Abstract
This is the second part of the article based on the thesis work for a Masters of Science in Wound Healing and Tissue Repair, Cardiff University, to develop an evidence‐based protocol for the care of pilonidal sinus wounds (PSWs) healing by secondary intent, using a modified Reactive Delphi process. The sample included surgeons, clinic physicians, nurses and enterostomal therapy nurses experienced in the care of these wounds. Item generation involved an extensive review of the literature to identify key aspects of evidence‐based wound care essential to wound healing, infected wounds and pilonidal wounds healing by secondary intent and drawing on clinical experience. The participants responded via an electronic Delphi website, using a 4‐point Likert rating scale and a ranking system. Comments were invited. Feedback was provided to the participants at the end of each round, that included comments, consensus scores, content validity index and additional information that provided rationale and references, or minor revision if requested. This project successfully achieved the objectives, which were to identify the areas of care that negatively or positively influences healing of postoperative PSWs and to inform, educate and broaden the considerations regarding these factors for health care professionals.
Keywords: Consensus protocol, Modified Reactive Delphi, Pilonidal sinus wounds
INTRODUCTION
At the time of this thesis research, no published evidence‐based guidelines were found for care of pilonidal sinus wounds (PSWs) healing by secondary intention, or following failed primary closure. The goal therefore was to seek consensus about what constitutes best practice care for postoperative and infected PSWs healing by secondary intent and to create a treatment protocol.
MATERIALS AND METHODS
A modified Reactive Delphi (MRD) was chosen as the method with which to gain consensus. The aim of a Delphi procedure is to determine the amount of agreement among participants (1), and can be used as a reliable consensus method for health care research where little supportive research evidence exists, such as in the case of PSWs 2, 3. In a MRD, the researcher performs an extensive literature review, based on published research and knowledge drawn from experience. Clinical observation precedes theory, research or the opinion of experts and the experiential knowledge of the researcher can guide some of the search for literature (4). The results are synthesised to form the first round of questions 2, 3. The participants respond, drawing on opinions and/or clinical experiences, using a series of anonymous iterative surveys 2, 3, 5. A literature review was performed (see part 1 of this article) to identify the principle factors thought to influence the healing or delayed healing of postoperative and infected PSWs. These were synthesised into a 81‐item questionnaire for round 1. A diagrammatic representation of the pilot and the main study is shown in Figure 1.
Figure 1.
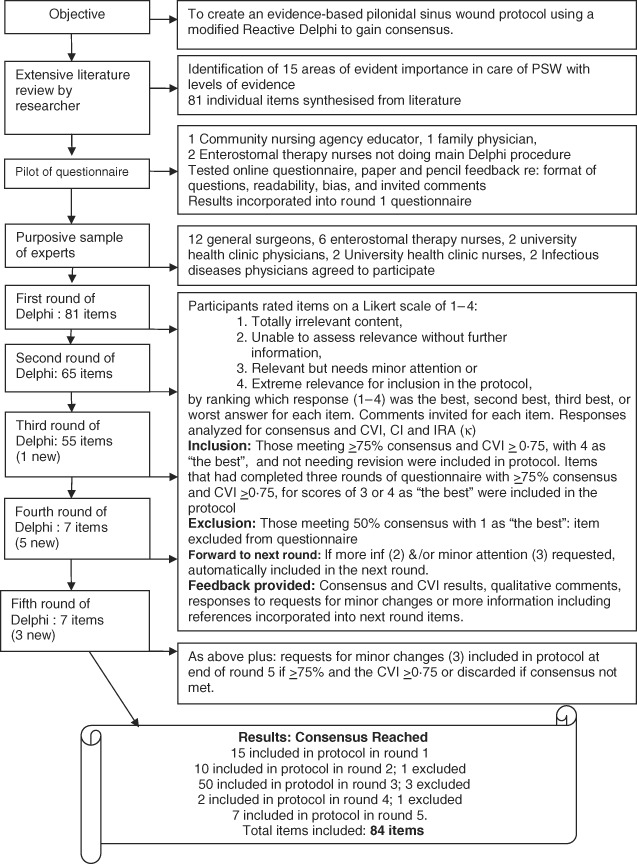
Delphi process for study (13).
Selection of participants
A minimum of five participants is considered to be sufficient to overcome chance agreement to endorse an item as content valid (6). The purposive sample consisted of health care professionals involved in the treatment and care of individuals with PSWs within the geographical health region in which the researcher worked. They either knew the researcher or knew her because of mutual patients with PSWs. This included 12 general surgeons, 2 infectious diseases specialists, 6 registered nurses (RNs) enterostomal therapy nurses and 4 university health clinic physicians and clinic RNs, who expressed intent in participating in the questionnaire. This was a diverse, heterogeneous population with regard to formal education, expertise in wound care and location of work, considered best when exploring areas of uncertainty, such as this PSW topic (7). There was no requirement for the participants to estimate their own degree of expertise for each item, or for the questionnaire in total. The incentive to participate was the opportunity to be involved in the development of a consensus protocol that would embed evidence‐based practices for the care of PSWs. The informed consent signed by participants indicated that they could withdraw from this study at any time.
Item generation
Over the course of the five rounds, there were 89 items, creating a risk for loss of concentration and attrition of participants (8), although precedent existed for successful large Delphis 9, 10. The participants were asked to add any additional items not captured in the questionnaire in round 1 and to comment on any item that they wished to in each round, although not compulsory. At the beginning of each round, the researcher outlined the inclusion criteria for the protocol and provided feedback consisting of additional information (including references) when requested, the consensus and content validity index (CVI) results and qualitative comments from the previous round. If necessary, the researcher could add new items between rounds (11).
The questionnaire used free online software called the Delphi Decision Aid (12), affiliated with the Wharton Business School at the University of Pennsylvania. This allowed text‐only questions, and a 4‐point Likert ordinal rating scale with descriptors similar to Lynn's (6), as well as a ‘ranking’ option. Ranking forces the participants to be discriminant in their responses (4). It ensured anonymity and confidentiality of the participants' responses, immediate rating results with comments and dispersion of ranking for each item. The researcher only knew who had responded to each round, but not what their choices were or how many items they responded to. Participants needed to answer each question to go to the next item. Reminders were generated, and deadlines extended in rounds 1–3. In rounds 4 and 5, the researcher set a more realistic deadline (Figure 1).
Ethical considerations
Ethics approval was obtained from the Ethics Review Board of the local Community Care Access Centre through which most of the community patients with PSWs are seen. Additional approval was necessary through the Office of Research Ethics and Grants, for the local university health clinic to participate.
Analysis
A criticism of many Delphi studies is the lack of consistent measure of statistical analysis other than consensus (13), although there is no agreement as to the best method of analysis 7, 13. The attainment of consensus does not necessarily mean that the answer is correct. The tendency of researchers using Delphi to assign an arbitrary criterion for determining consensus is criticised as a weakness, when using descriptors such as ‘unimportant’, ‘high’ or ‘strong’(14). A more reliable and transparent process is accomplished by assigning a numerical value as the consensus level for inclusion, prior to the start of the first round. Opinions of what this should be differ widely, with as little as 51% agreement recommended (2).
There are three possible scenarios influencing the reliability of consensus in a Delphi:
-
•
When the number of participants falls in subsequent rounds, consensus may be the result of attrition (15).
-
•
Convergence of opinion indicates a true acceptance of the rationale behind the item as the rounds continue, which is ideal 2, 15.
-
•
Conformance, where participants alter their answer to conform to that of the other participants based on the previous round, not on their own opinion (16).
Consensus served two purposes in this study. The Consensus agreement was defined as between 50% and 100% of the participants ranking the item with a score of 3 (relevant but needs minor attention) or 4 (extreme relevance for inclusion in the protocol) as ‘the best' for each item, dichotomising the results. The number of times that each of the four possible scores ranked ‘the best' was an indication of the amount of agreement among participants. Any items that had a score of 2 (more information) or 3 (minor attention) in rounds 1, 2 and 4 were required to go to the next round, regardless of the consensus result (6). The second use of consensus was as part of the inclusion and exclusion criteria for the protocol. If an item had 75% consensus indicating that the score of 4 was ‘the best', a CVI of 0·75, and did not need more information or revision, it was included in the protocol. Eliminated items did not meet the 50–100% consensus, and did not need either more information or minor attention.
The researcher chose three additional measures of analysis. The CVI determines if the items contained within the questionnaire were relevant to the topic 4, 6. Consensus occurs as the variance of the responses decreases over the course of the rounds (17). Confidence intervals (CI), the range of two values (upper and lower), can be used to compare the distribution or variance of responses in a Delphi procedure (18). A high (>0) CI will validate a high level of importance, or agreement, so that a high CI indicates high consensus (19). A wide CI may also confirm that the heterogeneous participant panel represented different levels of education and wound knowledge, or that one or more participants were not using the questionnaire correctly.
Inter‐rater agreement (IRA) using a weighted Cohen's coefficient kappa (κ), measures the extent to which the participants are reliable in their ratings (20), how they understand the rating task (21), and if they used the rating scale in a similar manner (22). IRA represents the sum of weighted frequencies corrected for chance (4). This is an important additional measure of consensus and content validity because of concern that dichotomising the responses increases the possibility of agreement by chance alone by 50% (11). IRA is especially useful when the rating scale contains verbal descriptors of the categories, such as those used in this study, although interpretations can be difficult (11). κ is sensitive to bias among the participants, to the sample size and to the distribution of the data, so that a low κ statistic may occur in spite of other higher consensus values for the same item.
The results of the CI and κ analysis would determine how closely the participants agreed or disagreed, but would not be part of the decision to include or eliminate from the protocol. This study did not evaluate the influence of asynchronous interaction of the participants.
RESULTS
Attrition occurred almost immediately. Whilst the response rate increased over the course of the five rounds, from 52% in round 1 to 100% in rounds 4 and 5, the actual number of participants decreased from 12 to 7. Many of the items had scores of 2 (unable to assess relevance without further information) or 3 (relevant but needs minor attention) without specific directions as to what was needed, but there were a number of qualitative comments. A sample of the comments appears in Table 1. Verbal comments from the two general surgeons who did participate included the fact that participation was making them think about their patients with PSW in a new way, with more awareness of issues such as friction in the natal cleft.
Table 1.
Sample of data from qualitative comments
| Microbiology of infected PSW |
| The microbiology of a pilonidal sinus culture had almost no relevance in respect to treatment. |
| Validity of signs and symptoms of localised chronic wound infection and deeper wound infections |
| ‘Would be good to give example of’ does not have good tensile strength, some people may not understand the term. For example, ‘pulls apart easily’. |
| Action based on signs and symptoms of infection |
| Need to add based on the sensitivities shown on the c&s of the semi‐quantitative swab. |
| Systemic antibiotics for PSW |
| This combination provides minimal Gram negative coverage. If no improvement by day 14, why not repeat culture and modify treatment based on results? |
| Topical antimicrobials to peri‐wound skin |
| Only needs to include the distance of the peri‐wound skin, for example, 10 cm. |
| Topical antimicrobials to wound bed |
| List some of the common bacteria found in PSWs that silver is effective against. |
| Local wound interventions |
| Is there any research to back this up, what is superficial undermining, less than what depth? |
| Optimal positioning for wound assessment and care |
| Have never used this position so I can not comment. |
| Wound cleansing |
| A few but not most silver dressing products require sterile water as an irrigation fluid. |
| Principles of moist wound healing |
| A point related to the need to individualise for each client. |
| Topical negative pressure wound therapy |
| The guidelines need to be broader to allow for the exceptions and also discussion with the physician because they may have a reasonable endpoint in mind for the wound. Think of our oncology clients who need wound closure to carry on with chemo, not likely for a pilonidal but. I like this guideline! |
| Peri‐wound skin care |
| Need to clarify the 5 cm strip, should be width from the wound. |
| Pain control |
| Need to provide a more specific statement. |
| Physical activities with pilonidal wounds |
| We know that friction and moisture are factors, the above information states no research has been carried out. |
| Nutrition and wound healing |
| Most people have a healthy diet and I would need to see more evidence that oral supplementation is a beneficial cost. |
| Patient education pre‐healing and post‐healing activities, nutrition and hygiene post‐healing hygiene |
| Knowledge promotes compliance and focus on what is achievable. None of my patients are going to lose weight because they have this process. |
PSW, pilonidal sinus wounds.
The number of items requiring minor attention, more information, included in the protocol or excluded in each round is shown in Figure 2. Requests for more information or minor attention decreased over the course of the rounds, while items meeting the inclusion criteria for the protocol increased.
Figure 2.
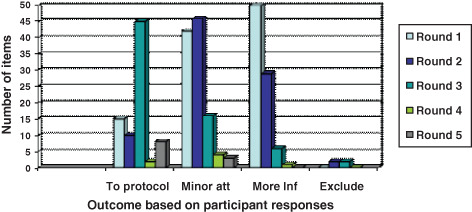
Summary of participants' responses all rounds.
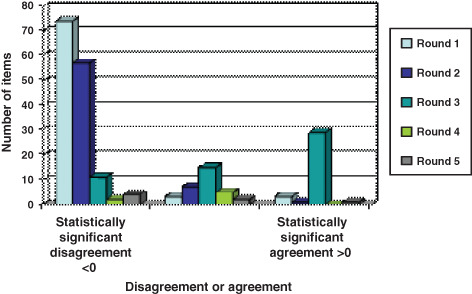
The results in all four data analysis methods (consensus, CVI, CI and IRA) generally improved over the course of the rounds. Figure 3 shows the consensus in each round. In round 1, only 8 items had 91–100% consensus, with the largest group of 27 items having 81–90%. Five items had <50% consensus, but continued in the rounds because they required more information or revision. Round 3 had the largest number of items with a 91–100% consensus. The total number of items having CVI >0·75 per round and the representative percentage (4, 5) were both calculated. In comparing the percentage of items having a CVI of 0·75–1·0 over the course of the rounds, the scores went from 75%, 83%, 96%, 86% and 100%, indicating high relevance of these items to the topic of PSW care.
Figure 3.
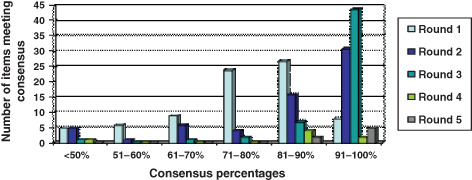
Consensus summary all rounds.
Figure 4.
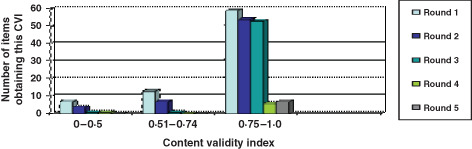
Content validity index summaries all rounds by number of items.
Figure 5.
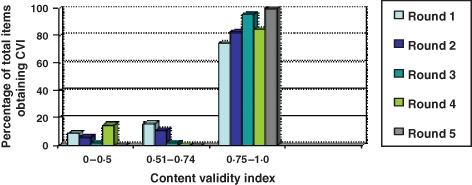
Content validity index summary all rounds by percentage of items.
The CI calculation was for 95%, which means that if this study was repeated 100 times, the researcher could be 95% confident that the CI would contain the mean response for that item, with a true value somewhere between the low CI and the upper CI (23). The null value for this study was zero. To calculate the CI, the number of times each of the Likert scale choices for each item were ranked ‘the best' (one) to ‘the worst' (four) were placed in a frequency distribution table found on the Vassar University website: http://faculty.vassar.edu/lowry/kappa.html. The CI results, comparing the distribution of responses, loosely follow the trend of the consensus levels for items receiving 91–100% in the first three rounds. CI remained narrow for most items throughout the first, second, fourth and fifth rounds, with most of the responses having a difference of 0·3–0·5 between the upper and lower CI. Round 3 was an exception with 58% having a CI upper and lower limit of 1·0, indicating perfect agreement (Figure 6). The responses of one participant seemed to indicate that they had the opposite opinion to others for several items. It is difficult to ascertain whether this individual truly disagreed, or whether they were using the ranking and rating scales incorrectly.
Figure 6.
Confidence interval summaries all rounds: null value = 0.
The same κ shareware from Vassar University calculated the unweighted κ results to provide the inter‐rater reliability analysis. Landis and Koch's (24) descriptors regarding the relative strength of κ agreement were used (Figure 7). The IRA ‘perfect agreement' scores combined with those with ‘almost perfect agreement', showed 16·4% in round 1 increasing to 80% in round 3, supporting the consensus results.
Figure 7.
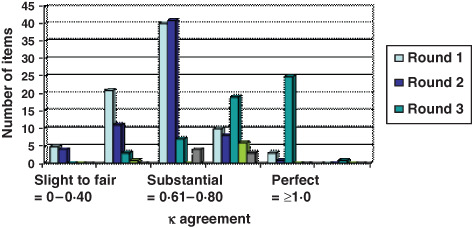
Inter‐rater agreement summary all rounds: relative strength of κ agreement (24).
Table 2 shows the number of new items for each topic per round. The choice of items for round 1 was dependent on the initial literature review, as outlined in part 1 of this article. Additional items were added based on comments or requests for more information from the participants. Four items were excluded from the protocol, three having level IIb evidence and one level IV. There was no apparent correlation between the level of evidence for the items and the inclusion or exclusion from the protocol.
Table 2.
Number of new items per round and results of study *
| Topic | Number of new items generated for this topic for round | Highest level of evidence | Number of items excluded | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||
| Microbiology of infected PSW | 1 | 0 | 0 | 0 | 0 | IIb | 0 |
| Validity of signs and symptoms of localised chronic wound infection | 6 | 0 | 0 | 0 | 0 | IIb | 0 |
| Action based on signs and symptoms of localised chronic wound infection | 2 | 0 | 0 | 0 | 0 | IIb | 0 |
| Validity of signs and symptoms of deeper wound infection | 7 | 0 | 0 | 0 | 0 | IIb | 0 |
| Action based on signs and symptoms of deeper wound infection | 2 | 0 | 0 | 0 | 0 | IIb | 0 |
| Antimicrobial usage for PSW: systemic antibiotics | 2 | 0 | 0 | 0 | 0 | IIb | 2 |
| Antimicrobial usage for PSW: topical antiseptics/antimicrobials | 4 | 0 | 0 | 0 | 0 | IV | 0 |
| Local wound interventions | 3 | 0 | 0 | 0 | 0 | IV | 0 |
| Optimal positioning for wound assessment and care | 1 | 0 | 0 | 0 | 0 | IV | 0 |
| Wound cleansing | 7 | 0 | 0 | 0 | 0 | Ia | 0 |
| Principles of moist wound healing | 18 | 0 | 0 | 0 | 0 | Ia | 1 |
| Topical negative pressure wound therapy | 3 | 0 | 1 | 5 | 3 | Ia | 1 |
| Peri‐wound skin care | 6 | 0 | 0 | 0 | 0 | Ib | 0 |
| Pain control | 3 | 0 | 0 | 0 | 0 | IV | 0 |
| Physical activities with PSW | 3 | 0 | 0 | 0 | 0 | IV | 0 |
| Nutrition and wound healing | 4 | 0 | 0 | 0 | 0 | Ib | 0 |
| Patient education | 8 | 0 | 0 | 0 | 0 | IIa | 0 |
PSW, pilonidal sinus wound. *Significance of the new items are given in bold.
DISCUSSION
The degree of immediate attrition of the participants at the start of the first round was a disappointment, but perhaps pragmatic. This was naively expected to be a short questionnaire of 15 to 20 topic items, but to represent each intervention or clinical observation as a single item, this was impossible. With 81 items, the time needed to complete each round increased with the addition of ‘more information’. This time commitment meant that many panel members, who truly wanted to participate, simply could not. Others did not like the online survey tool, or the mnemonics regarding signs of wound infection, and declined to participate. This contributed to a reduction in the sample size from a possible 24 to only 7. This was still adequate as per Lynn (6), but a larger sample would have had a stronger power for the results.
In this MRD process, where items forwarded to the next round contained additional information and references or revisions, it is difficult to distinguish whether the participants were conforming or converging. The researcher was the sole reviewer of the literature to develop the first round of the questionnaire. Although a recognised and acceptable step in this type of research 7, 25 it can engender concern about bias and leading questions (17). However, the CVI increased over the course of the rounds, supporting the content validity of the items. The CI results support Graham et al.'s (17) prediction that consensus increases as the variance decreases. As previously mentioned, there was an opportunity for participants to add items of their own in rounds 1 and 2, but they did not. The successful IRA (κ) results appear to downplay the effect of any bias by the researcher on the results. If the protocol had been limited to only items where a strong level (i.e. levels I–II) of research evidence existed, the scope of the project would have been of questionable utility.
As described in part 1 of this article, the levels of evidence adopted by the Registered Nurses' Association of Ontario as part of their Nursing Best Practice Guideline series (26) were used. These were chosen because they were familiar to health care professionals working in the Province of Ontario, Canada, where this study occurred. Many items had a high level of evidence about chronic wounds in general, but were not specific to PSWs. By completing this MRD, the researcher has gained level IV evidence, that of ‘expert committee’ for much of the topic area.
Although there was significant difference in the way the participants rated the item on the polymicrobial nature of PSW's, with the CI being below the null value, it met the inclusion criteria in round 1. Eighty‐three percentage of the participants agreed that specific systemic antibiotic treatment regimens outlined by Marks et al. (27) (level of evidence IIb) were irrelevant, choosing to base treatment on the specific semi‐quantitative culture and sensitivity results, not by a predetermined antibiotic listed in a protocol. This correlates strongly to the wound bed preparation (WBP) algorithm (28), where the emphasis is on ‘treat the cause’. The protocol subsequently recommends testing for both aerobic and anaerobic bacteria. Since this review, the literature has reported that anaerobes accounted for over 60% of the bacteria seen in surgical site infections, some of which are not detectable by traditional laboratory testing (29). Some are organised as biofilms, further complicating the approach to diagnosis and interventions. The level of evidence is also IIb.
Unfortunately, the use of the mnemonics ’Non healing, Exudate increased, Red friable, Debris and Smell (NERDS) and STONES (Size increasing, Temperature increasing, Os; probes to bone, New or satellite lesions, Erythema/Edema/Induration and Smell)’(30), to differentiate the symptoms of superficial and deep infection, irritated two potential participants to a point that they declined to participate. An introduction to the mnemonics with references or placing these susceptible items near the end of the questionnaire might have prevented this response (23). However, the consensus regarding high relevance went from 63% in round 1 to 100% in round 3. As this research was completed in 2008, the mnemonic STONES has been updated to include a second ’E’ (Exudate increased) in research that validates these signs, and is now called ‘STONEES’(31).
Taking a semi‐quantitative swab for culture and sensitivity had a level of evidence of IIb (32), but advice to perform it in response to an ambiguous two or three of the signs and symptoms was only expert opinion (level IV) (30). The participants decided that two signs and symptoms would be sufficient in round 1. However, validation for a presence of three signs and symptoms as indicative of infection has been achieved, and the final protocol reflects this substantiation (31).
Turnbull et al.'s (33) recommendations for the optimal ‘jackknife’ positioning for perianal interventions would be difficult to replicate in the home environment. Modifying this positioning met the protocol inclusion criteria in round 3. The IRA changed from substantial to moderate, and then back to substantial agreement.
The wound cleansing items were included in an attempt to move from ritualistic sitz baths to evidence‐based interventions 34, 35. Irrigation techniques used for lacerations and traumatic wounds had level IIb evidence, but none existed for PSWs. All cleansing items met the inclusion criteria by round 3. Since this review, further opinion identifying tissue irrigation as a form of mechanical debridement as an important part of the accepted strategy for disrupting wound biofilms has been published (36), and may have a bearing on care of PSWs.
All of the characteristics of the ‘ideal’ dressing met inclusion criteria, including reasons why normal saline wet‐to‐dry gauze dressings are not advisable. Conversely, the risk of gauze leaving lint particles in the wound bed causing foreign body granulomas 37, 38 was considered ‘totally irrelevant'. The use of foam versus gauze dressings in PSWs with resultant pain reduction and increased patient satisfaction (39) also met the inclusion criteria (level IV evidence).
The participants believe that topical negative pressure wound therapy (TNPWT) should only be used for chronic surgical wounds when moist interactive dressings used for 4 weeks had not reduced the wound size by 30% 40, 41 (level Ia). The participants indicated a need to include decision making about TNPWT for postoperative PSW wounds. This prompted the researcher to review the European Wound Management Association (42) position document on TNPWT, adding criteria to guide initiation and discontinuation of the therapy in rounds 4 and 5. All six new items met the inclusion criteria, with substantial to almost perfect agreement.
Although there was no literature to support the activity of decontaminating the PSW peri‐wound skin, there was strong level Ib evidence for the bactericidal activity of chlorhexidine on skin 43, 44. Cleansing 5 cm of the peri‐wound skin with chlorhexidine 0·5% correlated to the distance recommended for depilation of hair to reduce the bacterial load (45), and met the protocol inclusion criteria. Unaccountably, the consensus decreased from 100% in round 2, where it needed minor revision, to 84% in round 3.
The researcher created six items around peri‐wound depilation of hair where two would have sufficed, one for during healing and the other for post‐healing. The participants supported the existing level IV evidence. However, new research has found that performing razor depilation as a precautionary measure to prevent recurrence actually resulted in a statistically significant (P = 0·01) increase in recurrence compared with individuals who did not shave (46). Those authors recommended that further study of other depilation techniques such as laser hair removal be undertaken.
One participant commented on the impact of friction and shearing forces in the natal cleft postoperatively caused by physical activity, arguing that although there was no published evidence, there was experiential knowledge that such activities would be harmful. Another participant countered that in spite of the risks, their experience was that individuals who participated in physical activities had an improved quality of life, and may have had stronger, more flexible tissue. Overall, there was a desire to limit physical activities causing friction or shearing forces, although it was believed that some individuals may need to participate to have an improved quality of life, where the psychosocial needs might outweigh the physical evidence (level IV opinion). There was almost perfect IRA.
The participants made many comments regarding the probable increased need for zinc, protein, calories and Vitamin C for purposes of optimising their PSW healing potential. A measure to assess whether the dietary intake was adequate for healing (47), and recommendations to improve the intake or add a specific dose of supplement if intake was inadequate met inclusion criteria and were added to the protocol (level IV opinion).
Educating patients about limiting physical activity to prevent tissue damage, and the need for good personal hygiene in the natal cleft, had only level IV evidence but were supported 45, 48, 49, 50. The increased risk of obesity in contributing to pilonidal sinus disease (PSD) recurrence had level IIa evidence. The Delphi participants had difficulty suggesting a weight reduction program post‐healing for individuals with a body mass index >29. The researcher collapsed the fourth and fifth items into one about knowledge of obesity and achieved consensus.
The importance of chronic inflammation became evident as the researcher was responding to requests for more information in the items about friable granulation tissue, and the physical effects of friction in the wound bed. It has been hypothesised that the reason for increased staphylococcal infections seen in PSWs and axillary wounds is damage to the wound surface, caused by friction of the dressing because of body movements (51). This also occurs around percutaneous feeding tubes, where peristalsis causes slight movement of the tube, creating friction (52). If doing the research again, this topic would be included because this appears to be a key point with PSWs.
The protocol (Table 3) consists of items that met the inclusion criteria, beginning with a holistic assessment, and includes positioning for optimal visualisation, signs and symptoms of infection and appropriate actions, local wound care, physical activity, nutritional considerations follow and concludes with patient education, in which the individual with a PSW is a primary decision maker or key participant (45). An algorithm based on the WBP algorithm (53) serves as a visual cue for decision‐making paired with the protocol (Figure 8). As with the 2000 WBP paper for holistic care of chronic wounds, the treatment of PSWs requires recommendations and rationales based not only on published literature, but also on the experience of the ‘experts’. By considering all of these factors, we can start to fully assess and evaluate the status of the person with a PSW, as well as the PSW itself, and implement appropriate treatment promptly.
Table 3.
Postoperative PSW evidence‐based protocol
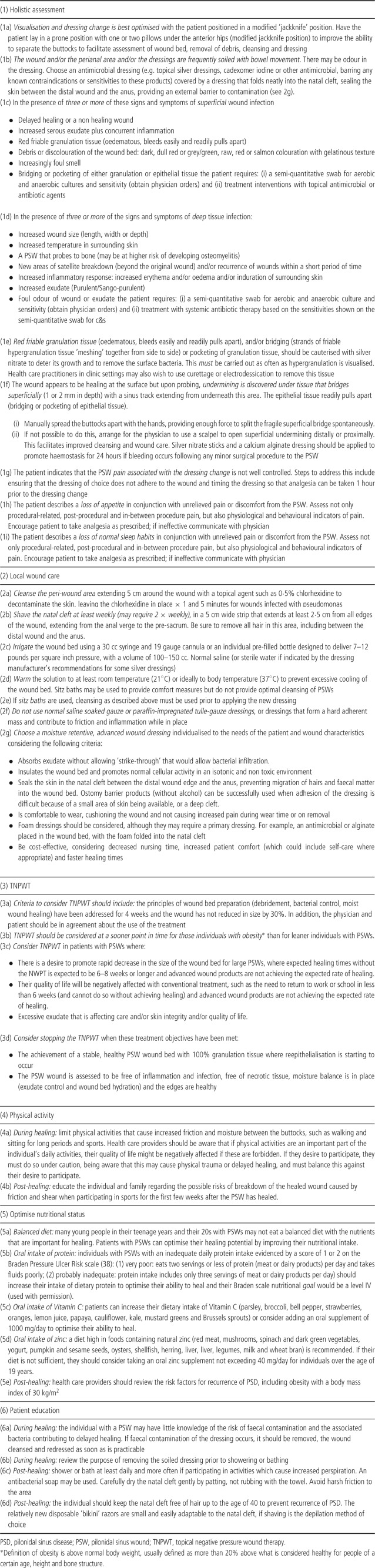
Figure 8.
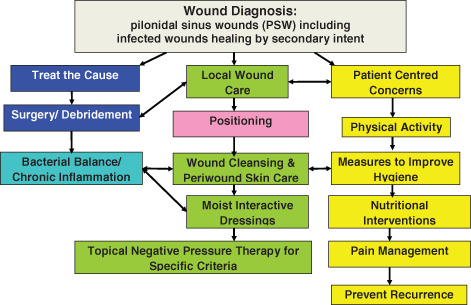
Algorithm for pilonidal sinus wound care protocol.
CONCLUSION
As this thesis work was completed in 2008, a comprehensive review of the aetiology and results of surgical and non surgical interventions has been published (54). The authors concluded that simple day surgery procedures such as trephining of pits and single sinuses was rational, safe and effective for patients with PSD, and would eradicate midline skin pits without wide excision of the abscesses. This is based on the theory that midline pits are the cause of all PSD. For individuals with complex or recurring PSD, more complicated Z and V–Y flap procedures, or modified Karydakis procedures such as the Bascom cleft lift operation were recommended by the authors (54). In theory, this approach to surgery would result in a faster time to healing without the open midline wounds that we see today.
However, this MRD procedure was intended to assist health care practitioners and providers to deal with the challenges posed when wide excision results in large open wounds. It successfully achieved the objectives, which were to identify the areas of care that negatively or positively influences healing of postoperative PSWs, and to inform, educate and broaden the considerations regarding these factors for health care professionals. The extensive literature review formed the basis of the questionnaire items. The feedback between rounds involved additional literature reviews in order to be informed, and did educate and broaden the considerations of the participants, contributing to this success. This is just a start on the journey to provide informed and successful care for this perplexing wound population. It is hoped that this will build on work by Bradley (55), who studied the phenomenology of the lived experience of having a PSW, and whose thesis work has been published posthumously 56, 57. Currently, the Delphi author is working with physicians and nurses who have a similar interest in determining what interventions can improve the outcomes for the PSW population. The goal is to apply this protocol and collect a case study series with a sample of 50 participants, to determine if there are improved healing times with the implementation of the protocol, and what , if any, interventions appear to be related to any successes. Fifty baseline chart audits of individuals with PSW who did not receive the protocol interventions have been performed to provide a control group. This client population deserves additional efforts and understanding on the part of health care providers, to achieve better knowledge and outcomes.
ACKNOWLEDGEMENTS
The authors thank Ron Shannon, MPH, Freelance Health care Economist, Clifton Park, New York for his generous assistance and advice with the statistical analysis and also Simon Galperin, The Delphi Decision Aid (Armstrong 2003), Wharton Business School at the University of Pennsylvania for assistance with data extraction.
This article constitutes thesis work by CH for the MSc in Wound Healing and Tissue Repair at Cardiff University, 2008, for which SH was the thesis advisor.
REFERENCES
- 1. Jones J, Hunter D. Education and debate: qualitative research: consensus methods for medical and health services research. BMJ [Online] 1995;311:376–80. URL http://www.bmj.com/cgi/content/full/311/7001/376 [accessed on 16 March 2005]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McKenna HP. The Delphi technique: a worthwhile research approach for nursing. J Adv Nur 1994;19:1221–5. [DOI] [PubMed] [Google Scholar]
- 3. Mullen PM. Delphi: myths and reality. J Health Organ Manag 2003;17:37–52. [DOI] [PubMed] [Google Scholar]
- 4. Streiner DL, Norman GR. Health measurement scales. Oxford: Oxford University Press, 2003:21. [Google Scholar]
- 5. Bowles N. The Delphi technique. Nurs Stand 1999;13:32–6. [DOI] [PubMed] [Google Scholar]
- 6. Lynn MR. Determination and quantification of content validity. Nurs Res 1986;35:382–5. [PubMed] [Google Scholar]
- 7. Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, Marteau T. Consensus development methods and their use in clinical guideline development. Health Technol Assess [Online] 1998;2. URL http://www.ncchta.org/execsumm/summ203.htm [accessed on 17 April 2005]. Now available at http://www.hta.ac.uk/fullmono/mon203.pdf [accessed on 12 February 2011]. [PubMed] [Google Scholar]
- 8. Custer RL, Scarcella JA, Stewart BR. The modified Delphi technique ‐ a rotational modification. J Vocat Tech Edu [Online] 1999;15. URL http://scholar.lib.vt.edu/JVTE/v15n2/custer.html [accessed on 16 March 2005]. [Google Scholar]
- 9. Lindeman CA. Delphi survey of priorities in clinical nursing research. Nurs Res 1975;24:434–41. [DOI] [PubMed] [Google Scholar]
- 10. Campbell SM, Cantrill JA, Roberts D. Prescribing indicators for UK general practice: Delphi consultation study. BMJ 2000;321:425–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wynd CA, Schmidt B, Schaefer MA. Two quantitative approaches for estimating content validity. West J Nurs Res 2003;25:508–18. [DOI] [PubMed] [Google Scholar]
- 12. Armstrong SJ. Delphi Decision Aid. The Wharton School, University of Pennsylvania, Philadelphia, PA [Online], 2003. URL http://armstrong.wharton.upenn.edu/delphi2/ [accessed on 29 November 2005].
- 13. Schmidt K, Montgomery LA, Bruene D, Kenney M. Determining research priorities in pediatric nursing: a Delphi study. J Pediatr Nurs 1997;12:201–7. [DOI] [PubMed] [Google Scholar]
- 14. Williams PL, Webb C. The Delphi technique: a methodological discussion. J Adv Nurs 1994;19:180–6. [DOI] [PubMed] [Google Scholar]
- 15. Rowe G, Wright G. The Delphi technique as a forecasting tool: issues and analysis. Int J Forecast 1999;15:353–75. [Google Scholar]
- 16. Hsu C‐C, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval [Online] 2007;12. URL http://pareonline.net/getvn.asp?v=12&n=10 [accessed on 24 February 2008]. [Google Scholar]
- 17. Graham B, Regehr G, Wright JG. Delphi as a method to establish consensus for diagnostic criteria. J Clin Epidemiol 2003;56:1150–6. [DOI] [PubMed] [Google Scholar]
- 18. Akins RB, Tolson H, Cole RB. Stability of response characteristics of a Delphi panel: application of bootstrap data expansion. BMC Med Res Methodol [Online] 2005;5:37. URL http://www.biomedcentral.com/1471‐2288/5/37 [accessed on 7 July 2008]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique. J Adv Nurs 2006;53:205–12. [DOI] [PubMed] [Google Scholar]
- 20. Rubio DM, Berg‐Weger M, Tebb SS, Lee ES, Rauch S. Objectifying content validity: conducting a content validity study in social work research. Soc Work Res 2003;27:94–100. [Google Scholar]
- 21. Gauthier DM, Froman R. Preferences for care near the end of life: scale development and validation. Res Nurs Health 2001;24:298–306. [DOI] [PubMed] [Google Scholar]
- 22. Bates‐Jensen BM, Vredevoe DL, Brecht ML. Validity and reliability of the pressure sore status tool. Decubitus 1992;5:20–8. [PubMed] [Google Scholar]
- 23. Neutens JJ, Rubinson L. Data collection through surveys and self‐reports. Chapter 6. In: Research techniques for the health sciences, 3rd edn. San Francisco, CA: Benjamin Cummings, 2002:115–116, 118,129–132, 220,247–248. [Google Scholar]
- 24. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:1159–74. [PubMed] [Google Scholar]
- 25. Hanafin S. Review of literature on the Delphi technique [Online], 2004. URL www.nco.ie/upload_documents/Delphi_Technique_A_Literature_Review.pdf [accessed on 12 April 2005].
- 26. Kozell K, Bauer N, Flahr D, Goetz D, Kohr R, Labate T, MacLeod F, Norton L, Parslow N, Savage P, Woo K, Mayo S. Assessment and management of stage I to IV pressure ulcers. In: RNAO Nursing Best Practice Guidelines Project (revised). Toronto, Ontario: Registered Nurses Association of Ontario, 2007:17.
- 27. Marks J, Harding KG, Hughes LE, Ribeiro CD. Pilonidal excision‐healing by open granulation. Br J Sur 1985;72:637–40. [DOI] [PubMed] [Google Scholar]
- 28. Schultz GS, Sibbald RG, Falanga V, Ayello E, Dowsett C, Harding K, Romanelli M, Stacey MC, Teot L, VanScheidt W. Wound bed preparation: a systematic approach to wound management. Wound Repair Regen 2003;11:1–28. [DOI] [PubMed] [Google Scholar]
- 29. Wolcott RD, Gontcharova V, Sun Y, Zischakau A, Dowd SE. Bacterial diversity in surgical site infections: not just aerobic cocci anymore. J Wound Care 2009;18:317–23. [DOI] [PubMed] [Google Scholar]
- 30. Sibbald RG, Woo K, Ayello E. Increased bacterial burden and infection: the story of NERDS and STONES. Adv Skin Wound Care 2006;19:447–61. [DOI] [PubMed] [Google Scholar]
- 31. Woo KY, Sibbald RG. A cross‐sectional validation study of using NERDS and STONEES to assess bacterial burden. Ostomy Wound Manage 2009;55:40–8. [PubMed] [Google Scholar]
- 32. Levine NS, Lindberg RB, Mason AD, Pruitt BA. The quantitative swab culture and smear: a quick, simple method for determining the number of viable aerobic bacteria on open wounds. J Trauma 1976;16:89–94. [PubMed] [Google Scholar]
- 33. Turnbull GK, Vanner SJ, Burnstein M. The colon. Chapter 11. In: Thomson ABR, Shaffer EA, editors. First principles of gastroenterology: the basis of disease and an approach to management, 3rd edn. Edmonton: Canadian Association of Gastroenterology, [Online], 1997. URL http://gastroresource.com/GITextbook/En/Default.htm [accessed on 2 April 2006].
- 34. Blunt J. Wound cleansing: ritualistic or research‐based? Nurs Stand 2001;16:33–6. [DOI] [PubMed] [Google Scholar]
- 35. Tejirian T, Abbas MA. Sitz bath: where is the evidence? Scientific basis of a common practice. Dis Colon Rectum 2005;48:2336–40. [DOI] [PubMed] [Google Scholar]
- 36. Philips PL, Wolcott RD, Fletcher J, Schultz GS. Biofilms made easy. Wounds Int [Online] 2010. URL http://www.woundsinternational.com/article.php?issueid=303&contentid=123&articleid=8851&page=1 [accessed on 23 July 2010]. [Google Scholar]
- 37. Sturdy JH, Baird RM, Gerein AN. Surgical sponges: a cause of granuloma and adhesion formation. Ann Surg 1967;128:128–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sari A, Basteri Y, Karabacak T, Tasdelen B, Demirkan F. The potential of microscopic sterile sponge particles to induce foreign body reaction. Int Wound Care J 2006;3:363–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vermeulen H, Ubbink D, Goossens A, de Vos R, Legemate D. Dressings and topical agents for surgical wounds healing by secondary intention. Cochrane Database Syst Rev 2006:1–10, Art. No.: CD003554. DOI:10.1002/14651858.CD003554.pub2. [DOI] [PMC free article] [PubMed]
- 40. Ontario Health Technology Advisory Committee. OHTAC recommendations: vacuum‐assisted closure (VAC) for chronic wounds. The Medical Advisory Secretariat, Ministry of Health and Long Term Care, Toronto, ON [Online], 2004. URL http://www.health.gov.on.ca/english/providers/program/mas/tech/recommend/rec_vac_121604.pdf [accessed on 3 November 2005].
- 41. Ontario Health Technology Advisory Committee. OHTAC health technology literature review vacuum assisted closure therapy for wound care. The Medical Advisory Secretariat, Ministry of Health and Long Term Care, Toronto, ON [Online], 2004. URL http://www.health.gov.on.ca/english/providers/program/mas/tech/reviews/pdf/rev_vac_120104.pdf [accessed on 3 November 2005].
- 42. Vowden K, Téot L, Vowden P. Selecting topical negative pressure therapy in practice. In: Moffat C, Banwell P, Vowden P, Franks P, Gottrup F, Horsch RE, Moore Z, Romanelli M, Ágreda JJS, Téot L, Vowden K, editors. European Wound Management Association (EWMA). Position document: topical negative pressure in wound management. London: MEP Ltd., 2007:10–13. [Google Scholar]
- 43. Aly R, Maibach HI. Comparative study on the antimicrobial effect of 0.5% chlorhexidine gluconate and 70% alcohol on the normal flora of the hands. Appl Environ Microbiol 1979;37:610–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Payne DN, Babb JR, Bradley CR. An evaluation of the suitability of the European suspension test to reflect in vitro activity of antiseptics against clinically significant organisms. Lett Appl Microbiol 1999;28:7–12. [DOI] [PubMed] [Google Scholar]
- 45. Armstrong JH, Barcia PJ. Pilonidal sinus disease: the conservative approach. Arch Surg 1994;129:914–8. [DOI] [PubMed] [Google Scholar]
- 46. Petersen S, Wietelmann K, Evers T, Hüser N, Matevossian E, Doll D. Long‐term effects of postoperative razor epilation in pilonidal sinus disease. Dis Colon Rectum 2009;52:131–4. [DOI] [PubMed] [Google Scholar]
- 47. Bergstrom N, Braden B, Laguzza A, Holman A. The Braden scale for predicting pressure sore risk. Nurs Res 1987;36:205–10. [PubMed] [Google Scholar]
- 48. Raffman RA. A re‐evaluation of the pathogenesis of pilonidal sinus. Ann Surg 1959;150:895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Al‐Naami MY. Outpatient pilonidal sinotomy complemented with good wound care and surrounding skin care. Saudi Med J 2005;26:285–8. [PubMed] [Google Scholar]
- 50. Miller D, Harding K. Pilonidal sinus disease. World Wide Wounds [Online] 2003. URL www.worldwidewounds.com/2003/december/Miller/Pilonidal‐sinus.html [accessed on 23 March 2004].
- 51. Marks J, Harding KG, Hughes LE. Staphylococcal infections of open granulating wounds. Br J Surg 1987;74:95–7. [DOI] [PubMed] [Google Scholar]
- 52. Borkowski S. G tube care: managing hypergranulation tissue. Nursing 2005;35:24. [DOI] [PubMed] [Google Scholar]
- 53. Sibbald RG, Williamson D, Orsted HL, Campbell K, Keast D, Krasner D, Sibbald D. Preparing the wound bed – debridement, bacterial balance and moisture balance. Ostomy Wound Manage 2000;46:14–35. [PubMed] [Google Scholar]
- 54. Thompson MR, Senapati A, Kitchen P. Simple day‐case surgery for pilonidal sinus disease. Br J Surg 2011;98:198–209. [DOI] [PubMed] [Google Scholar]
- 55. Bradley L. The lived experience of young adults with chronic pilonidal sinus disease: a phenomenological approach. WUWHS Second Congress, Paris, France: Poster Presentation, 2004.
- 56. Bradley L. Pilonidal sinus disease: a review. Part one. J Wound Care 2010;19:504–8. [DOI] [PubMed] [Google Scholar]
- 57. Bradley L. Pilonidal sinus disease: a review. Part two. J Wound Care 2010;19:522–30. [DOI] [PubMed] [Google Scholar]


