Abstract
A 61‐year‐old patient was affected by flaccid paraplegia for 20 years because of post‐traumatic medullar injury caused by an accidental fall, with stage IV sacral pressure ulcer for 3 years. The patient later developed stage IV sacral pressure ulcer. After 6 months, a new granulation tissue formation appeared in the wound and a reduction of its diameter was observed (length 20 cm, width 15 cm, depth 5 cm). We therefore treated the wound with PRP (platelet rich plasma) intra‐lesion and peri‐lesional injections. The wounds were covered with three‐dimensional polymerised hyaluronic acid medicated biologic dressing. After the surgery, a moderate reduction in diameter and the depth was observed. Super‐oxidised solution (SOS‐Dermacyn) was applied to control infection locally together with negative pressure to control the exudate and the local bacteremia, to avoid infectious complications without application of systematic antibiotic therapy.
Keywords: Dermacyn, VAC therapy, Pressure ulcer
Introduction
A 61‐year‐old patient was affected by flaccid paraplegia for 20 years because of post‐traumatic medullar injury, level D10–D11, caused by an accidental fall, with stage IV sacral pressure ulcer for 3 years. The patient has come to our attention; he has already undergone surgery in the other structure with local gluteal flap to cover the defect. The patient subsequently developed a stage IV sacral pressure ulcer. Since 2008, the patient was treated in our department: Plastic and Reconstructive Surgery at the University of Rome “Tor Vergata”. The patient was initially medicated three times a week with a Polyurethane Sterile Foam Dressing. Based on our protocol, similar protocol to T.I.M.E., the patient underwent a photographic follow‐up; periodic wound culture was performed to determine how to treat the infection with an antibiotic therapy. Moreover, a fistulography with contrast medium was performed, and the result did not reveal any evidence of fistulous tract. After 6 months, a formation of new granulation tissue appeared in the wound and a reduction of its diameter was observed (length 20 cm, width 15 cm, depth 5 cm) (1, 2, 3). We then decided to treat the wound with intra‐lesion and peri‐lesional PRP (platelet rich plasma) injections. The wounds were covered with a three‐dimensional polymerised hyaluronic acid medicated biologic dressing (1, 2). After the operation, a moderate reduction of diameter and depth was observed. However, continuing with the medication and during the antibiotic treatment, no signs of infection were observed. When antibiotics treatment was not used, there was a recurrence of the infection signs in the wound bed, such as an increase of exudate, change of colour, hyperaemia, periwound maceration and fever. The goals of treatment of pressure ulcers should be resolution of infection and promotion of wound healing. A combination of surgical debridement and medical interventions may be required (3).
Figure 1.

Preoperative view: at time 0 days.
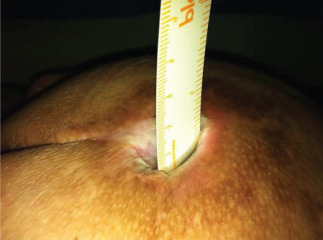
Figure 2.

Dermacyn® application and Polyurethane Sterile Foam Dressing with negative pressure.
Figure 3.
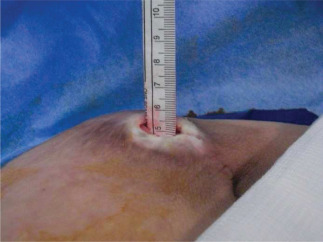
Preoperative view: depth 5 cm.
Given the patient's general conditions (substitution of aortic valve), it was impossible to prolong the antibiotic therapy for longer than 20 days. Given the difficulties and side effects resulting from systemic antibiotic therapy, in particular, repeated episodes of diarrhoea, we tried an alternative for the control of local bacterial infection in the wound. In addition, the decubitus position was predisposed to the continuous contamination by faecal and urine bacteria in this condition. Dermacyn® was applied to check the infection locally together with the negative pressure to control the exudate and the bacteremia, to avoid the infection complications without applying systematic antibiotic therapy, Dermacyn® was applied on the wound for 15–20 minutes and a Polyurethane Sterile Foam Dressing with negative pressure (80 mmHg) was positioned to cover the wound (Figure 2).
Discussion
The sacral pressure ulcer is a locally damaged area of the skin and subcutaneous tissue caused by pressure, traction, friction and/or a combination of these (working definition EPUAP). Contributions to the onset of pressure ulcer risk factors both local (thermal changes, moisture, maceration, dehydration), and systemic (age, immobility, malnutrition, chronic systemic diseases, acute diseases, vascular diseases, medical–surgical, anaemia, were toxic, hypoalbuminosis). A pressure ulcer is an area of skin that breaks down when constant pressure is placed against the skin and reduces blood supply to that area. After an extended amount of time with decreased tissue perfusion, ischaemia occurs and can lead to tissue necrosis and in the worst case it can reach muscles and bones. Factors that can contribute to the formation of pressure ulcers could be intrinsic (systemic disease, medication, malnourishment, age, dehydration, lack of mobility, incontinence, skin condition, weight) and extrinsic (external influences which cause skin distortion, pressure, shearing forces, friction, moisture) 4, 5.
Pressure ulcers can form anywhere on the body. The most frequent formations are in sacral area (30–40%), heel (15–20%), ischiatic region (5–15%), great trochanter (10–15%), malleolar region (6–7%).
A pressure ulcer is localised injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction. A number of contributing or confounding factors are also associated with pressure ulcers; the significance of these factors is yet to be elucidated (NPUAP, 2007). The ulcers are classified in four stages, starting from a normal erythaema which is characterised by an intact skin with non‐bleachable redness of a localised area usually over a bony prominence (stage I), to the worst case with a full thickness tissue loss with exposed bone, tendon or muscle. Eschar may be present on some parts of the wound bed (stage IV).
The European guidelines for pressure ulcer wounds treatment are based on the ‘classes of risk’ include: control of incontinency and moisture, education and training of the patient and family, evaluation of the risk, anti‐decubitus system, adequate diet and food tips, personal hygiene, distribution of weight, periwound skin care and control of pain 6, 7, 8.
Device with negative pressure
The VAC technique is a safe, easy and effective means in chronic wound care management (9), it is a sub‐atmospheric pressure device consists of a polyurethane foam dressing that can be either open‐cell honeycomb drainage (green) or a honeycomb structure with cells mixed open and closed (white) draining and thermal insulation. 10, 11. The polyurethane foam, shaped and inserted into the cavity, subjected to vacuum, allows for debriding tissue and stimulates the granulation tissue. Subsequently, the wound is covered with a hydrocolloid adhesive provided with central opening to allow the attachment of the device, which generates the negative pressure, and the subsequent drainage of the fluids of secretion 12, 13. The secondary hydrocolloid dressing protects the surrounding skin and is permeable by gas and water vapour, while maintaining a moist environment ideal for the movement of fibroblasts and macrophages from the periphery to the centre of the lesion, with the formation of points where the cells that participate in neo‐angiogenesis are deposited to stimulate the new granulation tissue. The dressing is connected to a suction cup that allows you to adjust the negative pressure and allows using it in a continuous or intermittent (14).
Dermacyn wound care
Dermacyn® Wound Care is a super‐oxidised solution used for debridement, irrigation and moistening of acute and chronic wounds, ulcers, cuts, abrasions and burns. Through reducing the microbial load and assisting in creating a moist environment, it enables the body to perform its own healing process.
This solution is the result of superoxide electrolysis of pure water and sodium chloride (15).
In wounds treated with, Dermacyn® starts a process of phagocytosis, which destroys pathogenic microorganisms. Dermacyn® surrounds the bacterium and attacks the cell wall, proteins contained in it are denatured by reactive oxygen species that causes cellular lysis. Come result of osmosis the cell wall breaks and are disintegrated microorganisms are destroyed.
Dermacyn® is immediately ready for use without any dilution, the product must be applied directly on the area to be treated by dipping, spraying spray irrigation pressure or through sterile gauze. (16).
The treatment consists in the dip up to 15 minutes daily during the initial phase, in the opinion of the physician responsible, wetting and/or spray at each dressing change according to the specific needs of the individual case. This solution and safe because it does not damage the tissues, not toxic, does not irritate the skin, ready for use without dilution or mixing, is stable and valid for a period of 1 year, neutral pH between 6·2 and 7·8, colourless so it masks the necrotic tissue. (17).
Conclusion
To evaluate the efficacy of the combination Dermacyn® and NPWT, we assessed the following parameters: reduction of exudates with a change in colour and reduction of odour, infection and the size of pressure ulcer (Table 1). The evaluation of improvements of the wound, in terms of size, was evaluated at a time of 50 days (Table 2). The dressings were performed every 5 days.
Table 1.
Results
| Date | NPWT + Dermacyn |
|---|---|
| Exudate | < post 48 hours, disappearance in five applications |
| Odour | < post 1 applications |
| Infection | < post 3 applications |
| Ulcer diameter | <1 cm2 for every applications |
| Ulcer depth | <post 3 applications |
| Granulation tissue growth | Good |
| Healing time | <30% compared to others protocols |
| Colour | Colour change from green to yellow |
Table 2.
Decrease in ulcer depth in relation to dressing changes performed every 5 days
| Wound depth | 5 days | 10 days | 15 days | 20 days | 25 days | 30 days | 35 days | 40 days | 45 days | 50 days |
|---|---|---|---|---|---|---|---|---|---|---|
| 5 cm | 4·8 cm | 4·5 cm | 4·2 cm | 3·8 cm | 3·3 cm | 2·7 cm | 1·9 cm | 1·4 cm | 0·9 cm | 0·5 cm |
To conclude, we noticed an immediate reduction of exudate with decreased maceration of surrounding skin (4, 5).
Figure 4.

Postoperative view: depth 0·5 cm.
Figure 5.
Postoperative view: at time 50 days.
The bacteriostatic action of NPWT has been enhanced by the addition of Dermacyn®. It enabled an immediate (as early as the first application) dispersal of the odour and exudates, change in colour, from green with yellow, also the dissipation of periwound maceration and hyperaemia to allow the growth of peri‐lesional and bottom edges of the ulcer and the appearance of granulation tissue.
The association of the two has ensured a significant reduction in healing time by controlling the local bacterial infection until the complete elimination of regional debridement of the necrosis with formation of granulation tissue.
References
- 1. de Leon JM, Driver VR, Fylling CP, Carter MJ, Anderson C, Wilson J, Dougherty RM, Fuston D, Trigilia D, Valenski V, Rappl LM. The clinical relevance of treating chronic wounds with an enhanced near‐physiological concentration of platelet‐rich plasma gel. Adv Skin Wound Care 2011;24:357–68. [DOI] [PubMed] [Google Scholar]
- 2. Cervelli V, De Angelis B, Lucarini L, Spallone D, Balzani A, Palla L, Gentile P, Cerulli P. Tissue regeneration in loss of substance on the lower limbs through use of platelet‐rich plasma, stem cells from adipose tissue, and hyaluronic acid. Adv Skin Wound Care 2010;23:262–72. [DOI] [PubMed] [Google Scholar]
- 3. Iori I, Pizzini AM, Arioli D, Favali D, Leone MC. Infected pressure ulcers: evaluation and management [Review. Italian]. Infez Med 2009;17 Suppl 4:88–94. [PubMed] [Google Scholar]
- 4. Kerihuel JC. Effect of activated charcoal dressings on healing outcomes of chronic wounds. J Wound Care 2010;19:208–14. [DOI] [PubMed] [Google Scholar]
- 5. Kaitani T, Tokunaga K, Matsui N, Sanada H. Risk factors related to the development of pressure ulcers in the critical care setting. J Clin Nurs 2010;19:414–21. [DOI] [PubMed] [Google Scholar]
- 6. Scevola S, Nicoletti G, Brenta F, Isernia P, Maestri M, Faga A. Allogenic platelet gel in the treatment of pressure sores: a pilot study. Int Wound J 2010;7:184–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thiessen FE, Andrades P, Blondeel PN, Hamdi M, Roche N, Stillaert F, Van Landuyt K, Monstrey SJ. Flap surgery for pressure sores: should the underlying muscle be transferred or not? Plast Reconstr Aesthet Surg 2010;64:84–90. [DOI] [PubMed] [Google Scholar]
- 8. Makai P, Koopmanschap M, Bal R, Nieboer AP. Cost‐effectiveness of a pressure ulcer quality collaborative. Cost Eff Resour Alloc 2010;8:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Citak M, Backhaus M, Meindl R, Muhr G, Fehmer T. Rare complication after VAC‐therapy in the treatment of deep sore ulcers in a paraplegic patient. Arch Orthop Trauma Surg 2010;130:1511–4. [Epub 20 March 2010]. [DOI] [PubMed] [Google Scholar]
- 10. Nather A, Chionh SB, Han AYY, Chan PPL, Nambiar A. Effectiveness of vacuum‐assisted closure (VAC) therapy in the healing of chronic. Ann Acad Med 2010;39:353–8 [PubMed] [Google Scholar]
- 11. Gorecki CA, Brown JM, Briggs M, Nixon J. Evaluation of five search strategies in retrieving qualitative patient‐reported electronic data on the impact of pressure ulcers on quality of life. J Adv Nurs. 2010;66:645–52. [DOI] [PubMed] [Google Scholar]
- 12. Agha‐Mohammadi S, Hurwitz DJ. Enhanced recovery after body‐contouring surgery: reducing surgical complication rates by optimizing nutrition. Aesthetic Plast Surg 2010;34:617–25. [DOI] [PubMed] [Google Scholar]
- 13. Cho I, Noh M. Braden Scale: evaluation of clinical usefulness in an intensive care unit. J Adv Nurs 2010;66:293–302. [DOI] [PubMed] [Google Scholar]
- 14. Napoli B, Benigno A, D'Arpa N, Amico M, Conte F. Local treatment of burns with honeycomb expanded polyurethane (Ligasano). Ann Burns Fire Disaster 2008;XXI:1. [PMC free article] [PubMed] [Google Scholar]
- 15. Gonzales‐Espinosa D, Perez Romano L, Guzman‐Soriano B, Arias E, Bongiovanni CM, Gutierrez AA. Effects of PH neutral, superoxidised solution on human dermal fibroblasts in vitro. Int Wound J 2007;4:241–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Paola LD, Brocco E, Senesi A, Merico M, de Vito D, Daros R. Super‐oxidized solution (SOS) therapy for infected diabetic foot ulcers. Wounds 2006;18:262–70. [Google Scholar]
- 17. Nelson EA, O'Meara S, Golder S, Dalton J, Craig D, Iglesias C. Systematic review of antimicrobial treatments for diabetic foot ulcers. Diabet Med 2005;23:348–59. [DOI] [PubMed] [Google Scholar]


