Abstract
Extensive volar injuries are common and devastating because of the long‐term adhesion potency. The gliding effect of the adipose tissue is essential in preventing tendon adhesions after injury. In this study, we present the results of performing adipofascial flaps for the reconstruction of soft tissue defects following wrist trauma. The study included 15 patients. Adipofascial flaps were performed for immediate coverage of the tissue defect in 2 patients and for late adhesion‐related problems in 13 patients. Flap dimensions varied from 8 × 14 to 8 × 20 cm. All but one of the flaps and skin grafts survived uneventfully. None of the patients, whether immediate or late, required another operation to address further adhesion problems. Since adipofascial flaps provide a gliding surface, they are a good choice for immediate coverage of soft tissue defects in the wrist that are not suitable for skin grafting alone as well as for late adhesion‐related problems.
Keywords: Adipofascial flap, Soft tissue defect, Tendon adhesion, Wrist
Introduction
Both the hand and the wrist are important for being able to perform daily activities independently. However, while the hand is the most active part of the upper limb, it is also the least protected (1). Extensive volar injuries are common and devastating because of long‐term adhesion potency. Tendon injuries in the wrist may start to adhere to the overlying skin and fascia, and these adhesions inevitably produce functional disability 2, 3. Reconstruction of wrist defects is challenging because, in order to prevent adhesions, it requires thin and elastic soft tissue coverage with a dependable vascular supply to provide a gliding surface for the tendinous structures.
The gliding effect of the adipose tissue is essential for preventing tendon adhesions after injury 4, 5. Since adipofascial flaps provide a gliding surface, they are a good choice for coverage of soft tissue defects in the wrist that are not suitable for skin grafting alone. The flaps are particularly useful for localised soft tissue defects with denuded tendons, nerves or vascular structures. Therefore, in this study, we present the results of adipofascial flaps for both immediate and late reconstruction of soft tissue defects following wrist trauma.
Materials and methods
Between 2007 and 2010, adipofascial turnover flaps were performed either immediately or for late adhesion‐related problems in 15 patients (12 males and 3 females) who had extensive volar soft tissue defects in their wrists (Table 1). The causes of these injuries included sharp lacerations (eight patients), traffic accidents (five patients) and gunshot wounds (two patients). The location of injuries ranged from the distal wrist crease to the flexor musculotendinous junction (zone 5). Adipofascial flaps were performed for immediate coverage of the tissue defect in 2 patients (Figure 1) and for late adhesion‐related problems in 13 patients (Figure 2).
Table 1.
Patient demographics
| No. | Age/sex | Etiology | Timing of the treatment | Follow‐up period (months) |
|---|---|---|---|---|
| 1 | 34/Male | Gunshot | Immediate | 19 |
| 2 | 23/Male | Sharp laceration | Late | 16 |
| 3 | 43/Male | Sharp laceration | Late | 14 |
| 4 | 18/Female | Sharp laceration | Late | 13 |
| 5 | 30/Male | Traffic accident | Late | 22 |
| 6 | 21/Male | Sharp laceration | Immediate | 16 |
| 7 | 35/Male | Sharp laceration | Late | 14 |
| 8 * | 12/Male | Sharp laceration | Late | 19 |
| 9 | 41/Male | Gunshot | Late | 16 |
| 10 | 36/Female | Traffic accident | Late | 19 |
| 11 | 23/Male | Sharp laceration | Late | 13 |
| 12 | 39/Female | Traffic accident | Late | 14 |
| 13 | 41/Male | Traffic accident | Late | 14 |
| 14 | 32/Male | Traffic accident | Late | 19 |
| 15 | 27/Male | Sharp laceration | Late | 13 |
*The patient had partial flap necrosis.
Figure 1.

(A) A 34‐year‐old male patient with a gunshot wound in the volar wrist area. (B) Immediate coverage of the defect with an adipofascial turn overflap. (C) Full recovery of the hand function after 9 months of follow‐up.
Figure 2.
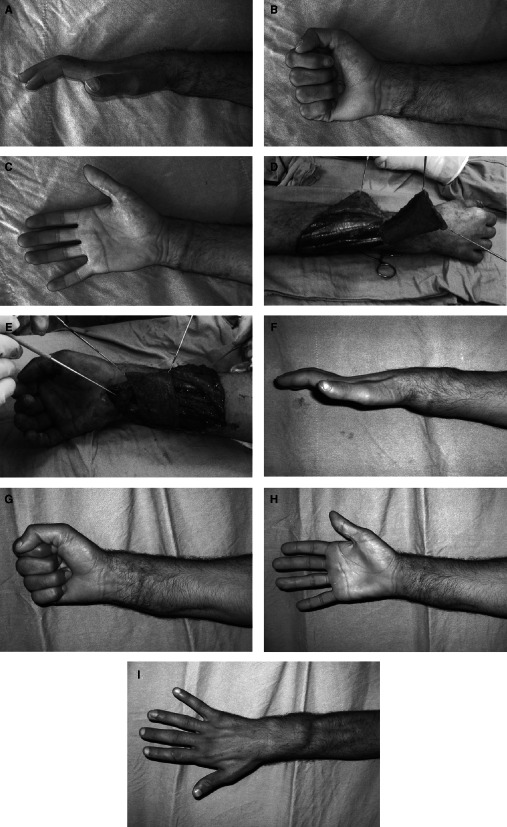
(A) A 27‐year‐old male patient who had been previously operated for sharp laceration injury of the wrist had flexor tendon adhesion. Preoperative lateral view of the hand. (B) Preoperative limitation of the fist closure. (C) Preoperative volar view of the same hand. (D) After the adipofascial flap was harvested. (E) Flexor tendons at the volar wrist area were covered with the adipofascial flap. (F) Lateral view at the postoperative sixth month. (G) Patient satisfied with the fist closure at the postoperative sixth month. (H) Volar view at the postoperative sixth month. (I) Donor site morbidity is minimal.
Operative technique
Vascular pedicle dissection is not mandatory for flap harvesting. However, we used a handheld Doppler flow meter to detect the distal cutaneofascial arterial perforators, and the flaps were designed to preserve some of these perforators. The adipofascial flap was raised by means of a lazy‐S incision made proximal to the defect area. The skin was then incised proximal to the defect or adhesion area, and dissection was initiated from the subdermal layer, just superficial to the dorsal veins. Some of the subcutaneous fat attached to the dermis of the elevated skin flaps was left, in order to preserve flap perfusion. The large veins at the proximal edge of the dissection were either ligated or coagulated, and the subcutaneous nerves were preserved. The adipofascial flap was then dissected over the muscular fascia through the proximal edge of the defect. An adequate amount of space was left between the proximal edge of the defect and the pedicle of the flap to preserve the previously detected cutaneofascial arterial perforators. Once the adipofascial flap had been turned over distally, to cover the defect, it was sutured in place using an absorbable suture material, with no tension. After the donor site had been closed, either full or split‐thickness skin graft was placed over the adipofascial flap.
Hand physiotherapy
Physiotherapy was provided for the patients using a combination of modified Duran and modified Kleinert protocols (6). Patients' hands were placed in dorsal splints, with the wrist in 30° of palmar flexion and the metacarpophalangeal joints in 50–60° of flexion. The interphalangeal joints were allowed to complete active extension. Controlled passive mobilisation was allowed after the third day following the operation. The patients were instructed to extend the involved digit, or digits, actively against the tension of the rubber band ten times every hour. They were also given a passive exercise program to follow four times a day for all digits including those that were not involved. A hand therapist saw all of the patients once a week during the first month, once every 2 weeks for the second and third months and once a month after that.
Results
The mean follow‐up period was 16 (13–22) months. The mean age was 30 (12–43) years. Flap dimensions varied from 8 × 14 to 8 × 20 cm. All but one of the flaps and skin grafts survived uneventfully. Partial flap necrosis occurred in one patient (6%). No other complications, such as haematoma or infection, were observed. None of the patients, whether immediate or late, required another operation to address further adhesion problems. The long‐term aesthetic and functional results were satisfactory, and the patients expressed a high degree of satisfaction.
Discussion
Complex wounds in the wrist have unique reconstructive challenges. Beyond the consideration for soft tissue coverage, surgeons must recognise the complex functional concerns that are relevant to the zone of injury and strive to include these priorities in the operative plan. Both the hand and the wrist are vulnerable to extensive trauma in which tendons, vascular structures, nerves and bones are easily destroyed and exposed.
The most common complication after surgical repair of tendon injuries is the formation of adhesions. Several methods have been proposed to reduce adhesion formation in order to improve functional outcomes 7, 8. Atraumatic handling of the tissue during the operation and physiotherapy performed on the hand in the early postoperative period are crucial in order to avoid adhesion formation (9). Even when these requirements are met, however, tendon injuries in the wrist may adhere to the overlying skin and fascia (3).
Free flaps or pedicled fascial flaps provide an excellent reconstructive option in cases of exposed tendon, joint or bone where soft tissue coverage is needed 10, 11. Both pedicled and free flaps incorporating fascial components are well established in the literature as effective in providing a smooth gliding surface through the immediate coverage of severe soft tissue defects in the wrist. The fascial flaps widely used for wrist defects include the radial forearm, serratus anterior, lateral arm, temporoparietal, dorsal ulnar forearm and posterior interosseous flaps, and have a number of pros and cons 12, 13, 14, 15, 16, 17, 18, 19, 20.
Adipofascial flaps also have potential as pliable soft tissue coverage for immediate and late reconstruction of wrist defects. They provide a thin, broad, well‐vascularised coverage and a gliding surface for tendons (10). In addition, these flaps may prevent the unsightly donor sites that can result from a fasciocutaneous flap. They are useful and reliable even in elderly patients without relevant morbidity (7). Indeed, we found adipofascial flaps to be superior to the sophisticated composite flaps that require multiple secondary revisions, are more time consuming, and have greater risk of donor site morbidity. The superiority of the adipofascial flaps, which results from the gliding effect of the adipose tissue and fascial strength and pliability, is because of the single‐stage coverage, the reduced adherences to underlying nerve, tendon, vascular or skeletal tissues and the low‐friction interface that these flaps provide. However, they should be avoided for immediate reconstruction in patients with a wide trauma zone proximal to the defect, because the vascular pedicle may have been injured.
Conclusion
The adipofascial turnover flap is a single‐stage procedure with minimal donor site morbidity and can be used safely for coverage of complicated wrist defects that involve exposed tendon, bone or neurovascular structures. Since adipofascial flaps provide a gliding surface, they are a good choice for immediate coverage of soft tissue defects in the wrist that are not suitable for skin grafting alone as well as for late adhesion‐related problems.
Acknowledgement
None of the authors has a financial interest in any medical device or product mentioned in this article.
References
- 1. Hoppenfeld S. Physical examination of the hand and wrist. In: Hoppenfeld S, editor. Physical examination of the spine and extremities. New York: Prentice‐Hall, 1974:59–104. [Google Scholar]
- 2. Weinzweig N, Chin G, Mead M, Gonzalez M. “Spaghetti wrist”: management and results. Plast Reconstr Surg 1998;102:96–102. [DOI] [PubMed] [Google Scholar]
- 3. Gelberman RH, Manske PR. Factors influencing flexor tendon adhesions. Hand Clin 1985;1:35–42. [PubMed] [Google Scholar]
- 4. Edinburg M, Widgerow AD, Bidduph SL. Early postoperative mobilization of flexor tendon injuries using a modification of the Kleinert technique. J Hand Surg Am 1987;12:34–8. [DOI] [PubMed] [Google Scholar]
- 5. Pettengill KMS, Strien GV. Postoperative management of flexor tendon injuries. In: Hunter JM, editor. Rehabilitation of the hand and upper extremity. St Louis: Mosby, 2002:431–56. [Google Scholar]
- 6. Guzelkucuk U, Duman I, Taskaynatan M, Dincer K. Comparison of therapeutic activities with therapeutic exercises in the rehabilitation of young adult patients with hand injuries. J Hand Surg Am 2007;32:1429–35. [DOI] [PubMed] [Google Scholar]
- 7. Braga SJ, Padoin AV, Gazzalle A, da Cunha GL. Dorsal forearm adipofascial turnover flap among the elderly. J Hand Surg Eur Vol 2011;36:370–5. [DOI] [PubMed] [Google Scholar]
- 8. Lister G. Pitfalls and complications of flexor tendon surgery. Hand Clin 1985;1:133–46. [PubMed] [Google Scholar]
- 9. Schneider LH. Tenolysis and capsulectomy after hand fractures. Clin Orthop Relat Res 1996;327:72–8. [DOI] [PubMed] [Google Scholar]
- 10. Taghinia AH, Carty M, Upton J. Fascial flaps for hand reconstruction. J Hand Surg Am 2010;35:1351–5. [DOI] [PubMed] [Google Scholar]
- 11. Jaquet JB, van der Jagt I, Kuypers PD, Schreuders TA, Kalmijn AR, Hovius SE. Spaghetti wrist trauma: functional recovery, return to work, and psychological effects. Plast Reconstr Surg 2005;115: 1609–17. [DOI] [PubMed] [Google Scholar]
- 12. Jones NF, Jarrahy R, Kaufman MR. Pedicled and free radial forearm flaps for reconstruction of the elbow, wrist and hand. Plast Reconstr Surg 2008;121:887–98. [DOI] [PubMed] [Google Scholar]
- 13. Chang SM. The distally based radial forearm fascia flap. Plast Reconstr Surg 1990;85:150–1. [DOI] [PubMed] [Google Scholar]
- 14. Buehler MJ, Pacelli L, Wilson KM. Serratus fascia “sandwich” free‐tissue transfer for complex dorsal hand and wrist avulsion injuries. J Reconstr Microsurg 1999;15:315–20. [DOI] [PubMed] [Google Scholar]
- 15. Ulusal BG, Lin YT, Ulusal AE, Lin CH. Free lateral arm flap for 1‐stage reconstruction of soft tissue and composite defects of the hand: a retrospective analysis of 118 cases. Ann Plast Surg 2007;58:173–8. [DOI] [PubMed] [Google Scholar]
- 16. Seradge H, Adham MN, Seradge E, Hunter D. Free vascularized temporal parietal flap in hand surgery. Orthopedics 1995;18:1083–5. [DOI] [PubMed] [Google Scholar]
- 17. Choupina M, Malheiro E, Guimarães I, Pinho C, Silva P, Ferreira P, Reis J, Amarante J. Osteofasciocutaneous flap based on the dorsal ulnar artery: a new option for reconstruction of composite hand defects. Br J Plast Surg 2004;57:465–8. [DOI] [PubMed] [Google Scholar]
- 18. Xu G, Lai‐jin L. Coverage of skin defects in spaghetti wrist trauma: application of the reverse posterior interosseous flap and its anatomy. J Trauma 2007;63:402–4. [DOI] [PubMed] [Google Scholar]
- 19. Carty MJ, Taghinia A, Upton J. Fascial flap reconstruction of the hand: a single surgeon's 30‐year experience. Plast Reconstr Surg 2010;125:953–62. [DOI] [PubMed] [Google Scholar]
- 20. Tintle SM, Wilson K, McKay PL, Andersen RC, Kumar AR. Simultaneous pedicled flaps for coverage of complex blast injuries to the forearm and hand. J Hand Surg Eur Vol 2010;35:9–15. [DOI] [PubMed] [Google Scholar]


