Abstract
Chronic wounds represent an aberrant biochemistry that creates a toxic proteolytic milieu which can be detrimental to the healing process. Rebalancing the wound microenvironment and addressing elevated protease activity (EPA) could therefore help facilitate healing. To understand how clinicians currently diagnose and manage excessive proteolytic activity, 183 survey responses from US wound specialists were collated and analysed to find out their perceptions on the role of proteases. The majority of respondents (>98%) believed proteases were important in wound healing and that a point‐of‐care (POC) protease test could be useful. This study yielded a low response rate (7·1%, n = 183); however, there were adequate data to draw significant conclusions. Specialists perceived that fibrin, slough, granulation tissue and rolled wound edges could indicate EPA. About 43% of respondents, however, failed to give a correct response when asked to review photographs to determine if excessive protease activity was present, and the perceived visual signs for EPA did not correlate with the wounds that had EPA; no statistical differences between professions were observed. Respondents chose debridement, wound cleansing and advanced therapies as important in reducing excessive protease activity. It was concluded that specialists have a need for POC diagnostic tests. On the basis of the responses to wound photos, it was determined that there were no visual cues clinicians could use in determining excessive protease activity. Additional research is recommended to evaluate the efficacy of a POC diagnostic test for protease activity and the treatments and therapies applied when EPA is found.
Keywords: Human neutrophil elastase, Matrix metalloproteases, Point‐of‐care diagnostic tests, Proteases, Serine proteases, Wound care
Introduction
Wound healing is a dynamic and complex biological process involving organised phases and includes coagulation, inflammation, epithelialisation, matrix deposition, angiogenesis, proliferation, cellular remodelling and wound contraction 1, 2. Complex interactions must occur between growth factors and proteinases, matrix components and cell types such as platelets, macrophages, fibroblasts and endothelial cells before each stage can complete and move sequentially onto the next (3). Together, these processes result in the restoration of tissue integrity and functional healing (4).
Review of the literature
It is well documented that there are many biochemical differences between acute and chronic wounds (5) and it is widely accepted that most acute wounds follow a well‐orchestrated sequence of events required for healing, typically without significant intervention within 2–4 weeks. However, chronic wounds become stalled in this process and are thought to be stuck in the inflammatory phase of healing, which can persist for months or even years (6). This has been shown by a number of clinical and in vitro studies 7, 8, 9. These studies have shown that chronic wounds contain elevated levels of inflammatory cytokines, protease activity and free radicals. The misregulation and imbalance of these biomarkers form a hostile environment, which is not conducive to wound healing 7, 8, 9 and leads to persistent chronicity by causing further wound damage and the degradation of growth factors required for tissue production 10, 11. For healing to occur, it is necessary to correct this environment; to target a therapy towards these wounds, it would be beneficial to establish which factors were creating the negative environment (Figure 1).
Figure 1.
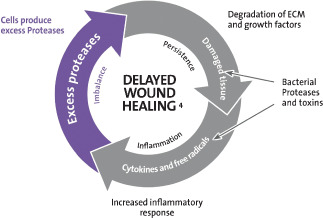
Cullen circle: a theoretical model to explain delayed wound healing (23).
A number of studies revealed that both the matrix metalloproteinases (MMPs) and serine proteases are elevated in chronic wounds. MMP 8, 9 and human neutrophil elastase, all of which are inflammatory derived proteases, have been shown to be the most predominant proteases in the chronic wound fluid 12, 13, 14. Proteases, predominantly MMPs and neutrophil‐derived elastase, play a critical role in each of these stages and are required for wound healing to occur 15, 16. They are highly regulated throughout the process of wound healing, and there must be a controlled balance between the level of proteases and protease inhibitors for wound healing to occur (17). Studies have shown that when elastase is in excess, a detrimental effect on wound healing can occur because of degradation of growth factors and fibronectin, a major component of the extracellular matrix 18, 19, 20. This elevated protease activity (EPA) is often coupled with a decrease in elastase inhibitors such as alpha‐1‐proteinase inhibitor and alpha‐2‐macroglobulin 19, 20. It is when this balance is upset in favour of protease‐induced degradation that a non‐healing wound occurs; in general, an imbalance in protease activity has been associated with many other chronic diseases, for example, metastatic tumours, rheumatoid arthritis and emphysema.
It is important to correct this underlying biochemistry if the wound is to progress to healing. One approach is to modify the wound environment by significantly reducing the harmful factors such as proteases, free radicals and excess metal ions while simultaneously protecting the positive factors such as matrix proteins and growth factors, leading to an overall increase in new tissue formation and progression towards healing (14). However, the biochemical imbalance in all chronic wounds is not always the same and this is why a variety of treatments and devices is required. For example, the presence of bacteria can exacerbate this problem and amplify an already hostile environment, eliciting more inflammation and producing virulence factors, such as bacterial proteases, which intensify the proteolytic milieu (21).
Stremitzer et al. (22) investigated a variety of specialists to assess their judgement of signs and symptoms relating to chronic wounds. Diabetic foot ulcers were described by 16 wound therapists (8 physicians and 8 nurses); granulation tissue, fibrin coverage, necrosis, size and depth of the lesion, wound exudate and wound edges were judged, and the therapeutic consequences were determined. Study data showed an extensive heterogeneity and a wide spread of results among all groups, unlike any other field of medical diagnostics. As the choice of treatment by a specialist is based on the assessment of the wound, it is possible that, in practice, this can lead to suboptimal therapy, prolonged treatment and patient morbidity (22).
A number of perceived signs and symptoms are presently being used to alert the clinician to chronic inflammation and potentially EPA. These include swelling, pain, colour, fibrin deposition and pebbled granulation tissue, to name but a few. However, to date, there have been no studies to substantiate these observations; at present, there are no validated visual cues that conclusively indicate the presence of EPA in the wound microenvironment (23). Clinicians are, therefore, relegated to decision‐making based on intuition; this often leads to inappropriate treatment choices and the use of advanced therapies as ‘last resorts'(24).
The international consensus on the role of proteases in wound diagnostics
The goal of this consensus was to explore the importance of EPA in wound healing and what the value of having a point‐of‐care (POC) diagnostic would be for use in clinical practice (23). Several markers identified that could potentially be used as the basis for a diagnostic test for non‐healing wounds. At present, proteases, specifically protease activities, have been identified as the best available marker for non‐healing wounds and these could provide useful information to the clinician about wound status and whether a particular treatment is appropriate or likely to improve clinical outcome. Therefore, EPA could be used as a predictive marker for non‐healing wounds and to determine if a patient is likely to respond to a protease‐modulating therapy.
Study design
To further investigate the current understanding of EPA and its relevance to clinical practice, a survey was sent to 2573 US wound specialists, with a range of disciplines and experience, to determine their attitudes and perceptions regarding the role of proteases in wound healing. The results are discussed and interpreted in this article. Questions included in the survey cover the importance, relevance, clinical significance and treatment choices for chronic wounds with EPA, to try and establish what the current understanding of EPA is for wound care specialists and its importance to them in clinical practice.
Methods
The aim of this research was to investigate attitudes and perceptions of clinicians surrounding proteases and wound healing. The method chosen for this research was a survey, and the selected research tool was a questionnaire. This research design represented a non‐experimental, descriptive, web‐based quantitative survey of self‐reported data of a large sample size using structured, and no disguised questions.
Survey process
In this study, some of the data were based on perception and some were objective to the extent that recall and self‐reporting were accurate. One assumption is that inaccuracies (errors in measurement) are randomly distributed. SurveyMonkey™ (SM) was used for purposes of capturing questionnaire data. SM is a US‐based company that enables users to create their own web‐based surveys.
A computer and Internet access were required for the participants who were given the following information:
Introductory and follow‐up letters;
A prompt to click on a website embedded in the letter to access SM.
A list of 13 multiple choice questions; some with multiple answers, and others asking the participants to put certain answers in order of preference.
Survey population
Wound management remains a multidisciplinary/ transdisciplinary endeavour. Therefore, it was reasonable to postulate that specialists in most acute care, office/clinic, rehabilitation facilities and long‐term care facilities could play a pivotal role in the care of patients with wounds and possess important didactic and clinical knowledge, leading to the collection of relevant data for this study. Specialists were, therefore, solicited from a large cross section of clinicians including physicians, podiatrists, nurses and physical therapists, among others.
Survey details
On 15 March 2011 and then again on 22 March 2011 (for the recipients who did not respond to the first round), participants were asked to fill out a 13‐part questionnaire about their attitudes and perceptions surrounding proteases and wound healing. The participants were contacted via e‐mail from a mailing list provided by the American Academy of Wound Management (AAWM) and prompted to proceed to SM to answer the questionnaires. SM is a website open to the public (www.surveymonkey.com) that anyone can subscribe to for the creation of surveys and statistical analysis if upgrades are purchased.
The AAWM is a voluntary, not‐for‐profit organisation established for the purpose of awarding credentials to interdisciplinary practitioners in the field of wound management. The AAWM offers three certifying examinations: Certified Wound Care Associate (CWCA) for those practitioners without a minimum of a Baccalaureate degree in a health‐related or physical science; Certified Wound Specialist (CWS) for those individuals with a minimum of a Baccalaureate degree and Certified Wound Specialist‐Physician (CWS‐P) for clinicians who have attained the MD, DO, DPM degree and have successfully passed the CWS examination. For purposes of this study, the researchers chose to focus on the CWS category as it was determined that this was the most prevalent, and clearly representative of the multidisciplinary approach to wound management.
The 2573 questionnaires were sent by e‐mail from a mailing list to US clinicians; 183 responses, 7·1% of the total, were received and analysed. Although the response rate was lower than expected, there were still sufficient numbers to perform meaningful statistical analysis.
Ethical considerations
No patients were required for this study. General and ethical approval was obtained from the Snyder Wound Research Institute, LLC, Tamarac, FL. Working with the investigators required that the participant answer questions regarding the way he/she thought about their attitudes and perceptions surrounding proteases and wound healing. As individual scores were not tallied, the analysis and interpretation of collected data did not in any way compromise the integrity of the individual. In the pre‐questionnaire letter to specialists, confidentiality was guaranteed.
Specialists certified by AAWM were aware that the organisation permits members to purchase and use their mailing list for educational purposes and participation is voluntary.
The hard copies of the questionnaire printed from SM were kept in a separate locked drawer that could only be accessed by the researcher. The electronic data were stored on a password protected computer that could only be accessed by the researcher.
Data analysis
Analysis of the data gleaned from this study used several statistical models:
Nominal cross tabulation
Ranking data
Pearson chi‐square
The Statistical Program for the Social Sciences (SPSS) version 17 aided in formulating the calculations, particularly of the raw data.
Subsequent to SM capturing results and collating the data in an easily readable chart format, these figures as well as the raw data were analysed using the SPSS.
Results
Respondent demographics
The results in 2, 3, 4 and Table 1 show the respondents, demographics. About 183 (out of 2573) US wound specialists who were surveyed responded.
Figure 2.
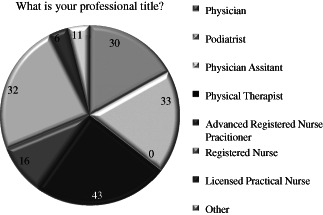
182 clinicians responded to this question.
Figure 3.
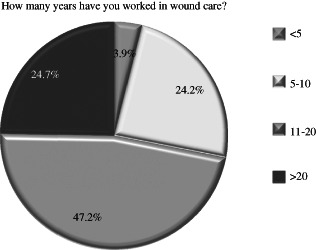
178 clinicians responded to this question.
Figure 4.
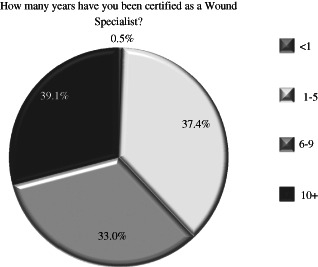
179 clinicians responded to this question.
Table 1.
177 clinicians responded to this question
| What is your professional title? Answer options | Response (%) |
|---|---|
| Physician | 16.5 |
| Podiatrist | 22.9 |
| Physician assistant | 0.0 |
| Physical therapist | 22.0 |
| Advanced registered nurse practitioner | 7.3 |
| Registered nurse | 24.8 |
| Licensed practical nurse | 3.7 |
| Other | 2.8 |
Clinical importance of proteases
5, 6, 7 support the key findings and agree with the conclusions of the International consensus on the role of proteases in wound diagnostics that EPA, and a diagnostic test for its detection, is of significant importance to clinicians. An overwhelming positive response was seen to these questions with over 97% of clinicians indicating that a POC diagnostic test for EPA would be beneficial.
Figure 5.
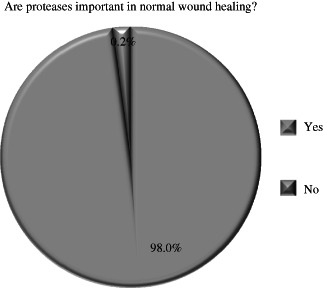
98% responded ‘yes’ to the question. 2% responded ‘no’.
Figure 6.
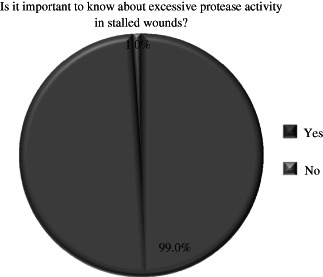
99% responded ‘yes’ to the question. 1% responded ‘no’.
Figure 7.
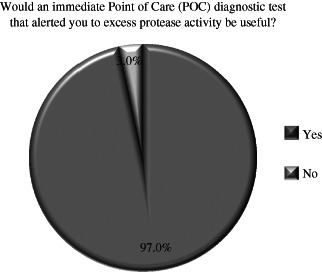
97% responded ‘yes’ to the question. 3% responded ‘no’.
Clinicians were asked why they thought proteases were important in wound healing and to rate which of their roles were most important. As can be seen from Figure 8, debridement, stimulation of growth factors and fibroblasts were scored highly as was fibrin removal, whereas epithelialisation was scored as the least important. As proteases have an important role in wound healing, clinicians were also asked to rate which of the inflammatory proteases most important to wound healing (Figure 9). In general, MMPs were most commonly rated as central to wound healing; however, human neutrophil elastase was also recognised to play a key role.
Figure 8.

Of the 178 clinicians that responded to this survey debridement was ranked first choice and stimulation of epithelialization was ranked as least important.
Figure 9.

167 clinicians responded to this question.
Perceived clinical signs of EPA
Currently, there are no diagnostic tests for the detection of EPA available in the USA. As 98% of clinicians responded that proteases are important to wound healing, they were asked, at present, which signs and symptoms they use as indicators of EPA. The results suggest that clinically there is no agreement of EPA (Figure 10). Although wound colour (57·7%) and fibrin (53·7%) were perceived as most important, rolled edges (39%), pebbled granulation tissue (38·4%) and swelling (32·8%) were also deemed important. Pain was considered the least important symptom in diagnosing EPA.
Figure 10.

177 clinicians responded to this question.
Because EPA ‘diagnosis’ is currently attempted through visual cues and clinical assessment, clinicians were asked to look at a series of wound pictures with limited clinical information and asked to determine if the wounds presented had EPA. Examples can be seen in Figure 11. A series of pictures were assessed but no conclusive agreement on EPA in these wounds shown was determined. About 43% of respondents failed to give a correct response when asked to review five photographs to determine if excessive protease activity was present. When asked why they chose a particular response, perceived visual cues were noted in a random pattern based on the wound type. A detailed review of the raw data showed that clinicians chose some symptoms (i.e. fibrin and rolled wound edges) to make decisions positively or negatively indicating that there were no clear reasons why clinicians thought EPA was present. In addition, there were no statistical differences between professions. Furthermore, there was an inverse relationship between experience and correct responses; those with <5 years of clinical experience and involved in the treatment of less wounds did better than those with more experience and greater patient contact.
Figure 11.

Photos for this study were supplied courtesy of Dr. Thomas Serena, MD, FACS.
Clinicians were asked to consider what techniques could be useful in managing EPA (Table 2). Clinicians were asked how they treated EPA in practice (Figure 12); debridement, cleansing and advance dressings followed by moist wound healing scored highly, whereas systemic drug therapies and negative pressure were less favoured.
Table 2.
Management of elevated protease activity
| Techniques that may reduce EPA |
|---|
| Cleansing |
| Debridement |
| Protease inactivators |
| Antiseptic dressings |
| Anti‐inflammatory |
| Dressing and devices that adsorb or remove exudates |
Figure 12.

Therapies were ranked, 1 being most important and 7 being the least important. Of the 177 clinicians that responded to this survey debridement, cleansing and advanced therapies were their top three choices.
Discussion
The survey conclusively showed the need to assess and determine EPA in wounds and that detecting EPA with a POC diagnostic test would be useful. Analysis further showed that knowing the protease activity status of a wound was important and could aid in treatment selection. These conclusions were supported by the literature; the International consensus on the role of proteases in wound diagnostics (23), for example, had previously discussed the significance of EPA within the clinical setting. Furthermore, this study showed that clinical signs and symptoms did not frequently correlate with the dynamics of the local wound microenvironment and often could not aid in providing appropriate treatments. This research supported the contention that there are no visual cues to detect EPA and coincided with research performed by Stremitzer et al. (22), among others, which suggested that diagnoses should not be based on visual impressions alone. Approximately 50% of clinicians surveyed failed to recognise wounds with EPA. The results were equivalent to flipping a coin and therefore based on chance. Although there is no evidence in the current literature validating any symptom/symptoms that would be indicative of EPA; treatments have been validated and are well known to the medical/wound care community (14). The majority believed that the appropriate treatment to help control protease activity should be administered locally/topically, with debridement, cleansing and advanced dressings.
The variation in response to the symptoms thought to indicate EPA, and the fact that 98% of clinicians believed that proteases were important in normal wound healing, could explain why clinicians indicated that a POC diagnostic test could be helpful. A detailed review of the raw data showed that clinicians chose some symptoms (i.e. fibrin and rolled wound edges) to make decisions positively or negatively, indicating that there were no clear reasons why clinicians thought EPA was present. Pebbled granulation, usually associated with healthy tissue, was chosen by 39% of respondents as a marker for EPA. Additionally, swelling and pain, usually associated with inflammation or infection, were viewed as least important; these statements appeared incongruous to what one would ‘expect’ and further supported the hypothesis concerning the absence of visual cues.
There was an inverse relationship between experience and correct responses; those with <5 years of clinical experience and involved in the treatment of less wounds did better than those with more experience and greater patient contact; this could have occurred because of over‐confidence in recognising perceived visual cues by the more experienced specialists or because of less exposure to newer theories and wound management techniques.
Limitations of the study
All goals and endpoints of this study were accomplished. However, the response rate of 7·1% was comparatively low based on the numbers of specialists polled; non‐response bias is a possibility as the specialists who returned the questionnaires may have been more interested in the subjects posed than those who did not respond. A lower than expected response rate could cause sample bias or loss of power (25). The reasons for a low response rate could stem from lack of incentives and concerns about anonymity as well as unfamiliarity with the material. In addition, potential respondents may have perceived some terms used in the questionnaire as potentially confusing or ambiguous (25). Despite this, however, a sufficient number of responses were received (n = 183) in order to perform analysis and show statistically significant differences, when present. In addition, the data collected for many of the questions appeared very distinct, which would suggest that among these respondents, a common opinion was strongly held. Finally, the survey asked respondents to give their impressions of EPA by reviewing five photos; increasing the number of photos could have potentially gleaned more generalisable results.
Conclusion
Many clinical and in vitro studies support the premise that chronic wounds contain a hostile and aberrant biochemistry, causing these wounds to be stuck in the inflammatory phase of wound healing. This biochemical imbalance is, in part, due to excessive MMP and serine proteases, specifically human‐neutrophil‐derived elastase activity; left unchecked, these enzymes can destroy the entire extracellular matrix. This survey confirmed clinicians' perceptions of the importance of proteases in wound healing. The link between the biochemical environment and treatment was also perceived to be essential. About 97% of respondents agreed that POC diagnostic tests to evaluate protease activity could be useful in diagnosing and treating chronic wound in a timely and efficient manner.
There was no agreement on common signs and symptoms of EPA; in fact, respondents used the same symptoms to evaluate both the absence and the presence of EPA; this supports the premise that there are no visual cues to detect EPA.
The study concluded that treatment of suspected EPA was mainly topical with debridement, cleaning and advanced dressings.
No statistical differences were found between the professional groups surveyed. Additional research is recommended to evaluate the efficacy of a POC diagnostic test for protease activity and the treatments and therapies applied when EPA is found. While a POC test for detecting EPA is available in Europe, there is currently no test available in the USA. However, it is expected that in the future, many diagnostic tests will be available to help determine the underlying defects resulting in non‐healing wounds. These will help clinicians make more informed decisions about treatment choices and help heal wounds more effectively and efficiently by targeting therapies early in the treatment regime.
References
- 1. Clark R. Cutaneous tissue repair: basic biological considerations. J Am Acad Dermatol 1985;13:701–25. [DOI] [PubMed] [Google Scholar]
- 2. Mast BA, Schultz GS. Interactions of cytokines, growth factors, and proteases in acute and chronic wounds. Wound Repair Regen 1996;4: 411–20. [DOI] [PubMed] [Google Scholar]
- 3. Nwomeh BCM, Yager DR, Cohen IK. Physiology of the chronic wound. Clin Plast Surg 1998;25:341. [PubMed] [Google Scholar]
- 4. Hackam DJ, Ford HR. Cellular, biochemical and clinical aspects of wound healing. Surg Infect 2002;3:S23–35. [DOI] [PubMed] [Google Scholar]
- 5. Tarnuzzer RW, Schultz GS. Biochemical analysis of acute and chronic wound environments. Wound Repair Regen 2002;4:321–25. [DOI] [PubMed] [Google Scholar]
- 6. Falanga V, Grinnell F, Gilchrest B, Maddox YT, Moshell A. Workshop on the pathogenesis of chronic wounds. J Invest Dermatol 1994; 102:125–27. [DOI] [PubMed] [Google Scholar]
- 7. Harris IR, Yee KC, Walters CE, Cunliffe WJ, Kearney JN, Wood EJ, Ingham E. Cytokine and protease levels in healing and non‐healing chronic venous leg ulcers. Exp Dermatol 1995;4:342–9. [DOI] [PubMed] [Google Scholar]
- 8. Salim AS. The role of oxygen‐derived free radicals in the management of venous (varicose) ulceration: a new approach. World J Surg 1991;15:264–9. [DOI] [PubMed] [Google Scholar]
- 9. Wysocki AB, Staiano‐Coico L, Grinnell F. Wound fluid from chronic leg ulcers contains elevated levels of metalloproteinase's MMP‐2 and MMP‐9. J Invest Dermatol 1993;101:64–8. [DOI] [PubMed] [Google Scholar]
- 10. Grinnell F, Zhu M. Fibronectin degradation in chronic wounds depends on relative levels of elastase, α1 proteinase inhibitor and α2 macroglobulin. J Invest Dermatol 1996;106:335–41. [DOI] [PubMed] [Google Scholar]
- 11. Yager DR, Chen SM, Ward SI, Olutoye OO, Diegelmann RF, Cohen IK. Ability of chronic wound fluids to degrade peptide growth factors is associated with increased levels of elastase activity and diminished levels of proteinase inhibitors. Wound Repair Regen 1997;5:23–32. [DOI] [PubMed] [Google Scholar]
- 12. Nwomeh BC, Liang H‐X, Cohen KI, Yager DR. MMP8 is the predominate collagenase in healing wounds and non‐healing ulcers. J Surg Res 1999;81:189–95. [DOI] [PubMed] [Google Scholar]
- 13. Rayment EA, Upton Z, Shooter GK. Increased matrix metalloproteinase‐9 (MMP‐9) activity observed in chronic wound fluid is related to the clinical severity of the ulcer. Br J Dermatol 2008;158: 951–61. [DOI] [PubMed] [Google Scholar]
- 14. Cullen B, Smith R, McCulloch E, Silcock D, Morrison L. Mechanism of action of PROMOGRAN, a protease modulating matrix for treatment of diabetic foot ulcers. Wound Repair Regen 2002;10:16–25. [DOI] [PubMed] [Google Scholar]
- 15. Kyriakides TR, Wulsin D, Skokos EA, Fleckman P, Pirrone A, Shipley JM, Senior RM, Bornstein. Mice that lack matrix metalloproteinase‐9 display delayed wound healing associated with delayed reepithelization and disordered collagen fibrillogenesis. Matrix Biol 2009;28:65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cole AM, Shi J, Ceccarelli A, Kim YH, Park A, Ganz T. Inhibition of neurophil elastase prevents cathelicidin activation and impairs clearance of bacteria from wounds. Blood 2001;97:297–304. [DOI] [PubMed] [Google Scholar]
- 17. Singer AJ, Clark RAF. Cutaneous wound healing. New Engl J Med 1999;10:738–46. [DOI] [PubMed] [Google Scholar]
- 18. Herrick S, Ashcroft G, Ireland G, Horan M, McCollum C, Ferguson M. Up‐regulation of elastase in acute wounds of healthy aged humans and chronic venous leg ulcers are associated with matrix degradation. Lab Invest 1997;77:281–8. [PubMed] [Google Scholar]
- 19. Chen SM, Ward SI, Olutoye OO, Diegelmann RF, Kelman Cohen I. Ability of chronic wound fluids to degrade peptide growth factors is associated with increased levels of elastase activity and diminished levels of proteinase inhibitors. Wound Repair Regen 1997;5:23–32. [DOI] [PubMed] [Google Scholar]
- 20. Grinnell F, Zhu M. Fibronectin degradation in chronic wounds depends on the relative levels of elastase, alpha1‐proteinase inhibitor and alpha2‐macroglobulin. Invest Dermatol 1996;106:335–41. [DOI] [PubMed] [Google Scholar]
- 21. Davies CE, Wilson MJ, Hill KE, Stephens P, Hill CM, Harding KG, Thomas DW. Use of molecular techniques to study microbial diversity in the skin. Chronic wounds re‐evaluated. Wound Repair Regen 2001;9:332–40. [DOI] [PubMed] [Google Scholar]
- 22. Stremitzer S, Wild T, Hoelzenbein T. How precise is the evaluation of chronic wounds by health care professionals? Int Wound J 2007;4:156–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. The role of proteases in wound diagnostics. International consensus. 2011. Wounds International.
- 24. Snyder R, Cullen B. Point of care diagnostic tests in wound management: targeted therapy for excessive protease activity the first frontier. Wound care and hyperbaric medicine. 2011;2:54–61. [Google Scholar]
- 25. Sivo SA, Saunders C, Chang Q. How low should you go? Low response rates and the validity of inference in IS questionnaire research. J Assoc Inf Syst 2006;7:6. [Google Scholar]


