Abstract
For several wound products compelling evidence is available on their effectiveness, for example, from systematic reviews. The process of buying, prescribing and applying wound materials involve many stakeholders, who may not be aware of this evidence, although this is essential for uniform and optimum treatment choice. In this survey, we determined the general awareness and use of evidence, based on (Cochrane) systematic reviews, for wound products in open wounds and burns among wound care stakeholders, including doctors, nurses, buyers, pharmacologists and manufacturers. We included 262 stakeholders. Doctors preferred conventional antiseptics (e.g. iodine), while specialised nurses and manufacturers favoured popular products (e.g. silver). Most stakeholders considered silver‐containing products as evidence‐based effective antiseptics. These were mostly used by specialised nurses (47/57; 82%), although only few of them (9/55; 16%) thought using silver is evidence‐based. For burns, silver sulfadiazine and hydrofibre were most popular. The majority of professionals considered using silver sulfadiazine to be evidence‐based, which contradicts scientific results. Awareness and use of the Cochrane Library was lower among nurses than among doctors (P < 0·001). Two thirds of the manufacturers were unaware of, or never used, the Cochrane Library. Available compelling evidence in wound care is not equally internalised by stakeholders, which is required to ensure evidence‐based decision making.
Keywords: Decision making, Evidence‐based practice, Implementation, Systematic review, Wound care
INTRODUCTION
To date, health care professionals are expected to keep abreast of current professional knowledge, and to apply research evidence in their daily practice in order to deliver the highest possible quality of care. Ideally, the evidence‐based practice (EBP) paradigm promotes evidence‐based decision making with patients in clinical practice, preferably derived from proper (Cochrane) systematic reviews, if any, or well‐performed clinical trials. Reality, however, shows that 30–40% of patients receive care that is not in accordance with available high quality research evidence, while another 20–30% of patients receive care that is even contraindicated (1). Furthermore, the existence of guidelines does not guarantee its actual application. Guideline recommendations are followed in on average 67% of the treatment decisions made (2). From these figures, it is obvious that the EBP paradigm has not yet been adopted by all health care professionals in their daily practice (3).
In wound care, an additional phenomenon is apparent. The available therapeutic options to choose from may be influenced by many different health care stakeholders (i.e. doctors, nurses, manufacturers, buyers, pharmacists), as well as by the patients' preferences. Although the experiential knowledge from all these stakeholders is a necessity, it is not a sufficient basis for clinical decision making (4). Hence, odds are high that the eventual treatment given is not evidence‐based if one or more of these stakeholders do not make an evidence‐based decision or are not aware of available high quality evidence. In other words, a joint venture is needed to make evidence‐based wound treatment work.
Evidence‐based wound care could also be seen as a challenge. Because of the lack of high quality research evidence or evidence‐based guidelines to help choose the most appropriate form of local wound care and thus challenging evidence‐based decision making (5). However, for some indications in wound care high quality evidence is available, which does make evidence‐based treatment decisions possible 6, 7, 8, 9, 10, 11. Recently, well‐performed systematic reviews with recommendations as to the use of antiseptics for preventing and treating wound infections have been produced and disseminated at various (inter)national conferences and among different audiences 6, 7, 8, 9, 10. These reviews, for example, present high quality evidence about the effectiveness of honey dressings, iodine and silver sulfadiazine for specific wounds. For many years, iodine has been dissuaded because of its purported adverse effects, but was recently shown to be at least as effective as other antiseptics without serious harmful effects, such as a delay in wound healing, particularly in chronic and burn wounds (6). In contrast, silver sulfadiazine, although still the treatment of choice in burn wounds, was found not to counteract infections more than other antiseptic agents, while decelerating wound healing in patients with partial‐thickness burns 9, 11.
Because of the growing body of high quality evidence on the (in)effectiveness of certain (antiseptic) wound dressings or agents, it seems unethical to administer ineffective treatments or to withhold patients from the best available evidence‐based treatments.
Therefore, the aim of this study was to explore the general awareness and use of compelling research evidence, based on available (Cochrane) systematic reviews, among several groups of wound care stakeholders in health care.
METHODS
Study setting
From April to September 2010, we contacted 31 Dutch medical centres, including all university (n = 8) and burn centres (n = 3), 13 home care institutions, 100 primary care facilities and 12 manufacturers of wound care products to take part in this study.
Participants
A representative, broad range of different health care professionals involved in wound care was recruited. These involved surgeons, plastic surgeons, dermatologists, general practitioners (GPs), surgical nurses, home care nurses, specialised wound care nurses, as well as manufacturers of wound care products, totalling eight professional groups. We aimed for about 25 professionals per group to obtain a full scale of possible answers. We included twice as many clinical and wound specialist nurses as they are key performers in daily wound care. Furthermore, interviews were planned with the heads of the hospital's buyer and pharmacy departments.
Questionnaire
To assess awareness and use in daily practice of the available, high quality research evidence on antiseptics and wound care products by wound care stakeholders in the Netherlands, a short questionnaire was designed. It consisted of five questions, each relating to personal preference and awareness of evidence from (Cochrane) systematic reviews:
-
1
When considering an antiseptic dressing for an open wound, what would be your top three of wound care products?
-
2
For which antiseptic wound care products has the effectiveness been established, based on high‐level evidence, for the treatment of open wounds?
-
3
What would be your top three wound care products for the local treatment of open partial‐thickness burns?
-
4
For which wound care products has the effectiveness been established, based on high quality research evidence, for the treatment of open partial‐thickness burns?
-
5
How often do you consult the Cochrane Library?
A list of various wound care products was given to choose from (1, 2). This list was based on common usage in daily practice and available evidence from (Cochrane) systematic reviews 6, 8, 9, 11. Participants also had the opportunity to choose ‘other’. Furthermore, we noted the stakeholders' age and function.
Table 1.
Choices of antiseptic products in the treatment of open wounds and awareness of evidence
| Professionals | Total (N) * | Chlorhexidine (%) | Eusol® (%) | Fucidin® (%) | Furacin® (%) | Honey (%) | Iodine (%) | Silver product (%) | Other (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Surgeons | Usage | 24 | 13 (54) | 7 (29) | 6 (25) | 1 (4) | 6 (25) | 9 (38) | 9 (38) | 8 (33) |
| Evidence ** | 22 | 14 (64) | 6 (27) | 3 (14) | 4 (18) | 10 (45) | 9 (41) | 12 (55) | NA | |
| Plastic surgeons | Usage | 25 | 8 (32) | 13 (52) | 14 (56) | 8 (32) | 6 (24) | 8 (32) | 6 (24) | 1 (4) |
| Evidence ** | 25 | 12 (48) | 8 (32) | 11 (44) | 10 (40) | 9 (36) | 14 (56) | 9 (36) | NA | |
| Dermatologists | Usage | 37 | 15 (41) | 11 (30) | 19 (51) | 1 (3) | 2 (5) | 24 (65) | 21 (57) | 2 (5) |
| Evidence ** | 37 | 17 (46) | 7 (19) | 15 (41) | 1 (3) | 7 (19) | 14 (38) | 19 (51) | NA | |
| General practitioners | Usage | 8 | 3 (38) | 0 (0) | 6 (75) | 0 (0) | 1 (13) | 8 (100) | 3 (38) | 2 (25) |
| Evidence ** | 7 | 2 (29) | 1 (14) | 4 (57) | 1 (14) | 1 (14) | 4 (57) | 4 (57) | NA | |
| Specialised nurses | Usage | 57 | 6 (11) | 14 (25) | 11 (19) | 2 (4) | 31 (54) | 24 (42) | 47 (82) | 24 (40) |
| Evidence ** | 55 | 2 (4) | 11 (20) | 8 (15) | 3 (5) | 13 (24) | 35 (64) | 9 (16) | NA | |
| Surgical nurses | Usage | 65 | 27 (42) | 25 (38) | 13 (20) | 7 (11) | 15 (23) | 23 (35) | 37 (57) | 33 (51) |
| Evidence ** | 51 | 26 (51) | 14 (27) | 14 (27) | 7 (14) | 17 (33) | 25 (49) | 26 (51) | NA | |
| Home care nurses | Usage | 17 | 5 (31) | 6 (38) | 7 (44) | 0 (0) | 7 (44) | 9 (56) | 11 (69) | 2 (13) |
| Evidence ** | 15 | 5 (33) | 6 (40) | 4 (27) | 1 (7) | 8 (53) | 5 (33) | 8 (53) | NA | |
| Manufacturers | Usage | 23 | 2 (9) | 6 (26) | 4 (17) | 0 (0) | 13 (57) | 7 (30) | 20 (87) | 15 (65) |
| Evidence ** | 21 | 1 (5) | 1 (5) | 1 (5) | 0 (0) | 6 (29) | 14 (67) | 13 (62) | NA | |
NA, not applicable.
* N is total number of participants who answered the question.
**Evidence is number of respondents who have the opinion that the effectiveness of a particular product is evidence‐based.
Table 2.
Choices of wound care products in the treatment of open partial‐thickness burns and awareness of evidence
| Professionals | Item | Total (N) * | Chlorhexidine (%) | Film (%) | Hydrofibre (%) | Honey (%) | Iodine (%) | Paraffin gauze (%) | Silver sulfadiazine (%) | Silver‐containing dressing (%) | Other (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgeons | Usage | 23 | 0 (0) | 1 (4) | 11 (48) | 0 (0) | 2 (9) | 11 (48) | 20 (87) | 2 (9) | 4 (17) |
| Evidence ** | 23 | 1 (4) | 1 (4) | 10 (43) | 3 (13) | 2 (9) | 2 (9) | 7 (30) | 4 (17) | NA | |
| Plastic surgeons | Usage | 25 | 1 (4) | 6 (24) | 13 (52) | 1 (4) | 0 (0) | 15 (60) | 20 (80) | 4 (16) | 0 (0) |
| Evidence ** | 24 | 2 (8) | 5 (21) | 10 (42) | 2 (8) | 4 (17) | 6 (25) | 18 (75) | 6 (25) | NA | |
| Dermatologists | Usage | 34 | 2 (6) | 6 (18) | 11 (32) | 2 (6) | 2 (6) | 21 (62) | 15 (44) | 14 (41) | 11(32) |
| Evidence ** | 33 | 3 (9) | 4 (12) | 5 (15) | 3 (9) | 4 (12) | 8 (24) | 8 (24) | 7 (21) | NA | |
| General practitioners | Usage | 6 | 1 (17) | 0 (0) | 2 (33) | 0 (0) | 2 (33) | 4 (67) | 5 (83) | 0 (0) | 0 (0) |
| Evidence ** | 7 | 2 (29) | 0 (0) | 2 (29) | 2 (29) | 2 (29) | 3 (43) | 3 (43) | 1 (14) | NA | |
| Specialised nurses | Usage | 56 | 2 (4) | 4 (7) | 49 (88) | 3 (5) | 1 (2) | 31 (55) | 40 (71) | 16 (29) | 0 (16) |
| Evidence ** | 57 | 3 (5) | 1 (2) | 36 (63) | 2 (4) | 6 (11) | 3 (5) | 41 (72) | 4 (7) | NA | |
| Surgical nurses | Usage | 50 | 6 (12) | 12 (24) | 23 (46) | 5 (10) | 3 (6) | 37 (74) | 27 (54) | 12 (24) | 5 (10) |
| Evidence ** | 41 | 9 (22) | 12 (29) | 19 (46) | 10 (24) | 12 (29) | 17 (41) | 21 (51) | 19 (46) | NA | |
| Home care nurses | Usage | 16 | 1 (7) | 2 (13) | 6 (40) | 3 (20) | 1 (7) | 12 (80) | 9 (60) | 4 (27) | 3 (20) |
| Evidence ** | 10 | 2 (20) | 1 (10) | 2 (20) | 2 (20) | 1 (10) | 7 (70) | 7 (70) | 3 (30) | NA | |
| Manufacturers | Usage | 21 | 0 (0) | 4 (19) | 16 (76) | 2 (10) | 0 (0) | 5 (24) | 8 (38) | 10 (48) | 13 (62) |
| Evidence ** | 19 | 1 (5) | 3 (16) | 11 (58) | 2 (11) | 1 (5) | 1 (5) | 3 (16) | 8 (42) | NA |
NA, not applicable.
* N is total number of participants who answered the question.
**Evidence is number of respondents who have the opinion that the effectiveness of a particular product is evidence‐based.
Collection of responses
We used different methods to collect the responses. Firstly, during a national meeting of specialised wound care nurses and during presentations of Plastic Surgeons and Dermatologists we used electronic voting devices: ResponseCard™ keypads linked to TurningPoint for Microsoft® PowerPoint® (Turning Technologies, Ohio – version: 4·1 · 0·9020). No discussion was allowed. Secondly, we contacted medical centres and home care institutions by telephone. Thirdly, we distributed 35 CDROMs with the questions to doctors and nurses of 12 Dutch medical centres. Fourthly, some hospitals and home care centres requested we should attach the questionnaire to a cover letter addressed to the local doctors, nurses, and manufacturers, which was distributed via email. Health care professionals could only respond once to the questions.
Data analysis
Data were entered into PASW statistics 18·0 (SPSS Inc, Chicago, IL). Statistical analyses included descriptive statistics of the top three choice of wound care products used, and awareness of evidence. The relation between age and the use of the Cochrane Library among the different groups were compared using the Kruskal–Wallis test, with P < 0·05 considered significant. The same test was used to detect differences between the professional groups. The Mann–Whitney U test was used to compare the awareness and use of the Cochrane Library among doctors and nurses.
We used the chi‐square (χ 2) statistic to whether the different methods of investigation (by email, phone or plenary presentation) influenced the results.
RESULTS
A total of 262 professionals were included in this survey; 96 doctors, 143 nurses and 23 manufacturers of wound care products. The age distribution of the professionals is shown in Table 3. The age distributions are representative of the Dutch health care professional situation.
Table 3.
Age distribution of professionals (in years)
| <31 | 31–40 | 41–50 | 51–60 | >61 | |
|---|---|---|---|---|---|
| Surgeons (n = 24) | 5 | 8 | 5 | 3 | 3 |
| Plastic surgeons (n = 25) | 13 | 7 | 3 | 2 | 0 |
| Dermatologists (n = 39) | 21 | 9 | 4 | 5 | 0 |
| General practitioners (n = 8) | 0 | 2 | 3 | 2 | 1 |
| Specialised nurses (n = 57) | 3 | 15 | 25 | 12 | 2 |
| Nurses (n = 69) | 38 | 8 | 9 | 13 | 1 |
| Home care nurses (n = 17) | 5 | 4 | 6 | 2 | 0 |
| Manufacturers (n = 23) | 5 | 7 | 4 | 7 | 0 |
Completeness of data
In total, 126 of 262 (48%) questionnaires were filled in completely, without any missing data. The main reason for missing data was a lack of experience with treatment of patients with burn wounds or not supplying three preferences. After comparing the complete questionnaires with the results of the incomplete ones, no substantial differences were found in the top three. Therefore, we present the results of all answers given. No significant differences were found between a shorter (telephone or electronic voting devices) or longer (email or CDROM) answering time.
Products for open wounds
The first choice of antiseptics used for the treatment of open wounds as given by the professional groups is shown in Table 4. The first choice within the groups of specialised nurses and manufactures for the local treatment of open wounds was silver‐containing products. Doctors were more inclined to use conventional antiseptic products (e.g. Eusol®, chlorhexidine and iodine) than nurses, who more often chose popular antiseptic agents (e.g. silver products). Usage and awareness among the respondents of available evidence for each antiseptic wound care product is given in Table 1. In the majority of the professional groups (six of the eight groups), over 50% of the respondents held the opinion that the effectiveness of silver‐containing products is evidence‐based. This opinion was also found in half of the groups for iodine and in 2/8 groups for chlorhexidine. In contrast, neither Eusol® nor Furacin® was considered supported by evidence. Notably, silver‐containing products were mostly used by specialised nurses (47/57; 82%), but only few (9/55; 16%) stated to be aware of any evidence about the effectiveness of silver for open wounds. Remarkably, the number of doctors who used honey was lower than the number of doctors who stated to be aware of the evidence of its effectiveness. The opposite was observed in specialised wound care nurses and manufacturers.
Table 4.
Stakeholders' first choice of antiseptic products in the treatment of open wounds
| Surgeons | Chlorhexidine (42%) |
| Plastic surgeons | Eusol (28%) |
| Dermatologists | Iodine (65%) |
| General practitioners | Iodine (38%) |
| Specialised nurses | Silver‐containing products (32%) |
| Surgical nurses | Chlorhexidine (20%) |
| Home care nurses | Iodine (59%) |
| Manufacturers | Silver‐containing products (48%) |
Products for burn wounds
The majority of professionals reported silver sulfadiazine, as their first choice for the local treatment of open partial‐thickness burns (Table 5). In half of the groups (4/8), over 50% of the respondents answered that the effectiveness of silver sulfadiazine is evidence‐based. This was also the case in 2/8 groups for hydrofibre and in 1 group for paraffin gauze, but none of the groups considered the effectiveness of chlorhexidine, film, honey, or iodine as evidence‐based (Table 2). Strikingly, all groups often used paraffin gauze (with the exception of manufacturers), but only few in each group stated to be aware of any evidence about its effectiveness.
Table 5.
Stakeholders' first choices of wound care products in the treatment of partial‐thickness burns
| Surgeons | Silver sulfadiazine (67%) |
| Plastic surgeons | Silver sulfadiazine (76%) |
| Dermatologists | Silver sulfadiazine (32%) |
| General practitioners | Silver sulfadiazine (38%) |
| Specialised nurses | Hydrofibre (54%) |
| Surgical nurses | Silver sulfadiazine (29%) |
| Home care nurses | Paraffin gauze (41%) |
| Manufacturers | Hydrofibre (39%) |
Awareness and use of the Cochrane Library
Figure 1 shows the awareness and use of the Cochrane Library in daily practice.
Figure 1.
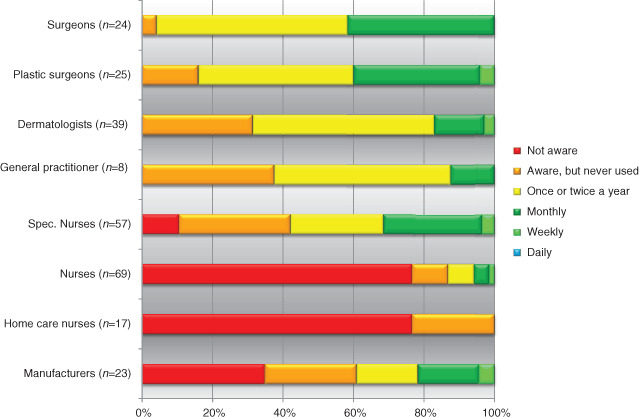
Cochrane Library knowledge and use.
Doctors
All doctors were aware of the Cochrane Library; almost half of them used it once or twice a year. Surgeons (10/24; 42%) and plastic surgeons (10/25; 40%) tended to use the Cochrane Library more frequently (monthly or more often) than dermatologists (6/39; 15%) and GPs (1/8; 13%). However, this difference was not statistically significant (P = 0 · 724). Surprisingly, more than a quarter of the dermatologists and GPs was aware of the Cochrane Library but never used it.
Nurses and manufacturers
Awareness and usage of the Cochrane Library was lower among nurses than among doctors (P < 0·001). Nevertheless, this awareness was much higher in specialised nurses than in surgical and home care nurses (P = 0 · 001), of whom more than 75% stated to be unaware. The usage of the Cochrane Library among these nursing groups was poor, although more than a quarter of the specialised wound care nurses used it on a monthly basis. Among the manufacturers, two thirds were not aware of, or never used, the Cochrane Library.
Age and use of the Cochrane Library
No significant relations were found between age and awareness or use of the Cochrane Library among any of the groups.
Buyer and pharmacy departments
From the interviews with representatives of the buyer and pharmacy departments we learned that they had no preference and were not aware of any evidence regarding the effectiveness of the wound care products and could therefore not answer the questions posed. They merely ordered and delivered the products as requested by the doctor or nurse taking care of the wound patients.
DISCUSSION
Choices made in wound care by the various stakeholders are not always evidence‐based, despite the availability of compelling research evidence from systematic reviews with recommendations for practice. For example, most health care professionals hold the opinion that the effectiveness of silver‐containing wound care products, in particular silver sulfadiazine, is established, but this is in contrast with the results of three Cochrane systematic reviews 8, 9, 11, which suggest silver sulfadiazine has more disadvantages compared with other antiseptics. These reviews report on evidence that is sometimes over 10 years old, but this has not reached the minds of present‐day wound care professionals yet. The latency between the publication of evidence and its integration in daily practice may take a quarter of a century, and the scientific and clinical realms seem to have reconciled themselves with this notion (12).
There is an ongoing discussion about the usefulness of Cochrane systematic reviews 13, 14. Most of these reviews end by concluding that the volume and quality of the existing research is low, the consistency of study designs is lacking (e.g. regarding study endpoints), few replication studies exist, meta‐analysis is usually impossible because of heterogeneity of the studies, and most included studies are at high risk of bias (13). Therefore, clinicians often receive no recommendations what to do in daily practice (14). On the other hand, reality shows that many published trials have methodological inadequacies. Therefore, it is important that Cochrane reviews highlight these methodological inadequacies, so that researchers pay more attention to the methodological quality of future research. In the case of the absence of compelling evidence, clinicians should rely on expert‐opinion and consensus‐based guidelines to assist clinical decision making (13).
Findings in our study are supported by previous cross‐sectional studies. Knops et al. showed that surgeons use only about half of the convincing evidence (3). Four other studies investigated the awareness and use of the Cochrane Library; they concluded that there is little awareness 15, 16, 17, and subsequently little use of the Cochrane Library among health care professionals 16, 17, 18. From a study performed by Sigouin et al. it is known that differences between professional groups exist, as they found a significant difference in favour of oncologists compared with oncology nurses related to awareness of the Cochrane Library (15). Therefore, our results seem also true for other countries than only the Netherlands.
To turn the tide, Adamsen et al. proposed to develop an education strategy to provide stakeholders with evidence‐based knowledge that empowers them to make evidence‐based decisions (19). Nevertheless, a recently published systematic review showed that there is insufficient evidence about which types of interventions are effective to encourage the use of systematic reviews by professionals in clinical decision making (20). Although it is accepted that not all professionals should be involved in research, stakeholders should be able to critique and apply research pertinent to their area 21, 22. This is in accordance with the conceptual framework Strauss et al. described, in which they propose that professionals can practice evidence‐based medicine in one of three modes – as a doer, a user or a replicator (23). Journal clubs may also be used as a feature to keep abreast of the latest research evidence and enable continuing professional education (24).
Not solely educational features will bridge the gap between evidence and practice. Other strategies are also needed. For example, a multidisciplinary local wound care committee, including those able to search and present relevant evidence, should coordinate the wound care policy within an institution or region. In addition, this may reduce the variability between professionals and institutions in the use of wound care materials (e.g. wound care materials used for the treatment of donor site wounds (25). Furthermore, opinion leaders and managers should be involved as they are important in improving and promoting evidence‐based care (26). Moreover, to improve the change of professional practice and implementation of evidence‐based recommendations, barriers should be identified and dealt with (27).
It is not only the task of the professionals to bridge the gap. Scientists should reach out and carry out reliable and relevant research and produce readable information (28). This is seldom the case; scientists pay relatively little attention to the implementation of the findings of their research in routine clinical care and usually use passive approaches to disseminate information (e.g. publication in professional articles). These approaches are generally ineffective, and at best, result only in small changes in practice (29). Hence, scientists and professionals should work together to investigate relevant clinical questions derived from daily practice. Finally, the awareness‐to‐adherence model which describes seven stages (awareness, acceptance, applicable, available and able, acted on, agreed to, and adherence) may help to get insight if the transfer between the different stages is insufficient 30, 31. If this is the case, specific interventions could be used to improve this. For example, electronic scanning and alert services may be useful to help stakeholders to become aware of important changes, such as the journal of Evidence‐based Medicine and Evidence‐based Nursing (31). Furthermore, stakeholders should act aptly in terms of internalising convincing evidence in their daily practice. In some cases, simple reminders help to act correctly (31). Finally, stakeholders should not forget the role of the patient. Patients are to be informed adequately on potential risks and benefits to improve their adherence to the wound protocol after discharge from hospital.
A limitation of this study is the small scope of the (Cochrane) systematic reviews we used for the assessment of awareness and usage of evidence. However, the wounds involved (possibly with the exception of burn wounds) reflect daily practice in wound care and may well be indicative of the situation for other indications. Second, it could be possible that stakeholders rarely turn to the Cochrane Library for answers to clinical dilemmas. Currently, an increasing number of medical schools and residency programmes are instituting curricula for teaching evidence‐based principles (32). Therefore, modern stakeholders in wound care should be aware of the available evidence in the Cochrane Library, but its use is not (yet) sufficiently implemented.
Third, we used a self‐reported questionnaire, which may have led to socially desirable answering and, subsequently, to an overestimation of Cochrane Library usage (33). Yet, this does not change the inferences from our study. Fourth, the questionnaire used is not validated. However, at present, there is no validated questionnaire available. We tried to obtain a first insight in this problem and to make the issue clear for future, more focused studies. Fifth, it is unclear whether the respondents answered reliably, that is, were they really aware of the evidence if they stated there is evidence of effect. Hence, we may even have overestimated their awareness. Lastly, the number of GP respondents in this study was limited, despite of our efforts to contact them. Therefore these results should be interpreted with caution. However, our results from GPs seem to be in accordance with two previous studies 18, 34. They found that despite the preferences of GPs for evidence‐based information (e.g. systematic reviews and randomised clinical trials) (34), the majority of respondents were unaware of, or did not use, the Cochrane Library 18, 34.
Present‐day reality is that producing systematic reviews with recommendations and disseminating the results does not naturally result in more awareness and use of the evidence in the Netherlands. Using wound care products while contradicting evidence is available endorses this statement. Although our results may not be surprising, it is important that the basic premise has been confirmed by a quantitative analysis to invoke improvement actions. The present availability of compelling research evidence and the positive attitude towards EBP 3, 17, 35, 36, 37 should make evidence‐based decision making in wound care possible.
ACKNOWLEDGEMENTS
We would like to thank all wound care stakeholders who completed the questionnaire. Their participation made this study possible. AME participated in the design of this study and drafted this article. MNS participated in the design of this study and was involved in drafting this article. DTU and HV were involved in designing of this study, and gave intellectual input on this article. They are the project leaders and have overall responsibility for this study. All authors have read and approved the final version of this article.
REFERENCES
- 1. Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Q 1998;76:517–63,509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grol R. Successes and failures in the implementation of evidence‐based guidelines for clinical practice. Med Care 2001;39:II46–54. [DOI] [PubMed] [Google Scholar]
- 3. Knops AM, Vermeulen H, Legemate DA, Ubbink DT. Attitudes, awareness, and barriers regarding evidence‐based surgery among surgeons and surgical nurses. World J Surg 2009;33:1348–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Thompson C. Clinical experience as evidence in evidence‐based practice. J Adv Nurs 2003;43: 230–7. [DOI] [PubMed] [Google Scholar]
- 5. Ubbink DT, Vermeulen H, Lubbers MJ. Local wound care: evidence‐based treatments and dressings. Ned Tijdschr Geneeskd 2006;150: 1165–72. [PubMed] [Google Scholar]
- 6. Vermeulen H, Westerbos SJ, Ubbink DT. Benefit and harm of iodine in wound care: a systematic review. J Hosp Infect 2010;76:191–9. [DOI] [PubMed] [Google Scholar]
- 7. Jull AB, Rodgers A, Walker N. Honey as a topical treatment for wounds. Cochrane Database Syst Rev 2008;4:CD005083. [DOI] [PubMed] [Google Scholar]
- 8. Vermeulen H, van Hattem JM, Storm‐Versloot MN, Ubbink DT. Topical silver for treating infected wounds. Cochrane Database Syst Rev 2007; 1:CD005486. [DOI] [PubMed] [Google Scholar]
- 9. Storm‐Versloot MN, Vos CG, Ubbink DT, Vermeulen H. Topical silver for preventing wound infection. Cochrane Database Syst Rev 2010;3: CD006478. [DOI] [PubMed] [Google Scholar]
- 10. O’Meara S, Al‐Kurdi D, Ologun Y, Ovington LG. Antibiotics and antiseptics for venous leg ulcers. Cochrane Database Syst Rev 2010;1:CD003557. [DOI] [PubMed] [Google Scholar]
- 11. Wasiak J, Cleland H, Campbell F. Dressings for superficial and partial thickness burns. Cochrane Database Syst Rev 2008;4:CD002106. [DOI] [PubMed] [Google Scholar]
- 12. Lee TH. Eulogy for a quality measure. N Engl J Med 2007;357:1175–7. [DOI] [PubMed] [Google Scholar]
- 13. Bell‐Syer S, Brady M, Bruce J, Cullum N, Foxlee R, Jull A, Margolis D, McInnes L, Nelson A, O’Meara S, Ubbink D. Letter: evidence‐based wound care in the UK: a response to David Leaper's editorial in International Wound Journal April 6 (2). Int Wound J 2009;6:306–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Leaper D. Evidence‐based wound care in the UK. Int Wound J 2009;6:89–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sigouin C, Jadad AR. Awareness of sources of peer‐reviewed research evidence on the internet. JAMA 2002;287:2867–9. [DOI] [PubMed] [Google Scholar]
- 16. Novak K, Miric D, Jurin A, Vukojevic K, Aljinovic J, Caric A, Marinovic GM, Poljicanin A, Kosta V, Rako D, Marusic A, Marusic M, Puljak L. Awareness and use of evidence‐based medicine databases and Cochrane Library among physicians in Croatia. Croat Med J 2010;51:157–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O’Donnell CA. Attitudes and knowledge of primary care professionals towards evidence‐based practice: a postal survey. J Eval Clin Pract 2004;10:197–205. [DOI] [PubMed] [Google Scholar]
- 18. Ram FSF, Wellington SR. General practicioners use of the Cochrane Library in London. Prim Care Resp 2002;11:123–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Adamsen L, Larsen K, Bjerregaard L, Madsen JK. Moving forward in a role as a researcher: the effect of a research method course on nurses' research activity. J Clin Nurs 2003;12:442–50. [DOI] [PubMed] [Google Scholar]
- 20. Perrier L, Mrklas K, Shepperd S, Dobbins M, McKibbon KA, Straus SE. Interventions encouraging the use of systematic reviews in clinical decision‐making: a systematic review. J Gen Intern Med 2011;26:419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Upton D. Attitudes towards, and knowledge of, clinical effectiveness in nurses, midwives, practice nurses and health visitors. J Adv Nurs 1999;29:885–93. [DOI] [PubMed] [Google Scholar]
- 22. Carrion M, Woods P, Norman I. Barriers to research utilisation among forensic mental health nurses. Int J Nurs Stud 2004;41:613–9. [DOI] [PubMed] [Google Scholar]
- 23. Straus SE, Green ML, Bell DS, Badgett R, Davis D, Gerrity M, Ortiz E, Shaneyfelt TM, Whelan C, Mangrulkar R. Evaluating the teaching of evidence based medicine: conceptual framework. BMJ 2004;329:1029–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee AG, Boldt HC, Golnik KC, Arnold AC, Oetting TA, Beaver HA, Olson RJ, Carter K. Using the journal club to teach and assess competence in practice‐based learning and improvement: a literature review and recommendation for implementation. Surv Ophthalmol 2005;50:542–8. [DOI] [PubMed] [Google Scholar]
- 25. Eskes AM, Gerbens LAA, Ubbink DT, Vermeulen H. Current treatment policies of donor site wounds after split‐skin grafting: a national survey. Ned Tijdschr Heelkd 2011;20:66–9. [Google Scholar]
- 26. Doumit G, Gattellari M, Grimshaw J, O’Brien MA. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2007;1:CD000125. [DOI] [PubMed] [Google Scholar]
- 27. Baker R, Camosso‐Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, Robertson N. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2010;3:CD005470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Straus S, Haynes RB. Managing evidence‐based knowledge: the need for reliable, relevant and readable resources. CMAJ 2009;180:942–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ 1998;317:465–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999;282:1458–65. [DOI] [PubMed] [Google Scholar]
- 31. Glasziou P, Haynes B. The paths from research to improved health outcomes. Evid Based Nurs 2005;8:36–8. [DOI] [PubMed] [Google Scholar]
- 32. Hatala R, Guyatt G. Evaluating the teaching of evidence‐based medicine. JAMA 2002;288: 1110–2. [DOI] [PubMed] [Google Scholar]
- 33. Adams AS, Soumerai SB, Lomas J, Ross‐Degnan D. Evidence of self‐report bias in assessing adherence to guidelines. Int J Qual Health Care 1999;11:187–92. [DOI] [PubMed] [Google Scholar]
- 34. Suter E, Verhoef M, O’Beirne M. Assessment of the information needs and use of information resources on complementary and alternative medicine by Alberta family physicians. Clin Invest Med 2004;27:312–5. [PubMed] [Google Scholar]
- 35. Chiu YW, Weng YH, Lo HL, Hsu CC, Shih YH, Kuo KN. Comparison of evidence‐based practice between physicians and nurses: a national survey of regional hospitals in Taiwan. J Contin Educ Health Prof 2010;30:132–8. [DOI] [PubMed] [Google Scholar]
- 36. Egerod I, Hansen GM. Evidence‐based practice among Danish cardiac nurses: a national survey. J Adv Nurs 2005;51:465–73. [DOI] [PubMed] [Google Scholar]
- 37. Ubbink DT, Vermeulen H, Knops AM, Legemate DA, Oude RK, Heineman MJ, Roos YB, Fijnvandraat CJ, Heymans HS, Simons R, Levi M. Implementation of evidence‐based practice: outside the box, throughout the hospital. Neth J Med 2011;69:87–94. [PubMed] [Google Scholar]


