Abstract
This article describes the barriers, changes and achievements related to implementing one element of a wound care programme being best practice care. With the absence of a coordinated approach to wound care, clinical practice within our Area Health Service (AHS) was diverse, inconsistent and sometimes outdated. This was costly and harmful, leading to overuse of unhelpful care, underuse of effective care and errors in execution. The major aim was to improve the outcomes and quality of life for patients with wound care problems within our community. A collaborative across ten sites/services developed, implemented and evaluated policies and guidelines based on evidence‐based bundles of care. Key barriers were local resistance and lack of experience in implementing structural and cultural changes. This was addressed by appointing a wound care programme manager, commissioning of a strategic oversight committee and local wound care committees. The techniques of spread and adoption were used, with early adopters making changes observable and allowing local adaption of guidelines, where appropriate. Deployment and improvement results varied across the sites, ranging from activity but no changes in practice to modest improvement in practice. Evaluating implementation of the leg ulcer guideline as an exemplar, it was demonstrated that there was a statistically significant improvement in overall compliance from 26% to 84%. However, only 7·7% of patients received all interventions to which they were entitled. Compliance with the eight individual interventions of the bundle ranged from 26% to 84%. Generic performance was evaluated against the wound assessment, treatment and evaluation plan with an average compliance of 70%. Early results identified that 20% of wounds were healed within the target of 10 days. As more standardised process are implemented, clinical outcomes should continue to improve and costs decrease.
Keywords: Bundle, Clinical practice guideline, Evidence‐based practice, Spread, Wound care
INTRODUCTION
The purpose of this article is to describe and discuss issues and achievements related to the best practice care element of a wound care programme. Programme evaluation (1) shows our accountability in reporting on the expenditure of public funds, validating programme objectives and the degree of implementation and achievement of clinical goals.
Traditionally, the medical profession has directed the care of wounds. However, over the past 30 years, wound management decision making has gradually been incorporated into the nurse's scope of practice (2). More recently, wound care is being delivered by a vast array of people including clinicians, patients and/or carers, in a variety of settings, and often in isolation (3).
In 2005 Northern Sydney Area Health Service (AHS) amalgamated with the Central Coast AHS to become Northern Sydney Central Coast Health Service (NSCCHS). Covering 2500 km2, NSCCHS serves a population of 1·1 million, using approximately 10 000 staff across seven major sites as well as domiciliary care.
Historically, each facility within NSCCHS had undertaken a number of quality improvement activities to develop wound management practices, but these were usually self‐generated and not part of a collaborative approach. Subsequently, most sites, workgroups and professionals believed that their system was independent and autonomous, and specific to the disparate patient conditions that each clinician/group dealt with. For instance, those managing leg ulcers were autonomous in their treatment which was quite different to clinicians preventing surgical site infections.
It was recognised that the autonomy of each of the two AHSs prior to amalgamation could be a significant barrier to the project. In addition, previous efforts to improve wound care were un‐coordinated because of professional, geographical and personal priorities along with a lack of leadership across the sites. This showed itself in seemingly intractable problems with little coordination of what and how to change and improve this growing clinical problem. So, in this context, the issue of cultural change was considered to be a defining intervention with the standardisation and incorporation of the continuum of care into clinical guidelines being the lever for this change.
Other best practice programmes were in place across the AHS, such as for pressure ulcer management. So there was no shortage of innovators and opinion leaders (4) to agree that a wound care programme led and supported by early adopters would allow for a critical mass to observe and agree on the implementation possibilities and positive outcomes that a wound care programme could deliver.
Wound care is generic across all patient populations:
-
•
Approximately 270 000 people in Australia have a chronic wound (5);
-
•
12· 1% of patients' surgical wounds healed by secondary intention (6), which extends the healing time and wound care resources required;
-
•
Treatment of infected surgical wounds can add up to 10 days of hospital care to the length of treatment (7);
-
•
15· 9% of surgical sites have iatrogenic infections in acute care; 28·1% skin and soft tissue infection in non acute settings (8);
-
•
Prevalence of chronic leg ulcers ranges between 1·1 and 3·0 per thousand adults in western countries (9) with treatment costs per patient approximating A$12 000 per annum;
-
•
Cost to treat is estimated to be A$3 billion per annum for the management of leg ulcers (10).
PROBLEM
Arguably, wound care is a high volume, high risk, high cost and unreliable health care activity. Delayed healing and infections related to inappropriate treatment results in preventable pain and reduced quality of life.
New South Wales has yet to conduct epidemiological studies appropriate to the topic. However, the high volume of wounds is evidenced by a prevalence study in Western Australia (11) of 3000 patients which confirmed that:
-
•
48% of patients had at least one wound;
-
•
28% of patients had acute wounds;
-
•
9% of patients had pressure ulcers;
-
•
11% of patients had skin tears.
It was identified that the AHS required that a wound care programme should not just be isolated to acute settings. This was because just one of our two domiciliary home nursing services provides around 100 000 home visits a year for wound care (2004–2005) of which approximately half are related to the treatment of leg ulcers.
AIM
The aims of the proposed changes were to:
-
•
Improve the outcomes and quality of life for patients with wound care problems within the NSCCHS ‘community’;
-
•
Empower clinicians and patients through the development of a wound care programme that enables delivery of best practice, innovation and cost‐effective care.
STUDY QUESTIONS
The primary improvement‐related question was ‘What needs to happen to ensure that patients with wounds have optimal healing?’ Secondary to implementation of changes, an evaluation would include seeking answers to the following questions:
-
•
How effective has the generic and site‐specific deployment plan been?
-
•
What patient, organisational and staff processes and outcomes have been affected?
Because it was our intention that the programme would evolve over time, our improvement‐related questions were not set in concrete. As the programme took shape, the reaction to performance and emerging complexities were mirrored in the change and scope of indicators we monitored.
METHODS
The wound care programme had an executive sponsor with tactical support from the Patient Safety Manager. The project leader was the Clinical Nurse Consultant Stomal Therapy/Wound Care seconded, initially, to undertake a gap analysis.
To give a balanced view of the state of wound care across the AHS a number of different sources of information were explored. The elements that formed the gap analysis were:
-
1
A literature review to establish international best practice standards in wound care;
-
2
Interviews were held with key stakeholders in wound care;
-
3
A visit to a tertiary referral wound care clinic identified to have best practice models;
-
4
A small audit sample provided documentation across the breadth of all wound types. Each medical record was then mapped against international best practice standards for leg ulcers, non complicated surgical wounds and wounds considered complicated through infection or wound breakdown.
During this process it was identified that wound care was being delivered by a vast array of people including clinicians, patients and/or carers, in a variety of settings, and often in isolation. Care was sometimes not in keeping with current local, national and international best practice guidelines, and there was no standardisation in practice between staff and between sites. With the absence of a coordinated approach to wound care across NSCCH, practice was diverse, inconsistent and sometimes outdated. This was costly and harmful, leading to overuse of unhelpful care, underuse of effective care and errors in execution. Although no data were available, there was consensus that re‐admission and patient harm were linked to a lack of continuity of care for patients on discharge.
Cost ineffectiveness and inappropriate use of the vast array of wound care products were also linked to a lack of standardisation and outdated staff wound care knowledge. Clinicians were concerned about the increasing costs of products, especially those associated with antimicrobial dressings. Costs were not just measured in product use. Inappropriate indirect costs were being generated through lack of knowledge and skill, as well as extended clinical time. Additionally, there was no monitoring system to track patient outcomes in relation to length of stay, treatment, cost, improved quality of life and analgesic use.
One of the high volume, high risk and problem areas identified was the clinical management of wounds. A gap analysis identified that fewer than half of the audited clinical areas had guidelines in place to ensure best practice information guided nursing interventions. Only 20% of clinical guidelines addressed the whole continuum of care (i.e. included general practitioners and community nurses). Half of the clinicians identified that they required assistance to develop and implement guidelines. It was highlighted that assistance may include direction from a dedicated wound care CNC/specialist and/or clinical nurse educators. Most clinicians sought to access guidelines via our Intranet; however, existing information technology support did not make this always available.
There were also examples of good wound care practice and initiatives, specifically that all clinical areas had guidelines for pressure ulcer prevention, the majority of which addressed the continuum of care.
Eight elements of a wound care programme
Development of a strategic plan defined the vision and necessary structure, resources, procedures and actions to achieve the future and incorporated the following eight elements:
-
1
Best practice care;
-
2
Models of care;
-
3
Health promotion by prevention;
-
4
Education;
-
5
Care management;
-
6
Information management;
-
7
Research and innovation;
-
8
Cost effectiveness.
This article describes the issues and achievements of the best practice care element.
SOLUTIONS
The following objective was agreed: Persons with wound care issues will receive safe, appropriate and effective care. This will be achieved by developing, implementing and evaluating evidence‐based guidelines for all major categories of acute and chronic wounds. Subsequently, approximately 30 policies/guidelines were identified as requiring standardisation or initial development.
Framework for developing, implementing and evaluating policies and guidelines
An agreed framework for developing wound care policies/clinical guidelines included:
-
•
A process for policy/guideline development designed so that local Wound Care Committees could develop/modify their own;
-
•
A system developed for determining the ‘level of complexity’ of the policies/guidelines developed and the implementation requirements for each;
-
•
Ensuring relevancy across the care continuum by including general practitioners and community care;
-
•
Publishing one page policy summaries based on the key principles;
-
•
Developing a method to monitor the clinical application of guidelines.
Structures and processes
The programme included a number of structures including:
-
•
A wound care programme manager was appointed to guide the multidisciplinary Area Wound Care Committee and other key stakeholders to develop and implement the wound care programme within the 2‐year timeframe and ensure it was sustainable;
-
•
The Area Wound Care Committee role was to develop strategies and operational plans to achieve the programme goals, provide governance and oversight of the system for wound care monitoring and link to the management board regarding programme performance;
-
•
The best practice working party role was to action the strategic plan through formulating and overseeing the development of around 30 policies, processes and evidence‐based guidelines.
-
•
Local wound care committees and clinical networks as shown in Figure 1 had the role of reviewing and providing feedback on newly developed or standardised evidence‐based guidelines as well as implementing strategies and operational plans. Each site wound care committee chair was a member of the area wound care committee.
Figure 1.
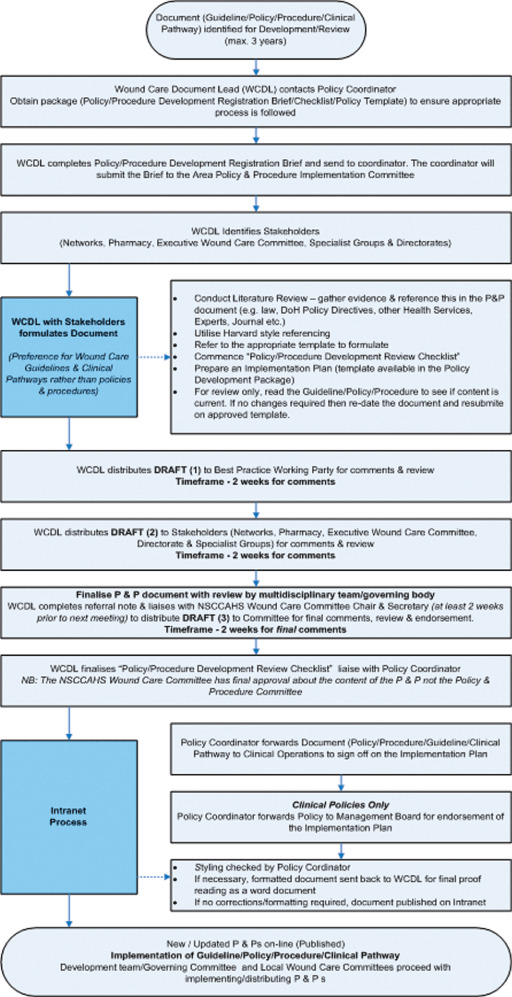
Local wound care committees and clinical networks.
Standardisation can be reviled in one organisation and revered in another. The key is to only standardise processes where absolutely necessary. To work, changes must be not only adopted locally but also adapted locally (12). On the basis that people do not resent change, but do resent being changed, the overriding principle was that users would develop the guidelines. No one will disagree with a decision/action they have put forward. Thus policies were allowed to be adapted by local wound care committees. For example, the wound swabbing guidelines suggest that in community health it may be beneficial and will provide a more accurate swab result if the wound swab is collected by the pathology service.
Once implemented, we were aware of the need to treat guidelines as living, breathing documents that can and must be constantly improved and maintained in line with current best practice. We developed a process for the spread of our guidelines which was partly a technical process and part leadership processes, and in this capacity was able to show and/or emulate leadership processes. When a group takes on this leadership mantle it produces synergy which is a powerful way to effect positive change. Each local committee chair was supported by the wound care programme manager who used situational leadership by supporting, coaching, delegating or directing, dependent on the need of the colleague (13).
Deployment
Understanding that the success of adoption of change lies in people being able to adapt it at the local level (12), we developed an executive steering group with membership of each of the site chair persons, programme manager and the programme sponsor who were able to consider site‐specific implementation needs and variations to the guidelines. Guidelines are more likely to be effective if they take into account local circumstances and are disseminated by an ongoing educational and training programme. A two‐pronged approach to deployment was developed which involved communication and notification as well as education and training according to the stratified complexity of the guideline. The categories of complexity were defined, by the author, as straight forward, Intermediate or complex.
Guidelines are a means to capture and retain organisational knowledge and as such were posted on our Intranet; for those with limited computer access the local wound care committees also made these available in a printed format in a resource folder. The one‐page summaries provided clinicians with a snapshot view of the principles and essentials of care related to that patient group/key associated risks. General practitioners and medical students along with allied health professionals (podiatrists and occupational therapists) were invited to wound care seminars and also provided with documentation of the new processes so that they were aware of their role and that of other stakeholders. Patients and carers are able to access guidelines from the internet at http://www.nsccahs.health.nsw.gov.au/services/wound.care/index.html.
A formal communication plan documented which stakeholder groups required what communication message and the most appropriate vehicle for reaching them. For instance, there was weekly e‐mail information to members of the Area Wound Care Committee, each site Director of Nursing and the clinical networks. A bi‐monthly wound care programme Newsletter provided highlights of recently endorsed guidelines/policies and this was replicated on the wound care programme webpage.
RESULTS
There are many purposes of evaluation including enlightenment, accountability, programme improvement, clarification or development and symbolic reasons (1). One of our major objectives was accountability, being the obligation to report on the expenditure of public funds, validate the programme objectives and degree of implementation, and achievement of clinical goals.
Generic evaluation questions were:
-
1
Is the programme reaching the target population?
-
2
Is the programme being implemented in the ways specified?
-
3
Is the programme effective?
-
4
How much does the programme cost?
-
5
What is the cost of the programme relative to its effectiveness?
At this stage, we have assessed immediate outcomes (1 and 2) concerning deployment.
Using the Institute for Healthcare Improvement Assessment Scale for Collaboratives (14) the eight sites were rated as:
-
•
2·0: Activity, but no changes – one tertiary referral hospital;
-
•
2·5: Changes tested, but no improvement – one tertiary, three district hospitals and domiciliary care;
-
•
3·0: Modest improvement – one district hospital;
-
•
3·5: Improvement – one district hospital.
A survey of the 35 staff involved in the wound care programme found that 97% stated the programme was achieving its goals, positively influencing clinical care and the clinician's ability to provide best practice and supporting change locally. In addition, staff reported that guidelines enhanced their morale through empowerment and access to information. Along with participation in our extensive education and training programme, this increased professional knowledge.
Of the approximately 30 policies and guidelines identified as in need of development or revision, half were completed over a period of 17 months.
Various wound care interventions were monitored as bundles of care and analysed appropriately (15) using MINITAB™ statistical software (16). ‘Bundles’ comprise a small number of proven interventions, often three to five, and known to improve clinical outcomes. Performance related to leg ulcer management guidelines is provided as exemplars of bundle monitoring.
Composite compliance indicators monitor the proportion of all care that was given. Less than 100% means patients received some care bundle interventions but not all. Credit is given for incomplete or partial care.
Figure 2 shows a control chart with the first audit achieving 26% compliance and the second audit achieving 84%. Statistical significance is identified by at least one, and in this case two, datum being outside of the upper control limit (UCL) and or lower control limit (LCL) which is set at three standard deviations (SD) from the mean (green line), being the red horizontal lines. Control charts are dissimilar from classical biostatistical tests. Three SDs are the default for control charts in most statistical software packages as the aim is to be sensitive enough to quickly signal when a special cause exist, that is the data are not random. Using three SDs also means that the chart should rarely signal a ‘false alarm’ when the data are random. Whilst Figure 2 produced an average compliance of 57%, the process exhibits special cause variation, being one or more points outside of the red control limits, making calculation of the summary statistics at right inaccurate.
Figure 2.
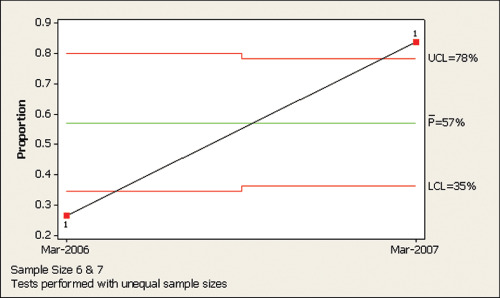
Composite compliance: proportion of leg ulcer bundle implemented – March 2006 and March 2007.
Figure 3 shows how a control chart should be split so that only common cause variation is displayed in the second part of the chart along with appropriate summary statistics, at right. This is called an historical control chart. The 2007 process shows a performance of 84% and can be predicted, unless there is significant change to the fundamental process, to achieve between 68% and 100% in future audits. However, with only one datum, prediction should be extremely cautious.
Figure 3.
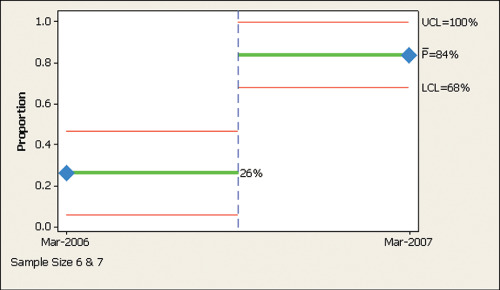
Historical control chart. Composite compliance: proportion of leg ulcer bundle implemented – March 2006 and March 2007.
A more sensitive indicator than composite compliance is the proportion of patients who receive all elements of the care bundle or the perfect process. Figure 4 shows that on average only 7·7% of patients received the perfect process compared with 84% composite compliance in Figure 3. Measuring the perfect process monitors the provision of all care the patient is eligible for which more closely reflects the interests and likely desires of patients and their families.
Figure 4.
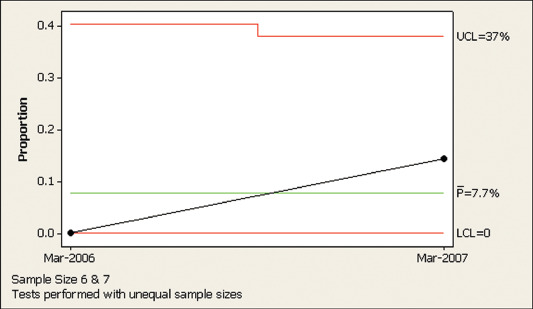
Perfect process: proportion of patients receive full leg ulcer bundle – March 2006 and March 2007.
Each intervention in the care bundle should be monitored separately, as in Figure 5, to give direction to specific areas of non compliance. In this case, ‘referral to specialist' is the lowest achieving indicator at around 20%. As the next highest bundle intervention of Ankle Brachial Pressure Index (ABPI) performs at 57%, referral to specialist is clearly special cause variation which should be addressed.
Figure 5.
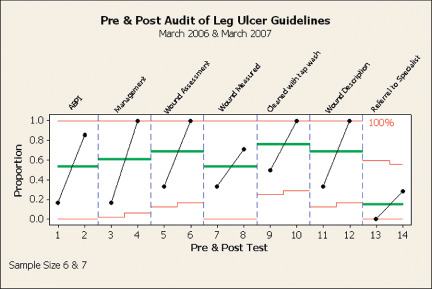
Pre‐ and post‐audit of leg ulcer guidelines – March 2006 and March 2007.
One district hospital achieved a result of 20% of patients attaining wound healing within the goal of 10 days.
Ongoing improvements to the wound care programme continue to be implemented over time. A wound assessment, treatment and evaluation form was implemented in early 2009. Figure 6 shows that five of the eight key documentation requirements are achieving at or above the intermediate goal of 75%. In this case, simple data display as with bar graphs is deemed appropriate, for wards and the area wound care committee.
Figure 6.
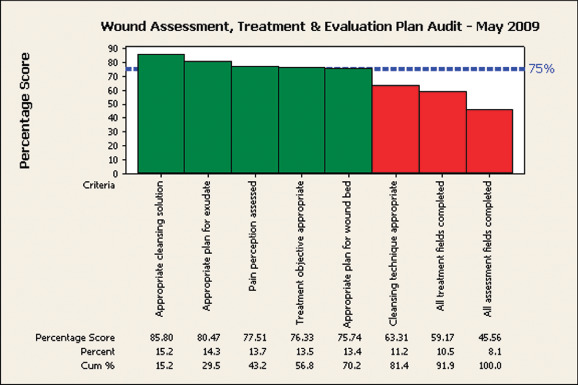
NSCCHS wound assessment, treatment and evaluation plan audit – May 2009.
There were six wound care committees across ten sites and a good evaluation includes comparisons, where appropriate. A bar graph is not the appropriate analysis when comparing the sites to determine who is performing differently from the rest. Figure 7 shows that, as expected, half the sites are performing above average and half are below the average of 70% as shown by the green horizontal line. But the graph also shows that all six sites are within three SDs of the system average as represented by the red horizontal control limits which are of varying height because of the disparate number of audits conducted at each site. This means that whilst each site is performing numerically different from another, there is no statistically significant difference in performance with the data provided. The goal then becomes to change, upward, the performance of all sites.
Figure 7.
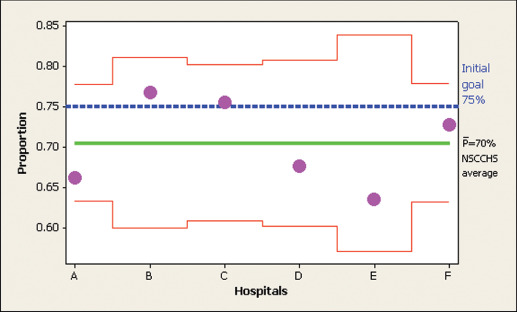
NSCCHS wound care assessment and treatment plan evaluation (n = 169) – May 2009.
DISCUSSION
Early results have showed that the aim of providing appropriate and effective care has begun. But much more needs to be performed and achieved.
Evaluations of multi‐faceted programmes suffer from the difficulty of disentangling the impact of programme activities from that of external influences. However, the indicators monitored included a series of intermediate results in the cause and effect chain. Monitoring of health outcomes was also conducted where possible.
Our goal was also to effect positive change on population health, and this can be attained by encouraging and facilitating an increase in health education. External community sharing and easy access to guidelines for the community and public were enabled by publishing the guidelines on the internet. These assist other key partners involved in wound care to improve patient outcomes, continuity of care and share the great work of our wound care programme.
This article sought to publish a generic template of structures and processes which can be used to achieve wound healing. When there is a generic patient care problem, it makes sense for there to be a collaborative approach, involving all salient professional and patient/carer groups, to work together. Even at this early stage of evaluation, we are sure that safe, consistent, appropriate care is being provided across the patient journey.
A well‐implemented project has been developed into a programme which is demonstrating limited success at this early stage.
ACKNOWLEDGEMENTS
We acknowledge the clinical teams which participated in developing and implementing the programme. We thank Sharon McKinley, Professor of Critical Care Nursing – University of Technology, Sydney and NSCCHS for her assistance in reading and editing this article.
REFERENCES
- 1. Owen JM. Program evaluation: forms and approaches. Sydney: Allen and Unwin, 1993. [Google Scholar]
- 2. Madsen W, Reid‐Searl K. Overcoming tradition: teaching wound management into the twenty‐first century. Collegian 2007;14:7–10. [Google Scholar]
- 3. Gottrup F. Multidisciplinary wound healing concepts. EWMA J 2003;3:5–11. [Google Scholar]
- 4. NHS Modernisation Agency. Improvement leaders' guide to sustainability and spread. London: Ancient House Printing Group, 2002. [Google Scholar]
- 5. Australian Wound Management Association. Wound awareness campaign 2008 [WWW document]. URL www.elephantintheroom.com.au [accessed on 13 April 2008].
- 6. McNaughton V, Orsead HL. Surgical site infections in community care clients – early detection and rational care through recognition of client specific risk factors. Wound Care Can 2005;3:10–13. [Google Scholar]
- 7. Zoutman D, McDonald S, Vethanayagan D. Total and attributable cost of surgical wound infections at a Canadian tertiary‐care centre. Infect Control Hosp Epidemiol 1998;19:254–9. [DOI] [PubMed] [Google Scholar]
- 8. Health Protection. Scotland health protection report Scotland – November 2007 [WWW document]. URL www.hps.scot.nhs.uk/ewr/article.aspx [accessed on 12 April 2008].
- 9. Baker SR, Stacey MC, Hoskins SE, Thompson PJ. Aetiology of chronic ulcers. Eur J Vasc Surg 1992;6:245–51. [DOI] [PubMed] [Google Scholar]
- 10. Bennett G, Moody M. Wound care for health professional. London: Chapman Hall, 1995. [Google Scholar]
- 11. URL http://www.health.wa.gov.au/WoundsWest/docs/WWWPS_08_State‐wide_Report_overview.pdf [accessed on 17 June 2010].
- 12. Joiner BL. Fourth generation management: the new business consciousness. New York: Joiner Associates Incorporated, 1994. [Google Scholar]
- 13. Blanchard KH, Zigarmi P, Zigarmi D. Leadership and the one minute manager: increasing effectiveness through situational leadership. New York: Harper Collins, 1985. [Google Scholar]
- 14. URL http://www.ihi.org/NR/rdonlyres/84B476B5‐0C6E‐48F6‐8B7F‐F86EB155EA06/665/AssessmentScaleforCollaboratives1.pdf [accessed on 8 December 2008].
- 15. Nolan T, Berwick D. None‐or‐all measurement raises the bar on performance. JAMA 2006;295: 1168–70. [DOI] [PubMed] [Google Scholar]
- 16. Minitab, Inc. Minitab 15 Statistical Software (2007). [Computer software]. State College, PA [WWW document]. URL www.minitab.com [accessed on 29 August 2009].


