Abstract
Epidermolysis bullosa (EB) is a progressive familial disorder composed of dermal mucosal blisters, flexion contractures and pseudosyndactylies. Flexion contractures and pseudosyndactyly can be treated with surgery but usually require skin grafting. Because of poor wound healing, skin graft harvesting is a challenge in these patients. In order to prevent donor‐site morbidities due to skin graft harvesting some alloplastic materials were introduced. In this study, we focused on Suprathel® as a new allograft material for covering the skin defects of a patient with dystrophic EB.
Keywords: Epidermolysis bullosa, Hand deformity, Pseudosyndactyly
Introduction
Epidermolysis bullosa (EB) is a group of inherited diseases characterised with blister formation as a result of minor trauma. The size of the blisters is variable and may occur either on cutaneous surfaces or mucosal tracts. The depth of involvement, the layer of the blister formation and the severity of the disease varies among EB types 1.
Although more than 23 subtypes have been documented, there are three major groups of EB such as simplex, junctional and dystrophica 2. This classification is based on the level of cleavage plane of the blisters 1. EB simplex is caused by the mutations in the genes that encode keratins 5 and 14. Junctional EB is related to the mutations in the genes encoding laminin or type 17 collagen and dystrophic EB is related to the mutation in the gene encoding type 7 collagen 3. Diagnosis starts with taking patient history and physical examination 4. Biopsy taken from fresh blisters for electron microscopy and immunofluorescence antigenic mapping is helpful in making the diagnosis 1.
Patients with recessive dystrophic EB typically exhibit extensive scarring and mutilation with an early age at onset. A multi‐disciplinary team programme should be included in the management of the patients 5. Therapy includes preventing blistering; estimating protein, vitamin, mineral and energy requirements; treatment for chronic wounds; and preventing development of squamous cell carcinoma 6.
Hand deformities in EB are a critical problem. Epidermal degloving, pseudosyndactyly, nail problems, flexion contractures at interphalangial (IP) and metacarpophalangeal (MCP) joints, adduction contracture at first MCP joint, ‘mitten‐like’ deformity, osteoporosis of hand bones, subluxations at IP and MCP joints, ankylosis of the proximal interphalangeal (PIP) joints, cystic deformities of the distal radius and ulna can be observed. The major debilitating extracutaneous complication of inherited EB is development of pseudosyndactyly 7.
This study focused on the treatment for hand deformities in a 14‐year‐old boy with advanced hand pathologies. We report our experience with a new improved skin substitute, Suprathel® (PolyMedics Innovations GmbH, Denkendorf, Germany), and its use in EB patients.
Case report
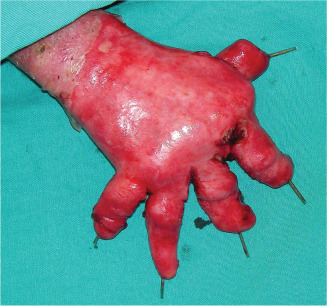
A 14‐year‐old boy with dystrophic EB was admitted with flexion contractures of all fingers, adduction contracture of thumb, pseudosyndactyly, mitten‐like deformity and blisters on both his hands (Figure 1). It was his first admission for surgery. The mitten‐like deformity was also localised on both his feet. Hand deformities were evaluated by the rehabilitation unit and possible postoperative exercises were decided.
Figure 1.

Preoperative photo of the patient.
The patient also had iron‐deficiency anaemia and protein malnutrition. Iron, zinc, selenium and calcium supplements were given to the patient immediately. He was unable to eat solids because of intraoral blisters and pain. As he was able to eat soft foods, caloric and protein support with fluid nutrition products were given.
When considering wound healing, a number of factors that influence the healing process were addressed. Primarily, skin damage is reduced by removing possible sources of friction, trauma or padding. His family was informed about these issues and his nutritional status was optimised.
In order to prevent infection, mupirocin dressings were used and the wounds were covered with non‐adherent dressings. The blisters were punctured with a sterile needle. The patient was also evaluated by a dermatologist for skin care.
The patient was operated under general anaesthesia. Antisepsis was maintained with povidone‐iodine without rubbing; 3/0 nylon loop sutures were placed through the terminal segments of the digits to act as digital retractors. This minimised handling of skin but allowed excellent exposure. The epidermis of the hand was completely removed (degloving). After the glistening dermis was exposed, closed capsulotomies of the PIP, DIP and MCP joints were performed. Kirschner wires were used to maintain the extension of the fingers (Figure 2). In order to avoid skin graft healing problems at the donor site, a new product, Suprathel®, was applied as an allograft for covering the glistening dermis. The allograft was not attached to the dermis with sutures. Vaseline gauze was used to separate the web spaces and to cover the allograft. Then saline‐soaked gauze was used around the digits, hand and forearm to provide moisture to the wound healing environment and the non‐adherent dressing. Once all surfaces were covered with saline‐soaked dressings, sterile cotton was used to make a boxing glove‐type dressing. A volar splint was then applied to maintain wrist dorsiflexion, MCP and IP joint extension and thumb abduction.
Figure 2.
Intraoperative photo of the hand.
The first dressing change was performed under sedation and anaesthesia 1 week after surgery. Epithelialisation islands on the fingers and dorsum of the hand were observed. Suprathel® remnants were not removed. Both the hands were washed with temperate saline. Vaseline gauze was used to cover all the surface of the hands. Saline‐soaked gauze was placed on the web spaces and over the vaseline gauze. The web spaces were separated by wet sterile cotton. The hands were then covered with cotton bandage and thermoplastic volar splint was applied. Thermoplastic splint is of light weight with low friction surface and has memory allowing easy adjustment. Second dressing was performed 1 week after the first one. The redressing was performed in the same manner. Kirschner wires were removed. Epithelialisation was complete on both hands except a small (1 × 2 cm2) de‐epithelialised region on the dorsum of the hand (Figure 3A and B). At the end of the second week, range of motion exercises was performed under the direction of hand occupational therapist.
Figure 3.
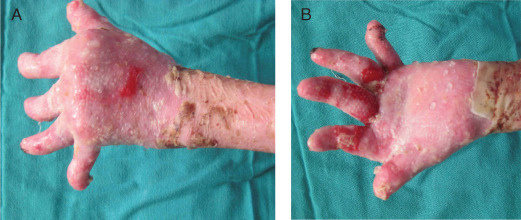
(A) and (B) Postoperative 2‐week view of the hands.
Discussion
EB patients with hand deformities face serious impact on psychomotor and social development, social isolation and overall a poor quality of life. Therefore, hand surgery should be performed to alleviate their condition. Surgical approaches vary with severity of involvement. The treatment for hand deformity is composed of a three‐step approach in the literature: degloving, closed capsulotomy and covering of the wound with autologous or synthetic materials 6, 8.
The treatment for hand deformities in dystrophic EB patients with allogeneic products was previously reported by Jinnah et al. They used tissue‐engineered skin in their study 9. This treatment uses a live, bilayered skin and is equivalent to the treatment for ulcers caused by diabetes and venous insufficiency 3. But the wound healed only after 6–18 weeks which was a very long time 10. Dermagraft® is a living dermal skin product made of human dermal fibroblasts applied to recessive dystrophic EB patients and provided complete epidermal coverage after 8 weeks of treatment 11. Composite cultured skin (CCS) has been used in the treatment for donor sites and mitten‐like deformities in EB, but clinical trials are still going on 12. Also amniotic membrane grafts, epidermal keratinocyte grafts and different splints have been used in the treatment for EB with hand deformities 9, 13, 14, 15, 16, 17.
Suprathel® is a synthetic copolymer composed of DL‐lactide (>70%) and ε‐caprolactone. It is non‐toxic, water‐vapour permeable to prevent maceration, non‐adherent and biocompatible. It has been used for toxic epidermal necrolysis, Stevens‐Johnson syndrome and burn victims to cover the skin. In both study groups, it reduced the pain and was easily handled than other materials. Also, it adhered rapidly and protected the wound from infections 18, 19.
To the best of our knowledge, this is the first report to show that Suprathel® treatment in EB results in faster wound healing. The advantages of this therapy are easy and quick application, absence of donor‐site morbidity, sutureless adaptation, quick epithelialisation that started at 1 week and closed at 2 weeks (such that the rehabilitation can start early), lower cost than other synthetic materials used for this purpose, easy availability, and can be used anywhere in the body. Also, its elastic property allows usage in indented areas such as fingers.
Hand therapy and postoperative splinting are very important in the treatment for EB. Aggressive splinting with web protection was performed and early occupational therapy was provided under the direction of the same hand therapist. It should be noted that web‐space protecting gloves and exercises must be continued for lifetime to prevent recurrence of mitten‐like deformity 20.
In this study we treated a patient with dystrophic EB for untreated mitten‐like and serious hand deformities. We used Suprathel® for covering both hands until the epithelialisation could begin. If quick epithelialisation is required in patients with donor‐site problems, this product is very beneficial.
Acknowledgements
The authors have no conflict of interest to declare, sources of support and disclosure of funding received for this work from any of the organisations.
References
- 1. Marinkovich MP, Bauer EA. Inherited epidermolysis bullosa. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's dermatology in general medicine, 6th edn. New York: McGraw‐Hill, 2008:505–16. [Google Scholar]
- 2. Fine J‐D, Eady RA, Bauer EA, Briggaman RA, Bruckner‐Tuderman L, Christiano A, Heagerty A, Hintner H, Jonkman MF, McGrath J, McGuire J, Moshell A, Shimizu H, Tadini G, Uitto J. Revised classification system for inherited epidermolysis bullosa: report of the Second International Consensus Meeting on diagnosis and classification of epidermolysis bullosa. J Am Acad Dermatol 2000;42:1051–66. [PubMed] [Google Scholar]
- 3. Bello YM, Falabella AF, Schachner CA. Management of epidermolysis bullosa in infants and children. Clin Dermatol 2003;21:278–82. [DOI] [PubMed] [Google Scholar]
- 4. Marinkovich MP. Update on inherited bullous dermatoses. Dermatol Clin 1999;17:473–85. [DOI] [PubMed] [Google Scholar]
- 5. Oliveira TM, Sakai VT, Canido LA, Silva SM, Machado MA. Clinical management for epidermolysis bullosa dystrophica. J Appl Oral Sci 2008;16:81–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fivenson DP, Scherschun L, Cohen LV. Apligraf in the treatment of severe mitten deformity associated with recessive dystrophic epidermolysis bullosa. Plast Reconstr Surg 2003;112:584–8. [DOI] [PubMed] [Google Scholar]
- 7. Fine JD, Johnson LB, Weiner M, Stein A, Cash S, Deleoz J, Devries DT, Suchindran C. Pseudosyndactyly and musculoskeletal contractures in inherited epidermolysis bullosa: experience of the national epidermolysis bullosa registry, 1986‐2002. J Hand Surg [Br] 2005;30:14–22. [DOI] [PubMed] [Google Scholar]
- 8. Cavallo AV, Smith PJ. Surgical treatment of dystrophic epidermolysis bullosa of the hand. Tech Hand Up Extrem Surg 1998;2:184–95. [DOI] [PubMed] [Google Scholar]
- 9. Phillips J, Rockwell WB. Surgical treatment of recessive dystrophic epidermolysis bullosa in the hand: use of tissue‐engineered skin (Apligraf). Ann Plast Surg 2003;50:441–2. [DOI] [PubMed] [Google Scholar]
- 10. Falabella AF, Valencia IC, Eaglestein W, Schachner LA. Tissue‐engineered skin (Apligraf) in the healing of patients with epidermolysis bullosa wounds. Can J Plast Surg 2002;10:27–30. [DOI] [PubMed] [Google Scholar]
- 11. Williamson D, Coutts P, Sibbald RG. The role of dermal skin substitutes in the management of hard to heal unusual wounds. Can J Plast Surg 2002;10:27–30. [Google Scholar]
- 12. Eisenberg M, Llewelyn D. Surgical management of hands in children with recessive dystrophic epidermolysis bullosa: use of allogeneic composite cultured skin grafts. Br J Plast Surg 1998;51:608–13. [DOI] [PubMed] [Google Scholar]
- 13. Glicenstein J, Mariani D, Haddad R. The hand in recessive dystrophic epidermolysis bullosa. Hand Clin 2000;16:637. [PubMed] [Google Scholar]
- 14. Mullett F. A review of the management of the hand in dystrophic epidermolysis bullosa. J Hand Ther 1998;11:261. [DOI] [PubMed] [Google Scholar]
- 15. Witt PD, Chang CJ, Mallory SB, Lind AC. Surgical treatment of pseudosyndactyly of the hand in epidermolysis bullosa: Histological analysis of an acellular allograft dermal matrix. Ann Plast Surg 1999;43:379. [DOI] [PubMed] [Google Scholar]
- 16. Pajardi G, Pivato G, Rafanelli G. Rehabilitation in recessive dystrophic epidermolysis bullosa. Tech Hand Up Extrem Surg 2001. Sep;5:173–7. [DOI] [PubMed] [Google Scholar]
- 17. Eisenberg M, Llewelyn D. Surgical management of hands in children with recessive dystrophic epidermolysis bullosa: use of allogeneic composite cultured skin grafts. Br J Plast Surg 1998;51:608–13. [DOI] [PubMed] [Google Scholar]
- 18. Pfurtscheller K, Zobel G, Roedl S, Trop M. Use of Suprathel dressing in a young infant with TEN. Pediatr Dermatol 2008;25:541–3. [DOI] [PubMed] [Google Scholar]
- 19. Uhlig C, Rapp M, Hartmann B, Hierlemann H, Planck H, Dittel KK. Suprathel‐an innovative resorbable skin substitute for the treatment of burn victims. Burns 2007;33:221–9. [DOI] [PubMed] [Google Scholar]
- 20. Ladd AL, Eggleston JM. Hand management for patients with epidermolysis bullosa. In: Mathes SJ, Hentz VR, editors. Plastic surgery, 2nd edn. Philadelphia: Saunders Elsevier, 2006:431–7. [Google Scholar]


