Abstract
A 40‐year‐old female presented with history of swelling at the upper and middle of the left leg since 6 months was confirmed as post cancer surgery non healing wound not responding to conventional antibiotic therapy and local wound care in an operated case of synovial sarcoma of the knee, monophasic fibrous type with no lung metastasis. Post surgical non healing wound not responding to conventional therapy was treated successfully with local application of 3% citric acid ointment for 25 days.
Keywords: Post surgical non healing wound, Synovial sarcoma of the knee, Citric acid treatment
INTRODUCTION
Wound healing in cancer patients is a matter of critical importance. Wound management in cancer patients is complicated by tumour biology, the patient's disease state and additional comorbidities. The degree of damage to surrounding tissue impacts overall wound healing. Radiation therapy following surgical resection to control local–regional disease has negative healing effects because of local tissue fibrosis and vascular effects. Chemotherapeutic agents either administered alone or as combination therapy with surgery and radiation, may have detrimental effects on the cells involved in the process of wound healing. In addition, the diminished nutritional status in cancer patients is an important factor contributing to inability of wound to heal after surgical procedure. Thus the multiple treatment modalities such as surgery, radiation therapy and chemotherapeutic regimens interact and impact their abilities to heal wounds delaying the wound healing process in cancer patients 1, 2, 3, 4.
THE CASE
We report a case of post cancer surgery non healing wound not responding to conventional antibiotic therapy and local wound care in an operated case of synovial sarcoma of the knee. This post surgical non healing wound was treated successfully with local application of 3% citric acid ointment for 25 days.
A 40‐year‐old female presented with history of swelling at the upper and middle of the left leg since 6 months. She also complained of pain while walking. She gave history of surgery performed in the same area 13 years ago in which upper end of the left fibula was excised. However, she did not have any record of the histopathology reports and treatment taken at that time.
She was investigated this time with X‐ray of the local part, which showed extensive soft tissue component along with absence of fibular head and destruction of upper end of remaining fibula. The magnetic resonance imaging showed that the popliteal vessels were displaced by the soft tissue mass but not infiltrated. The posterolateral muscle compartment was involved. Patient did not have any locoregional lymphadenopathy. Computerised tomography scan of the chest showed no lung metastasis. A core needle biopsy showed histopathology of synovial sarcoma, monophasic fibrous type (Figure 1).
Figure 1.
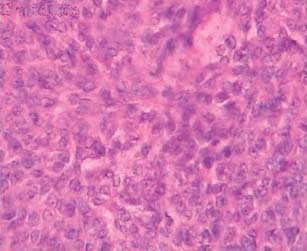
Microscopy of monophasic synovial sarcoma with fibrosarcomatous appearance (H&E, 40×).
On the basis of histopathology findings, the patient was operated. The skin incision included the previous scar and suture marks. The soft tissue mass was excised with wide muscle margins all around along with the involved length of fibula. The common peroneal nerve was euthanised as it was going through the mass. The wound (approximately 16 cm in length) was closed with a suction drain. Patient received injection ceftriaxone 1 g BD, injection amikacin 750 mg OD and injection metrogyl 100 cc TDS as antibiotic cover for 5 days. Patient was discharged with advice to take radiation therapy.
Postoperatively after a week, she came back with complain of pus discharge from operation site. On examination, there was purulent collection in the wound. Lower end of the wound was opened and daily dressing using betadine solution was performed for 4 weeks. Patient did not respond to this therapy and the purulent discharge continued (Figure 2). The culture studies of purulent discharge yielded 16 colonies of Staphylococcus aureus resistant to ampicillin, amikacin, cefoperazone, ceftazidime, ciprofloxacin, gentamicin, gatifloxacin and methicillin.
Figure 2.

Operated case of synovial sarcoma of the knee – before application of citric acid ointment.
After taking her written consent, a decision to use 3% citric acid ointment, prepared in white soft paraffin (100% pure white soft paraffin) by mechanical mixing in a mortar by taking all sterile precautions. The citric acid ointment, instead of betadine (used earlier as a topical agent in this case), was applied daily once after irrigation and cleaning of wound with normal saline and wound was dressed with sterile pad. This treatment modality was used until the wound healed completely. The wound healed completely in 25 applications of citric acid ointment in 25 days (3, 4).
Figure 3.

Operated case of synovial sarcoma of the knee – after 16 applications of citric acid ointment.
Figure 4.

Operated case of synovial sarcoma of the knee – after 25 applications of citric acid ointment.
DISCUSSION
The use of citric acid has been reported for the effective management of chronic wound infections not responding to conventional injectable or oral antibiotic therapy and local wound care management 4, 5, 6, 7.
It has been found that citric acid has antibacterial activity and effectively controls the infection. This antiseptic property may be because of lowering of pH that makes an environment unsuitable for growth and multiplication of bacteria causing wound infections. It also enhances epithelisation, which is a major factor in wound healing. Hydration, oxygenation and removal of dead tissue ensure good epithelisation. Histological studies showed that citric acid has been found to actuate the wound healing process by boosting fibroblastic growth and neo‐vascularisation, which in turn increases microcirculation of wounds that enables the formation of healthy granulation tissue thereby leading to faster healing of wound (8). All these actions increase migration of epithelial cells from surrounding skin and epithelisation acts as stimulus for laying of ground substance.
In this case, as only 16 colonies were grown, infection was not a significant component as per the standard criteria of infection (9). The degree of damage produced by surgery may be the more important cause rather than infection for non healing of wound for weeks together in spite of injectable antibiotic therapy and daily local wound care.
Successful healing of wound in a cancer patient is an indication that in addition to its role in controlling a variety of bacterial infections as a topical agent, citric acid may also act as a stimulator for wound healing in patients with damaged tissue. The results of this study indicate that when a healing of wound is a matter of great concern because of one or other reasons, one can think of citric acid therapy, which could be reliable and effective option for management of non healing wounds, even in cancer patients.
REFERENCES
- 1. Payne WG, Naidu DK, Wheeler CK, Barkoe D, Mentis M, Salas RE, Smith DJ, Robson MC. Wound healing in patients with cancer. Eplasty 2008;8. [PMC free article] [PubMed] [Google Scholar]
- 2. Bernstein EF, Sullivan FJ, Mitchell JB, Salmon GD, Glatstein E. Biology of chronic radiation effects on tissues and wound healing. Clin Plast Surg 1993;20:435–53. [PubMed] [Google Scholar]
- 3. Rudolph R, Arganese T, Woodward M. The ultrastructure and etiology of chronic radiotherapy damage in human skin. Ann Plast Surg 1982;9:282–92. [DOI] [PubMed] [Google Scholar]
- 4. Dobbs WGH. A statistical study of the effects of roentgen rays on wound healing. Am J Roentgenol 1939;41:625–32. [Google Scholar]
- 5. Nagoba BS, Deshmukh SR, Wadher BJ, Mahabaleshwar L, Gandhi RC, Kulkarni PB, Mane VA, Deshmukh JS. Treatment of superficial pseudomonal infections with citric acid – an effective and economical approach. J Hosp Infect 1998;40:155–157. [DOI] [PubMed] [Google Scholar]
- 6. Nagoba BS, Wadher BJ, Chandorkar AG. Citric acid treatment of non‐healing ulcers in leprosy patients. British J Dermatology 2002;146:1101. [DOI] [PubMed] [Google Scholar]
- 7. Nagoba BS, Wadher BJ, Rao AK, Kore GD, Gomashe AV, Ingle AB. Simple and effective approach for the treatment of chronic wound infections caused by multiple antibiotic resistant Escherichia coli. J Hosp Infect 2008;69:177–80. [DOI] [PubMed] [Google Scholar]
- 8. Nagoba BS, Gandhi RC, Wadher BJ, Potekar RM, Kolhe SM. Microbiological, histopathological and clinical changes in chronic wounds after citric acid treatment. J Med Microbiol 2008;57:681–2. [DOI] [PubMed] [Google Scholar]
- 9. Robson MC. Infection in the surgical patient: an imbalance in the equilibrium. Clin Plast Surg 1979;6:493–503. [PubMed] [Google Scholar]


