Abstract
Although being a safe and standardised procedure, free‐flap reconstruction can be harmful if unpredictable situations occur intraoperatively. The case presented reveals a situation in which an unscheduled interdisciplinary approach allowed to complete our reconstructive aim. An extensive defect at the thigh was planned for reconstruction by means of a free rectus abdominis flap. As the distant part of the flap showed a compromised perfusion during operation and had to be partially discarded, our colleagues from the vascular surgery department created an arterio‐venous loop for anastomosis. This allowed a more distant positioning of the flap and ensured a complete defect reconstruction.
Keywords: Arterio‐venous loop, Chronic wound, Free‐flap, Radiation injury, Thigh
Introduction
According to the literature, microsurgical free‐flap reconstruction is supposed to be successful in up to 95% of cases 1, 2 and has become a standardised procedure in reconstructive surgery. If no sufficient arterial inflow or venous outflow is guaranteed, an interdisciplinary approach with vascular bypass surgery and free‐flaps is one method to salvage extremities in danger of amputation 3, 4.
We want to present the case of a patient where an unpredictable situation during the operation occurred with the need for emergency arterio‐venous (AV) loop and 1‐stage free‐flap procedure.
Case report
An 83‐year‐old man with the diagnosis of a pleomorphic sarcoma of the lower anterior thigh was referred to our Department of Plastic and Hand Surgery, after radio‐chemotherapy with a total dose of 62·5 gray and radical surgical tumor excision (R0) was done. A full‐thickness soft‐tissue defect of approximately 10 × 5 cm2 remained. After the wound was treated with negative pressure wound therapy (NPWT, KCI, San Antonio, TX), the patient received split‐skin grafting.
During the follow‐up visits at the outpatient clinics, secondary partial loss of the split‐skin graft was noted and a local infection developed. The patient was readmitted to the hospital, several wound debridements became necessary and repetitive NPWT cycles were performed. Microbiological analysis revealed a multiresistent Pseudomonas aeruginosa and Enterococcus faecalis – the patient received an intravenous antibiotic therapy according to microbiological resistance testing.
During hospital stay, the patient fell on his leg and developed an extensive haematoma with partial rupture of the quadriceps muscle adjacent to the chronic wound. Because of cardiac arrhythmia, he was under anticoagulation therapy with low‐molecular‐weight heparin in a therapeutic dosage. An emergency operation became necessary where parts of the quadriceps muscle had to be revised. Afterwards, the patient was discharged from the hospital with an ambulatory NPWT device for further wound conditioning. However, the patient was again readmitted to our hospital with a deep wound infection and partial necrosis of the quadriceps muscle. After an extensive debridement of all the necrotic tissue, reconstruction with a free‐flap became indispensable (Figure 1).
Figure 1.

Defect after extensive debridement of all the necrotic tissue.
A free rectus abdominis muscle flap was planned in order to transfer well‐vascularised tissue into the poorly perfused and irradiated region. A latissimus dorsi flap – although desirable due to pedicle length, size of the flap and lower donor site morbidity – was regarded not to be the first choice as we did not want to risk postoperative haemorrhage at the donor site – which occurs more often in case of a free latissimus dorsi flap compared with the free rectus abdominis muscle flap. A perforator‐based periumbilicar skin island was included in order to monitor postoperative flap perfusion 5 (Figure 2). However, during the operation, it turned out that the most cranial part of the rectus muscle showed a compromised perfusion and had to be resected. Thus, the flap became too short to cover even the very distant part of the wound, as the pedicle length did not allow a more distant placement of the flap. Therefore, we decided to perform an emergency AV‐loop procedure in an interdisciplinary approach with our colleagues from the vascular surgery division. An AV‐loop was created, using the ipsilateral greater saphenous vein, which was connected with its distal ending to the femoral artery proximal to the defect (Figure 3). The AV‐loop was then transected at its midpoint and the flap was anastomosed to the arterial and venous branches in an end‐to‐end fashion. Within 5 days postoperatively, the perforator‐based monitor skin island was removed bedside by a simple ligation of the perforator vessel. The flap healed without any further complications and the patient was discharged from the hospital (Figure 4).
Figure 2.

Reconstruction with a free rectus abdominis muscle in combination with a perforator‐based monitor skin island.
Figure 3.
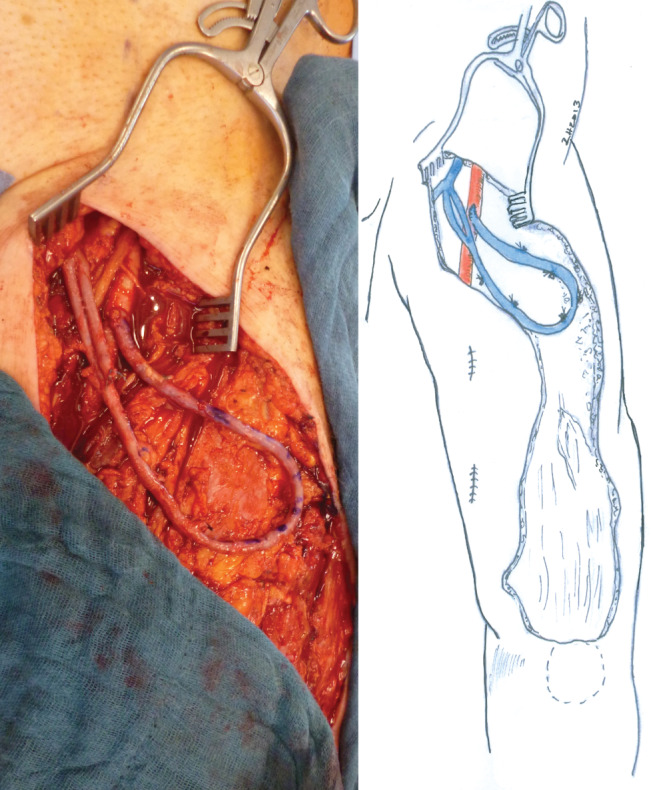
Arterio‐venous (AV)‐loop using the ipsilateral greater saphenous vein, connected with its distal ending to the femoral artery proximal to the defect.
Figure 4.
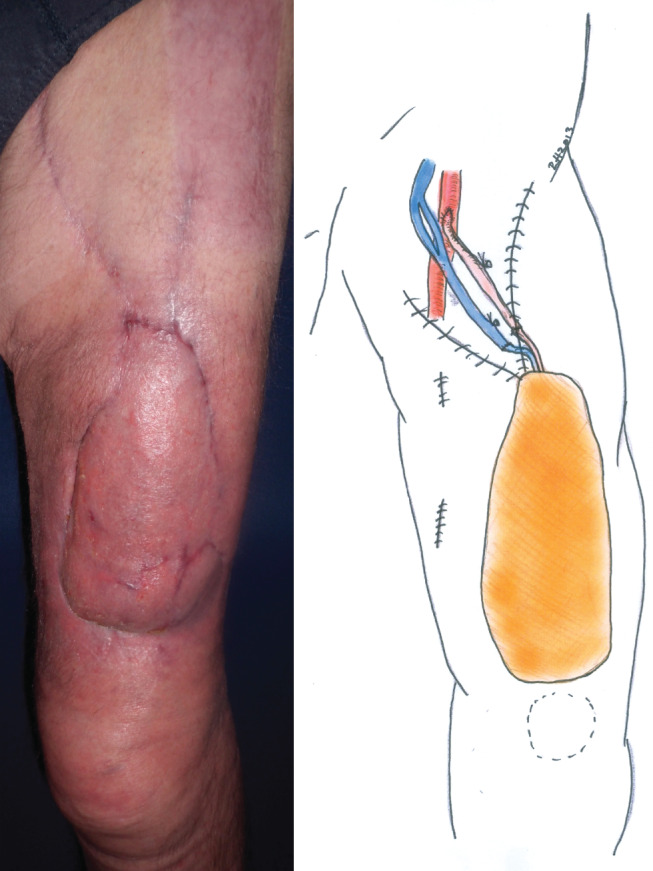
Result 3 months after free‐flap transfer.
Discussion
As long as techniques like tissue engineering 6, 7 are not applicable to replace endogenous tissue for defect reconstruction in daily clinical routine, the plastic surgeon has to deal with the distinct advantages and disadvantages of the chosen flap for reconstruction. As outlined above, in our case, the latissimus dorsi flap probably represents the more convenient flap but comes along with a relative high risk of postoperative haemorrhage at the donor site, which we thought to be inappropriate for our patient because of his co‐morbidities. Simple split‐skin grafting failed because of the chronic irradiated wound. Radiation injury occurs in about 95% of patients receiving radiation therapy and ranges in severity from a mild erythaema to a moist desquamation and ulceration 8. Despite thorough and repeated wound debridement, the bacterial colonisation could not be eliminated, maybe due to a persisting biofilm 9. In order to stop the vicious circle, a free‐flap reconstruction seemed to be the best option. As – due to poor perfusion of the most cranial muscle section – parts of the flap had to be discarded and there were no alternative recipient vessels outside the irradiated area close enough to the defect, the shortened rectus abdominis muscle flap had no sufficient length to cover the very distant part of the defect. Only the unscheduled emergency interdisciplinary approach between plastic and vascular surgeons allowed the successful reconstruction of the defect. In the past, the principle of combinations of microvascular flap transfer and vascular reconstruction has been described in case of scheduled interdisciplinary approaches 3, 4.
In the recent literature, there are discussions whether to perform free‐flap reconstruction in combination with an AV‐loop using a one‐ or two‐stage procedure. Supporters of a two‐stage procedure argue that this approach divides the case into two more manageable procedures, which ensures each respective surgical team adequate time to perform their part of the procedure. Furthermore, in a two‐stage procedure, the AV‐loop can be observed by means of, for example, Doppler sonography for several days to ensure that it has adequate flow 10. In our case, we needed only a short AV‐loop that was very proximal to the leg with a large diameter, which comes along with a comparable low risk. Therefore, we decided to do a one‐stage procedure and to complete the whole operation.
This successful emergency procedure of an AV‐loop for free‐flap salvage suggests that this technique may be a helpful tool as a last resort in complex wound reconstruction of the thigh.
References
- 1. Lineaweaver W, Akdemir O, Schleich A. Management strategies following microsurgical flap failure. Microsurgery 2010;30:61–3. [DOI] [PubMed] [Google Scholar]
- 2. Taeger CD, Horch RE, Dragu A, Beier JP, Kneser U. Perforator flaps. A new era in reconstructive surgery. Chirurg 2012;83:163–71. [DOI] [PubMed] [Google Scholar]
- 3. Kneser U, Arkudas A, Beier JP, Dragu A, Stubinger A, Lang W, Horch RE. Extended skin and soft tissue defects after vascular wounds: plastic surgical concepts. Zentralbl Chir 2013;138:536–42. [DOI] [PubMed] [Google Scholar]
- 4. Horch RE, Lang W, Beier JP, Kneser U. Differential indication for autologous bypasses in microsurgical extremity reconstruction. In: Jacobs M, editor. Prevention and management of vascular complications. 2011:175–82. [Google Scholar]
- 5. Beier JP, Horch RE, Dragu A, Arkudas A, Kneser U. Perforator‐based monitoring skin islands in free muscle flaps: teaching old dogs new tricks. Plast Reconstr Surg 2012;129:586e–7. [DOI] [PubMed] [Google Scholar]
- 6. Horch RE, Kneser U, Polykandriotis E, Schmidt VJ, Sun J, Arkudas A. Tissue engineering and regenerative medicine ‐where do we stand? J Cell Mol Med 2012;16:1157–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rath SN, Strobel LA, Arkudas A, Beier JP, Maier AK, Greil P, Horch RE, Kneser U. Osteoinduction and survival of osteoblasts and bone‐marrow stromal cells in 3D biphasic calcium phosphate scaffolds under static and dynamic culture conditions. J Cell Mol Med 2012;16:2350–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ryan JL. Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol 2012;132(3 Pt 2):985–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bradley BH, Cunningham M. Biofilms in chronic wounds and the potential role of negative pressure wound therapy: an integrative review. J Wound Ostomy Continence Nurs 2013;40:143–9. [DOI] [PubMed] [Google Scholar]
- 10. Lind B, McCarthy W, Derman G, Jacobs C. Arteriovenous loop grafts for free tissue transfer. Vasc Endovascular Surg 2012;46:30–3. [DOI] [PubMed] [Google Scholar]


