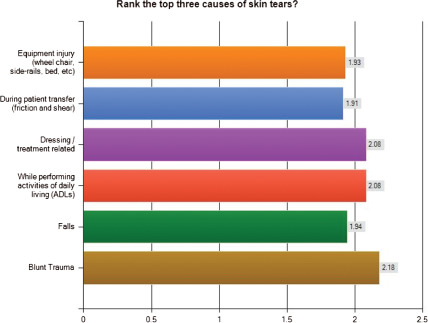
Most commonly reported causes of skin tears (n = 1012).
Table 5.
Most commonly reported areas that skin tears occur (n = 1012)
| Rank order the top three common areas of the body that you see skin tears | ||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | Rating average | n | ||
| 1 | Arms | 789 | 152 | 49 | 1·25 | 990 |
| 2 | Legs | 165 | 602 | 144 | 1·98 | 911 |
| 3 | Head, neck, and face | 17 | 27 | 189 | 2·74 | 233 |
| 4 | Back, shoulders | 19 | 28 | 198 | 2·73 | 245 |
| 5 | Buttocks | 72 | 162 | 360 | 2·48 | 594 |
| 6 | Missing data | 115 | ||||
| Total number of respondents | 1012 | |||||
Figure 2.
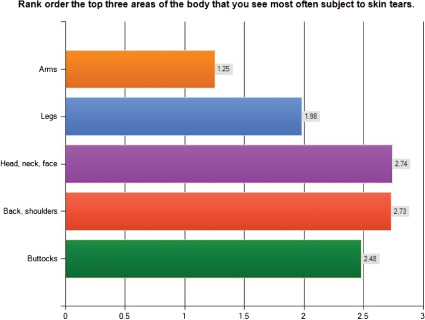
Most commonly reported areas that skin tears occur (n = 1012).
Respondents were asked to record what treatment options were currently used in clinical practice. The majority of the sample indicated they used non‐adhesive dressings (35·89%, n = 322; Figure 3). A further 204 respondents (22·74%) reported using skin closures or tape and 190 (21·18%) described using foam dressings.
Figure 3.
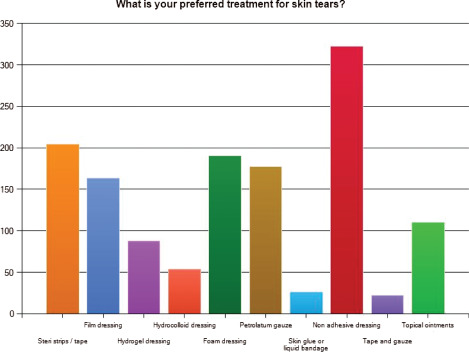
Reported treatment options for skin tears (n = 897).
Participants were asked to provide information on what their facility did to prevent STs. Table 6 summarises the responses to this question. The replies indicate that skin care was used most frequently, as was the use of protective clothing. Other preventative measures included education, careful manual handling and transfers as well as using risk assessment tools to identify those patients most at risk of skin damage.
Table 6.
What does your facility do to prevent skin tears?
| What does your facility do to prevent skin tears? (multiple responses) n = 833 respondents | Number of responses | % |
|---|---|---|
| Moisturisers (creams)/skin prep (barrier)/skin care programme | 262 | 31 |
| Protective clothing or devices for limbs | 219 | 26 |
| Education | 171 | 14 |
| Careful manual handling/use of lifting or transfer equipment | 156 | 31 |
| Risk assessment measures | 146 | 18 |
| Cautious use of tape/dressings | 82 | 10 |
| Appropriate choice of dressing | 32 | 4 |
| Pad side rails/wheelchairs or equipment | 65 | 8 |
| Refer to dietician/refer to other specialists | 50 | 6 |
| Pressure ulcer related responses | 43 | 5 |
| Audit/Monitor/incident reporting | 21 | 3 |
| Policy/protocol for prevention | 21 | 3 |
| Hourly (frequent) rounding or monitoring of patient/skin | 7 | 1 |
| Nail/jewellery policy | 5 | 1 |
| Bed alarms/wander guards | 4 | <1 |
| Visual alerts on Beds, that is,. ‘Please take care of my skin’ or ‘Fragile Skin Alert’ | 2 | <1 |
| Missing response | 138 | 17 |
The final question asked respondents whether their facility used any clinical guidelines or protocols for skin care. Over three‐quarters of the sample indicated they did use a guideline or protocol (77·3%, n = 772; Table 7).
Table 7.
Use of clinical guidelines/protocols for skin care
| Does your facility follow clinical practice guidelines/protocols for skin care? | ||
|---|---|---|
| n | % | |
| Yes | 772 | 77·3 |
| No | 227 | 22·7 |
| Missing data | 128 | 11·4 |
| Total number of responses | 999 | |
Discussion
The purpose of this survey was to explore and gather data on current beliefs and practices associated with the prediction, prevention, assessment and management of STs. Given the limited literature available pertaining to these wounds, the authors viewed this cross‐sectional survey as a key starting point in establishing the extent to which health care professionals encounter STs and how they are managed, and to ultimately create a paradigm shift to have STs viewed as acute wounds that have a high risk of becoming complex acute wounds if mismanaged 2.
The results of the study indicated that a quarter of the sample treated between 20 and 49 wounds in a typical week with slightly fewer treating between 1 and 5 wounds per week. Of the number of wounds treated the majority of respondents indicated that approximately 1–5% were STs. This supports previous statements in the literature 2, 6, 7, 8, 9 that they have a prevalence rate which is potentially equal to or higher than pressure ulcers. Given the predicted high prevalence of STs, it is imperative that STs are reported and documented in a consistent manner using a universal language for description and documentation. It has been reported in the literature that there is no consistency in the assessment and documentation of STs 3, 8, 9. The majority of the respondents in the current survey reported a problem with current assessment and documentation of STs in their practice settings. Furthermore, an overwhelming percentage of the sample favoured a simplified method for documenting and assessing STs. Many of the respondents reported that they did not use any tool or classification system for assessing and documenting STs but the majority did report completing a weekly wound assessment on all STs.
Patients who are dependent on others for total care are at the greatest risk for STs 10. These patients frequently acquire STs during routine activities such as dressing, bathing, repositioning and transferring. Independent ambulatory patients are at the second highest risk and the majority of their STs occur on their lower extremities. In the elderly population STs are often related to the environment 11. In 1990, Payne and Martin 12 conducted a 3‐month, descriptive study in 10 long‐term care facilities to describe STs, identify risk factors and determine the rate of healing of STs. Among the predominant risk factors, impaired activity, mobility, sensation and cognition all demonstrated an increased risk for ST development. McGough‐Carny and Kopac 13 conducted a similar study in a Veterans Affairs nursing home and concluded that dependency in activities of daily living, sensory loss, limited mobility, use of assistive devices and impaired cognition were risk factors for ST development. When STs are reported, the causative factor is often not known. When the cause is known, STs are frequently linked to wheelchair injuries; blunt trauma from accidently bumping into objects, transfers or falls 4, 5. White et al 10 concluded that key times during which STs occur are during the peak activity hours of 6:00 AM–11:00 AM and 3:00 PM–9:00 PM. In this survey respondents ranked, equipment injury, patient transfer and falls as the top three causes of STs with blunt trauma being ranked the least frequent. With regards to location the arms and legs were the most commonly reported areas prone to STs.
Product selection for the management of STs should be dependent on a comprehensive assessment of the patients and their wounds. Dressing selection should be based on choosing a dressing that will maintain a moist wound environment, be appropriate in accordance to the local wound environment, protect the peri‐wound skin, control or manage exudate, control or manage infection, optimise caregiver time and minimise pain 3, 5, 14, 15. Best practice supports that a skin flap/pedicle should be approximated if possible, and covered with one of the following type of dressings: hydrogel, alginate, lipido‐colloid‐based mesh, foam dressings, soft silicone, absorbent clear acrylic dressing or non‐adherent impregnated gauze mesh dressing applied depending on wound bed characteristics 2. Hydrocolloids and transparent film dressings are not recommended over STs, as they may cause skin stripping and injury to the healing ST if not removed properly 9, 16. In this survey respondents were asked to record what treatment options were currently used in clinical practice. The majority of the sample indicated that they used non‐adhesive dressings, adhesive strip dressings or tape and foam dressings. This may indicate that further education is required to ensure that interventions to minimise the risk of additional trauma are used.
The responses to the survey about what their facility did to prevent STs indicated that skin care protocols were used most frequently, as was the use of protective clothing. Other preventative measures included education, careful manual handling and transfers as well as using risk assessment tools to identify those patients most at risk of skin damage. These results were encouraging as they indicate that practitioners are taking into account strategies for prevention as well as treatment and management. The responses related to whether facilities used any clinical guidelines or protocols for skin care showed that over three‐quarters of the sample indicated that these were used. This supports previous claims that help to diminish the impact of STs on our health care systems, it is imperative that a systematic prevention programme be implemented 9.
Development of definitions and the ISTAP Toolkit
In response to these survey results, ISTAP as part of a consensus document established an agreed definition for STs, which states that, ‘A skin tear is a wound caused by shear, friction and/or blunt force resulting in the separation of skin layers. A skin tear can be partial thickness (separation of the epidermis from the dermis) or full thickness (separation of both the epidermis and the dermis from the underlying structures)’. Building on the consensus document and the survey results, in 2012 ISTAP developed and validated the ISTAP Skin Tear Classification system 9, thus fulfilling the need for a simplistic and accurate method for describing and documenting STs.
The ISTAP have also established a tool kit based on this initial survey to aid in the prevention, assessment and treatment of STs 17. The tool kit is based on an extensive literature review, international input from health care professionals and expert opinion. It has undergone an extensive peer review in the form of a modified Delphi process. The goal of the ISTAP Skin Tear Tool Kit was to provide a foundation to assist and guide individuals, their circle of care and health care professionals in the risk assessment, prevention and treatment of STs.
The ISTAP Skin Tear Tool Kit is designed to allow the clinician to implement a systematic approach to the prevention, management and treatment of STs. The tool kit includes components that will serve as a basis for education and implementation guidance for prevention and treatment programmes. It includes the following:
risk assessment pathway
ST decision algorithm
pathway to assessment/treatment of STs
ISTAP Classification System
prevalence study data collection sheet
quick reference guide
medications that can affect the skin
high‐risk drugs associated with fall
product selection guide
During the development of the tool kit, ISTAP recognised that STs are unique in that they are common acute wounds in older adults. However, the critically ill, neonate and paediatric population are also at risk for STs. The role of identifying STs using a comprehensive skin assessment requires further study.
Conclusion
The international survey was designed and conducted in order to begin establishing the extent to which health care professionals encounter STs and how they are managed, and to ultimately create a paradigm shift. This study explored current practices in assessment, prediction, prevention and treatment of STs. The results of this study support the current literature and supported the establishment of the ISTAP's consensus document, the ISTAP Skin Tear Classification System and the ISTAP Tool Kit to aid in the prevention, assessment and treatment of STs using a simplified classification system. It is acknowledged that the majority of the respondents to the questionnaire were from North America so results may not be generalizable. The survey was an important first step in raising the global awareness of STs and to stimulate discussion and research of these complex acute wounds.
References
- 1. Carville K, Lewin G, Newall N, Haslehurst P, Michael R, Santamaria N, Roberts P. STAR: a consensus for skin tear classification. Prim Intent 2007;15:18–28. [Google Scholar]
- 2. LeBlanc K, Baranoski S, Skin Tear Consensus Panel Members . Skin tears: state of the science: consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care 2011;24(9 Suppl):2–15. [DOI] [PubMed] [Google Scholar]
- 3. LeBlanc K, Baranoski S. Prevention and management of skin tears. Adv Skin Wound Care 2009;22:325–32. [DOI] [PubMed] [Google Scholar]
- 4. Bank D, Nix D. Preventing skin tears in a nursing and rehabilitation centre: an interdisciplinary effort. Ostomy Wound Manage 2006;52:38–46. [PubMed] [Google Scholar]
- 5. LeBlanc K, Christensen D, Orsted H, Keast D. Best practice recommendations for the prevention and treatment of skin tears. Wound Care Canada 2008;6:14–32. [Google Scholar]
- 6. LeBlanc K, Christensen D, Culhane B, Cook J. Pilot study of the prevalence of skin tears in a long term care facility in eastern Ontario, Canada 2011. J Wound Ostomy Continence Nurs 2013; 580–84. [DOI] [PubMed] [Google Scholar]
- 7. Carville K, Lewin G. Caring in the community: a prevalence study. Prim Intent 1998;6:54–62. [Google Scholar]
- 8. Carville K, Smith JA. Report on the effectiveness of comprehensive wound assessment and documentation in the community. Primary Intent. 2004;12:41–8. [Google Scholar]
- 9. LeBlanc K, Baranoski S, Holloway S, Langemo D. Validation of a new classification system for skin tears. Adv Skin Wound Care 2013;26:263–5. [DOI] [PubMed] [Google Scholar]
- 10. White M, Karam S, Cowell B. Skin tears in frail elders. A practical approach to prevention. Geriatr Nurs 1994;15:95–9. [DOI] [PubMed] [Google Scholar]
- 11. Ratliff CR, Fletcher KR. Skin tears: a review of the evidence to support prevention and treatment. Ostomy Wound Manage 2007;53:32–42. [PubMed] [Google Scholar]
- 12. Payne R, Martin M. The epidemiology and management of skin tears in older adults. Ostomy Wound Manage 1990;26:26–37. [PubMed] [Google Scholar]
- 13. McGough‐Carny J, Kopac CA. Skin tears in institutionalized elderly: An epidemiological study. Ostomy Wound Manage 1998;44(3A Suppl):14S–25. [PubMed] [Google Scholar]
- 14. Sibbald RG, Orsted HL, Coutts PM, Keast DH. Best practice recommendations for preparing the wound bed: update 2006. Wound Care Canada 2006;4:15–29. [DOI] [PubMed] [Google Scholar]
- 15. Stephen‐Haynes J, Callaghan R, Bethell E, Greenwood M. The assessment and management of skin tears in care homes. Br J Nurs 2010;20:S12–6. [DOI] [PubMed] [Google Scholar]
- 16. Edwards HE, Gaskill D, Nash RE. Treating skin tears in nursing home residents: pilots study comparing four types of dressings. Int J Nurs Pract 1998;4:25–32. [DOI] [PubMed] [Google Scholar]
- 17. LeBlanc K, Baranoski S, Christensen D, Langemo D, Sammon MA, Edwards K, Holloway S, Gloeckner M, Williams A, Sibbald RG, Regan M. International Skin Tear Advisory Panel: a tool kit to aid in the prevention, assessment and treatment of skin tears using a simplified classification system. Adv Skin Wound Care 2013;26:459–76. [DOI] [PubMed] [Google Scholar]


