Abstract
Foot complications cause substantial morbidity in Tanzania, where 70% of leg amputations occur in diabetic patients. The Step by Step Foot Project was initiated to train healthcare personnel in diabetic foot management, facilitate transfer of knowledge and expertise, and improve patient education. The project comprised a 3‐day basic course with an interim period 1‐year of for screening, followed by an advanced course and evaluation of activities. Fifteen centres from across Tanzania participated during 2004–2006 and 12 during 2004–2007. Of 11 714 patients screened in 2005, 4335 (37%) had high‐risk feet. Of 461 (11%) with ulcers, 45 (9·8%) underwent major amputation. Of 3860 patients screened during 2006–2007, there was a significant increase in the proportion with ulcers and amputations compared with 2005 (P < 0·001), likely a result of enhanced case finding. During 2005–2008, there was a fall in the incidence of foot ulcers in patient referrals to the main tertiary care centre in Dar es Salaam and a parallel fall in amputation among these referrals. In conclusion, the Step by Step Foot Project in Tanzania improved foot ulcer management for persons with diabetes and resulted in permanent, operational foot clinics across the country. This programme is an effective model for improving outcomes in other less‐developed countries.
Keywords: amputation, diabetes, foot ulcers, less‐developed countries, surveillance
INTRODUCTION
The prevalence of diabetes mellitus is increasing in populations across the African continent. Among the affected persons, lower limb ulceration is perhaps the most common complication, resulting in substantial morbidity (e.g. partial amputation or complete loss of limb) and mortality, and rising or unsustainable healthcare costs for individuals and healthcare providers alike (1). In Tanzania, approximately 800 000–1 000 000 persons of the entire population of 33 000 000 are estimated to have diabetes; urban areas are particularly affected with prevalence rates reaching 12% versus 1% in rural areas (2).
In Dar es Salaam, the largest city in Tanzania, about 80% of diabetes patients admitted to the inpatient medical service at Muhimbili National Hospital (MNH) with foot ulcer complications also have severe peripheral neuropathy and a history of poor glycaemic control (3). Approximately 33% of these patients end up with major amputation of the affected limb; and among those who delay seeking medical attention, the mortality rate is > 50%, largely attributable to progressive gangrene and development of overwhelming sepsis (3). The seriousness of the issue and the clinical and public health implications are underscored by the fact that the overall mortality rate for all persons with diabetes admitted to the MNH medical inpatient service with any kind of lower limb complication is approximately 27% (3).
There are several clearly identifiable aetiological factors associated with foot ulceration and amputations in Tanzania 3, 4, 5. These include poor understanding of diabetes and its complications among healthcare professionals and patients alike, bare‐foot walking, delays in seeking medical attention or delay in patient referral for specialist foot care, poor diabetes control, or preferences by patients for alternative traditional therapies in the first instance 3, 4, 5, 6, 7, 8, 9, 10.
Until 2004, diabetic foot services throughout Tanzania, especially in rural areas, were very limited or were largely manned by untrained healthcare professionals. Compounding the problem was the lack of sustainable infrastructure for diabetic foot management, trained personnel and formal podiatry services in the country. Not surprisingly, as with many other less‐developed countries, there were no structured educational programmes established for training healthcare personnel on how to identify and manage diabetic foot complications effectively. Equally, there was no identifiable specialist service infrastructure to support or train clinicians and other healthcare professionals to care for people suffering with diabetic foot ulcer disease and its sequelae. For all these reasons, the ‘Step by Step’ Foot Project – a programme aimed at educating healthcare providers – was instituted in several regions across Tanzania in 2004 (2). We carried out this study to determine the efficacy of this project in improving patient outcomes.
MATERIALS AND METHODS
The ‘Step by Step’ training programme is an organised course focused primarily on diabetic foot education, training and support. It was established and instituted through collaboration between the International Diabetes Federation (IDF) Consultative Section and the International Working Group on the Diabetic Foot, together with the Diabetic Foot Society of India (DFSI) and the Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania. The goal was to assist doctors and nurses in the identification and characterisation of diabetic foot complications, and equip them to manage such complications effectively through a structured programme of education and training (2). An experienced national and international faculty was responsible for the teaching and supervision of the practical sessions. Basically, the programme consists of consecutive educational seminars given a year apart, each event lasting three days. In addition, the ‘Step by Step’ programme organisers developed a wide array of health education material for healthcare providers who deal with the diabetic foot in less‐developed settings. These materials include written, visual and audiovisual information pertaining to diabetes and its complications, with particular emphasis on foot pathology and management, and are aimed at both patients and healthcare professionals. The materials are issued to Step by Step course participants at the time of registration for the seminars.
The ‘Step by Step’ training programme that was adapted for Tanzania was designed for and attended by a pair of personnel (doctor and nurse) from 15 sponsored centres in 14 regions across the country. The programme was fully supported by the Tanzanian Ministry of Health, which also facilitated adequate medical and nursing staffing for existing diabetes clinics across the nation. The curriculum consisted of formal lectures, practical demonstrations, live patient examinations and pertinent problem solving, and interactive hands‐on sessions with patients who had existing foot problems. The detailed educational component included didactic lectures in the following areas: foot‐care knowledge; history taking skills; clinical examination; screening for neuropathy (10 g monofilament, sharp sensation and vibration perception) and ischaemia (pedal pulse palpation); basic biomechanical assessment; diagnosis and management of diabetic foot infections; basic applied podiatry and foot ulcer management; the utility and application of off‐loading interventions; development of appropriate, realistic and sustainable management plans; and patient health education issues. Although not an inherent component of the Step by Step Program, lectures in general diabetes management were included to make the programme more comprehensive.
Clinical data forms were issued to each of the 15 participating centres for recording characteristics and demographics of screened patients, medical and surgical history, clinical features and severity of foot complications, grading of ulcers, and outcomes, including amputations and mortality. These forms had to be completed and returned to the principal investigator (ZGA) every quarter. Peripheral neuropathy was ascertained by the patient's ability to detect pressure caused by a 10 g monofilament on the feet at different sites and vibration sense using a 128 Hz tuning fork. Peripheral vascular disease was determined by the presence or absence of palpable pulses in the feet.
All participants from the 15 centres were provided with health education materials for doctors, nurses and patients and posters for the centres on diabetic foot. Screening, therapeutic and diagnostic kits for management of the diabetic foot were given to each centre. On completion of the course, participants were expected (and encouraged) to disseminate acquired knowledge and skills to their medical and nursing colleagues, and to organise formal diabetic foot education sessions for patients under their care. An infrastructure for networking and support was also established and facilitated by the principal investigator (ZGA).
The first official course was conducted in 2004 and during the following year participating delegates attended the second and more advanced course in which a forum was provided for the sharing of problems, experiences and knowledge. In 2006, the principal investigator (ZGA) audited 11 of the 15 participating foot‐care centres to monitor progress and logistic problems, and to offer support. The 11 audited centres were chosen primarily because of ease of accessibility. All 11 centres were proactive in diabetic foot management, but expressed a need for more training in podiatry skills.
A third and final course was conducted in July 2007; however, because of budget constraints only participants from nine of the most active teams were invited to attend this final course. This third course focused on (i) podiatry skills, (ii) the utility of and rationale for off‐loading interventions in ulcer healing and (iii) practical presentations and demonstrations of complex ulcer cases for which active attendee participation was encouraged.
To determine whether the Step by Step intervention was effective in improving patient outcomes, we monitored temporal trends in rates of major amputation among persons with foot ulcers in one of the participating centres that already had an established surveillance system for diabetic foot complications. For this activity, we chose the diabetes clinic at MNH in Dar es Salaam: the principal investigator (ZGA) has been conducting active surveillance of foot complications among MNH diabetes patients since 1997. Thus, we were able to determine and analyse temporal tends in major amputation rates resulting directly from diabetic foot ulcers in patients referred to the MNH clinic during 2000–2008. The denominator for the amputation rate was the annual number of foot referrals to MNH.
RESULTS
Effectiveness of Step by Step
In total, 15 pairs of doctors and nurses from 15 centres located in 14 Tanzanian regions participated in the first two training programmes held in 2004 and 2005. During the 2005 calendar year, following the 2004 course, participants from 14 centres screened 11 866 persons with diabetes for foot complications. Of these, 4434 (37%) had a foot complication (i.e. one or more of neuropathy, ischaemia, infection or ulceration); a total of 538 (12%) patients had active foot ulcer disease and 52 (9·7%) of these proceeded to major amputation of the affected limb; 17 (3%) died from causes directly attributable to progression of their foot complication. During 2006, participants from these 14 centres screened a further 2850 patients (Table 1). In this screened population, the proportion of high‐risk feet that were active ulcers was significantly higher in 2006 compared with 2005 (23% versus 12%, P < 0·0001). In addition, patients screened and found to have active foot ulcers in 2006, and referred to hospital for further management, were significantly more likely to undergo a major amputation compared with 2005 ulcer patients (20% versus 9%, P < 0·0001; Table 1).
Table 1.
Outcome data after 1 year of the basic course, 2005–2006 (14 centres)
| 2005 | 2006 | P‐value | |
|---|---|---|---|
| Number of patients screened | 11 866 | 2850 | – |
| Number of patients with high‐risk foot | 4434 (37%) | 1106 (38%) | NS |
| Number of patients with foot ulcers | 538 (12%) | 256 (23%) | <0·0001 |
| Number of reported amputations | 52 (9%) | 51 (20%) | <0·0001 |
| Clinical officers trained | 69 | 125 | – |
| Nurses trained | 147 | 176 | – |
| Diabetic sessions with patients | 163 | 563 | – |
NS, not significant.
Of the 14 centres that screened patients during 2005–2006, 12 continued screening activities and management of foot ulcer disease in 2007. Compared with 2005, patients screened by these 12 centres during 2006 through 2007 were significantly more likely to be diagnosed with a high‐risk foot complication compared with 2005 patients, to have active foot ulcers, or to proceed to major amputation of the relevant limb (Table 2).
Table 2.
Outcomes for the 12 centres that aggregated data during 2005 through 2007
| 2005 | 2006 through 2007 | P‐value | |
|---|---|---|---|
| Number of patients screened | 11 714 | 3860 | – |
| Number of patients with high‐risk foot | 4335 (37%) | 1523 (39·5%) | < 0·01 |
| Number of patients with foot ulcers | 461 (10·6%) | 422 (27·7%) | < 0·0001 |
| Number of reported amputations | 45 (9·8%) | 74 (17·5%) | < 0·001 |
| Clinical officers trained | 69 | 79 | – |
| Nurses trained | 146 | 65 | – |
| Diabetic sessions with patients | 153 | 743 | – |
Temporal trend analysis
4324 patients with diabetes and with various diabetic foot complications were referred and admitted to MNH during 2000–2008; 736 (17%) of these patients had active foot ulcer disease (Figure 1). Ulcer occurrence in these patients peaked in 2005 and then declined over the subsequent years. During 2000 through 2008, the mean annual amputation rate among diabetic foot ulcer patients referred to MNH was 17·6%. Before the institution of the Step by Step Program, amputation rates for MNH referrals were > 1 SD above the mean annual rate (Figure 2). After 2005, the occurrence of foot ulcer disease among patients referred to MNH and the annual amputation rates in these patients decreased significantly and by 2008 fell to almost two SD below the mean (1, 2).
Figure 1.
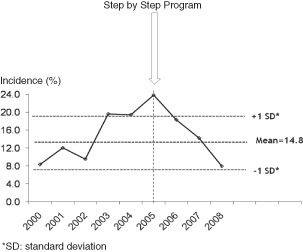
Incidence of foot ulcer disease among all patients referred and admitted to Muhimbili National Hospital with a foot complication, Dar es Salaam, Tanzania, 2000–2008.
Figure 2.
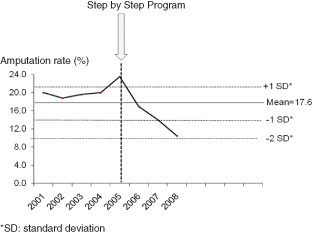
Temporal trends in amputation rates among diabetic foot ulcer referrals to Muhimbili National Hospital, Dar es Salaam, Tanzania, 2000–2008. The denominator is the total annual number of foot referrals to MNH.
DISCUSSION
The introduction of the Step by Step diabetic foot training programme in Tanzania has enhanced the management of patients with foot ulceration resulting in improved outcomes among persons with active ulcers; this study has documented improved management of diabetic foot ulcer disease at the local level and less referrals to the main tertiary care centre in the country for amputation. And for the first time in Tanzania, institution of a formal interventional training programme for healthcare providers has enabled or facilitated permanent, operational foot clinics in 14 regions across the country and a diabetes service infrastructure braced for the future. At the same time, the programme has engendered and raised the awareness of diabetic foot complications among both healthcare providers and patients alike, and facilitated ongoing training among medical and nursing personnel involved in diabetic foot care as well as training and development of additional staffing, and hiring of more such skilled personnel.
One of the remarkable achievements of the Step by Step Program was the relatively large number (nearly 12 000) of patients screened and identified with one or more foot complications in the participating regions during the 2005 calendar year following the first training course. That fewer (2850) patients were recorded during the subsequent year suggests that most of the at‐risk patients were likely identified in 2005 – an attestation of the diligence, tenacity, and propensity for hard work among the participants, and the value of the education and training modules of the Step by Step Program itself. The higher rate of active foot ulcers among patients identified with a foot complication in 2006 versus 2005 (23% versus 12%) suggests that the former group of patients were either persons with longstanding diabetes who previously had never sought or received medical attention or persons known to have diabetes but who were lost to follow‐up. This inference is supported by the fact that persons screened in 2006 and 2007 were significantly (P < 0·0001) more likely to have active ulcers as the major foot problem or to undergo major amputation of the affected limb (P < 0·001).
The data from Dar es Salaam show fewer referrals of patients with foot ulcers to MNH following institution of Step by Step and a significant fall in the number of amputations among those who end up being referred to MNH, suggesting that patients are receiving improved care at the primary care level. For those patients who are eventually referred for specialist foot care at MNH, the improved management at the primary care level is translated into better opportunities to save limbs in the tertiary care setting leading to overall enhanced outcomes.
A root cause analysis of possible reasons for the relatively high morbidity and mortality rate associated with diabetic foot ulceration in Tanzania has identified and implicated several key factors 8, 11. First, lack of healthcare professionals trained in diabetes foot care across Tanzania appears to be a universal problem. Unforeseen consequences of this absence of training are manifest by the doctor not even being aware of foot‐care basics and the negative effect of this lack of awareness on patient outcomes; lack of a team or multidisciplinary approach in managing the diabetic foot; and the reality of patients being blindly referred to the surgery department for premature amputation before conservative treatment is even given a try. Second, patient's lack of knowledge of diabetes and its complications has long been identified as an important determinant of patient outcomes and there is a myriad of published data in the medical literature that addresses this ‘lack of education’ issue. Third, in less‐developed countries like Tanzania, education of persons with diabetes on foot‐care issues is often left to staff not totally familiar with the management of complicated foot ulcer disease. Oftentimes, in these settings, foot‐care services are run by personnel with little or no experience or specialist training in diabetic foot care. In short, education of patients is often given short thrift and treated generically as an afterthought, as it were.
The paucity of specialist podiatry services aimed specifically at diabetic foot management has resulted either in patients not receiving the pertinent foot care that is necessary for better outcomes or in personnel with no podiatry experience making clinical decisions on foot care, including indiscriminate amputation of a limb that could have been salvaged had the patient received proper management. Hence, the reason for the inclusion of specialised podiatry training in the Step by Step Program. Potential areas for improvement of the Step by Step Program include training of healthcare personnel in the conduct of basic microbiology techniques (e.g. gram staining of deep tissue biopsies) that are not expensive or time consuming, and using these results to enhance clinical and therapeutic decision making in diabetic foot management. In 2009, Step by Step Program organisers invited 30 private centres including 60 teams of doctors and nurses to participate in the course; in 2010, cobblers from the respective centres were invited to participate as part of an effort to extend the multidisciplinary profile of care‐giving teams beyond medicine and nursing. Also, in 2009, the first Step by Step training seminars, aimed specifically at surgeons from centres in 20 regions, were held in Tanzania; the focus was largely on optimising surgical practice to salvage diabetic feet and reduce rates of amputation. To date, training has now been expanded from government and private centres to 43 centres in 21 regions across Tanzania. Following the success of Step by Step in improving patient outcomes in Tanzania, the authors believe that similar successes are achievable in other African countries. Thus far, the project has been exported successfully to the Democratic Republic of Congo (15 centres trained), Guinea (13 centres trained), Pakistan, Egypt and four Caribbean islands.
Step by Step is a training programme that focuses on (i) targeted screening and surveillance activities; (ii) early detection of foot complications and ascertainment of risk factors that could likely lead to disease progression; (iii) improving education of healthcare personnel who are actively involved in the management of the diabetic foot and (iv) the enhancement of diabetic foot management skills. One of the potential benefits of such a programme to less‐developed countries is the enabling of healthcare providers in these settings to target and manage limited human and financial resources more effectively. It is hoped that the successful establishment of this model of diabetic foot care in Tanzania will encourage other less‐developed countries to do likewise. Finally, one of the least visible but important upshots of the Step by Step Program has been the highlighting of the importance of epidemiology and surveillance activities for characterising foot complications in persons with diabetes, and for monitoring disease progression and outcomes, such as temporal trends of amputations rates and mortality.
In conclusion, institution of the Step by Step Foot Project in Tanzania improved foot ulcer management for persons with diabetes, enhanced the sharing of knowledge and skills among doctors and nurses, and resulted in permanent, operational foot clinics across the country. We also showed the feasibility of managing high‐risk feet at the regional level through a programme of education aimed at both healthcare providers and patients allied with dissemination of information to other healthcare professionals involved in patient care, and empowerment of persons with diabetes to take better care of their feet on their own volition, detect problems earlier and seek timely help when problems arise. Early detection and treatment of diabetic foot complications through sustained education and targeted screening programmes, such as this one, serves as a working model to reduce morbidity and mortality and improve patient outcomes in other less‐developed countries.
ACKNOWLEDGEMENTS
This work was made possible through generous funding from the World Diabetes Foundation and academic support from the International Diabetes Federation, the International Working Group on the Diabetic Foot, the Diabetic Foot Society of India and the Muhimbili University College of Health Sciences, Dar es Salaam, Tanzania. The first pilot‘Step by Step’ training programme in Tanzania was initiated in 2003 by Zulfiqarali G. Abbas (Tanzania), Sharad Pendsey (India), Vijay Vishwanathan (India), Karel Bakker (The Netherlands), Neil Baker (United Kingdom) and Alethea Foster (United Kingdom). Finally, we are most grateful to Shabneez Gangji and Kulsum Ramadhani in Dar es Salaam for their excellent secretarial assistance.
REFERENCES
- 1. Boulton AJ, Vileikyte L, Ragnarson‐Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005;366:1719–24. [DOI] [PubMed] [Google Scholar]
- 2. Bakker K, Abbas ZG, Pendsey S. Step by step, improving diabetic foot care in the developing world. A pilot study for India, Bangladesh, Sri Lanka and Tanzania. Pract Diab Intern 2006;23:365–9. [Google Scholar]
- 3. Gulam‐Abbas Z, Lutale JK, Morbach S, Archibald LK. Clinical outcome of diabetes patients hospitalized with foot ulcers, Dar es Salaam, Tanzania. Diabet Med 2002;19:575–9. [DOI] [PubMed] [Google Scholar]
- 4. Wikblad K, Smide B, Bergström A, Kessi J, Mugusi F. Outcome of clinical foot examination in relation to self‐perceived health and glycaemic control in a group of urban Tanzanian diabetic patients. Diabetes Res Clin Pract 1997;37:185–92. [DOI] [PubMed] [Google Scholar]
- 5. Neuhann HF, Warter‐Neuhann C, Lyaruu I, Msuya L. Diabetes care in Kilimanjaro region: clinical presentation and problems of patients of the diabetes clinic at the regional referral hospital – an inventory before structured intervention. Diabet Med 2002;19:509–13. [DOI] [PubMed] [Google Scholar]
- 6. Abbas ZG, Archibald LK. Challenges for management of the diabetic foot in Africa: doing more with less. Int Wound J 2007;4:305–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abbas ZG, Archibald LK. The diabetic foot in Sub‐Saharan Africa: a new management paradigm. Diab Foot J 2007;10:128–36. [Google Scholar]
- 8. Abbas ZG, Archibald LK. Epidemiology of the diabetic foot in Africa. Med Sci Monit 2005;11:RA262–70. [PubMed] [Google Scholar]
- 9. Abbas ZG, Viswanathan V. The diabetic foot in Africa and India. Int Diab Monitor 2007;19:8–12. [Google Scholar]
- 10. Abbas ZG, Gill GV, Archibald LK. The epidemiology of diabetic limb sepsis: an African perspective. Diabet Med 2002;19:895–9. [DOI] [PubMed] [Google Scholar]
- 11. Abbas ZG, Lutale JK, Archibald LK. Diabetic foot ulcers and ethnicity in Tanzania: a contrast between African and Asian populations. Int Wound J 2009;6:124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


