Abstract
The objective of the study was to assess the cost‐effectiveness of Vacuum Assisted Closure® (V.A.C.®) Therapy compared with advanced wound care (AWC) for the treatment of diabetic foot ulcers (DFUs) in France. A cost‐effectiveness model intended to reflect the management of DFUs was updated for the French setting. The Markov model follows the progression of 1000 hypothetical patients over a 1‐year period. The model was populated with French‐specific data, obtained from published sources and clinical experts. The analysis evaluated costs and health outcomes, in terms of quality‐adjusted life‐years (QALYs), wounds healed and amputations, from the perspective of the payer. The patients treated with V.A.C.® Therapy experienced more QALYs (0·787 versus 0·784) and improved healing rates (50·2% versus 48·5%) at a lower total cost of care (€24 881 versus €28 855 per patient per year) when compared with AWC. Sensitivity analyses conducted around key model parameters indicated that the results were affected by hospital resource use and costs. DFU treatment using V.A.C.® Therapy in France was associated with lower costs, additional QALYs, more healed ulcers and fewer amputations than treatment with AWC. V.A.C.® Therapy was therefore found to be the dominant treatment option.
Keywords: Cost‐effectiveness, Diabetic foot ulcers, Negative pressure therapy, V.A.C.® Therapy
INTRODUCTION
Foot ulceration is a common and disabling complication associated with diabetes (1). The prevalence of diabetes is growing rapidly worldwide (2); the prevalence of drug‐treated diabetes in France is estimated to be 4%, corresponding to 2·5 million individuals (3). The lifetime risk of a person with diabetes developing a foot ulcer is as high as 25% (4); the significant economic and patient burden associated with this is increasingly recognised (5).
Diabetic foot ulcers (DFUs) can result in infection, gangrene and may ultimately lead to amputation (6). Treatment of such wounds can be very complicated and can thus place pressure on health care resources because of prolonged hospitalisation, rehabilitation and home nursing care (7). In addition to the financial costs, DFUs have a significant impact on the health‐related quality of life of individuals (8).
A range of treatments is marketed for DFUs including advanced wound therapy (e.g. alginates and hydrogels), bioengineered tissue or skin substitutes and negative pressure therapy using foam dressings. Negative pressure therapy, using V.A.C.® Therapy, involves the controlled application of negative pressure to the wound site. Open‐cell foam dressings are cut to size, placed in the wound, covered with an adhesive drape and a pressure sensing pad allowing the therapy unit to monitor and adjust the negative pressure. Tubing connects the pad and foam to a canister housed in the computerised therapy unit that intermittently or continuously generates the negative pressure to draw wound fluid through the foam dressing and into the canister (9). A moist wound environment is created which promotes wound healing and prepares the wound bed for closure (10).
Evidence has shown V.A.C.® Therapy to improve clinical treatment outcomes in DFU patients, with significant improvements in wound volume and healing rates when compared with standard moist wound care 10, 11, 12, 13. Although the clinical effectiveness of V.A.C.® Therapy is well established, the treatment regime is often perceived as more costly than traditional and advanced wound dressings; hence in the context of cost‐containment measures in European health care systems, economic evaluations are becoming crucial for optimal use of allocated resources. Various health economic publications are available about negative pressure therapy 7, 10, 11, 14, 15, 16, 17, 18, 19, 20, 21, 22. However, these do not entirely reflect the French health care setting specifically (e.g. costs and comparators used do not reflect the French standard of care). An economic model was developed by Flack et al. (20), for USA to determine the cost‐effectiveness of V.A.C.® Therapy compared with traditional or advanced wound care (AWC). V.A.C.® Therapy was found to be the dominant treatment option, that is, it was found to be more effective and lower cost than alternative treatment strategies. However, it should be acknowledged that the model was characterised by a number of assumptions regarding the effectiveness of treatment, because of the absence of long‐term outcomes on the strategies considered.
The objective of this study was to adapt the existing model by Flack et al. (20) to the French setting in order to establish the cost‐effectiveness of V.A.C.® Therapy compared with other advanced wound dressings for the treatment of DFUs in France, specifically. The analysis evaluated costs and health outcomes, in terms of quality‐adjusted life‐years (QALYs), in addition to clinical endpoints such as amputations and wounds healed.
METHODS
A cost‐effectiveness model has previously been developed for the analysis of V.A.C.® Therapy (KCI, San Antonio, TX) for DFU care in USA (20). The French analysis in this study is based on the original model structure (20) but has been updated to incorporate more relevant or recent data reflective of the current DFU treatment practices in France. The model structure and data inputs were reviewed by clinical experts in France to ensure local practice patterns were reflected. All data used in the model were derived from published sources wherever available 6, 10, 11, 23, 24. Where this was not possible, then values were elicited from clinical experts based in France.
The French adaptation of the model considers the cost‐effectiveness of V.A.C.® Therapy technology in comparison with other advanced wound dressings. Any evaluation which seeks to compare an intervention to AWC is challenging. AWC is a term taken to comprise a range of technologies, and while there are relatively few studies that show any difference in effect between these dressings, there are differences in the cost of the dressings. As such, attempts were made to identify an AWC regimen that was deemed to be relevant to France and supported by evidence. The choice of comparator was determined through consultation with clinical experts based in France. It was decided that a combination of Algosteril® (Laboratoires Brothier, Nanterre, France) alginate with Adaptic® (Systagenix Wound Management, Gargrave, UK) could be considered to be representative of the standard practice for wound management in France. The costs of the AWC treatment considered in the model are based on this regimen.
The model
The existing model has been described in detail elsewhere (20), hence we will summarise only the main points here. The model takes a Markov approach in order to follow the progression of 1000 hypothetical patients' DFUs, using various health states. Markov models enable a complex prognosis to be modelled through transitions between disease states over a series of discrete time periods, that is, cycles (25). The model is based on a time horizon of 1 year and uses monthly Markov cycles; at the end of each month patients can be in one of the following seven health states (Figure 1):
Figure 1.
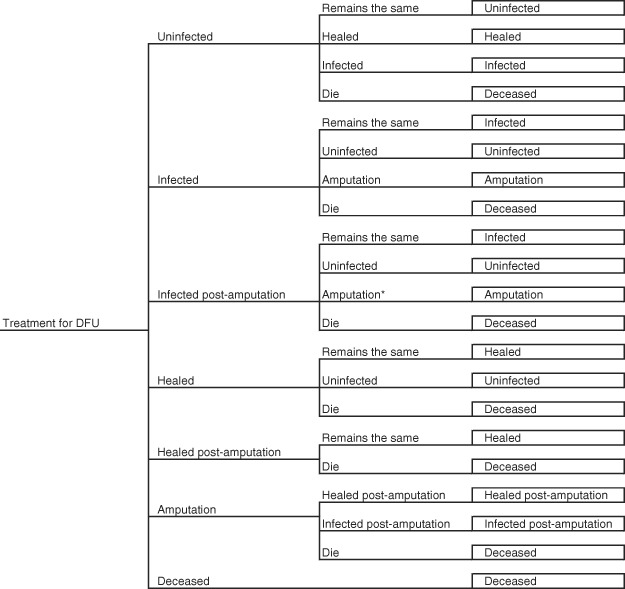
Diabetic foot ulcer model structure. * indicates second amputation.
-
•
Uninfected ulcer
-
•
Infected ulcer
-
•
Infected ulcer post‐amputation
-
•
Healed
-
•
Healed post‐amputation
-
•
Amputation
-
•
Dead
The possibility of progressing between the different health states is made on a clinical basis, because it may be possible to move between some states and not between others. For example, patients cannot move immediately from an infected ulcer to a healed ulcer; they must first progress to the uninfected state and subsequently move on to the healed state. It is not possible to move from the death state, as this is an absorbing state. The model enables the recurrence of disease states, such as infections being able to occur more than once over the course of 1 year; for example, a healed ulcer patient could encounter an infection by moving to an uninfected state and subsequently to an infected state.
If V.A.C.® patients have a wound which remains unhealed after 3 months of treatment, they are assumed to be non responders and switch to the advanced dressing arm. It is assumed that patients treated with advanced dressings continue with their treatment for the full 12 months if they remain unhealed.
Patients
The simulated DFU patients have either type 1 or type 2 diabetes and are aged 50–65 years. The model assumes that all patient characteristics other than the treatment regimes are equal, such as wound size and wound duration. It is assumed that on entering the model, patients have not previously undergone an amputation. The ratio of patients who enter the model with an infection has been updated from the US version; 28% of patients present with an infected DFU (10), and the remaining 72% present with an unhealed, uninfected DFU. The model accounts for the possibility that some infected ulcers are infected with gangrene and therefore encounter higher costs than those not infected with gangrene; 75% of infected ulcers are gangrenous (24).
Probabilities
The monthly transition probabilities between the health states are based on the published sources used for the original V.A.C.® model 6, 11, 23, 26, 27. Transition states for the AWC arm remain unchanged from the original model developed for USA.
Effectiveness data
Clinical effectiveness data on healing rates have been updated to incorporate findings from a recent study by Blume et al. (10). This randomised controlled trial (RCT) of over 300 patients found that those treated with V.A.C.® Therapy were 1·49 times more likely to heal than patients with advanced wound dressings (probability of healing is 43% for V.A.C.® Therapy and 29% for AWC). Healing times are based on data from the study by Armstrong and Lavery which focused on diabetic patients with partial foot amputation wounds; V.A.C.® patients take 1·8 months to heal compared with 2·5 months for AWC patients (11).
Utilities are used in economic evaluations in order to measure the benefits of a health care treatment or intervention. Utility values for the health states are sourced from the study by Redekop et al. (28), which estimated utility scores for health states involving foot ulcers and amputations (Table 1). The utility scores are used in order to generate QALYs for patients. QALYs take into account the impact of treatments on life expectancy as well as quality of life. Although there is no immediate reason to expect any difference in life expectancy in the two arms considered, extending the period without ulceration, infection and/or amputation should improve quality of life. The QALY is increasingly used in economic evaluations as it provides a single composite measure of treatment outcome.
Table 1.
Utility values used in the model
| Health state | Utility value |
|---|---|
| Uninfected ulcer | 0·75 |
| Infected ulcer | 0·70 |
| Infected ulcer post‐amputation | 0·60 |
| Healed ulcer | 0·84 |
| Healed ulcer post‐amputation | 0·64 |
| Amputation | 0·64 |
| Deceased | 0·00 |
Source: Redekop et al. (28).
Resource use
The monthly resource use for each DFU health state was established by conducting interviews with clinical experts who have experience of French DFU treatment practices. Resources considered in the model include inpatient and outpatient resources for each health state, with the full list provided in Table 2. The resource use items include:
Table 2.
Resource use per month according to health state, for V.A.C.® Therapy and AWC
| Uninfected ulcer | Infected ulcer | Infected post‐amputation | Amputation | |||||
|---|---|---|---|---|---|---|---|---|
| New cases | Old cases | New cases | Old cases | New cases | Old cases | |||
| Inpatient costs | ||||||||
| Average hospital stay * | VAC | 0·0 | 0·0 | 22·5 | 0·0 | 18·3 | 0·0 | 0·0 |
| AWC | 0·0 | 0·0 | 31·5 | 0·0 | 18·3 | 0·0 | 0·0 | |
| Number of nurse visits † | VAC | 0·0 | 0·0 | 9·0 | 0·0 | 7·3 | 0·0 | 12·2 |
| AWC | 0·0 | 0·0 | 30·4 | 0·0 | 18·3 | 0·0 | 30·4 | |
| Number of dressing changes | VAC ‡ | 12·2 | 12·2 | 12·2 | 12·2 | 12·2 | 12·2 | 12·2 |
| AWC § | 30·4 | 30·4 | 30·4 | 30·4 | 30·4 | 30·4 | 30·4 | |
| Number of canister changes | VAC ¶ | 7·6 | 7·6 | 7·6 | 7·6 | 7·6 | 7·6 | 7·6 |
| Day case visits in hospital | Both ** | 1·0 | 1·0 | 0·0 | 1·0 | 0·0 | 1·0 | 2·0 |
| Antibiotics courses | Both | 100% | 100% | |||||
| Orthopaedic appliances | Both | 100% | 100% | |||||
| Surgery (amputation) | Both | 100% | ||||||
| Prostheses | Both | 100% | ||||||
| Outpatient costs | ||||||||
| Home care (nurse) visits †† | VAC | 12·2 | 12·2 | 3·2 | 12·2 | 4·9 | 12·2 | 1·0 |
| AWC | 30·4 | 30·4 | 0·0 | 30·4 | 12·2 | 30·4 | 1·0 | |
| Specialist consultations | Both | 2·0 | 0·0 | 2·0 | 1·0 | 2·0 | 1·0 | 1·0 |
| Tests | Both | 100% | 100% | |||||
Percentages indicate the proportion of patients that the cost is applied to; in addition, healed patients visit the specialist 0·33 times per month, on average. Source: expert clinical opinion and V.A.C.® Therapy treatment guidelines.
V.A.C., Vacuum Assisted Closure; AWC, advanced wound care.
*Hospital stay includes nurse (not specific to dressings) and physician visits.
†Nurse visits specific to dressing changes when in hospital.
‡V.A.C.® Therapy dressings are changed every 48–72 hours.
§AWC dressings are changed every day.
¶Canister is changed every 3–5 days.
**Day visit lasts for 1·5 hours on average.
††Home care nurse visits for the period of time not in hospital.
-
•
The number of days spent as an inpatient
-
•
Nurse and physician visits
-
•
Use of orthopaedic appliances and prostheses
-
•
Antibiotic regimens and tests
-
•
Outpatient consultations
-
•
Home care visits
Additional resource use categories considered to be representative of French practice have been incorporated in the model, such as specialist visits, day case visits and offloading devices. In order to generate the average stay in hospital, clinical experts were asked to determine the proportion of patients who are hospitalised and the typical duration of the hospital stay for these individuals, acknowledging that not all patients who experience a DFU will require hospitalisation.
To capture the distinction between resources used in the initial, more intensive treatment phase and those used in later phases for the uninfected and infected ulcer states, the model incorporates costs for the initial month following the development of an ulcer as well as subsequent months. This is intended to be more representative than assuming that resource use remains constant over the course of managing an ulcer.
Cost data
Country‐specific cost data were sourced from established databases. When available, inpatient costs were retrieved from national price lists. The prices of consumables such as Algosteril® and Adaptic® dressings were obtained from the national medical aids reimbursement price list (Liste des Produits et Prestations Remboursables) (29). The costs associated with the use of V.A.C.® Therapy were provided by the manufacturer of the device (Laboratoires KCI Médical, Chilly Mazarin France). Dressing prices for both therapeutic strategies were calculated averages of prices for small and medium dressing sizes (hence excluding large dressings) usually used in clinical practice for the treatment of patients with DFUs.
Daily inpatient costs relating to patient hospitalisation are based on average daily tariffs charged by the hospitals and were calculated from various price lists of a selected number of French hospitals that were publicly available. Tariffs for outpatient visits and laboratory tests were retrieved from the national procedure price lists 30, 31. Orthopaedic appliances (e.g. prostheses, offloading devices) were provided by the same hospital in the Toulouse area. The costs for procedures in the hospital (e.g. amputation) and rehabilitation stays were taken from the national costs scale (Echelle Nationale des Coûts) (32).
Hospital personnel costs for physicians and nurses were calculated based on the national scale of annual salaries and an estimation of hours worked per year 33, 34. Finally, medication costs, for treating patients with infections, were either retrieved from the French ‘red book’ Vidal (for branded medication)(35) or from the national generics medication price list (36).
The model incorporates all relevant treatment costs and the costs associated with the various resources detailed above. The cost for each health state is calculated by multiplying the unit cost for the health care resources used when in that state by the volume of resources used. All costs are evaluated in 2008/2009 Euros. Unit costs are presented in Table 3.
Table 3.
Cost estimates used in the model (costs in 2008/2009 € values)
| Resource | Unit cost (€) |
|---|---|
| Inpatient costs | |
| Hospital cost per day | 790 |
| Hospital nurse visit | 24 |
| Day case in hospital | 79 |
| Antibiotics per course (infected patient) | 411 |
| Orthopaedic appliances | 132 |
| Amputation | 6679 |
| Prostheses | 885 |
| Outpatient costs | |
| Outpatient nurse clinic visit | 22 |
| Outpatient physician/specialist clinic visit | 28 |
| Home care (nurse) visit | 14 |
| Tests (infected patient) | 128 |
| Tests (infected post‐amputation patient) | 39 |
| Dressing costs | |
| V.A.C.® Therapy costs per dressing | 47 |
| ActiV.A.C.® Canister | 48 |
| Adaptic gauze | 1 |
| Alginate (Algosteril®) | 4 |
Analysis
The analysis is undertaken from the perspective of the payer, hence only direct costs are included. Because of the time horizon of the analysis being 1 year, costs and health benefits were not discounted.
The model investigates health outcomes in terms of QALYs and the number of amputations. Hence, the economic analysis generates results in the form of the incremental cost per QALY and the cost per amputation avoided.
Sensitivity analyses were conducted around key model parameters such as the price of V.A.C.® Therapy hospital stay, and the assumption of unhealed V.A.C.® patients switching to advanced wound dressings after 3 months in the base case was also explored. An additional analysis has been conducted to investigate the impact of an alternative proportion of patients entering the model with an infected DFU. The alternative value is based on findings from the Eurodiale Study (37), a prospective cohort study of 1232 DFU patients across Europe, which reported that 57·2% of patients present with an infected DFU.
RESULTS
Base case analysis
For the comparison of V.A.C.® Therapy against AWC, V.A.C.® Therapy was found to be the dominant treatment option for all outcomes explored in the analysis, that is:
-
•
V.A.C.® Therapy results in less amputations, at a lower cost
-
•
V.A.C.® Therapy results in more ulcers healed, at a lower cost
-
•
V.A.C.® Therapy results in more QALYs, at a lower cost
Hence, patients treated with V.A.C.® Therapy experienced more QALYs, more healed wounds and fewer amputations at a lower total cost of care. Treatment using V.A.C.® Therapy was associated with a total cost per patient per year of € 24 881 compared with € 28 855 per AWC patient. V.A.C.® Therapy generated 0·787 QALYs per patient compared with 0·784 QALYs per AWC patient. The results are shown in Table 4.
Table 4.
Results of V.A.C.® Therapy versus AWC for a cohort of 1000 patients, over a 12‐month period
| Outcomes | Costs (€) | Incremental cost per QALY | |||
|---|---|---|---|---|---|
| Amputations | Wounds healed | QALYs | |||
| V.A.C.® Therapy | 1·456 | 502 | 787 | 24 881 226 | |
| AWC | 1·459 | 485 | 784 | 28 854 981 | |
| Incremental | −0·003 | 18 | 3 | −3 973 755 | Dominates * |
V.A.C.®, Vacuum Assisted Closure; AWC, advanced wound care; QALY, quality‐adjusted life‐year.
*V.A.C.® Therapy results in more QALYs, at a lower cost.
More patients healed in the V.A.C.® Therapy group at 12 months, specifically 50·2% of the ulcers in the V.A.C.® cohort healed compared with 48·5% of those in the AWC cohort. The model predicted that over a period of 1 year, the number of amputations was lower for the V.A.C.® Therapy treatment arm compared with the AWC cohort, at 1·456 amputations compared with 1·459 amputations per 1000 patients, respectively. Patients treated with V.A.C.® Therapy benefited from additional ulcer‐free months; 4·40 compared with 3·79 per patient.
Additional analysis based on the Eurodiale Study: infected DFU patients
The analysis involving an alternative proportion of patients entering the model with an infected DFU (57·2%) resulted in higher costs and fewer QALYs for both of the treatment options. The total cost per patient per year was €39 917 and €48 915 for V.A.C.® Therapy and AWC, respectively. The corresponding QALYs were estimated to be 0·768 per V.A.C.® patient and 0·766 per AWC patient. The results of the additional analysis are displayed in Table 5.
Table 5.
Additional analysis of V.A.C.® Therapy versus AWC, using Eurodiale Study (37) for infected DFU patients *
| Outcomes: | Costs (€) | Incremental cost per QALY | |||
|---|---|---|---|---|---|
| Amputations | Wounds healed | QALYs | |||
| V.A.C.® Therapy | 2·330 | 418 | 768 | 39 916 496 | |
| AWC | 2·333 | 406 | 766 | 48 914 852 | |
| Incremental | −0·003 | 11 | 2 | −8 998 356 | Dominates † |
*For a cohort of 1000 patients, over a period of 12 months.
†V.A.C.® Therapy results in more QALYs, at a lower cost.
V.A.C.®, Vacuum Assisted Closure; AWC, advanced wound care; DFU, diabetic foot ulcer; QALY, quality‐adjusted life‐year.
Sensitivity analysis
Sensitivity analyses established the robustness of the model findings to variations in key parameters. The V.A.C.® acquisition costs had only a modest impact on the overall results; when V.A.C.® acquisition costs were doubled, the resulting annual cost per V.A.C.® patient of € 28 426 was still below that of AWC. The total costs of the two treatment arms equalised as the V.A.C.® acquisition cost was increased to approximately 2·1 times its actual cost.
If V.A.C.® patients who remain unhealed at 3 months continued on the V.A.C.® Therapy regimen for the full 12 months, rather than switching to AWC, then V.A.C.® Therapy had an associated cost of € 27 133 per patient per year, with QALYs unchanged. Inputs surrounding hospitalisation were influential, with costs rising to € 30 554 per V.A.C.® patient when V.A.C.® Therapy hospitalisation resource use was equivalent to that of the comparator. As a result of halving the cost of a hospital day, per‐patient costs reduced to € 16 943 and € 18 151 for V.A.C.® Therapy and AWC, respectively.
DISCUSSION
The results of this analysis indicate that V.A.C.® Therapy is a valuable treatment option for patients with DFUs, when compared with AWC in France. V.A.C.® Therapy was found to be dominant because of being less costly and more effective than the comparator. The clinical effectiveness of V.A.C.® Therapy is well established 10, 11, 12, 13; however, there is a paucity of cost‐effectiveness studies. The results from our study are expected to inform decision‐makers when selecting DFU treatments that show value for money in addition to clinical effectiveness in France. Our results are in line with the findings from the original US model, which also showed V.A.C.® Therapy to be the dominant strategy (20).
There was a trend towards marginal benefits in terms of the effectiveness endpoints considered in the analysis, at lower cost. The reasons behind the differences in wounds healed, amputations averted and QALYs gained being modest in magnitude include the short time horizon of the analysis (1 year) and the relatively low event rates which are not expected to differ considerably across treatment arms. It is important to note that the outcomes, such as the 0·784 QALYs and 0·787 QALYs gained for AWC and V.A.C.® Therapy patients, respectively, show a clinically important difference for individuals with DFUs. Considered at a cohort level, there were meaningful reductions in events, such as ulcers healed and amputations; however, it is recognised that over a 1‐year time period the differences at a per‐patient level are likely to be relatively small. It should be acknowledged that even if the two treatment arms are assumed to result in similar outcomes, V.A.C.® Therapy results in cost savings. The model has shown that, on average, annual savings of approximately €4000 can be realised for a DFU patient treated with V.A.C.® Therapy. Taking into account that between around 37 500 and 112 500 patients (1·5–4·5% (38) of 2·5 million DFU patients (3)) have DFUs in France, the potential cost savings could be substantial.
Despite the acquisition costs for the components of V.A.C.® Therapy being more expensive than AWC, the savings because of lower resource usage for V.A.C.® patients ultimately led to V.A.C.® Therapy being less expensive overall. A large proportion of the difference in costs between the two treatment arms arose from the reduced hospital stay for infected ulcer patients treated with V.A.C.® Therapy as opposed to AWC. In addition, V.A.C.® patients required fewer dressing changes, hence the associated nurse inpatient visits and home care visits were lower. Where the analysis included higher initial numbers of infected DFU patients, the cost differences became more significant in magnitude.
The term ‘advanced wound care’ can be used to encapsulate many different types of dressing. It is acknowledged that there are a range of advanced wound dressings that could have been included in our analysis. However, for the purposes of this study, AWC was costed on the basis of Adaptic® and Algosteril® which are considered to be a fair reflection of the standard of advanced wound dressings used in France. Evidence on the effectiveness of AWC dressings was derived from the original analysis conducted in USA, which was based on studies of various dressings, including Dermagraft® (Advanced BioHealing Inc., Westport, CT) and Apligraf® (Organogenesis Inc., Canton, MA). Clearly, the use of different therapies to derive costs and effectiveness is not ideal and an assumption that advanced wound dressings can be treated as a ‘class’ of products is also open to scrutiny. However, these assumptions were adopted because of the absence of robust trials of specific AWC dressings that might be considered to be representative of practice in France.
It should be emphasised that the analysis was undertaken for a duration of 1 year only. Therefore, the benefits (i.e. QALY gains, improved wound healing rates, fewer amputations) predicted by the model, which appear to be modest in the base case, are likely to be greater if extrapolated over a longer period. For instance, if results are extrapolated over a 2‐year or 3‐year time horizon, the cost savings increase to €4109 and €4146 per patient, respectively, with associated QALY gains of 0·004 for the two time horizons (as opposed to 0·03 for a 1‐year time horizon). However, the evidence that is currently available does not support extrapolation beyond a 1‐year time period, and any predictions beyond 1 year would be characterised by significant uncertainty.
Any economic model should be regarded as a simplified representation of the real world and as such, all model results are characterised by uncertainty and limitations. The main limitations in respect of this exercise relate to the availability of data to populate the model and the reliance on assumptions and clinical expertise to address gaps in the evidence. Limitations relating to the model structure and assumptions include the omission of a health state for ‘non‐infected ulcer post‐amputation’, and the potential for overlap between the ‘healed post‐amputation’ and ‘amputation’ health states. The use of monthly transitions between health states could also be seen as a limitation.
French‐specific data for resource use were established using clinical expert opinion and best practice guidelines (e.g. regarding dressing and canister changes). The experts interviewed were selected on the basis of their experience being relevant for the patient population considered by the model. The clinicians comprised of qualified physicians and professors with experience of practising and teaching in the area of nutritional diabetology, and specific experience of treating patients with DFUs in France, where some are specialised in the areas of infection more than others. Where views differed as to the resources used, the most commonly occurring response was inputted, or failing this mid‐values were taken. Where it was not possible to use data on this basis, because of the detailed nature of the data for example, the expert with the most relevant experience to the particular health state was used for the resource use information.
As previously highlighted for the original model (20), the model uses the best available data from a combination of sources from different countries. Although RCT evidence was used for the effectiveness data, further robust studies comparing V.A.C.® Therapy to AWC are needed in order to enable comprehensive economic analyses. One particular problem relating to effectiveness is the availability of high‐quality evidence on specific AWC regimens, which often leads to the synthesis of evidence on a number of different dressings to represent the effectiveness of AWC.
A conservative approach was taken wherever possible for the analysis. For example, where transition probabilities between health states were not available for V.A.C.® Therapy, these were assumed to be equivalent to advanced dressings. Because of an absence of evidence relating to transition probabilities for Algosteril® plus Adaptic® dressing, probabilities from the earlier evaluation by Flack et al. (20) were used, which were based on RCT data. As such, the comparator arm might be considered to be based on effectiveness evidence for treatments which are at the more aggressive end of the spectrum of AWC dressings, while costs are based on less expensive treatments. It is therefore probable that the benefits associated with V.A.C.® Therapy when compared with AWC have been underestimated by the model.
The challenges of effective wound management are becoming increasingly complex. The evidence relating to the effectiveness of V.A.C.® Therapy has been the topic of various discussions and summarised by recent reviews and consensus documents 39, 40, 41, 42. A systematic review considered RCT evidence of the therapy for patients with a range of wound types (39). The review concluded that, in general, there is little evidence to support V.A.C.® Therapy for wound treatment. It is worthwhile to note that of the 15 studies reviewed, only four related to diabetic wounds, with the majority involving small patient groups, and several shortcomings of the RCTs included in the review were highlighted. In contrast, a separate review reported various benefits associated with V.A.C.® Therapy such as more rapid wound healing, reduced complication rates and increased patient survival (40). In line with recommendations from the first review, further rigorous evaluation into negative pressure treatment is advised 39, 40. Consensus documents summarise the use of V.A.C.® Therapy and state that it can be used in a number of ways for the management of complex DFUs, with further evaluation into the economic impact of the therapy recommended 41, 42.
CONCLUSION
This analysis has showed that V.A.C.® Therapy is more effective and less costly compared with AWC for DFU treatment in France. Patients treated with V.A.C.® Therapy experienced additional QALYs, more healed ulcers and had fewer amputations than patients treated with advanced wound dressings. Because of the overall cost of care being lower for V.A.C.® patients, this was found to be the dominant treatment option.
ACKNOWLEDGEMENTS
Funding for this study was provided by KCI Europe Holding (Amstelveen, the Netherlands). VL Forest‐Bendien, an employee of KCI Europe Holding, was involved in the data collection. This work is attributed to York Health Economics Consortium, University of York, UK. The V.A.C.® Therapy System and certain components and methods are subject to one or more of the following patents: USA: 5636643, 5645081, 6142982, 6345623, 6553998, 6814079, 7004915, 7198046, 7216651; EU: EP777504, EP620720, EP865304, EP1088569, EP853950, EP1018967, EP1219311, EP1440667; other patents pending.
REFERENCES
- 1. Markowitz JS, Gutterman EM, Magee G, Margolis DJ. Risk of amputation in patients with diabetic foot ulcers: a claims‐based study. Wound Repair Regen 2006;14:11–7. [DOI] [PubMed] [Google Scholar]
- 2. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–53. [DOI] [PubMed] [Google Scholar]
- 3. Kusnik‐Joinville O, Weill A, Ricordeau P, Allemand H. Diabete traité en France 2007: un taux de prévalence proche de 4% et des disparités géographiques croissantes. Bull Epidémiol Hebd 2008;43:409–13. [Google Scholar]
- 4. Frykberg RG, Zgonis T, Armstrong DG, Driver VR, Giurini JM, Kravitz SR, Landsman AS, Lavery LA, Moore JC, Schuberth JM, Wukich DK, Andersen C, Vanore JV; American College of Foot and Ankle Surgeons. Diabetic foot disorders: a clinical practice guideline. J Foot Ankle Surg 2006;45:S1–66. [DOI] [PubMed] [Google Scholar]
- 5. Boulton AJ, Vileikyte L, Ragnarson Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005;366:1719–24. [DOI] [PubMed] [Google Scholar]
- 6. Ramsey SD, Newton K, Blough D, McCulloch DK, Sandhu N, Reiber GE, Wagner EH. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care 1999;22:382–7. [DOI] [PubMed] [Google Scholar]
- 7. Apelqvist J, Armstrong DG, Lavery LA, Boulton AJM. Resource utilization and economic costs of care based on a randomized trial of vacuum‐assisted closure therapy in the treatment of diabetic foot wounds. Am J Surg 2008;195:782–8. [DOI] [PubMed] [Google Scholar]
- 8. Ragnarson Tennvall G, Apelqvist J. Health related quality of life in patients with diabetes mellitus and foot ulcers. J Diabetes Complications 2000;14:235–41. [DOI] [PubMed] [Google Scholar]
- 9. Banwell P. V.A.C. Therapy clinical guidelines: a reference source for clinicians (International). Produced by Medical Education Partnership (MEP) Ltd on behalf of KCI Europe Holding BV. London, 2007. ISBN 978‐90‐78026‐01‐3. [Google Scholar]
- 10. Blume PA, Walters J, Payne W, Ayala J, Lantis J. Comparison of negative pressure wound therapy using vacuum‐assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers. Diabetes Care 2008;31:631–6. [DOI] [PubMed] [Google Scholar]
- 11. Armstrong DG, Lavery LA. Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomised controlled trial. Lancet 2005;366:1704–10. [DOI] [PubMed] [Google Scholar]
- 12. McCallon SK, Knight CA, Valiulus JP, Cunningham MW, McCulloch JM, Farinas LP. Vacuum‐assisted closure versus saline‐moistened gauze in the healing of postoperative diabetic foot wounds. Ostomy Wound Manage 2000;46:28–34. [PubMed] [Google Scholar]
- 13. Philbeck T, Schroeder W, Whittington KT. Vacuum‐assisted closure therapy for diabetic foot ulcers: clinical and cost analyses. Home Health Care Consultant 2001;8:27–32. [Google Scholar]
- 14. Schwien T, Gilbert J, Lang C. Pressure ulcer prevalence and the role of negative pressure wound therapy in home health quality outcomes. Ostomy Wound Manage 2005;51:47–60. [PubMed] [Google Scholar]
- 15. Frykberg RG, Williams DV. Negative‐pressure wound therapy and diabetic foot amputations: a retrospective study of payer claims data. J Am Podiatr Med Assoc 2007;97:351–9. [DOI] [PubMed] [Google Scholar]
- 16. Kaplan M. Negative pressure wound therapy in the management of abdominal compartment syndrome. Ostomy Wound Manage 2004;50(11A Suppl):20S–25S. [PubMed] [Google Scholar]
- 17. Niezgoda JA. The economic value of negative pressure wound therapy. Ostomy Wound Manage 2005;51(2A Suppl):44S–47S. [PubMed] [Google Scholar]
- 18. Kaplan M, Daly D, Stemkowski S. Early intervention of negative pressure wound therapy using Vacuum‐Assisted Closure in trauma patients: impact on hospital length of stay and cost. Adv Skin Wound Care 2009;22:128–32. [DOI] [PubMed] [Google Scholar]
- 19. De Leon JM, Barnes S, Nagel M, Fudge M, Lucius A, Garcia B. Cost‐effectiveness of negative pressure wound therapy for postsurgical patients in long‐term acute care. Adv Skin Wound Care 2009;22:122–7. [DOI] [PubMed] [Google Scholar]
- 20. Flack S, Apelqvist J, Keith M, Trueman P, Williams D. An economic evaluation of VAC therapy compared with wound dressings in the treatment of diabetic foot ulcers. J Wound Care 2008;17:71–8. [DOI] [PubMed] [Google Scholar]
- 21. Le Franc B, Sellal O, Grimandi G, Duteille F. Cost‐effectiveness analysis of vacuum‐assisted closure in the surgical wound bed preparation of soft tissue injuries. Ann Chir Plast Esthet 2010;55: 195–203. [DOI] [PubMed] [Google Scholar]
- 22. Lavery LA, Boulton AJ, Niezgoda JA, Sheehan P. A comparison of diabetic foot ulcer outcomes using negative pressure wound therapy versus historical standard of care. Int Wound J 2007;4:103–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Apelqvist J, Ragnarson Tennvall G, Larrson J, Persson U. Long‐term costs for foot ulcers in diabetic patients in a multidisciplinary setting. Foot Ankle Int 1995;16:388–94. [DOI] [PubMed] [Google Scholar]
- 24. Persson J, Willis M, Odegaard K, Apelqvist J. The cost‐effectiveness of treating diabetic lower extremity ulcers with becaplermin (Regranax): a core model with an application using Swedish cost data. Value Health 2000;3:39–46. [DOI] [PubMed] [Google Scholar]
- 25. Briggs A, Claxton K, Sculpher M. Decision modelling for health economic evaluation. Oxford: Oxford University Press, 2006. [Google Scholar]
- 26. Ragnarson Tennvall G, Apelqvist J, Eneroth M. Costs of deep foot infections in patients with diabetes mellitus. Pharmacoeconomics 2000;18:225–38. [DOI] [PubMed] [Google Scholar]
- 27. Apligraf Medicare product and related procedure reimbursement. www.apligraf.com/PDF?AplHotSheet_06_3qrt.pdf.7‐1‐2006. [database on the Internet] 2006 [accessed on 27 July 2006].
- 28. Redekop WK, Stolk EA, Kok E, Lovas K, Kalo Z, Busschbach JJ. Diabetic foot ulcers and amputations: estimates of health utility for use in cost‐effectiveness analyses of new treatments. Diabetes Metab 2004;30:549–56. [DOI] [PubMed] [Google Scholar]
- 29. Assurance Maladie en Ligne. Liste des Produits et Prestations Remboursables [database on the Internet] 2009. Version from 24 March. Available at: http://www.ameli.fr/professionnels‐de‐sante/gestionnaires‐de‐centres‐de‐sante/exercer‐au‐quotidien/liste‐des‐produits‐et‐prestations‐lpp/index.php.
- 30. Assurance Maladie en Ligne. Classification Commune des Actes Médicaux. [database on the Internet] 2009. Available at: http://www.ameli.fr/accueil‐de‐la‐ccam/index.php.
- 31. AMeli. Assurance Maladie en Ligne. Table Nationale de codage de Biologie. 2009.
- 32. Agence Technique de Information sur Hospitalisation. Echelle nationale de coûts. Echelle et coûts décomposés 2003‐2004 [database on the Internet] 2007. Available at: http://www.atih.sante.fr/?id=000370000AFF.
- 33. Chambaud L, Khennouf M, Lannelongue C, Mordelet P, Dusehu E, Geffroy L. Enquête sur la rémunération des médecins et chirurgiens hospitaliers. Inspection générale des affaires sociales 2009.
- 34. Infirmiers.com. La communauté infirmière. Comment lire votre fiche de paye? 2009.
- 35. Editions du Vidal. Le dictionnaire Vidal 2008. 84th ed. 2008. UBM Medica. ISBN 978‐2‐85091‐169‐9
- 36. Assurance Maladie en Ligne. Liste des groupes génériques soumis au TFR (actualisée au 1er mars 2009) [database on the Internet] 2009.
- 37. Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, Edmonds M, Holstein P, Jirkovska A, Mauricio D, Tennvall GR, Reike H, Spraul M, Uccioli L, Urbancic V, Van Acker K, Van Baal J, Van Merode F, Schaper N. Delivery of care to diabetic patients with foot ulcers in daily practice: results of the Eurodiale Study, a prospective cohort study. Diabet Med 2008;25:700–7. [DOI] [PubMed] [Google Scholar]
- 38. Richard J, Parer‐Richard C. Le pied diabétique: données épidémiologiques et économiques. In: Richard JL, Vannereau D, editors. Le pied diabétique. Paris: Editions MF, 2002:23–43. [Google Scholar]
- 39. Ubbink DT, Westerbos SJ, Nelson EA, Vermeulen H. A systematic review of topical negative pressure therapy for acute and chronic wounds. Br J Surg 2008;95:685–92. [DOI] [PubMed] [Google Scholar]
- 40. Hunter JE, Teot L, Horch R, Banwell PE. Evidence‐based medicine: vacuum‐assisted closure in wound care management. Int Wound J 2007;4:256–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. European Wound Management Association (EWMA). Position Document: Topical negative pressure in wound management. London: MEP Ltd, 2007. [Google Scholar]
- 42. World Union of Wound Healing Societies (WUWHS). Principles of best practice: vacuum assisted closure: recommendations for use. A concensus document. London: MEP Ltd, 2008. [Google Scholar]


