Dear Editors,
Fournier's gangrene is a fast progressing, life‐threatening necrotizing infection, which is commonly seen in the dermis and subcutaneous layers of the anogenital region. The infection is usually caused by organisms that spread along the subcutaneous and fascial planes across the perineum, scrotum and often beyond these tissues. The usual treatment is a prompt surgical debridement and, in many cases, a diverting colostomy 1, 2. Here, we present a Fournier's gangrene case, where a combined treatment with the Flexi‐Seal Faecal Management System 1 and a negative pressure wound therapy (NPWT) were used to achieve optimal results.
Presented case was a 43‐year old, female patient, with a body mass index of 38. She was first seen in the emergency unit with a large wound in the gluteal region and high fever. She had been diabetic for at least 5 years. There was also a history of abdominal hernia operation. An extensive necrosis was noted between right gluteal region and labium major. The necrosis was continuing to the femoral canal. The subcutaneous tissues and the deep fascia were also involved. The proximity to anal canal was about 3 cm (Figure 1A). A giant ventral hernia was noted, although we were not sure if it was related to the present problem.
Figure 1.
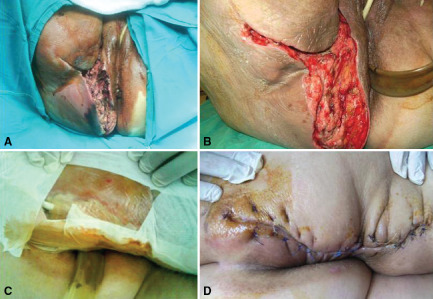
Wound progress over the course of time (refer to the text for explanation) (A) Presentation of Fournier's gangrene with perianal necrosisa. (B) Perineal region after extensive debridement and negative pressure therapy. (C) Combining Flexi‐Seal and negative pressure wound therapy in Fournier's gangrene. (D) Closure of wound region.
The clinical diagnosis of the wound was sepsis associated with Fournier's gangrene. An immediate surgical debridement was planned and performed. As medical treatment, ceftriaxone and metronidazole were used. At the end of the debridement, a Flexi‐Seal Faecal Management System was applied. This is a rectal tube allowing diversion of faecal matter from the rectum, aiming to decrease infectious load, and thus avoiding re‐infection (Figure 1B). A series of debridements was performed when necessary. At the end of the fourth debridement, no necrosis was seen. Then, to increase granulation tissue formation, NPWT was applied 2 (Figure 1C). This was continued for 28 days, with a dressing change every second day. The pressure was 60 mmHg, and continued with 5 min on and off intervals. At the end of the 28th day, the wound was ready to close with sufficient granulation formation (Figure 1D).
In the literature, there are few reported cases regarding the use of Flexi‐Seal Faecal Management System in Fournier's gangrene. Our approach differs from previous cases 3, 4, with the combination of Flexi‐Seal and NPWT, as presented here. This helped us to achieve faster wound healing.
The bacteria that cause the destructive infection in Fournier's gangrene syndrome are colonic in origin. Hence, faecal diversion using a colostomy has been a choice in the treatment of Fournier's gangrene with successful results. Flexi‐Seal is an alternative to colostomy with less complications 5.
NPWT is a leading wound management method, indicated by successful usage in almost every part of the human body. Recently, there are reports about its successful use in the wound management of Fournier's gangrene, in addition to conventional debridement. Once the necrosis is eliminated, NPWT helps to induce granulation tissue formation with the mechanisms of increased perfusion, fibroblast migration, remove of infected materials and excess exudates. The suggested pressure limits change between 50 and 125 mmHg. In critical areas such as in our case, the safe pressure would be better if maintained at the lower border. Hence, any complication such as perforation due to the high pressure is avoided 6.
The combined treatment with Flexi‐Seal Faecal Management System and NBWT in the management of Fournier's gangrene in this case seems promising. The advantages can be listed as: avoiding colostomy, rapid wound healing, shorter hospital stay, early return to work, and most importantly, contribution to survival.
Omer Faruk Ozkan, MD1, Ediz Altýnlý, MD2, Neset Koksal, MD3, Serkan Senger, MD4 & Atilla Celik, MD5
1Department of General Surgery, Faculty of Medicine, Çanakkale Onsekiz Mart University, Çanakale, Turkey
2Department of General Surgery, Faculty of Medicine, Bilim University, Istanbul, Turkey
3Department of General Surgery, Faculty of Medicine, Kafkas University, Kars, Turkey
4Department of General Surgery, Kartal State Hospital, Istanbul, Turkey
5Department of General Surgery, Bagcýlar Training and Research Hospital, Istanbul, Turkey
ozkanfomer@gmail.com
References
- 1. Bordes J. A non‐surgical device for faecal diversion in the management of perineal burns. Burns 2008;34:840–844. [DOI] [PubMed] [Google Scholar]
- 2. Desai KK, Hahn E, Pulikkottil B, Lee E. Negative pressure wound therapy: an algorithm. Clin Plast Surg 2012;39:311–324. [DOI] [PubMed] [Google Scholar]
- 3. Ohzeki T, Hayashi T, Hanai T, Uemura H. A case of Fournier's gangrene in which flexi‐seal was effective for evacuation management. Hinyokika Kiyo 2010;56:181–184. [PubMed] [Google Scholar]
- 4. Estrada O, Martinez I, Del Bas M, Salvans S, Hidalgo LA. Rectal diversion without colostomy in Fournier's gangrene. Tech Coloproctol 2009;13:157–159. [DOI] [PubMed] [Google Scholar]
- 5. Moorthy K, Rao PP, Supe AN. Necrotising perineal infection: a fatal outcome of ischiorectal fossa abscesses. J R Coll Surg Edinb 2000;45:281–284. [PubMed] [Google Scholar]
- 6. Silberstein J, Grabowski J, Parsons JK. Use of a vacuum‐assisted device for Fournier's gangrene: a new paradigm. Rev Urol 2008;10:76–80. [PMC free article] [PubMed] [Google Scholar]


