Abstract
Scars hypertrophy and widen when stretching mechanical forces are applied to resilient newly formed collagen before it reaches final maturity marring the final result of many surgical procedures and resulting in a clinical problem for many patients. Scar revision by surgical excision remains the traditional treatment for hypertrophic or widespread scars. It relies upon recruitment of local tissues for closure of the ensuing defect. Providing tension‐free skin closure is the best option to avoid recurrence. Although tissue expansion procedure is a valuable and reliable technique for scar revision, it has its own disadvantages and potential complications. We describe an alternative method for scar revision that may be applicable in certain situations. Instead of expanding the soft tissues to make available additional skin, deflation by liposuction may be affected to relax the skin envelope thus indirectly providing additional skin for scar revision. We call this method ‘reverse tissue expansion’.
Keywords: Liposuction deflation, Reverse tissue expansion, Scar management, Scar revision
INTRODUCTION
The skin is an organ in constant contact with the environment designed to adapt to stresses and strains. When injured, it consistently and rapidly repairs itself with necessary scar formation 1, 2 the rate and quality of which varies among individuals. Alterations in this process with deviation in the orderly pattern of healing, whether extrinsically or intrinsically derived, may result in the development of an abnormal scar (1). An overzealous healing response can create a raised nodule of fibrotic tissue, whereas ‘pitted’ and atrophic scars may result from inadequate replacement of deleted collagen fibres (3). Such textural changes are often permanent (3).
The aesthetic appearance of a scar is often the single most important criterion used by patients and physicians alike in judging surgical outcome (4). Ideal cosmetically acceptable scar is a nearly imperceptible soft fine line that is level with the skin, with good colour match, usually within or parallel to relaxed skin tension lines, and blends with the natural creases and folds 2, 4. This fine scar may be the demarcating line between acceptable and unacceptable aesthetic results 1, 5. Sometimes, the final outcome falls short of these expectations (4).
Abnormal scars usually can be classified into four etiologic categories: traumatic, poorly designed, poorly healed, and disease‐related (2). Scars with poor cosmetic results include those that are wide, raised, depressed, red, or pigmented, or those that transect natural creases and junctions (4). Depending on the type of abnormality, different techniques are used to improve the overall cosmetic appearance (4). Hypertrophic scars, however, are among the most common and frustrating problems after injury or surgery (5) and remain notoriously difficult to eradicate because of the high recurrence rates and the incidence of side effects associated with available treatment methods 1, 5.
A variety of techniques, both surgical and nonsurgical, exists for treatment of unsightly scars 5, 6. Surgical excision remains the traditional treatment for hypertrophic or widespread scars (1). It relies upon recruitment of local tissues for closure of the ensuing defect, and is best attempted on a mature scar, where surrounding tissues and the wound bed are not subject to exaggerated tension forces 6, 7. Surgical strategies for scar revision include excision with linear closure, excision with split‐ or full‐thickness skin grafting, Z‐plasty, W‐plasty, and if all other options fail, excision followed by flap coverage 2, 4, 8, 9.
The ability to use local tissues depends on the nature of the anticipated defect and the availability of adjacent tissue for local advancement (10). Irrespectively, important principles for any scar revision are tension‐free closure and wound edge eversion (7). Unfortunately, revision with tension‐free closure is not possible for large widespread scars with insufficient surrounding tissue laxity (2). In such situations, tissue expansion or serial scar excision may be used to provide more tissue for advancement or to provide local flap coverage of revised scars (8). Serial excision is not an unpopular method of revising scars 6, 11 and is possible due to stress relaxation (12). It has a major disadvantage of multiple procedures being necessary to render the desired scar reduction (11). Using conventional excision methods, the scar is partially excised and the adjacent skin advanced by undermining sufficiently. If more than two procedures are required, tissue expansion is useful as a complementary tool to reduce the number of necessary excisions 2, 6.
Tissue expansion with the use of internal tissue expanders is a reputable and reliable method for many forms of reconstruction 11, 13. It is based on the principle that living tissues respond in a dynamic fashion to a mechanical stress that is placed on them (10) whereby tissue growth is induced with the application of increasing tension (14). Other techniques such as presuturing 11, 15, 16, towel clips 11, 17, and skin‐stretching devices 11, 18, 19, 20 are also useful but are mainly applicable intraoperatively or a few days before definitive reconstruction. Lasheen et al. (21) successfully used external tissue expansion with negative pressure to overcome significant risk of complications. Their method nevertheless does not overcome the need for a specialised device (11). Traction‐assisted dermatogenesis with Micropore (3M, St. Paul, MN) taping is an additional none invasive method of tissue expansion recently described that is easy and cost effective to expand skin (11).
Although tissue expansion procedure is a valuable and reliable technique for scar revision, it has as with every surgical endeavour its own disadvantages and potential complications. At least two operations and multiple office visits are required during the expansion period 10, 22, 23. Tissue expansion with expanders has a significant major complication rate of approximately 25%. This complication rate may increase to above 40% in limbs 11, 24, 25. The most common complications are wound disruption and exposure of the implant, infection, haematoma or seroma, implant failure, pain, and skin ischaemia or necrosis 11, 24, 25, 26. We describe an alternative method for scar revision that may be applicable in certain situations. Instead of expanding the soft tissues to make available additional skin, deflation by liposuction may be affected to relax the skin envelope thus indirectly providing additional skin for scar revision. We call this method ‘reverse tissue expansion’.
MATERIALS AND METHODS
Two young female patients presented with widespread scars on their lateral thighs for revision. Both have had orthopaedic surgical procedures several years earlier with subsequent scar revision by other surgeons consisting in elliptical excision and direct linear closure. In both patients, widespread scars developed in addition to stitch marks and gross thigh contour deformity and were 12 and 13 on the visual analogue scale 27, 28. Both patients' scars were revised following liposuction deflation by elliptical excision and linear closure achieving a stable linear scar while improving thigh contour at the same time (1, 2, 3, 4, 5, 6).
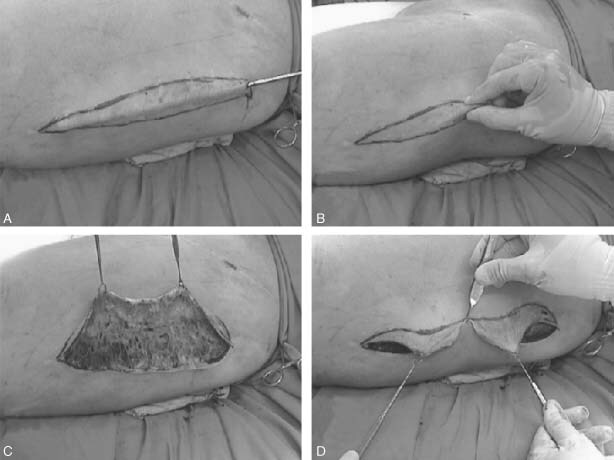
Figure 1.

(A, B, C) Patient with bilateral thigh scars following scar revision few years ago by another surgeon resulting in widespread scars with stitch marks and obvious contour deformity. (D, E, F, G) Markings for elliptical excision of scars and liposuction.
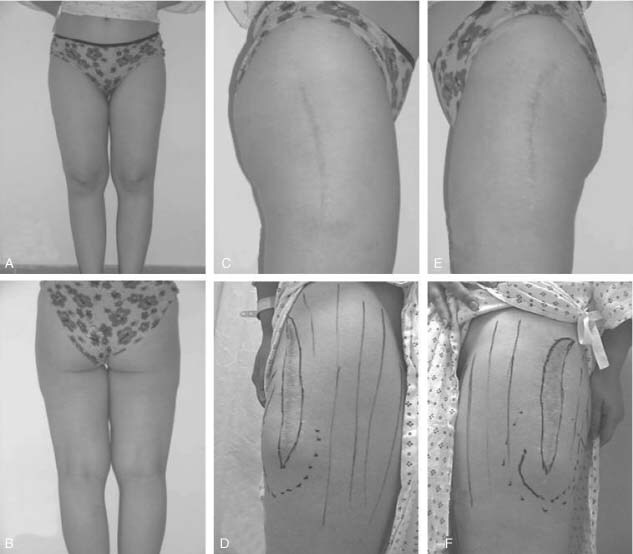
Figure 2.
(A, B) Complete deflation by liposuction of the scar together with standard thigh liposuction. (C, D) Simple excision of the scar and simple approximation without neither tension nor undermining.
Figure 3.

(Upper row) Result at 2 months. (Lower row) One year and half after liposuction and scar revision with net improvement in scar appearance and thigh contour.
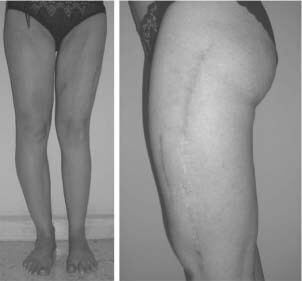
Figure 4.
Patient 1: Final stable result of linear scar revision with at 3 years despite 8 kg weight gain. (A, B) Pleasant thighs contour. (C, E) Right and left thigh scars with (D, F) preoperative scars shown for comparison. Scar excision was 5 cm in the mid portion.
Figure 5.
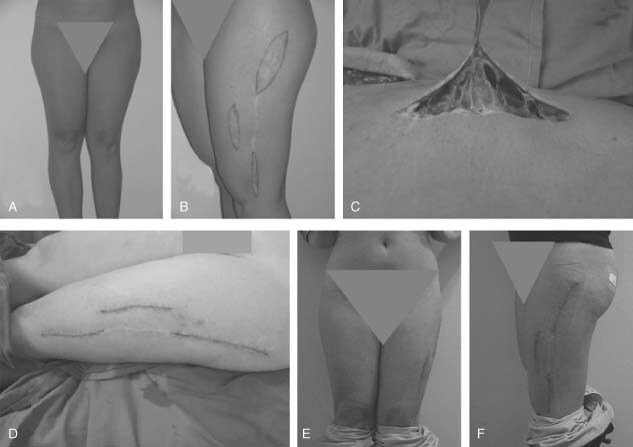
Patient 2: (A, B) Patient with lateral left thigh widespread scars and contour deformity following previous scar revision. (C) Complete scar deflation with bilateral standard thigh liposuction. (D) Immediate postoperative result following revision of the widespread scar segments only. (E, F) Result at 2 months.
Figure 6.
Patient 2: Result at 7 months with net improvement in thighs contour and symmetry and stable linear scars despite wide excision superiorly. Marks on anterior thighs are secondary to irritation and recent prolonged sun exposure at the beach.
DISCUSSION
A successful wound closure procedure is defined as a complete approximation of the wound margins with suturing of the skin (19). This, however, does not guarantee adequate scar evolution particularly if skin closure has been effected under tension such that some surgeons regard pathologic scaring as inevitable, regardless of surgical technique; others believe that their personal method of wound closure reduces it (29).
The skin has distinctive nonlinear viscoelastic properties and therefore can be stretched by applying mechanical forces 12, 14, 19. Skin immediate extensibility is the product of its intrinsic elasticity. When stretched, the skin's convoluted collagen fibres straighten and realign parallel to one another 11, 12. Further skin recruitment occurs secondary to mechanical creep which is elongation of skin with a constant load over time beyond intrinsic extensibility. With the passage of time stress relaxation enables the additional loading of skin to recruit even more tissue 11, 12. These processes have been described as the vehicle harnessed for wound closure with presuturing, intraoperative tissue expansion, skin‐stretching devices, and skin retraction with undermining 11, 12. Although these processes help to close skin defects, they also generate opposing reciprocal mechanical forces that tend to pull the edges of the sutured wound apart.
Mechanical tension, plays a critical role in control of cell growth and function, and is critical for tissue remodelling in many tissues, including skin 14, 30, 31. Mechanical stress accelerates wound healing by producing stronger and more organised scars, however, at the expense of scar stretching (32). It is demonstrated that hypertrophic scarring occurs in areas of high tension with ‘pull’ in many directions or intermittent tension and is possibly initiated by lymphocytes but definitely related to a prolongation of the inflammatory process, with increased fibroblast activity and overabundant extracellular matrix secretion (33). A stretched scar results from increased tension in one axis only (34) probably initiated by neutrophils and their neutral proteases (34).
When sutured under a significant amount of tension, the skin tends to retract although not eventually back to its original condition before stretching (35). This is the stretch‐back phenomenon which to a considerable extent reduces the benefits of fusiform excision and closure under tension (36). Studies on reduction of male baldness by serial excisions and closure under tension have shown that almost one third to one half of the excised bald area is lost due to the stretch‐back, and that almost all the stretching occurs during the first 8 weeks following surgery (36). Moreover, it was also shown that although undermining significantly diminishes the tension on wound margins, increasing amount of tension while advancing a scalp flap affects the compliance of the flaps in a nonlinear fashion demonstrating an exponential stress–strain characteristic of rapidly increasing stiffness (37).
Scars hypertrophy and widen when stretching mechanical forces are applied to resilient newly formed collagen before it reaches final maturity, a process that can take several months before being completed 38, 39. Tensile distracting forces can be caused by factors such as muscle pull, elastic forces of adjacent skin, and external pressure 38, 39. Widening of scars is thus mainly the result of mechanical influences on resilient and, as yet, immature collagen. This concept is probably validated by the outcome of healing wounds relative to the lines of Langer. These lines lie perpendicular to the tension vector of underlying muscular contraction 38, 39. Anecdotal evidence suggests that incisions created parallel to skin tension lines rarely form abnormal scars. Moreover, abnormal scarring rarely develops in loosely skinned elderly patients (40). However, a wide variation in scar formation can be observed at different anatomical locations even when wounds have been closed using considerable tension. This suggests that the amount of scarring is determined not only by the amount of tension applied on the wound but, more importantly, by the viscoelastic properties of the skin at various locations (35).
Widening of scars is a frustrating event that most if not all plastic surgeons have encountered (38). Even more frustrating is scar widening after re‐excision which can subvert even the most meticulous wound closure techniques (7). Most plastic surgeons have frequently encountered this frustrating sequence of events: closing a wound in the neatest manner possible, meticulously apposing all layers, using thin, absorbable intradermal sutures, and within a few months having a wide, ugly scar appear (38). Different approaches have been advocated to tackle this problem. Corticosteroid injections, although more indicated for hypertrophic rather than stretched scars, are still quite popular, however, the final even more disfiguring outcome, consisting of thin, atrophic, telangiectatic, erythematous skin, has made many reluctant to use them. Other modalities include irradiation, ultrasound, and silicone applications, as well as many others, but these treatment modalities do nothing to prevent or diminish the underlying distracting force which constitutes the main pathologic process (39). Millard (41) has described almost 40 years ago scar repair by the double‐breasted vest principle to overcome the problem of tension. This technique was later revised using a small amount of existing scar tissue to hold the tension of the re‐closure. A tongue of de‐epithelialised scar is buried under a carefully dissected skin flap thus taking the tension off the surface of the skin 7, 38.
Immobilisation is a basic therapeutic principle in wound healing, common to the treatment of lesions of all kinds. Casts, plates, and sutures minimise the negative effects of muscle tension on healing wounds, including skin lesions (39). Microporous tape has been reported to be a reliable way to support a scar 5, 33. Repeated microtrauma caused by continuous displacement of injured tissue induces a prolonged inflammatory response and distortion of healing tissues before they achieve strength and maturity. Clinically, this would manifest as scar widening, hypertrophy, or both (39). Anecdotal techniques of annulling muscle contraction by putting the face in a bandage mask for 3 months have been described but were poorly tolerated by the patients (39). More recently botulinum toxin injections simultaneous with scar revision surgery of the face has been described to induce temporary paralysis of the underlying muscles effectively minimising tension on the healing wound edges (39).
Providing tension‐free skin closure remains the best option to avoid recurrence of widespread or hypertrophic scars following surgical revision. Tissue expansion is invaluable in that regard. ‘Natural’ expansion of abdominal skin in conjunction with pregnancy as an internal autologus endogenous expander has been previously described as extremely useful for ventral hernia repair as well as for scar revision 42, 43, 44, 45. Similarly, lipodystrophy and obesity produce natural expansion. Removal of excess fat by liposuction will deflate the tissues and provide relaxed skin for scar revision.
Skin is an envelope confining a given body volume in a ratio surface/volume (S/V). For scar revision tension‐free skin closure S/V ratio must be increased at least to compensate for the scar surface that must be excised if not more. This can be achieved either by increasing S by expansion or decreasing V by ‘reverse expansion’ through liposuction (Figure 7). Liposuction with deflation of adjacent tissues reduces the volume and provides discontinuous undermining that will allow flap mobilisation and advancement without undermining 46, 47, 48, 49 facilitating wound closure without tension.
Figure 7.
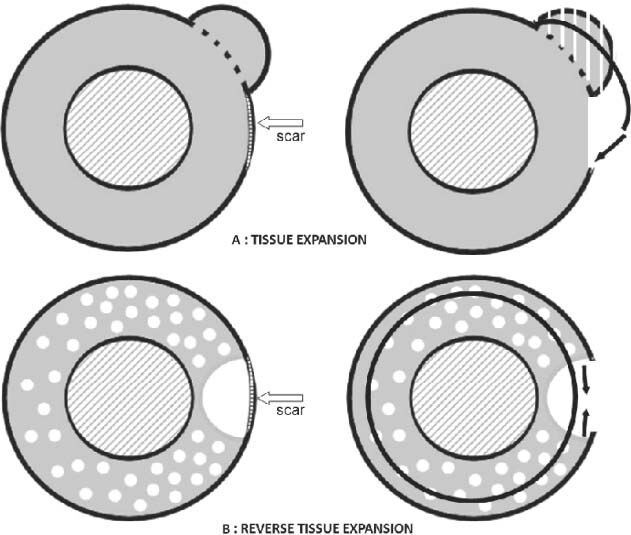
(A) Tissue expansion: S/V ratio increased by increasing S (inner circle: thigh muscle and bony mass circumference. Outer circle: thigh circumference). The increase in S should be at least 1·2 to 1·5 times the width of the scar to be excised. (B) Reverse tissue expansion: S/V ratio increased by decreasing V (white dots represent tunnelling by liposuction). Fat underlying the scar is completely aspirated resulting in total deflation of the area allowing skin approximation (represented by the middle circle on the right) after scar excision with no tension.
One major drawback of this technique, although, is that preoperative planning using exact measurements similar to standard tissue expansion is not applicable. Pinch test and clinical judgment are required to determine if a wide scar may be revised and closed primarily or additional skin may be required to allow closure with minimal tension. In that case, additional skin may be provided either with standard expansion or with liposuction provided that latter is indicated. As with other patients presenting for liposuction, surgical decision is made using clinical and aesthetic parameters. MRI or ultrasound, useful as research tools, are not routinely used to determine thickness of the fatty layer as these tests are clinically not relevant for routine liposuction and will result in additional costs to the patient. Liposuction is performed with the tumescent technique and is aimed at improving the patient's contour. Relaxed skin may be determined thereafter with the pinch test and is a welcomed addition that may be used secondarily for scar revision. Wound closure is performed in layers. The deep fascia is closed first with then the skin is approximated by interrupted sutures followed by a running subcuticular suture. Only resorbable sutures are used, 2‐0 Vicryl® (Polyglactin 910) for the fascia and 4‐0 Monocryl® (Poliglecaprone 25) [Ethicon, Inc. (Jhonson&Jhonson Intl) St‐Stevens‐Woluwe, Belgium] for the skin. A simple semi‐permeable dressing is then applied and the patient fitted with the regular liposuction compression garment for 6 weeks. Moist exposed burn ointment MEBO® (Gulf Pharmaceutical Industries, Ras Al Kahimah, UAE) previously shown to improve scar quality is also applied twice daily during this period 50, 51. Although some surgeons do insert drains following liposuction, we usually do not and we did not feel that drains were necessary even after scar revision.
Another drawback of combining liposuction with scar revision may be the theoretical compilation of complications. In fact, mild to moderate liposuction (not more than 1·5–2 l) is a well‐standardised procedure performed routinely with a low complication rate; when combined with scar revision it should, theoretically as well, reduce the complication rate of scar revision performed under tension. Compared to the high complication rate of tissue expansion in the lower extremity, combined liposuction and scar revision has probably a lower complication rate and is definitely a more convenient one‐stage procedure. It is also a more rewarding procedure to the patient that will benefit from an immediately apparent better contour.
CONCLUSION
Pathologic scaring marks the final result of many surgical procedures and remains a clinical problem for many patients (52). Scars on the trunk and extremities often hypertrophy and spread with very noticeable ‘track’ marks (4). Unsightly hypertrophic and widespread scars may cause functional and cosmetic deformities, discomfort, and psychological stress (7). Scar revision is a well‐established procedure and is indicated in certain situations for cosmetic and functional reasons (53). A successful scar revision can dramatically improve a patient's quality of life (2) . Unfortunately, achievement of satisfying long‐term results may present a real challenge (54).
The surgery and management of scars is a protracted and staged process (55). Scar revision requires planning and preoperative counselling regarding recurrence risks, particularly for keloid‐prone patients (1). Preparation of the skin through hygienic measures, scar softening (if indicated) with steroids, massage and pressure dressings, skilled execution of the surgical plan, and thorough postoperative wound care cannot be overemphasised to achieve favourable results (55). Although ‘there is no generic approach to timing or technique in scar revision’, the decision of how and when to intervene with a scar revision lies between the patient and the physician, with the latter providing strong and accurate guidance (56). Conservative timing allowing the natural process of healing is always to be primarily considered (56).
It is important to realise that in scar revision there are factors beyond the surgeon's control and factors certainly under his control 56, 57 the most important of which is to achieve skin closure with no tension. It must be realised also that improvement is not feasible with all scars; expectations must be tempered and realistic goals set (53). The decision to revise a scar must be reached by patient and surgeon, with realistic expectations and the end‐point clearly established. The simplest and most direct approach should then be taken to reach this goal (53). In certain situations, reverse tissue expansion by liposuction may be highly beneficial and even desirable. It not only provides tension‐free wound closure but also achieves improvement in body contour which will be much more gratifying to the patient than the actual improvement in scar quality.
REFERENCES
- 1. Slemp AE, Kirschner RE. Keloids and scars: a review of keloids and scars, their pathogenesis, risk factors, and management. Curr Opin Pediatr 2006;18:396–402. [DOI] [PubMed] [Google Scholar]
- 2. Batra RS. Surgical techniques for scar revision. Skin Therapy Lett 2005;10:4–7. [PubMed] [Google Scholar]
- 3. Alster T, Zaulyanov‐Scanlon L. Laser scar revision: a review. Dermatol Surg 2007;33:131–40. [DOI] [PubMed] [Google Scholar]
- 4. Lee KK, Mehrany K, Swanson NA. Surgical revision. Dermatol Clin 2005; 23:141–50. [DOI] [PubMed] [Google Scholar]
- 5. Atiyeh BS. Non‐surgical management of hypertrophic scars (Hss): evidence‐based therapies, standard practices and emerging modalities. Aesthetic Plast Surg 2007;31:468–92. Epub 2007 Jun 18. [DOI] [PubMed] [Google Scholar]
- 6. Mostafapour SP, Murakami CS. Tissue expansion and serial excision in scar revision. Facial Plast Surg 2001;17:245–51. [DOI] [PubMed] [Google Scholar]
- 7. Chen MA, Davidson TM. Scar management: prevention and treatment strategies. Curr Opin Otolaryngol Head Neck Surg 2005;13:242–7. [DOI] [PubMed] [Google Scholar]
- 8. Reish RG, Eriksson E. Scars: a review of emerging and currently available therapies. Plast Reconstr Surg 2008;122:1068–78. [DOI] [PubMed] [Google Scholar]
- 9. Nagasao T, Miyamoto J, Yoshikawa K, Ando Y, Nagasao M, Nakajima T. “Beak”‐plasty: a new effective modification of Z‐Plasty. Dermatol Surg 2007;33:344–9. [DOI] [PubMed] [Google Scholar]
- 10. Bascom DA, Wax MK. Tissue expansion in the head and neck: current state of the art. Curr Opin Otolaryngol Head Neck Surg 2002;10:273–7. [Google Scholar]
- 11. Daya M, Nair V. Traction‐assisted dermatogenesis by serial intermittent skin tape application. Plast Reconstr Surg 2008;122:1047–54. [DOI] [PubMed] [Google Scholar]
- 12. Wilhelmi BJ, Blackwell SJ, Mancoll JS, Phillips LG. Creep vs. stretch: a review of the viscoelastic properties of skin. Ann Plast Surg 1998;41:215–9. [DOI] [PubMed] [Google Scholar]
- 13. Radovan C. Tissue expansion in soft tissue reconstruction. Plast Reconstr Surg 1984;74:482–92. [DOI] [PubMed] [Google Scholar]
- 14. Pietramaggiori G, Liu P, Scherer SS, Kaipainen A, Prsa MJ, Mayer H, Newalder JMA, Alperovich MBS, Mentzer SJ, Konerding MA, Huang S, Ingber DE, Orgill DP. Tensile Forces Stimulate Vascular Remodeling and Epidermal Cell Proliferation in Living Skin. Ann Surg 2007; 246:896–902. [DOI] [PubMed] [Google Scholar]
- 15. Liang MD, Briggs P, Heckler FR, Futrell JW. Presuturing: a new technique for closing large skin defects. Clinical and experimental studies. Plast Reconstr Surg 1988;81:694–702. [DOI] [PubMed] [Google Scholar]
- 16. Meirson D, Reyes BA, Geronemus R. Presuturing in alopecia reductions. J Dermatol Surg Oncol 1990;16:828–30. [DOI] [PubMed] [Google Scholar]
- 17. Perlis CS, Dufresne RG Jr. Immediate skin stretching with towel clips and needles. Dermatol Surg 2005;31:697–8. [DOI] [PubMed] [Google Scholar]
- 18. Hirshowitz B, Lindenbaum E, Har‐Shai Y. A skin‐stretching device for the harnessing of the viscoelastic properties of skin. Plast Reconstr Surg 1993;92:260–70. [DOI] [PubMed] [Google Scholar]
- 19. Barnea Y, Gur E, Amir A, Leshem D, Zaretski A, Shafir R, Weiss J. Our experience with wisebands: a new skin and soft‐tissue stretch device. Plast Reconstr Surg 2004;113:862–9. [DOI] [PubMed] [Google Scholar]
- 20. Bjarnesen JP, Wester JU, Siemssen SS, Blomqvist G, Jensen NK. External tissue stretching for closing skin defects in 22 patients. Acta Orthop Scand 1996;67:182–4. [DOI] [PubMed] [Google Scholar]
- 21. Lasheen AE, Salim A, Hefny MR, Al‐Bakly E. External tissue expansion successfully achieved using negative pressure. Surg Today 2004;34:193–196. [DOI] [PubMed] [Google Scholar]
- 22. Keskin M, Kelly CP, Yavuzer R, Miyawaki T, Jackson IT. External filling ports in tissue expansion: confirming their safety and convenience. Plast Reconstr Surg 2006;117:1543–51. [DOI] [PubMed] [Google Scholar]
- 23. Bozkurt A, Groger A, O’Dey D, Vogeler F, Piatkowski A, Fuchs PCh, Pallua N. Retrospective analysis of tissue expansion in reconstructive burn surgery: evaluation of complication rates. Burns 2008;34:1113–8. Epub 2008 Aug 15. [DOI] [PubMed] [Google Scholar]
- 24. Cunha MS, Nakamoto HA, Herson MR, Faes JC, Gemperil R, Ferreira MC. Tissue expander complications in plastic surgery: a 10‐year experience. Rev Hosp Clin Fac Med Sao Paulo 2002;57:93–7. [DOI] [PubMed] [Google Scholar]
- 25. Pandya AN, Vadodaria S, Coleman DJ. Tissue expansion in limbs: a comparative analysis of limb and nonlimb sites. Br J Plast Surg 2002;55:302–6. [DOI] [PubMed] [Google Scholar]
- 26. Heitmann C, Levin S. Tissue Expansion. Tech Hand Up Extrem Surg 2003;7:7–11. [DOI] [PubMed] [Google Scholar]
- 27. Beausang E, Floyd H, Dunn KW, Orton CI, Ferguson MW. A new quantitative scale for clinical scar assessment. Plast Reconstr Surg 1998;102:1954–61. [DOI] [PubMed] [Google Scholar]
- 28. Duncan JA, Bond JS, Mason T, Ludlow A, Cridland P, O’Kane S, Ferguson MW. Visual analogue scale scoring and ranking: a suitable and sensitive method for assessing scar quality? Plast Reconstr Surg 2006;118:909–18. [DOI] [PubMed] [Google Scholar]
- 29. Sommerlad BC, Creasey JM. The stretched scar: a clinical and histological study. Br J Plast Surg 1978;31:34–5. [DOI] [PubMed] [Google Scholar]
- 30. Ingber DE. Cellular mechanotransduction: putting all the pieces together again. FASEB J 2006; 20:811–27. [DOI] [PubMed] [Google Scholar]
- 31. Ryan TJ. Exchange and the mechanical properties of the skin: oncotic and hydrostatic forces control by blood supply and lymphatic drainage. Wound Repair Regen 1995;3:258–64. [DOI] [PubMed] [Google Scholar]
- 32. Timmenga EJ, Andreassen TT, Houthoff HJ, Klopper PJ. The effect of mechanical stress on healing skin wounds: an experimental study in rabbits using tissue expansion. Br J Plast Surg 1991;44:514–9. [DOI] [PubMed] [Google Scholar]
- 33. Widgerow AD, Chait LA, Stals R, Stals PJ. New innovations in scar management. Aesthetic Plast Surg 2000;24:227–34. [DOI] [PubMed] [Google Scholar]
- 34. Meyer M, McGrouther DA. A study relating wound tension to scar morphology in the pre‐sternal scar using Langers technique. Br J Plast Surg 1991;44:291–4. [DOI] [PubMed] [Google Scholar]
- 35. Melis P, van Noorden CJ, van der Horst CM. Long‐term results of wounds closed under a significant amount of tension. Plast Reconstr Surg 2006;117:259–65. [DOI] [PubMed] [Google Scholar]
- 36. Nordström RE, Devine JW. Scalp stretching with a tissue expander for closure of scalp defects. Plast Reconstr Surg 1985;75:578–81. [DOI] [PubMed] [Google Scholar]
- 37. Raposio E, Santi PL, Nordström RE. Serial scalp reductions: a biomechanical approach. Dermatol Surg 1999;25:210–4. [DOI] [PubMed] [Google Scholar]
- 38. Wilson AM. Widening of scars: foe coaxed into a friend? The Millard technique revisited. Plast Reconstr Surg 2000;106:1488–93. [DOI] [PubMed] [Google Scholar]
- 39. Wilson AM. Use of botulinum toxin type a to prevent widening of facial scars. Plast Reconstr Surg 2006;117:1758–66. [DOI] [PubMed] [Google Scholar]
- 40. Akaishi S, Akimoto M, Ogawa R, Hyakusoku H. The relationship between keloid growth pattern and stretching tension: visual analysis using the finite element method. Ann Plast Surg 2008;60: 445–51. [DOI] [PubMed] [Google Scholar]
- 41. Millard DR. Scar repair by the double‐breasted vest principle. Plast Reconstr Surg 1970;45:616–9. [DOI] [PubMed] [Google Scholar]
- 42. DiGregorio VR. Two unusual postburn reconstructions using tissue expansion: one exogenous and one endogenous. Ann Plast Surg 1993;30:549–51. No abstract available. [DOI] [PubMed] [Google Scholar]
- 43. Del Frari B, Pülzl P, Schoeller T, Widschwendter M, Wechselberger G. Pregnancy as a tissue expander in the correction of a scar deformity. Am J Obstet Gynecol 2004;190:579–80. [DOI] [PubMed] [Google Scholar]
- 44. Riordan C, Budny P, Regan P. Pregnancy as an autologous tissue expander for closure of an abdominal‐wall defect. Br J Plast Surg 2003;56:64–6. [DOI] [PubMed] [Google Scholar]
- 45. Elwood ET, Ingram WL, Carlson GW. Pregnancy as a tissue expander in the repair of a massive ventral hernia. Ann Plast Surg 2000;45:431–3. [DOI] [PubMed] [Google Scholar]
- 46. Illouz YG. A new safe and aesthetic approach to abdominoplasty. Aesthetic Plast Surg 1992;16: 237–45. [DOI] [PubMed] [Google Scholar]
- 47. Mayr M, Holm C, Höfter E, Becker A, Pfeiffer U, Mühlbauer W. Effects of aesthetic abdominoplasty on abdominal wall perfusion: a quantitative evaluation. Plast Reconstr Surg 2004;114: 1586–94. [DOI] [PubMed] [Google Scholar]
- 48. Matarasso A. Liposuction as an adjunct to a full abdominoplasty. Plast Reconstr Surg 1995;95:829–36. [PubMed] [Google Scholar]
- 49. Matarasso A. Liposuction as an adjunct to full abdominoplasty revisited. Plast Reconstr Surg 2000;106:1197–1202. [DOI] [PubMed] [Google Scholar]
- 50. Atiyeh BS, Al‐Amm CA, El‐Musa KA, Sawwaf A, Dham R. Scar quality and physiologic barrier function restoration following moist and moist exposed dressings of partial thickness wounds. Dermatol Surg 2003;29:14–20. [DOI] [PubMed] [Google Scholar]
- 51. Atiyeh BS, Ioannovich J, Al‐Amm CA, El‐Musa KA, Dham R. Improving scar quality: a prospective clinical study. Aesthetic Plast Surg 2002;26:470–6. [DOI] [PubMed] [Google Scholar]
- 52. Armour A, Scott PG, Tredget EE. Cellular and molecular pathology of HTS: basis for treatment. Wound Repair Regen 2007;15:S6–17. [DOI] [PubMed] [Google Scholar]
- 53. Thomas JR, Prendiville S. Update in scar revision. Facial Plast Surg Clin North Am 2002;10:103–11. [DOI] [PubMed] [Google Scholar]
- 54. Zakkak TB, Griffin JE Jr, Max DP. Posttraumatic scar revision: a review and case presentation. J Craniomaxillofac Trauma 1998;4:35–41. [PubMed] [Google Scholar]
- 55. Horswell BB. Scar modification. Techniques for revision and camouflage. Atlas Oral Maxillofac Surg Clin North Am 1998;6:55–72. [PubMed] [Google Scholar]
- 56. Field LM. Timing scar revision, Letter to the Editor. Dermatol Surg 2006;32:1108–9. [DOI] [PubMed] [Google Scholar]
- 57. Borges AF. Timing of scar revision techniques. Clin Plast Surg 1990;17:71–6. [PubMed] [Google Scholar]


