Abstract
In recent years, adhesive wound dressings have been increasingly applied postoperatively because of their ease of use as they can be kept in place without having to cut and apply surgical tapes and they can cover a wound securely. However, if a wound dressing strongly adheres to the wound, a large amount of stratum corneum is removed from the newly formed epithelium or healthy periwound skin. Various types of adhesives are used on adhesive wound dressings and the extent of skin damage depends on how much an adhesive sticks to the wound or skin surface. We quantitatively determined and compared the amount of stratum corneum removed by eight different wound dressings including polyurethane foam using acrylic adhesive, silicone‐based adhesive dressing, composite hydrocolloid and self‐adhesive polyurethane foam in healthy volunteers. The results showed that wound dressings with silicone adhesive and self‐adhesive polyurethane foam removed less stratum corneum, whereas composite hydrocolloid and polyurethane foam using acrylic adhesive removed more stratum corneum.
Keywords: Adhesive wound dressings; Dressing removal; Periwound skin; Stratum corneum; Wound dressing
Introduction
Wound dressings have achieved remarkable progress in terms of availability and application. Recently, various types of wound dressings have been made commercially available and applied widely. Wound dressings should have one or more of the following functions or properties: (i) prevent dryness on the wound surface and maintain a moist environment; (ii) absorb excess exudate without leakage to the surrounding healthy skin; (iii) prevent bacterial contamination and subsequent wound infection; (iv) easy to use by being able to stay in place and adherent to the periwound surface and (v) easy to remove without causing pain and with less amount of stratum corneum removed from the normal skin and newly formed epithelium.
Previously, the choice of a wound dressing was based on the impact of the first three functions or characteristics mentioned above on the wound surface. In recent years, much importance has been given to easy‐to‐use products such as self‐adherent dressings and those that do not cause pain when choosing an appropriate wound dressing. In particular, pain and skin damage upon wound dressing removal have a significant impact not only on a patient's quality of life, but also on health care professionals who need to be fully aware of the patient's condition and to make careful assessment of the patient's pain. The present commercially available wound dressings rarely adhere to the wound surface or newly formed epithelium, and they cause minimal injury to the skin because they absorb excess exudate on the wound surface. At the time of wound dressing removal, injury to the surrounding healthy skin is usually caused, which is reported to increase wound surface area and pain, and consequently delays wound healing (1). In recent years, wound dressings using silicon‐based adhesive, which causes less injury to the skin as a wound contact layer, have been extensively used in order to solve this problem. Their beneficial clinical effects are highly appreciated.
On the other hand, studies objectively comparing the extent of tissue damage in terms of the amount of stratum corneum removed from healthy skin upon the removal of different wound dressings remain scarce (2). In clinical practice, it is ideal to select a wound dressing that is suitable for each wound condition by quantitatively analysing the amount of skin damage upon removal among a large number of wound dressings.
In this study, we quantitatively determined and compared the amount of stratum corneum of the skin removed by several different self‐adherent wound dressings in healthy volunteers.
Materials and methods
Ten healthy adult volunteers were enrolled in the study (five men and five women; age range, 24–53 years). Four different adhesive dressings (one forearm and two each) were applied to the inner hairless area of the forearm of each subject. Each piece of adhesive dressing measured 7·5 × 7·5 cm. Treatments were applied to the same area on the skin of the subjects 24 hours before the start of the study. The eight wound dressings used were as follows: (i) polyurethane foam using acrylic adhesive: Hydrosite AD plus (hereinafter referred to as ‘A’); (ii) polyurethane foam with silicone adhesive: Hydrosite AD gentle (G); (iii) Mepilex Border (B); (iv) dressing coated on one surface with a layer of soft silicone: Mepilex Transfer (T); (v) self‐adhesive polyurethane foam: Hydrosite ultrathin (U); (vi) composite hydrocolloid film: Replicare (R); (vii) DuoACTIVE ET (E) and (viii) DuoACTIVE CGF (C). Four pieces of each dressing were applied (Figure 1). The high and low temperatures on the evaluation day were 9·6 ° C and 2·5°C, respectively, with a humidity of 30%. Each dressing was removed from the forearm at a rate of approximately 1 cm/second by the same operator. During wound dressing removal, the room temperature and humidity were 14°C and 48%, respectively.
Figure 1.
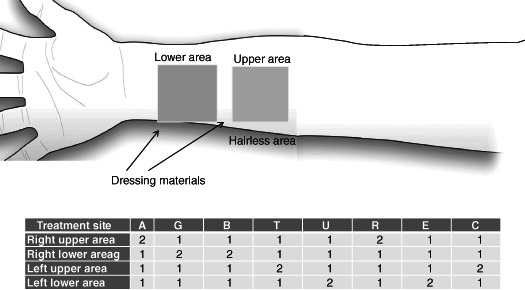
Application of adhessive wound dressing.
Quantification of the amount of stratum corneum removed
A transparent adhesive tape (Nichiban CT‐15M, Tokyo, Japan; the adhesive formulations are natural rubber and natural resin) was applied to the adherent surface of each wound dressing following its removal in order to print the stratum corneum to the adhesive tape. Thereafter, the printed stratum corneum on the adhesive tape was stained with Gentian violet (1% solution in water) for 45 seconds and washed off, and the stratum corneum printed on the adhesive tape was mounted on a glass slide. The tissue samples attached on a glass slide were examined under a videoscope at ×300 magnification (Bscan Pro, NTSC colour system; Toku Co. Ltd., Tokyo, Japan) and were recorded on a videotape. Among the samples videotaped, five visual fields per wound dressing were used as a still image (total: 25 visual fields). Each still image was dichotomised at a threshold value of 120 of 256 gradation levels by a personal computer, and the amount of stratum corneum removed was calculated on the basis of the proportion of black pixels.
For statistical analyses, multiple comparisons were performed using the Tukey method. A P‐value of < 0·05 was considered to indicate a statistically significant difference.
Results
Figure 2 shows the stained images of the stratum corneum printed on the adhesive tape from each wound dressing and the dichotomised images. Both the stained images and the dichotomised images are highly consistent with each other. In this regard, assessment of the areas of the stratum corneum removed from healthy skin was considered to be properly conducted.
Figure 2.
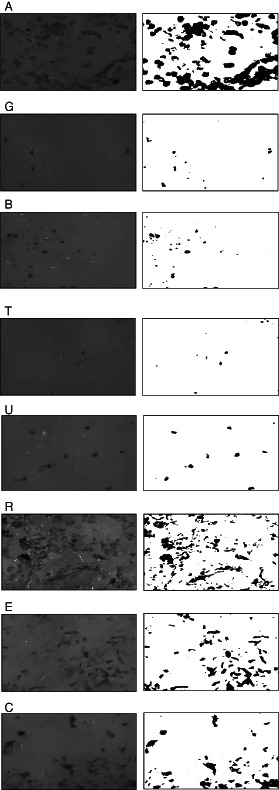
Stained images of the stratum corneum printed on the adhesive tape from each wound dressing and the dichotomised images (wound dressings: A, polyurethane foam using acrylic adhesive: Hydrosite AD plus; G, polyurethane foam using silicone adhesive: Hydrosite AD gentle; B, Mepilex Border; T, dressing coated on one surface with a layer of soft silicone: Mepilex Transfer; U, self‐adhesive polyurethane foam: Hydrosite ultrathin; R, composite hydrocolloid film: Replicare; E, DuoACTIVE ET; C, DuoACTIVE CGF).
Figure 3 and Table 1 show the desquamated area (%) of the stratum corneum for each wound dressing. There was a significant difference in the desquamated area (%) between wound dressing A and wound dressings G, B, T, U and between wound dressing R and wound dressings G, B, T, U (P < 0·05). According to the types of adhesive used, a lower amount of the stratum corneum was removed from healthy skin in the wound dressing using silicone adhesive (G, B, T; mean, 0·62%) and self‐adhesive polyurethane foam (U; 0·99%), whereas a higher amount of stratum corneum was removed in hydrocolloid (R, E, C; mean, 9·45%) and polyurethane foam using acrylic adhesive (A; mean, 12·97%).
Figure 3.
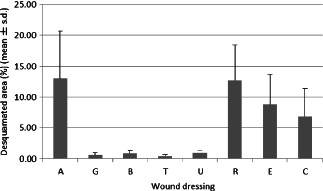
Percentage of desquamated area of the stratum corneum for each wound dressing (i.e. A, G, B, T, U, R, E or C).
Table 1.
Mean desquamated area (%) of the stratum corneum for each wound dressing
| Desquamated area (%) | A | G | B | T | U | R | E | C |
|---|---|---|---|---|---|---|---|---|
| Mean | 12·97 | 0· 59 | 0· 91 | 0· 37 | 0· 99 | 12·70 | 8· 82 | 6· 82 |
| SD | 7·70 | 0· 40 | 0· 42 | 0· 26 | 0· 38 | 5·71 | 4· 88 | 4· 57 |
Discussion
We set out to quantitatively determine and compare the amount of stratum corneum of the skin removed by several different self‐adherent wound dressings in healthy volunteers. In wound management, retention bandaging and adhesion of the wound dressing to the site are required to ensure adequate wound protection. In this context, adhesive wound dressings have been developed and routinely used. However, adhesive wound dressings may potentially damage the periwound skin and newly formed epithelium when they are removed. In many cases, particularly in chronic wounds, wound dressings are repeatedly applied to and removed from the same location of the skin, leading to skin stripping, that is, the sequential removal of the stratum corneum around the wound. As skin stripping progresses, the skin barrier may be lost, resulting in transepidermal water loss (3), which in turn causes an increase in the wound size, exacerbated wound pain and delayed wound healing (1). In patients with chronic wounds, the periwound skin is fragile and most of them have concurrent dermatitis. Thus, their periwound skin is increasingly vulnerable to damage by adhesive wound dressings 4, 5.
An ideal adhesive is one that (a) minimises adhesion to the wound surface and newly formed epithelium, (b) inhibits the leakage of exudate from wounds to the healthy skin and thereby minimising the risk of periwound skin maceration, (c) causes no damage upon removal, (d) creates a condition that facilitates wound healing and (e) securely retains wound dressings in place. Thus, an adhesive must have excellent and balanced properties. To meet these properties, it is recommended to use a wound dressing that has a layer for water absorption and whose adhesive appropriately adheres to the adherent surface without peeling the healthy skin upon removal. A good measure for assessing and comparing the clinical performance of various wound dressings is to determine the amount of stratum corneum removed from healthy skin upon removal of each type of wound dressing. Factors that may affect the level of adhesion of wound dressings to normal skin include skin conditions such as the amount of sebum, levels of dryness and sweating and the period of application (6).
We determined the amount of stratum corneum removed in ten healthy adults using a uniform method in which adhesive wound dressings were applied to the hairless area of the forearm of each subject for 24 hours and the same operator removed the adhesive dressings at the same speed (Figure 3). Therefore, the use of dressings and the conditions used in this study were similar to those in clinical practice. In this context, the study findings are considered to be consistent with those in the clinical setting except for the abnormal skin which is usually found surrounding ‘chronic’ wounds.
We used eight different adhesive wound dressings to compare the amount of stratum corneum removed from normal skin when the dressings were removed. An adhesive tape was applied to the adherent surface of each wound dressing to print the stratum corneum to the adhesive tape. Then, the printed stratum corneum on the adhesive tape was stained to determine the amount of stratum corneum removed.
It is possible to more accurately measure the amount of stratum corneum removed using a method in which the stratum corneum that is attached to the adherent surface is stained directly. However, as some adhesive wound dressings were stained by a dye, it was impossible to precisely quantify the amount of stratum corneum removed because of the staining of the dressing material itself.
Regarding quantification of the amount of stratum corneum removed, Dykes et al. used a silicone scar tape (Mepiform), hydropolymer dressing (Tielle) and hydrocolloid dressing (Duoderm Extra Thin) (7). They stained the shallow stratum corneum of the skin with eosin–methylene blue using the skin surface biopsy method and measured the optimal density. Warnig et al. (2) evaluated the amount of stratum corneum removed by adhesive wound dressings including polyurethane foam using acrylic adhesive (Allevyn adhesive), hydrocolloid, hydrofiber (Versiva XC, Biatain, Urgotul Trio) and polyurethane foam using silicone adhesive (Mepilex border) by vital staining with DHA and measured and compared changes in the status of each adhesive wound dressing before and after application using a chromametre and scanning electron microscope. The two studies showed that silicone adhesives removed less amount of stratum corneum.
Our findings were consistent with previous findings that wound dressings using silicone adhesive remove less amount of stratum corneum of normal skin than those using acrylic adhesive or hydrocolloid. Also, we reported for the first time that the removal of self‐adhesive polyurethane foam dressing was associated with damage to the skin similar to silicon dressing.
In recent years, the removal of wound dressings has been shown to cause the most intense pain among dressing‐related procedures (8). In particular, wound dressings may strongly adhere to the wound and pose problems of skin stripping upon dressing removal (9).
Klode et al. reported that the pain induced upon the removal of modern wound dressings was associated with the adhesive strength of a particular dressing (10). On the other hand, Warning et al. reported that pain was greater with wound dressings that peeled a larger amount of skin using the same peeling force (11). It can therefore be considered that less damage to the periwound skin resulting from the adhesion of wound dressing would reduce pain upon wound dressing removal. We previously showed by quantitative analysis that upon removal, less pain was induced by silicone adhesive dressing than by acrylic adhesive consistent with the present results (12).
Conclusion
We quantitatively determined and compared the amount of stratum corneum removed by eight different wound dressings in healthy volunteers. Wound dressings using silicone adhesive and self‐adhesive polyurethane foam removed less stratum corneum, whereas composite hydrocolloid and polyurethane foam using acrylic adhesive removed more stratum corneum.
Acknowledgements
We are indebted to Associate Professor Edward Barroga and Prof. J. Patrick Barron, Chairman of the Department of International Medical Communications of Tokyo Medical University, for their editorial review of the English manuscript. All authors declare that they have no conflicts of interest associated with this manuscript.
References
- 1. Hollinworth H, White R. The clinical significance of wound pain. In: White R, Harding K, editors. Trauma and pain in wound care. Wounds UK, 2006:3–16. [Google Scholar]
- 2. Waring M, Bielfeldt S, Matzold K, Wilhelm KP, Butcher M. An evaluation of the skin stripping of wound dressing adhesives. J Wound Care 2011;20:412, <414, 416–22. [DOI] [PubMed] [Google Scholar]
- 3. van der Valk PG, Maibach HI. A functional study of the skin barrier to evaporative water loss by means of repeated cellophane‐tape stripping. Clin Exp Dermatol 1990;15:180–2. [DOI] [PubMed] [Google Scholar]
- 4. Saap L, Fahim S, Arsenault E, Pratt M, Pierscianowski T, Falanga V, Pedvis‐Leftick A. Contact sensitivity in patients with leg ulcerations: a North American study. Arch Dermatol 2004;140:1241–6. [DOI] [PubMed] [Google Scholar]
- 5. Simon DA, Dix FP, McCollum CN. Management of venous leg ulcers. BMJ 2004;328:1358–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rippon M, White R, Davies P. Skin adhesives and their role in wound dressings. Wounds UK 2007;3:76–86. [Google Scholar]
- 7. Dykes PJ, Heggie R, Hill SA. Effects of adhesive dressings on the stratum corneum of the skin. J Wound Care 2001;10:7–10. [DOI] [PubMed] [Google Scholar]
- 8. Principles of best practice: minimising pain at wound dressing‐related procedures. A consensusdocument. London: MEP Ltd., 2004. URL http://www.wuwhs.org/datas/2_1/2/A_consensus_document_‐_Minimising_pain_at_wound_dressing_related_procedures.pdf [accessed on 8 April 2012].
- 9. Grocott P. The palliative management of fungating malignant wounds. J Wound Care 2000;9:4–9. [DOI] [PubMed] [Google Scholar]
- 10. Klode J, Schottler L, Stoffels I, Korber A, Schadendorf D, Dissemond J. Investigation of adhesion of modern wound dressings: a comparative analysis of 56 different wound dressings. J Eur Acad Dermatol Venereol 2011;25:933–9. [DOI] [PubMed] [Google Scholar]
- 11. Waring M, Rippon M, Bielfeldt S, Brandt M. Cell attachment to adhesive dressings: qualitative and quantitative analysis. Wounds UK 2008;4:35–47. [Google Scholar]
- 12. Matsumura H, Imai R, Gondo M, Watanabe K. Evaluation of pain intensity measurement during the removal of wound dressing material using‘the PainVision™ system’ for quantitative analysis of perception and pain sensation in healthy subjects. Int Wound J 2012; DOI: 10.1111/j.1742-481X.2011.00911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


