Abstract
Nicorandil, a second‐generation nitro derivative, has been reported to induce single or multiple ulcerations in many locations, including oral, anal, perianal, vulvovaginal, perivulval, penile, gastrointestinal, colic, peristomal and skin locations. Ocular locations are now highly suspected. Herein, we report the case of a 78‐year‐old woman who experienced corneal ulceration at second cataract surgery (right eye) while being treated with nicorandil for 3 years. Four years before, she had had an uneventful first cataract surgery (left eye). The ulcers healed within 6 weeks after simple withdrawal of nicorandil, an expected delay for this type of chemical ulcer. The substitution of nicorandil with classic nitric oxide donors has already been done without complication. Surgical intervention is unnecessary and inappropriate. Case reports of ocular side effects induced by nicorandil are rare and probably underestimated.
Keywords: Chemically induced, Corneal ulcer, Injuries, Nicorandil
Introduction
Nicorandil (ADANCOR®; Merck Serono, Lyon, France, IKOREL®; Sanofi‐Aventis France, Paris, France, etc.) is an original vasodilatator used to control angina. This drug is the first and only association of nitrates and potassium channel activators (PCA), and it is considered a second‐generation nitro derivative. The nicotinamide moiety that supports the PCA effect is also present in its metabolites. Initially marketed in Japan in 1984 by Chugai Co Ltd and later in European, Asian and Pacific countries, nicorandil was first found to be involved in the genesis of ulcers in 1997 1. Since then, many cases of single or multiple nicorandil‐induced ulcerations in oral, anal, perianal, vulvovaginal, perivulval, penile, gastrointestinal, colonic, peristomal and skin locations have been published 2. More recently, fistulae 3 and ocular locations 4 have been highly suspected. Surprisingly, neither PCA nor nitric oxide (NO) donors have been documented as inducing corneal ulcerations.
Case
A 78‐year‐old woman was admitted to our department in December 2011 after complaining of pain and photophobia of the right eye following cataract surgery performed 2 months earlier. Her medical history revealed an uneventful left eye cataract surgery 4 years previously. She also had hypertension since 1984, hypothyroidism since 1985 and angina and venous thromboembolic disease with stent insertion in 2009.
On admission, her usual treatment was levothyroxin, celiprolol, felodipine and valsartan; warfarin and nicorandil started in December 2009. Her ocular symptoms had begun 15 days after the surgery and she was immediately prescribed anti‐herpes simplex virus medication (valacyclovir).
When she presented, she had a persisting corneal ulceration (Figure 1). Valacyclovir was continued and local healing treatment (fluorometholone and sodium hyaluronate) was added. Ten days later, corneal ulceration had not improved; visual acuity was 20/125 and slit‐lamp examination revealed epithelial erosion, stroma thinning, folds in the Descemet's membrane and reactive peripheral neovascularisation. The anterior chamber was calm and fundus examination was normal. The lesion was not explained by mechanical (eyelid and ciliary pathologies, foreign body), inflammatory, infectious or local causes. No pathogen was found, polymerase chain reaction was negative for Acanthamoeba and corneal scrapings for direct examination and culture remained negative.
Figure 1.
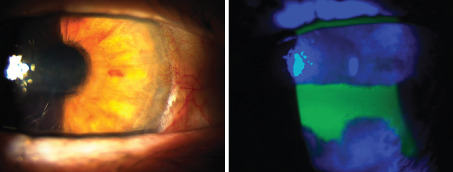
Corneal ulceration on slit‐lamp examination and fluorescein staining (right eye).
At that point, nicorandil treatment was suspected to be the causal agent of delayed corneal healing and persisting ulceration, and therefore was discontinued after the approval of the cardiologist. Valacyclovir was maintained. The patient underwent weekly medical supervision, and after 6 weeks, we observed complete healing, disappearance of symptoms and improved visual acuity (20/40). Nicorandil was not reintroduced. At 11‐month follow‐up, ocular lesion did not reoccur.
This case strongly suggests drug‐induced corneal ulceration, based on the sequence of events, the exclusion of other pathologies and the spontaneous regression of the side effect when the drug was discontinued. Nicorandil ulcerations seem to occur at vulnerable sites, being peristomal after the Hartmann's procedure, penile after circumcision and perianal after haemorrhoidectomy 5, 6, 7; they are also associated with implantation scarring after implanting a pace maker, diverticulosis, and so forth. In our case, the patient was not treated with nicorandil at first cataract surgery, which remained uneventful. However, she had been receiving nicorandil (20 mg/day) for 3 years before the second cataract surgery, which was complicated by corneal ulceration. In addition, the ulcers healed within 6 weeks after withdrawal of nicorandil, an expected delay for this type of chemical ulcer (15 days up to 4 months mainly depending on the location of the ulcer) 8. Case reports of ocular side effects induced by nicorandil are rare and probably underestimated 4.
The pathogeneses of nicorandil‐induced ulcerations (direct toxicity of the drug, steal phenomenon, etc.) are not yet elucidated. A recent hypothesis suggested that, most frequently, in cases of prolonged high‐dose treatment and/or after increased dosage, nicotinic acid and nicotinamide (two metabolites of nicorandil) may become unable to merge into the endogenous pool of nicotinamide adenine dinucleotide phosphate (NAD/NADP), leading to abnormal distribution of these two molecules in the whole body. In the case of a recent or maintained trauma, nicotinamide could increase blood flow at the edge of the raw area, inducing epithelial proliferation, while nicotinic acid may ulcerate this new epithelial tissue, ultimately flooding the whole scar 8.
Thus, this hypothesis of chemical ulceration is based on the effects of nicotinamide (PCA) coupled with the direct ulcerating effects of nicotinic acid, explained by an in vivo pKa of 4·9. The role of nicotinamide is strengthened by the fact that its vasodilating effects on blood tumour flow suggest that it may function as a radiosensitiser 9. Moreover, minoxidil, another PCA, acts directly on arterioles, dilating them without promoting oedema and leading to increased blood flow at the edge of the scar 10.
Discontinuation of nicorandil usually induces complete healing after a few weeks, mainly depending on the location of the ulcer. Surgical intervention is unnecessary and inappropriate, as it is ineffective and exacerbates morbidity (probably by digging the furrow for nicotinic acid). The replacement of nicorandil with a classic NO donor, under the aegis of a cardiologist, has already been done without complication.
This case confirms that nicorandil may induce ocular toxicity, which mostly occurs in the elderly and fragile population; a previously injured area, whether recent or maintained, symptomatic or not, is required for the genesis of nicorandil‐induced ulcer and simply withdrawing nicorandil treatment results in complete healing.
Acknowledgements
None of the authors has conflict of interest to declare. No financial support was received for this article.
Trechot F, Batta B, Petitpain N, Bazard MC, Angioi K, Trechot P. A case of nicorandil‐induced unilateral corneal ulceration.
References
- 1. Reichert S, Antunes A, Trechot P, Barbaud A, Weber M, Schmutz JL. Major aphthous stomatitis induced by nicorandil. Eur J Dermatol 1997;7:132–3. [Google Scholar]
- 2. Watson A, Ol‐Ozairi O, Fraser A, Loudon M, O'Kelly T. Nicorandil associated anal ulceration. Lancet 2002;36:546‐7. [DOI] [PubMed] [Google Scholar]
- 3. Trechot P, Petitpain N, Guy C, Pinzano A, Javot L, Schmutz JL, Marie B, Barbaud A. Nicorandil: from ulcer to fistula into adjacent organs. Int Wound J 2013;10:210–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Trechot P, Bazard MC, Petitpain N, Trechot F, Javot L, Angioi K. Conjunctival and corneal ulcerations: keep a sharp eye on nicorandil. Br J Ophthalmol 2012;96:463–4. [DOI] [PubMed] [Google Scholar]
- 5. Kidd L, Dixon C. Nicorandil‐induced peristomal ulceration. Int Wound J 2010;7:541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yap T, Philippou P, Perry M, Lam W, Corbishley C, Watkin N. Nicorandil‐induced penil ulcerations: a case series. BJU Int 2001; 107:268‐71. [DOI] [PubMed] [Google Scholar]
- 7. Riddell AD, Minhas U, Williams GL, Harding KJ. The role of nicorandil in non‐healing surgical wounds. Ann R Coll Surg Engl 2010;92:W16–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Trechot P, Claeys A, Petitpain N, Javot L, Schmutz JL, Barbaud A. Nicorandil and ulcerations: the Trojan horse ? J Eur Acad Dermatol Venereol 2012;26:925–6. [DOI] [PubMed] [Google Scholar]
- 9. Horsman MR, Chaplin DJ, Brown JM. Tumor radiosensitization by nicotinamide a result of improved perfusion and oxygenation. Radiat Res 1989;118:139–50. [PubMed] [Google Scholar]
- 10. Brenda E, Marques A, Saldiva PHN, Hidalgo GS, Goldenberg S. Action of papain, sugar, minoxidil, and glucagon on excisional wounds in rats. Curr Ther Res 1995;56:1285–97. [Google Scholar]


