Abstract
The aim of this study was to evaluate the effectiveness of applying locally made pressure off‐loading techniques on plantar foot ulcer in individuals with diabetes. This prospective study of 70 diabetic patients was conducted at the foot clinic of Baqai Institute of Diabetology & Endocrinology. Plantar foot ulcer, stages 1A and 2A according to the University of Texas classification, was treated by using three off‐loading techniques: modified foot wear (sandal), modified plaster of Paris cast with plywood platform and Scotchcast boot. The outcome was assessed at either complete wound healing (defined as complete epithelialisation) or at 12 weeks, whichever came first. Of the 70 patients, 24 were in modified foot wear group, 23 in modified plaster of Paris cast and 23 in Scotchcast boot group. There was almost equal proportion of patients healed within 12 weeks period treated with these three off‐loading techniques, i.e. 22 (95·7%) for modified foot wear group, 19 (95%) for modified plaster cast and 18 (94·7%) for Scotchcast boot group. No significant difference was observed in median healing time and cumulative wound survival at 12 weeks in the three off‐loading techniques. Modified foot wear group was the most cost effective ($7) amongst the three off‐loading techniques. It is concluded that in this cohort, no significant difference in healing time was observed in the three off‐loading techniques, although modified foot wear (sandal) was found to be a more cost‐effective treatment modality.
Keywords: Foot ulcer, Off loading, Pakistan
Introduction
Foot ulceration is the most common underlying cause of amputation in individuals with diabetes 1. Peripheral neuropathy and increased dynamic foot pressure have shown to predict an increased risk of foot ulceration 2. Several studies have demonstrated the increase in dynamic foot pressure in neuropathic foot 2, 3, 4, 5, 6, 7, 8.
High plantar foot pressure is a major risk factor in the development of plantar foot ulceration. Pressure on ulcer bed and repetitive trauma are the two major causes of persistence of ulcer once developed 9. Many methods can be used to offload an area of pressure to give the tissue time to heal without repetitive stress which leads to delayed wound healing, while keeping the patient ambulatory.
Total contact cast (TCC) is considered the gold standard modality in offloading and treating diabetic neuropathic ulcer 10, 11 and other modalities, such as DH Pressure Relief Walker, Charcot Restraint Orthotic Walker and Healing Sandal, are also being used for offloading the pressure at ulcer site.
Neuropathic ulcerations on the plantar aspect of the foot develop secondary to neuropathy and increase plantar peak pressure along with shear stress. Hence, decreasing the peak plantar pressure and transverse shear force is the most appropriate treatment 12, which is accomplished by offloading the ulcer site.
These offloading devices are not being used in Pakistan because of many reasons including the unavailability of materials, lack of expertise and the cost involved. To the best of our knowledge, this is the first study that shows the effectiveness of off‐loading devices in people with diabetes in Pakistan.
The aim of this study was to evaluate the effectiveness of locally made pressure off‐loading techniques [i.e. modified foot wear (sandal), modified plaster of Paris cast with plywood platform and Scotchcast boot] on plantar foot ulcer in individuals with diabetes.
Methodology
A prospective study of 70 diabetic patients was conducted at the foot clinic of Baqai Institute of Diabetology & Endocrinology (BIDE). Ethical approval for the study was obtained from the Institutional Review Board of the institute. Patients were randomised into one of the three off‐loading techniques through computerised randomisation schedule: modified foot wear (sandal), modified plaster of Paris cast with plywood platform and Scotchcast boot, after obtaining signed informed consent.
Inclusion and exclusion criteria
Individuals with diabetes having a significant loss of protective sensation, who were unable to sense 10 g Semmes–Weinstein monofilament and a vibration perception threshold of >25 V as measured using biothesiometer, and having plantar foot ulcer stages 1A and 2A according to the University of Texas classification were included in this study. Patients who had clinical evidence of infection at ulcer site, active Charcot neuropathy, significant peripheral vascular disease defined as absent dorsalis pedis or posterior tibial pulse and inability to walk were excluded.
All the study patients were followed up in the diabetic foot clinic on weekly basis for device inspection, wound care and wound debridement if needed. A window was made for wound cleansing and debridement in both modified plaster of Paris cast with plywood platform and Scotchcast boot made of fibreglass material.
Wounds were measured and photographs were taken at each visit. The outcome was assessed at either complete wound healing (defined as complete epithelialisation) or at 12 weeks, whichever came first. The cost of the three off‐loading techniques, which included the cost of materials (including plaster of Paris, cast padding, plywood, fibreglass, sandal, walking slipper) was calculated and the number of times the device had to be changed was also recorded.
Of the initially enrolled 70 patients, 62 patients completed the study, 6 were lost to follow‐up and 2 left against medical advice.
Statistical analysis
Data analysis was conducted using Statistical Package for Social Sciences (SPSS), version 13.0. Analysis of variance test was used to evaluate all continuous variables between the off‐loading groups and the effect of these continuous variables was also evaluated on healing of the ulcer using Mann–Whitney U‐test. Kaplan–Meier analysis (log‐rank test) was used to evaluate the healing time of each off‐loading device.
Results
Of the 70 patients, 24 were in modified foot wear group, 23 in modified plaster of Paris cast and 23 in Scotchcast boot group. There was no statistically significant difference observed between the groups with respect to age, duration of diabetes and severity of neuropathy (Table 1).
Table 1.
Baseline characteristics
| Modified foot wear (sandal) (n = 24) | Scotchcast boot (n = 23) | Modified plaster of Paris cast (n = 23) | Total (n = 70) | P‐value | |
|---|---|---|---|---|---|
| Age (years) | 49·79 ± 8·62 | 48·65 ± 9·03 | 52·34 ± 7·25 | 50·25 ± 8·36 | 0·312 |
| Male | 17 (70·8%) | 17 (73·9%) | 21 (91·3%) | 55 (78·6%) | 0·186 |
| Female | 7 (29·2%) | 6 (26·1%) | 2 (8·7%) | 15 (21·4%) | |
| Duration of diabetes (years) | 15·27 ± 7·04 | 13·40 ± 6·35 | 15·53 ± 7·29 | 14·71 ± 6·83 | 0·577 |
| HbA1c (%) | 10·14 ± 2·87 | 9·80 ± 1·92 | 10·53 ± 1·67 | 10·14 ± 2·22 | 0·697 |
| Vibration perception threshold (V) | 36·95 ± 11·17 | 39·13 ± 10·18 | 39·17 ± 10·36 | 38·41 ± 10·48 | 0·721 |
Data are presented as mean ± SD and n (%).
Most of the ulcers were on the big toe (33·3%) in modified foot wear group, 52·2% were on heel in Scotchcast boot group, and 30·4% of the ulcers were on first metatarsal head in modified plaster of Paris cast group (Table 2).
Table 2.
Wound characteristics
| Site of ulcer | Modified foot wear (sandal) (n = 24) | Scotchcast boot (n = 23) | Modified plaster of Paris cast (n = 23) | Total (n = 70) | P‐value |
|---|---|---|---|---|---|
| First metatarsal head | 6 (25%) | 3 (13%) | 7 (30·4%) | 16 (22·9%) | |
| Third metatarsal head | 2 (8·3%) | 1 (4·3%) | 3 (13%) | 6 (8·6%) | |
| Fourth metatarsal head | 0 (0%) | 0 (0%) | 2 (8·7%) | 2 (2·9%) | |
| Fifth metatarsal head | 2 (8·3%) | 3 (13%) | 2 (8·7%) | 7 (10%) | |
| Big toe | 8 (33·3%) | 4 (17·4%) | 6 (26·1%) | 18 (25·7%) | |
| Second toe | 3 (12·5%) | 0 (0%) | 0 (0%) | 3 (4·3%) | 0·002 |
| Third toe | 2 (8·3%) | 0 (0%) | 0 (0%) | 2 (2·9%) | |
| Fore foot | 0 (0%) | 0 (0%) | 1 (4·3%) | 1 (1·4%) | |
| Mid foot | 0 (0%) | 0 (0%) | 1 (4·3%) | 1 (1·4%) | |
| Heel | 1 (4·2%) | 12 (52·2%) | 1 (4·3%) | 14 (20%) | |
| Size of ulcer (cm2) | 0·97 ± 0·54 | 1·14 ± 0·55 | 1·23 ± 0·37 | 1·12 ± 0·5 | 0·209 |
Data are presented as mean ± SD and n (%).
There was almost equal proportion of patients healed within 12 weeks period treated with these three off‐loading techniques. No significant difference in median healing time was seen amongst patients healed within 12 weeks. Modified foot wear group was the most cost effective ($7) amongst these three off‐loading techniques as shown in Table 3.
Table 3.
Outcome of the patients
| Modified foot wear (sandal) (n = 23) | Scotchcast boot (n = 17) | Modified plaster of Paris cast (n = 20) | Total (n = 62) | P‐value | |
|---|---|---|---|---|---|
| Healing time (days)* | 34·0 | 46·0 | 45·0 | 42·50 | 0·767 |
| Healed (%) | 22 (95·7%) | 18 (94·7%) | 19 (95%) | 59 (95·2%) | 0·99 |
| Cost ($) | 7 | 35 | 20 | — | 0·000 |
Data are presented as mean ± SD and n (%).
Median healing time.
There was no significant difference observed in cumulative wound survival at 12 weeks in any of the three off‐loading techniques (Figure 1). With regard to the complications from the treatment, two patients (one each from modified plaster of Paris cast and Scotchcast boot) had broken the device and one patient in Scotchcast boot had mild laceration of local skin area.
Figure 1.
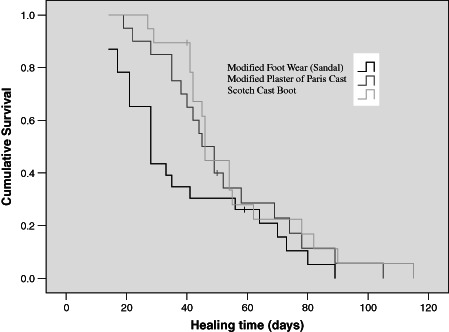
Cumulative wound survival at 12 weeks.
Discussion
Our study showed almost equal proportion of healing in modified foot wear group when compared with the other two groups. This could be because of the fact that the daily use of walking slipper and sandal is common in our culture than shoes, therefore patients are more compliant and less reluctant to use modified sandal. It was also observed in our study that wounds healed in almost same period of time in modified foot wear group than the other two modalities.
Median time to healing of Scotchcast boot in our study was also less than the described in a retrospective study using the Scotchcast boot for offloading diabetic foot wounds 13 but nearly equal to modified plaster of Paris cast although both are non removable devices. This could be because walking directly on Scotchcast boot without using supportive sandal increases edge effect as described by Armstrong and Athanasiou 14. Moreover, modified plaster of Paris cast has a plywood support which probably decreases direct pressure on the wound.
Although there was no significant difference observed in cumulative wound survival at 12 weeks in any of the off‐loading techniques but when compared in terms of cost, modified foot wear was the most cost‐effective treatment modality among the three groups. These locally made devices were also much cost effective than TCC and instant total contact cast (iTCC) 15.
Different methods to offload the foot include bed rest, wheel chair, felted foam, half shoes, crutch assisted gait, therapeutic shoes, TCC and removable cast walkers 16. However, TCC is considered the gold standard off‐loading modality 17.
This technique involves a moulded and minimally padded cast that maintains contact with the entire plantar aspect of the foot and the lower leg. Total contact casting has shown to be successful in healing 75–100% of diabetic neuropathic ulcerations 18. Although most of the physicians understand the effectiveness of this gold standard off‐loading technique in relieving plantar foot pressure, less than 2% of the centres are using this treatment modality 19. Healing time for TCC ranges from four to eight weeks 20, 21, 22, 23, 24, 25, 26, 27.
Both Armstrong and Katz also showed the effectiveness of TCC and removable cast walker (RCW) rendered irremovable (iTCC) 15. Because improper cast application can cause skin irritation and even in some cases ulceration, it requires a physician or cast technician with training or experience to safely apply a TCC.
Unfortunately, the technicians in our Institute, who can perform the application of TCC are not available. Furthermore, the extra cost of RCW and sometimes the casting material are the other limitations for using these modalities in our low‐resourced society. Hence, we are compelled to use the locally made off‐loading devices which are more cost effective and increase patient compliance. Similarly, there are some studies from India that show the effectiveness of locally made, low‐cost off‐loading techniques 28, 29.
Our study has some limitations such as: the sample size was small to detect possible differences which could have been present. Moreover, patients with ischaemic and infected foot ulcers were not included in the study.
Conclusion
In this patient cohort, no significant difference in healing time was observed in the three off‐loading techniques although modified foot wear (sandal) was found to be a more cost‐effective treatment modality. Furthermore, large‐scale studies are needed to show the effectiveness of off‐loading treatment modalities other than TCC and iTCC in low‐resourced countries.
Author contributions
ZM, AB, JA and SIZ performed the conception and design or acquisition of data or analysis and interpretation of data. ZM, AB, JA, MYA, AF and SIH drafted the article and revised it critically for important intellectual content. ZM, AB, JA, MYA, SIZ and AF approved the final version of the article to be published.
Acknowledgement
We acknowledge the support of Mr Bilal Tahir (Research Coordinator) and Ms Fariha Shaheen (Statistician), Research Department of Baqai Institute of Diabetology and Endocrinology in data entry and analysis.
References
- 1. Hill MN, Feldman H, Hilton SC, Holechek MJ, Ylitalo M, Benedict GW. Risk of foot complications in long term diabetic patient with and without ESRD: a preliminary study. ANNA J 1996;23:381–6. [PubMed] [Google Scholar]
- 2. LoGerfo FW. Vascular disease, matrix abnormalities and neuropathy: implications for limb salvage in diabetes mellitus. J Vase Surg 1987;5:793–6. [PubMed] [Google Scholar]
- 3. Payne CB. Biomechanics of the foot in diabetes mellitus: some theoretical consideration. J Am Podiatr Med Assoc 1998;88:285–9. [DOI] [PubMed] [Google Scholar]
- 4. Veves A, Sarmow MR, Giurini JM, Rosenblum BI, Lyons TE, Chrzan JS, Habershaw GM. Difference in join mobility in foot pressures between black & white diabetic patients. Diabet Med 1995;12:585–9. [DOI] [PubMed] [Google Scholar]
- 5. Stess RM, Jensen SR, Mirmiran R. The role of dynamic planter pressures in diabetic foot ulcers. Diabetes Care 1997;20:855–8. [DOI] [PubMed] [Google Scholar]
- 6. Helm PA, Walker SC, Pullium GF. Recurrence of neuropathic ulceration following healing in a total contact cast. Arch Phys Med Rehabil 1991;72:967–70. [PubMed] [Google Scholar]
- 7. Moss SE, Klein BEK. The prevalence and incidence of lower extremity amputation in a diabetic population. Arch Intern Med 1992;152:610–6. [PubMed] [Google Scholar]
- 8. Sims DS Jr, Cavanagh PR, Ulbrecht JS. Risk factors in diabetic foot. Recognition and management. Phys Ther 1988;68:1887–902. [DOI] [PubMed] [Google Scholar]
- 9. Lavery LA, Armstrong DG, Wunderkich RP, Tredwell JL, Boulton AJM. Predictive value of foot pressure assessment as part of population‐based diabetes disease management program. Diabetes Care 2003;26:1069–73. [DOI] [PubMed] [Google Scholar]
- 10. Boulton AJ. Pressure and the diabetic foot: clinical science and offloading techniques. Am J Surg 2004;187:17S–24S. [DOI] [PubMed] [Google Scholar]
- 11. Armstong DG, Nguyen HC, Lavery LA, van schie CH, Boulton AJM, Harkless LB. Offloading the diabetic foot wound: a randomized clinical trial. Diabetes Care 2001;24:1019–22. [DOI] [PubMed] [Google Scholar]
- 12. Anita R, Karl BL, Jana G, Megan S. Reduction of peak plantar pressure in people with diabetes‐related peripheral neuropathy: an evaluation of the DH Pressure Relief Shoe. J Foot Ankle Res 2012;5:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Knowles EA, Armstrong DG, Hayat SA, Khawaja KI, Malik RA, Boulton AJ. Offloading diabetic foot wounds using the scotch cast boot: a retrospective study. Ostomy Wound Manage 2002;48:50–3. [PubMed] [Google Scholar]
- 14. Armstrong DG, Athanasiou KA. The edge effect: how and why wound grow in size and depth. Clin Pod Med Surg 1998;15:105–8. [PubMed] [Google Scholar]
- 15. Katz IA, Harlan A, Miranda‐Palma B, Prieto‐Sanchez L, Armstrong DG, Bowker JH, Mizel MS, Boulton AJ. A randomized trial of two irremovable off‐loading devices in the management of plantar neuropathic diabetic foot ulcers. Diabetes Care 2005;28:555–9. [DOI] [PubMed] [Google Scholar]
- 16. Wu SC, Crews RT, Armstrong DG. The pivotal role of offloading in the management of neuropathic foot ulceration. Curr Diab Rep 2005;5:423–9. [DOI] [PubMed] [Google Scholar]
- 17. Lavery LA, Vela SA, Lavery DC, Quebedeaux TL. Reducing dynamic foot pressures in high‐risk diabetic subjects with foot ulcerations: a comparison of treatments. Diabetes Care 1996;19:818–21. [DOI] [PubMed] [Google Scholar]
- 18. Armstrong DG, Lavery LA, Wu S, Boulton AJ. Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds: a randomized controlled trial. Diabetes Care 2005;28:551–4. [DOI] [PubMed] [Google Scholar]
- 19. Stephanie CW, Jeffrey LJ, Anna KW, Daniel ER, David GA. Use of pressure offloading devices in diabetic foot ulcers. Diabetes Care 2008;31:2118–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Helm PA, Walker SC, Pulliam G. Total contact casting in diabetic patients with neuropathic foot ulcerations. Arch Phys Med Rehabil 1984;65:691–3. [PubMed] [Google Scholar]
- 21. Sinacore DR, Mueller MJ, Diamond JE. Diabetic plantar ulcers treated by total contact casting. Phys Ther 1987;67:1543–7. [DOI] [PubMed] [Google Scholar]
- 22. Myerson M, Papa J, Eaton K, Wilson K. The total contact cast for management of neuropathic plantar ulceration of the foot. J Bone Joint Surg 1992;74:261–9. [PubMed] [Google Scholar]
- 23. Walker SC, Helm PA, Pulliam G. Chronic diabetic neuropathic foot ulcerations and total contact casting: healing effectiveness and outcome probability (Abstract). Arch Phys Med Rehabil 1985;66:574. [Google Scholar]
- 24. Walker SC, Helm PA, Pulliam G. Total contact casting and chronic diabetic neuropathic foot ulcerations: healing rates by wound location. Arch Phys Med Rehabil 1987;68:217–21. [PubMed] [Google Scholar]
- 25. Armstrong DG, Lavery LA, Bushman TR. Peak foot pressures influence the healing time of diabetic foot ulcers treated with total contact casts. J Rehabil Res Dev 1998;35:1–5. [PubMed] [Google Scholar]
- 26. Lavery LA, Armstrong DG, Walker SC. Healing rates of diabetic foot ulcers associated with midfoot fracture due to Charcot's arthropathy. Diabet Med 1997;14:46–9. [DOI] [PubMed] [Google Scholar]
- 27. Lavery LA, Vela SA, Lavery DC, Quebedeaux TL. Total contact casts: pressure reduction at ulcer sites and the effect on the contralateral foot. Arch Phys Med Rehabil 1997;78:1268–71. [DOI] [PubMed] [Google Scholar]
- 28. Kshitij S, Lakshmi KS, Uma S, Smita S. Innovative approaches for improving diabetic foot care in India. Wounds International 2010;1; 2. http://www.woundsinternational.com/practice‐development/innovative‐approaches‐for‐improving‐diabetic‐foot‐care‐in‐india [accessed on 14 December 2012] [Google Scholar]
- 29. Agrawal VP, Sreeramulu PN. Most easy on the pocket offloading device costing <1$ for rural diabetic foot ulcers. Surg Curr Res 2012;2:124. [Google Scholar]


