Abstract
The objective of this study was to evaluate the efficacy of three off‐loading techniques to heal diabetic foot wounds: total contact casts (TCCs), healing sandals (HSs) and a removable boot with a shear‐reducing foot bed (SRB). This was a 12‐week, single‐blinded randomised clinical trial with three parallel treatment groups of adults with diabetes and a foot ulcer (n = 73). Ulcer healing was defined as full reepithelialisation with no drainage. Diabetic patients with grade UT1A or UT2A forefoot ulcers on the sole of the foot were enrolled. Patients with malignancy, immune‐compromising diseases, severe peripheral vascular disease (ankle‐brachial index < 0·60 or transcutaneous oxygen < 25 mm/Hg), alcohol or substance abuse within 6 months, untreated osteomyelitis or Charcot arthropathy with residual deformity that would not fit the HS or boot were excluded. In the intent‐to‐treat analysis, significantly higher proportion of patients were healed in the TCC group (69·6%) compared to those treated with the SRB (22·2%, P < 0·05). There was no difference in the rate of healed ulcers in the HS (44·5%) and TCC groups. Ulcers in the TCC group healed faster than those in the HS group (5·4 ± 2·9 versus 8·9 ± 3·5 weeks, P < 0·02). However, there was no difference in the time to healing in the TCC and SRB groups (6·7 ± 4·3 weeks, P = 0·28). Patients who used HS were significantly more active (4022 ± 4652 steps per day, P < 0·05) than those treated with TCCs (1447 ± 1310) or SRB (1404 ± 1234). It is concluded that patients treated with TCCs had the highest proportion of healed wounds and fastest healing time. The novel shear‐reducing walker had the lowest healing and highest rate of attrition during the study.
Keywords: Amputation, Cast, Diabetes, Infection, Off‐load, Ulceration
Introduction
Diabetes is the single most common contributing cause of lower extremity amputations in the USA 1, 2, 3. One of the most common components in the causal pathway to limb amputation in persons with diabetes is a neuropathic foot ulcer 4. A pivotal part of any treatment protocol to heal diabetic foot ulcers (DFUs) involves a strategy to ‘off‐load’ the foot, or more simply stated, a plan to reduce pressure and shear forces at the site of ulceration. Total contact casts (TCCs) are considered the theoretical gold standard to reduce plantar foot pressures and heal neuropathic foot ulcers; however, in the USA, only a fraction of the population have this therapy available to them 5. Clinical studies have demonstrated that total contact casting is effective in healing 72–100% of DFUs 5, 6, 7, 8, 9, 10, 11, 12, 13, 14.
The TCC technique has some inherent disadvantages that have limited widespread implementation. The application of TCC requires a skilled technician. Many clinical settings do not have a physician or cast technician available to properly apply a TCC. TCCs are contraindicated for wounds with soft tissue infections, osteomyelitis and vascular impairment. TCCs also do not allow patients to assess the foot or wound on a daily basis. Further adjunct therapies such as topical growth factors, topical antibiotics or debriding agents cannot be used on a regular basis along with casts. Because of these disadvantages, many physicians use off‐the‐shelf devices, such as removable cast walkers, healing sandals (HS) and therapeutic shoes and insoles 5.
The goal of this pilot study was to evaluate a shear‐reducing foot bed (SRB) to improve stress modulation in a removable cast boot. The amount of pressure reduction in various removable cast walkers on the sole of the foot is equivalent to that measured with TCCs 15. Several studies have indicated that removable boots can be as effective as a cast to heal DFUs. This study used a foot bed within the removable cast boot to reduce both pressure and shear forces 16, 17. None of the current commercially available products address the mitigation of shear stress. This study will evaluate the effectiveness of a novel, removable, cast walker specifically designed to reduce pressure and shear forces on the bottom of the foot to heal DFUs. Figures 1 and 2 show the foot bed design. When a shear force is applied to the shear‐reducing insole, the upper portion moves relative to the lower portion.
Figure 1.
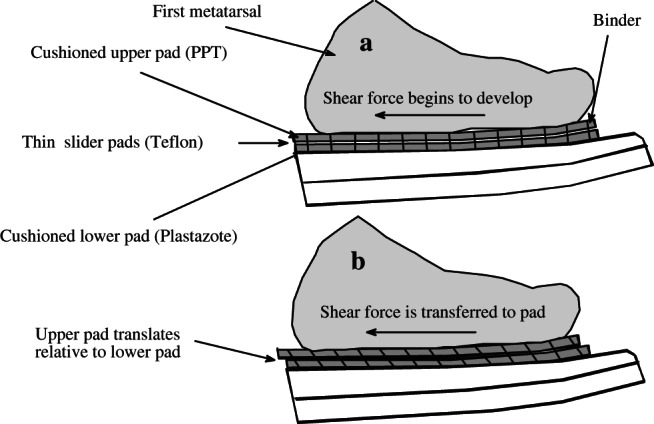
Reduction in shear is achieved as the upper portion of the pad displaces relative to the lower portion. The binders stretch and eventually stop this relative motion. Pressure reduction is maintained by using standard insole cushioning materials.
Figure 2.
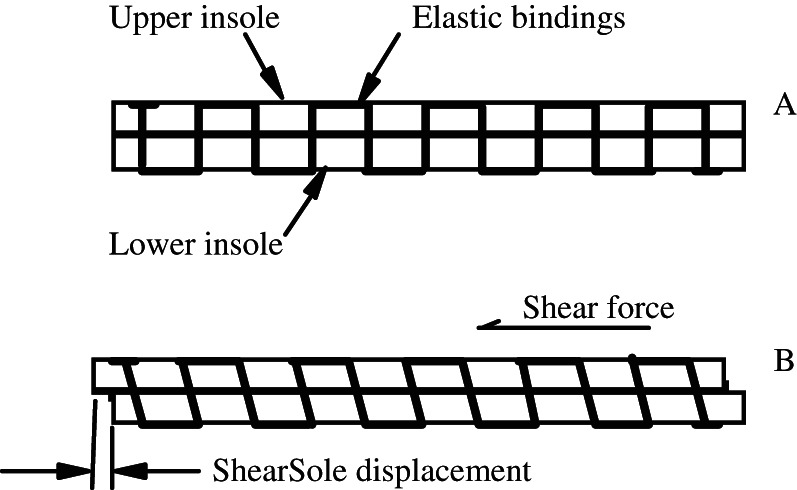
The insole is shown with no applied shear force (A) and with an applied shear force (B). As a result of shear, the upper portion of the insole displaces relative to the lower portion. The elastic bindings stretch and eventually stop the relative motion within the foot bed.
Methods
This study was a 12‐week, single‐blinded randomised clinical trial with three parallel treatment groups of adults with diabetes mellitus and a foot ulcer (73 patients). Patients were randomly assigned to one of the three treatment groups using a computer‐generated list: (i) shear‐reducing walker, (ii) HS with Plastazote foot bed or (iii) TCC. The primary end point was the proportion of healed ulcers during the 12‐week study. Ulcer healing was defined as full reepithelialisation with no drainage.
Inclusion and exclusion criteria
Diabetic patients with grade UT1A or UT2A forefoot ulcers (the University of Texas Ulcer Classification System) 18 on the sole of the foot were enrolled. If more than one ulcer was present, the largest ulcer meeting all the eligibility criteria was selected as the index ulcer. Other ulcers were treated in the same manner as the study ulcer. Patients were excluded based on the following criteria: inability to care for their ulcer during the study period (e.g. because of vacation, hospitalisation and disability), widespread malignancy, systematically immune‐compromising disease, severe peripheral vascular disease (ABI < 0·60 or transcutaneous oxygen < 25 mm/Hg), alcohol or substance abuse within 6 months, untreated osteomyelitis or Charcot arthropathy with residual deformity that was too severe to allow proper fit of the removable walking boot, and patients with postural stability that was not adequate to safely ambulate in a TCC or walking boot. The Sroufe Deluxe Chevron Shoe with an 8‐mm Plastazote insole was used (Sroufe, Austin, TX). This device is a high top shoe with Velcro closure over the ankle and forefoot to eliminate pistoning. A shear‐reducing cast walker was designed to reduce pressure and shear forces using GlideSoft® technology (Diabetica Solutions, San Antonio, TX). Wound debridement was performed ad labium. Wounds were dressed with hydrogel and covered with a single layer of fine mesh gauze. Pressure sensation was evaluated at ten sites on each foot using 10 g monofilaments including the plantar surface of the first, third and fifth toes, first, third and fifth metatarsal heads, the medial and lateral midfoot, central heel and the first intermetatarsal space on the dorsum of the foot. Data are reported as the average number of sites missed during the examination.
Activity log/pedometer
The activity of the patient was recorded using a pedometer worn strapped to the patient's waist 19. The pedometer recorded the number of steps per day. This number was recorded in an activity log book before the patient retired for the night. Patients were also asked to record their impression of the percent time they have worn their off‐loading device during each day. In order to enhance compliance, the research nurse contacted study participants between clinic visits to discuss their treatment, progress, compliance and recording of pedometer measurements.
Study visits
Patients were seen every 7–10 days for follow‐up. Wounds were evaluated at each clinical visit to ensure the absence of infection and to measure the size and depth of the wound. An acetate tracing of the wound was used to record the size of the wound at each visit. The top portion of a clean transparent acetate package was placed over the ulcer. The ulcer outline was carefully traced with an extra fine‐tipped permanent black marker. The inside of the ink line was used to define the margins of the ulcer. The wound areas are calculated by planimetry.
Patient satisfaction was assessed with a 10 cm visual analog scale. Patients were asked the following questions: (i) Are you satisfied with your foot care? (ii) Has your activity level been significantly altered? 7 (iii) Are you able to perform your normal daily activities? (iv) Is your off‐loading device comfortable? (v) Has your sleep activity changed significantly? (vi) Are you satisfied with your off‐loading device?
Statistical analysis
Data pertaining to demographic characteristics are summarised with descriptive statistics in Table 1. A χ 2 test was used to compare the proportion of subjects who had complete reepithelialisation. For continuous data we used multivariate analysis of variance with post hoc pairwise comparisons using the least squares difference test. For all analyses, we used an alpha of 5%. We evaluated the proportion of wound that healed with an ‘intent‐to‐treat’ (ITT) analysis using the last observation carried forward technique and a ‘per‐protocol’ analysis that only included subjects who completed the study. In the ITT analysis, patients who voluntarily withdrew from the studies and those who withdrew because of adverse events were counted as ‘not healed’. In the ‘per‐protocol analysis’ only subjects who completed the study were included in the analysis.
Table 1.
Demographic characteristics
| Healing sandals, n = 23 | Total contact cast, n = 23 | Shear walker, n = 27 | |
|---|---|---|---|
| % Male | 52·20 | 60·90 | 55·60 |
| Race | |||
| Hispanic | 14 (61%) | 12 (52%) | 17 (63%) |
| Non‐Hispanic white | 7 (30%) | 10 (43%) | 8 (30%) |
| African American | 1 (4%) | 1 (4%) | 2 (7%) |
| Other | 1 (4%) | 0 (0) | 0 (0) |
| Type II diabetes | 22 (95·7%) | 20 (87·0%) | 25 (92·6%) |
| Diabetes medications | |||
| Oral | 11 (47·8%) | 7 (30·4%) | 10 (37·0%) |
| Insulin | 7 (30·4%) | 5 (21·7%) | 8 (29·6%) |
| Combination | 4 (17·4%) | 9 (39·1%) | 8 (29·65) |
| None | 1 (4·3%) | 2 (8·7%) | 1 (4·3%) |
| Ulcer history | 13 (52·1%) | 15 (65·2%) | 23 (85·2%) |
| Amputation history | 15 (65·2%) | 10 (43·5%) | 4 (14·8%) |
| Vascular assessment | |||
| Right ABI | 1·11 ± 0·32 | 1·11 ± 0·19 | 1·13 ± 0·21 |
| Left ABI | 1·15 ± 0·27 | 1·16 ± 0·18 | 1·12 ± 0·23 |
| TCpO2 (mm/Hg) | 40·87 ± 13·83 | 37·39 ± 7·78 | 38·63 ± 9·24 |
| Neuropathy assessment | |||
| Right monofilament 10 g sites missed | 7·8 ± 2·3 | 7·9 ± 2·4 | 5·3 ± 4·7 |
| Left monofilament 10 g sites missed | 7·8 ±2·5 | 7·6 ± 2·5 | 4·7 ± 4·3 |
| Right vibration perception threshold | 56·2 ± 20·6 | 56·9 ± 21·3 | 40·6 ± 8·6 |
| Left vibration perception threshold | 50·6 ± 21·8 | 48·1 ± 18·4 | 39·0 ± 8·0 |
ABI, ankle‐brachial index; TCpO2, transcutaneous oxygen.
Results
There was no difference in race, sex, prevalence of type 2 diabetes, diabetes medications, neuropathy or vascular parameters among the three treatment groups (Table 1). The results of this study demonstrate that a significantly higher proportion of patients had healed in the TCC group compared to those treated with a SRB with a removable walker in both the ITT and per‐protocol analyses (Table 2). There was not a significant difference in the proportion of wounds that healed in the TCC and HS treatment groups in the ITT analysis; however, there was a significant difference in healing in the ‘per‐protocol analysis’ when TCC patients were compared to HS patients (P = 0·015). In addition, patients in the TCC group healed faster than those in the HS group (5·4 ± 2·9 versus 8·9 ± 3·5 weeks, P < 0·001). However, there was no difference in the time to healing in the TCC and shear‐reducing walker groups (6·7 ± 4·3 weeks, P = 0·22).
Table 2.
Study results for the three treatment groups
| Healing sandals, n = 23 | Total contact cast, n = 23 | Shear walker, n = 27 | |
|---|---|---|---|
| Wound size | 2·0 ± 3·5 | 2·2 ± 3·5 | 2·3 ± 4·1 |
| Time to heal (weeks) | 8·9 ± 3·5 | 5·4 ± 2·9 | 6·7 ± 4·3 |
| Activity | |||
| Average daily steps | 4022 ± 4652 | 1447 ± 1310 | 1404 ± 1234 |
| Range | 551–7664 | 25–4328 | 39–4112 |
| Wound healing | |||
| Healed (intent‐to‐treat) | 10 (43·5%) | 16 (69·6%) | 6 (22·2%) |
| Healed (per protocol) | 10 (50·0%) | 16 (88·9%) | 6 (40·0%) |
| Dropped | |||
| Infection | 3 (13·0%) | 1 (4·3%) | 4 (14·8%) |
| Voluntary withdrawal | 0 | 4 (17·4%) | 4 (14·8%) |
| Device‐related wounds | 0 | 0 | 1 (3·7%) |
| Non‐compliant with device | 0 | 0 | 3 (11·1%) |
| Completed study | 20 (87·0%) | 18 (78·3%) | 15 (55·6%) |
There was no difference among the three treatment groups in patient satisfaction with foot care, activity level, activities of daily living, comfort, sleep, satisfaction with the off‐loading device and willingness to use the same type of device again (Table 3). However, the average activity level was significantly higher in the patients treated with HS (4022 ± 4652 steps per day) compared to those treated with the TCC (1447 ± 1310, P = 0·014) and the shear‐reducing walker (1404 ± 1234, P = 0·007). The proportion of patients who completed the study was highest in the HS group (87%) and lowest in the shear‐reducing walker group (55·6%, P < 0·05, Table 2). There was no significant difference in study‐related adverse events among the treatment groups (P > 0·05). Infection and iatrogenic wounds were reported in 13·4% (n = 3) of patients in the HS group, 18·5% (n = 5) of shear‐reducing walker patients and 4·3% (n = 1) of TCC patients.
Table 3.
Subject satisfaction survey
| Range 10–0 (10 = VERY… 0 = NOT…) | Healing sandals, n = 23 | Total contact, n = 23 | Shear walker, n = 27 |
|---|---|---|---|
| Satisfied with foot care | 9·09 ± 1·56 | 9·02 ± 1·89 | 8·77 ± 2·06 |
| Activity level significantly altered | 7·87 ± 2·78 | 7·49 ± 2·97 | 7·02 ± 3·10 |
| Able to perform normal daily activities | 5·20 ± 3·51 | 5·66 ± 0·349 | 5·78 ± 3·30 |
| Comfort of off‐loading device | 7·71 ± 2·38 | 7·29 ± 2·68 | 7·06 ± 2·73 |
| Sleep activity changed significantly | 5·68 ± 2·96 | 5·90 ± 2·96 | 5·39 ± 3·05 |
| Satisfaction with off‐loading device | 8·47 ± 2·05 | 8·26 ± 2·29 | 7·88 ± 2·42 |
| Likely to wear this device again | 7·84 ± 2·77 | 6·97 ± 3·47 | 6·79 ± 3·41 |
Discussion
Shear is probably a strong component in many patients who develop wounds in the presence of relatively moderate vertical forces. Empirically, it appears that any force, including shear, imparted on neuropathic skin in a repetitive fashion should have a detrimental effect on the viability of the integument. Zhang et al. 20 concluded that the effects of shear are additive to the pressures causing damage to the deeper soft tissues as well as causing superficial damage. They noted that the internal compression stress in underlying soft tissues is a resultant of both pressure and shear components, which have been shown to have equal effects in the reduction of blood flow in tissues 20. Hosein and Lord suggested that the application of a shear force increases the stress ahead of the direction of the force, which places the soft tissue within this region already compressed by pressure at greatest risk 21. Empirically, we expected the foot bed design to provide a clinical advantage in the healing process. The shear modulation technology used in this study exhibited 57% less peak shear force than the standard foot bed constructs used in laboratory studies 16, 17. However, in practice, the approach was not successful.
This preliminary study was conducted to evaluate the proof‐of‐concept for a SRB with a walking boot to heal DFUs. The shear‐reducing boot was found to be less effective than total contact casting. In previous studies, the proportion of wounds that healed were much higher in removable boots (52–74%) 14, 22 and non‐removable boots (80–83%) 22, 23 compared with the very low rate of wound healing reported in this study in the shear‐reducing walker group. However, several studies have reported similar results with removable boots and TCC 23, 24, 25. In several studies that used TCC, 70–100% of study subjects achieved healing. 14, 22, 24, 25. This is similar to the results that were observed in our per‐protocol analysis (88%). However, in our ‘ITT evaluation’ only 69·7% of subjects were found to be healed.
Withdrawal from the study because of adverse events or voluntary termination of study participation was a pivotal factor in the proportion of healed patients in the ITT analysis. A significant difference was identified in subjects who did not complete the study among the treatment groups. In many DFU clinical trials the voluntary drop out rate is similar between the treatment groups 23, 26, 27. For instance, Veves et al. reported a similar rate of voluntary withdrawal (19·6% and 22·3%) but a lower rate of infection (28·6% and 47·9%) in patients who received bioengineered tissue and controls, respectively. Off‐loading randomised controlled trials (RCTs) usually report very low drop out rates (15–19%) 23.
In our study, the HS group had the lowest attrition (13%). In the HS group, three patients were discontinued because of infection and there were no voluntary drop outs. In contrast, in the TCC group, four patients did not complete the study (21·7%). One was due to infection and four voluntarily dropped out. The highest rate of study withdrawals was in the group with the poorest healing performance, the shear‐reducing walker group. Poor patient acceptance appears to be an important factor in drop outs. In the shear‐reducing walker group 43·3% of the patients did not complete the study; 14·3% voluntarily withdrew and 11·1% were removed from the study for poor compliance. In addition, four subjects were unable to complete the study because of infection and one developed a second wound. In Armstrong's off‐loading RCT, there was a substantial difference in study attrition between the patients treated with an ‘instant TCC’ and a removable walking boot. Not unlike our study, 44·4% of patients in the removable boot study group dropped out compared with 17·4% in the instant TCC group 22.
Success may have more to do with patient comfort, acceptance and compliance than the intrinsic effectiveness of the off‐loading device. However, data from a patient questionnaire showed that patient satisfaction was similar in all the three treatment groups. Despite significantly lower activity measured in the TCC and shear‐reducing walker groups, all the three study groups reported similar satisfaction with ‘activity limitations’ and ‘activities of daily living’. Similarly, the response to ‘would you use the off‐loading device again’ was similar among the treatment groups despite a very high rate of voluntary withdrawals and a very high drop‐out rate in shear‐reducing walker group patients.
There are important limitations to this study. As in many of the existing off‐loading studies 14, 22, 23, 24, 25 the sample size is small. This may have limited our ability to detect significant differences in outcomes or risk factors. Off‐the‐shelf products such as the HS and cast boot used in this study do not fit all patients correctly. For instance, patients with very short legs, wide feet or residual Charcot deformity often cannot use ready‐made devices. These patients are more amenable to casting because the cast can be moulded and customised to the structure of the foot and lower leg. In addition, the selection of patients was limited to subjects who were well perfused. This eliminates higher risk patients with ulcers that are less likely to heal 28.
Off‐loading is a central element in any treatment strategy to treat DFUs. The selection of an off‐loading device includes efficacy, safety, availability, cost and patient acceptance and compliance. If patients will not use a device then the risk of non‐healing is very high. The results of this study confirm the efficacy of TCC to heal DFUs. Conceptually, the shear‐reducing walker designed for this study should have provided an advantage. However, patient voluntary withdrawal and removal because of poor compliance changed the efficacy of this approach.
Acknowledgement
This study was funded by a grant from the National Institute of Health, National Institute of Diabetes and Digestive and Kidney Diseases 2R44 DK 56571‐02.
References
- 1. Lavery LA, van Houtum WH, Ashry HR, Armstrong DG, Pugh JA. Diabetes‐related lower‐extremity amputations disproportionately affect Blacks and Mexican Americans. South Med J 1999;92:593–9. [DOI] [PubMed] [Google Scholar]
- 2. Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes‐related amputations in minorities. Diabetes Care 1996;19:48–52. [DOI] [PubMed] [Google Scholar]
- 3. Van Houtum WH, Lavery LA. Outcomes associated with diabetes‐related amputations in The Netherlands and in the state of California, USA. J Intern Med 1996;240:227–31. [DOI] [PubMed] [Google Scholar]
- 4. Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care 1990;13:513–21. [DOI] [PubMed] [Google Scholar]
- 5. Wu SC, Jensen JL, Weber AK, Robinson DE, Armstrong DG. Use of pressure offloading devices in diabetic foot ulcers: do we practice what we preach? Diabetes Care 2008;31:2118–9. DOI: 10.2337/dc08-0771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Walker SC, Helm PA, Pullium G. Total contact casting and chronic diabetic neuropathic foot ulcerations: healing rates by wound location. Arch Phys Med Rehabil 1987;68:217–21. [PubMed] [Google Scholar]
- 7. Sinacore DR, Mueller MJ, Diamond JE, Blair VP, Drury D, Rose SJ. Diabetic plantar ulcers treated by total contact casting. A clinical report. Phys Ther 1987;67:1543–9. [DOI] [PubMed] [Google Scholar]
- 8. Mueller MJ, Diamond JE, Sinacore DR, Delitto A, Blair VP, Drury DA, Rose SJ. Total contact casting in treatment of diabetic plantar ulcers. Controlled clinical trial. Diabetes Care 1989;12:384–8. [DOI] [PubMed] [Google Scholar]
- 9. Helm PA, Walker SC, Pullium G. Total contact casting in diabetic patients with neuropathic foot ulcerations. Arch Phys Med Rehabil 1984;65:691–3. [PubMed] [Google Scholar]
- 10. Helm PA, Walker SC, Pullium GF. Recurrence of neuropathic ulceration following healing in a total contact cast. Arch Phys Med Rehabil 1991;72:967–70. [PubMed] [Google Scholar]
- 11. Myerson M, Papa J, Eaton K, Wilson K. The total‐contact cast for management of neuropathic plantar ulceration of the foot. J Bone Joint Surg Am 1992;74:261–9. [PubMed] [Google Scholar]
- 12. Coleman WC, Brand PW, Birke JA. The total contact cast. A therapy for plantar ulceration on insensitive feet. J Am Podiatry Assoc 1984;74:548–52. [DOI] [PubMed] [Google Scholar]
- 13. Lavery LA, Armstrong DG, Walker SC. Healing rates of diabetic foot ulcers associated with midfoot fracture due to Charcot's arthropathy. Diabet Med 1997;14:46–9. [DOI] [PubMed] [Google Scholar]
- 14. Armstrong DG, Nguyen HC, Lavery LA, van Schie CH, Boulton AJ, Harkless LB. Off‐loading the diabetic foot wound: a randomized clinical trial. Diabetes Care 2001;24:1019–22. [DOI] [PubMed] [Google Scholar]
- 15. Lavery LA, Vela SA, Lavery DC, Quebedeaux TL. Reducing dynamic foot pressures in high‐risk diabetic subjects with foot ulcerations. A comparison of treatments. Diabetes Care 1996;19:818–21. [DOI] [PubMed] [Google Scholar]
- 16. Lavery LA, LaFontaine J, Higgins KR, Lanctot DR, Constantinides G. Shear‐reducing insoles to prevent foot ulceration in high‐risk diabetic patients. Adv Skin Wound Care 2012;25:519–24 quiz 525–6. [DOI] [PubMed] [Google Scholar]
- 17. Lavery LA, Lanctot DR, Constantinides G, Zamorano RG, Athanasiou KA, Agrawal CM. Wear and biomechanical characteristics of a novel shear‐reducing insole with implications for high‐risk persons with diabetes. Diabetes Technol Ther 2005;7:638–46. [DOI] [PubMed] [Google Scholar]
- 18. Armstrong DG, Lavery LA, Harkless LB. Validation of a diabetic wound classification system. The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998;21:855–9. [DOI] [PubMed] [Google Scholar]
- 19. Hendelman D, Miller K, Baggett C, Debold E, Freedson P. Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Med Sci Sports Exerc 2000;32(9 Suppl):S442–9. [DOI] [PubMed] [Google Scholar]
- 20. Zhang M, Turner‐Smith AR, Roberts VC. The reaction of skin and soft tissue to shear forces applied externally to the skin surface. J Eng Med 1994;208:217–22. [Google Scholar]
- 21. Hosein R, Lord M. A study of in‐shoe plantar shear in normals. Clin Biomech (Bristol, Avon) 2000;15:46–53. [DOI] [PubMed] [Google Scholar]
- 22. Armstrong DG, Lavery LA, Wu S, Boulton AJ. Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds: a randomized controlled trial. Diabetes Care 2005;28:551–4. [DOI] [PubMed] [Google Scholar]
- 23. Katz IA, Harlan A, Miranda‐Palma B, Prieto‐Sanchez L, Armstrong DG, Bowker JH, Mizel MS, Boulton AJ. A randomized trial of two irremovable off‐loading devices in the management of plantar neuropathic diabetic foot ulcers. Diabetes Care 2005;28:555–9. [DOI] [PubMed] [Google Scholar]
- 24. Faglia E, Caravaggi C, Clerici G, Sganzaroli A, Curci V, Vailati W, Simonetti D, Sommalvico F. Effectiveness of removable walker cast versus nonremovable fiberglass off‐bearing cast in the healing of diabetic plantar foot ulcer: a randomized controlled trial. Diabetes Care 2010;33:1419–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Piaggesi A, Macchiarini S, Rizzo L, Palumbo F, Tedeschi A, Nobili LA, Leporati E, Scire V, Teobaldi I, Del Prato S. An off‐the‐shelf instant contact casting device for the management of diabetic foot ulcers: a randomized prospective trial versus traditional fiberglass cast. Diabetes Care 2007;30:586–90. [DOI] [PubMed] [Google Scholar]
- 26. Marston WA, Hanft J, Norwood P, Pollak R. The efficacy and safety of Dermagraft in improving the healing of chronic diabetic foot ulcers: results of a prospective randomized trial. Diabetes Care 2003;26:1701–5. [DOI] [PubMed] [Google Scholar]
- 27. Veves A, Falanga V, Armstrong DG, Sabolinski ML. Graftskin, a human skin equivalent, is effective in the management of noninfected neuropathic diabetic foot ulcers: a prospective randomized multicenter clinical trial. Diabetes Care 2001;24:290–5. [DOI] [PubMed] [Google Scholar]
- 28. Nabuurs‐Franssen MH, Sleegers R, Huijberts MS, Wijnen W, Sanders AP, Walenkamp G, Schaper NC. Total contact casting of the diabetic foot in daily practice: a prospective follow‐up study. Diabetes Care 2005;28:243–7. [DOI] [PubMed] [Google Scholar]


