Abstract
In these uncertain times of high health care costs, clinicians are looking for cost‐effective devices to employ in their everyday practices. In an effort to promote cost‐effective and proper wound repair, the hydrosurgical device allows accurate debridement of only unwanted tissue while precisely conserving viable structures for eventual repair. This prospective, randomised study compared procedures using the hydrosurgery system (VERSAJET™) with conventional debridement in order to assess clinical efficacy and cost‐effectiveness when treating subjects with chronic wounds. A total of 40 subjects were recruited. There was no difference in time to achieve stable wound closure between the treatment groups (P = 0·77). There were no significant differences between the two groups in terms of cost of the first operative procedure (P = 0·28), cost of surgical procedures during the study (P = 0·51), cost of study treatment (P = 0·29) or cost to achieve stable wound closure (P = 0·85). There were no differences in quantitative bacterial counts after debridement with either methods (P = 0·376). However, the time taken for the first excision procedure was significantly faster using the hydrosurgery system (VERSAJET) when compared with conventional debridement (P < 0·001). The total excision time for all procedures was significantly less for the Hydrosurgery group than for the conventional group (P = 0·005). Also, the Hydrosurgery group demonstrated significantly less intraoperative blood loss than conventional group for all procedures (P = 0·003). In this study, although there were no differences in time to stable wound closure or bacterial reduction between the two groups, the hydrosurgery system (VERSAJET) did offer advantages in terms of operative times and intraoperative blood loss and was cost‐neutral, despite the handpiece cost.
Keywords: Chronic wound, Clinical efficacy, Debridement, Hydrosurgery, Versajet
Introduction
Delayed healing wounds impact many people, causing morbidity, interference with quality of life, hardship for the subjects and economic strain on the health care system 1. In the fiscal year of 2004, there were more than 57 000 discharges under DRG code 217 (wound debridement and skin graft except hand, for musculoskeletal and connective tissue disease) in the USA 2. Mean length of stay (all payers) was 11 days and mean charges were $52 800. In 2005, Medicare funded 15 800 discharges under this code. Average charges for these subjects were $56 500 and average reimbursement was $18 265 3.
An essential component of the effective treatment of delayed healing wounds is the debridement of devitalised, bacterially contaminated or senescent tissue 4. Necrotic tissue excision, removal of bacterial burden and elimination of potential biofilm and senescent cells are all encompassed in debridement 5. Debridement of the chronic wound transforms the environment to onedressingseveryday of an acute wound 6. This creates an optimal environment in the wound bed, which facilitates the natural progression of wound healing 5. Sharp, or surgical, debridement is currently considered the gold standard for removal of necrotic tissue 6. A disadvantage of this approach is the removal of viable tissue with the excised necrotic tissue 7. This hinders the natural wound healing process, as viable tissue promotes revascularisation and delivery of growth factors 8.
In an effort to promote proper wound repair, the hydrosurgery system (VERSAJET™) has established a novel approach to wound management. It allows accurate debridement of only unwanted tissue, while precisely conserving viable structures for eventual repair 9. It employs a high‐pressure water jet at 15 000 psi to create a Venturi effect, which eliminates debrided tissues in the water stream, extricating it from the underlying tissue 8.
Methods
Study design
This prospective, open, randomised controlled, single‐centre clinical trial was designed to investigate the difference in time to closure of delayed healing dehisced incisions, delayed healing traumatic wounds or chronic cutaneous defects between those surgically excised with hydrosurgery system and those surgically excised using conventional surgical techniques. This study also looked at other relevant points such as the difference in time of actual excision procedure, cost per operative procedure, cost of reference wound‐related surgical procedures to achieve closure, quantitative bacteriology from standardised tissue biopsies and % of wounds clinically infected after first excision between the two methods of surgical excision. The study protocol received approval from the Institutional Review Boards at Northwestern University (project number STU0020035). All subjects gave written informed consent prior to participation.
Inclusion and exclusion criteria
Eligibility criteria included: age 18 years or older, with a delayed healing traumatic wound or chronic cutaneous defect of 30 days or more in duration, or a delayed healing dehisced incision that required excision, and deemed to require closure by primary intention or definitive cover with an autologous split‐thickness skin graft or flap; subjects who are hospital in‐subjects or will be an in‐subject for the period of first excision to closure; subjects deemed suitable for debridement with both hydrosurgery system and conventional surgical techniques; subjects undergoing surgical excision of their reference wound in the operating room and subjects able to understand the evaluation and willing to consent to the evaluation. Subjects were excluded if they met any of the following criteria: (i) subjects who had previously undergone surgical excision of the reference wound by the principal investigator in the last 30 days; (ii) subjects with coagulopathy (including those with haemophilia); (iii) subjects with vasculitis, non‐reconstructive peripheral vascular disease, pyoderma granulosa, renal failure or lymphoedema; (iv) subjects with irradiated, burn or ischaemic wounds; (v) subjects with a body mass index ≥35; (vii) subjects require a staged procedure, with hospital discharge occurring between the procedures; (vii) subjects require biological dressings or skin substitutes; (viii) subjects for whom wound healing by secondary intention was deemed necessary; (ix) subjects who had been treated with systemic immunosuppressants (including corticosteroids) or cytotoxic chemotherapy in the last 30 days, or who were anticipated to require such medications during the course of the study; (x) subjects known to have acquired immunodeficiency syndrome or known to be infected with human immunodeficiency virus; (xi) subjects with a known history of poor compliance with medical treatment and (xii) subjects who had participated in this evaluation previously or who were currently participating in another clinical study.
Randomisation and device regimens
All subjects who met the selection criteria and consented to participate in the evaluation were randomised to the treatment group (excision with hydrosurgery system) or control group (excision with conventional surgical techniques).
Figure 1 details the assessment points and data recorded in this evaluation.
Figure 1.
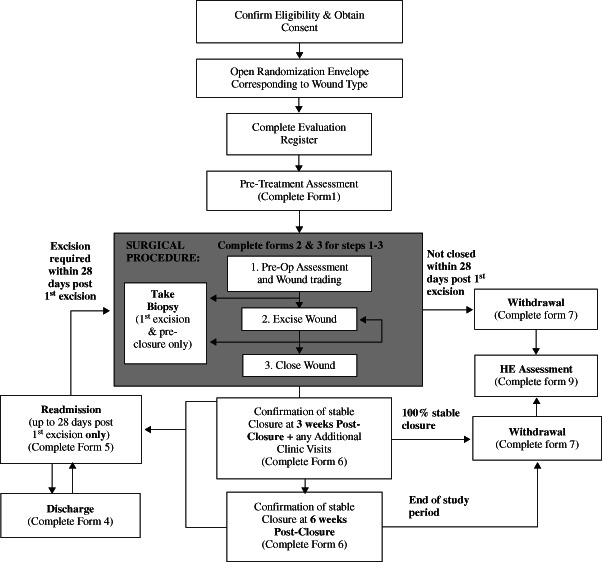
Assessment points and data.
Results
Forty evaluable subjects were recruited for the primary investigation of the effect of hydrosurgery system versus conventional debridement on the time to closure of delayed healing dehisced incisions and traumatic or chronic cutaneous defects. Of these, 21 subjects were in the Hydrosurgery group and 19 were in the Conventional group. The first subject was recruited on 21 November 2007 and the last subject completed the study on 19 September 2011. Subject demographics were well balanced between the treatment groups (see Table 1).
Table 1.
Subject demographics
| Hydrosurgery (n = 21) | Conventional (n = 19) | Total (n = 40) | |
|---|---|---|---|
| Age (years) | |||
| Mean | 52·2 | 57·1 | 54·5 |
| Median | 53 | 58 | 55·5 |
| Gender | |||
| Male | 16 (76·2%) | 10 (52·6%) | 26 (65%) |
| Female | 5 (23·8%) | 9 (47·4%) | 14 (35%) |
| Height (cm) | |||
| Mean | 171·4 | 172·2 | 171·8 |
| Median | 170·2 | 170·2 | 170·2 |
| Weight (lbs) | |||
| Mean | 176·4 | 165·3 | 171·2 |
| Median | 180 | 170 | 175 |
| ABI | |||
| Mean | 1·1 | 1·0 | 1·1 |
| Median | 1 | 1·1 | 1 |
ABI, ankle‐brachial index.
Six subjects (15%) had delayed healing dehisced incisions [4 (19%) Hydrosurgery versus 2 (10·5%) Conventional group subjects]. One subject (4·8%) had a delayed healing traumatic wound (1 Hydrosurgery subject) and 33 subjects (82·5%) had chronic cutaneous defects [16 (76·2%) Hydrosurgery versus 17 (89·5%) Conventional group subjects].
The reference wound dimensions (area and depth) and percentage of devitalised tissue were well balanced (Table 2). Reference wound type, duration, exposure of bone and tendon and exudate level were also well balanced between the treatment groups. The most frequently occurring wound was pressure ulcers with 19 (47·5%) wounds, followed by dehisced surgical incisions and diabetic foot ulcers, both with 6 (15%) wounds each.
Table 2.
Wound dimensions and area of devitalised tissue
| Hydrosurgery | Conventional | Total | |
|---|---|---|---|
| Reference wound area (cm2) | |||
| Mean | 15·6 | 19·6 | 17·4 |
| Median | 15·4 | 14·5 | 15·4 |
| Reference wound depth (mm) | |||
| Mean | 20 | 20 | 20 |
| Median | 11 | 8 | 10·5 |
| Devitalised tissue (%) | |||
| Mean | 50·4 | 50·8 | 50·6 |
| Median | 45 | 50 | 47·5 |
| Area of devitalised tissue (cm2) | |||
| Mean | 7·3 | 10·4 | 8·7 |
| Median | 5·2 | 6·2 | 5·4 |
Nine (42·9%) subjects in the Hydrosurgery group achieved stable wound closure during the study period compared with seven (26·8%) in the Conventional group. There was no difference in time to achieve stable wound closure between the treatment groups (P = 0·77).
A Kaplan–Meier plot of the probability of achieving stable wound closure against time is displayed in Figure 2. This illustrates the similarity in the time to achieve stable wound closure between the treatment groups, with the observed probability of achieving stable wound closure during the study period being slightly greater for the Hydrosurgery group than for the Conventional group. The median total length of hospital stay was 39 days for the Hydrosurgery group and 38 days for the Conventional group.
Figure 2.
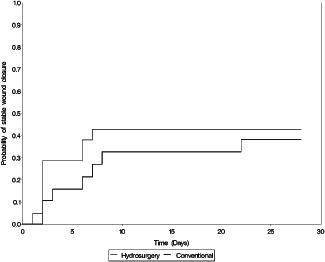
Kaplan–Meier plot of probability of achieving stable wound closure.
The mean cost of the first operative procedure was $4411·70 for the Hydrosurgery group and $6014·10 for the Conventional group subjects (P = 0·278). There was no significant difference in the mean cost of the surgical procedures for Hydrosurgery group ($13689·1) compared with the Conventional group ($12869·4) (P = 0·513). The mean cost of study treatment (surgical procedures + hospital stay) was $44290·1 for the Hydrosurgery group and $39940·5 for the Conventional group subjects (P = 0·287). There was no evidence (P = 0·851) of a difference in the cost to achieve stable wound closure between the treatments. The estimate for the ratio of the cost to achieve stable wound closure, Hydrosurgery : Conventional, was 0·851.
The median log10 total bacterial count pre‐first excision was 4·0 cfu/g for both the Hydrosurgery and the Conventional groups of subjects, and the median log10 total bacterial count post‐first excision was 3·2 and 3·3 cfu/g for the Hydrosurgery and the Conventional groups, respectively. This represents a median difference in the reduction in the total log10 bacterial count between the Hydrosurgery and the Conventional groups of 0·1 cfu/g, a difference that was not statistically significant (P = 0·376) (see Figure 3).
Figure 3.
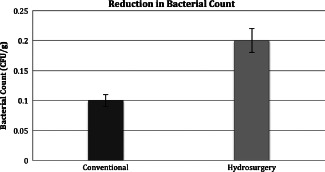
Reduction in bacterial count (P > 0·05).
The mean time for the first excision procedure was 7·3 minutes for the Hydrosurgery group subjects and 16·3 minutes for the Conventional group subjects (P < 0·001) (see Figure 4). The mean total excision time for overall excision procedure was 14·2 minutes for the Hydrosurgery group and 33·9 minutes for the Conventional group; this difference was statistically significant (P = 0·033) (see Figure 5).
Figure 4.
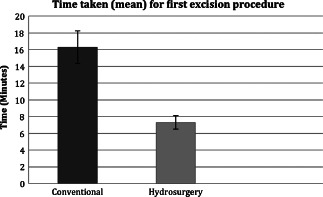
Mean time for the first excision procedure (P < 0·001).
Figure 5.
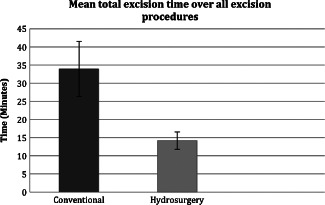
Mean total excision time over all excision procedures (P = 0·033).
There was significant evidence (P = 0·003) that the maximum blood loss for overall excision procedures was less for the Hydrosurgery group subjects than for the Conventional group subjects (see Figure 6). Similarly, it was observed that there was less blood loss for Hydrosurgery group during the first excision procedure than for the Conventional group (see Figure 6).
Figure 6.
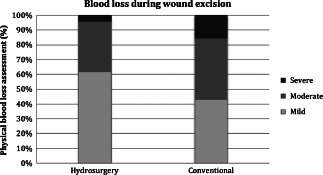
Physician assessment (%) with regard to blood loss during all excision procedures (P = 0·003).
No safety concerns were raised about the use of hydrosurgery system to surgically excise dehisced incisions, delayed healing traumatic wounds or chronic cutaneous defects.
Discussion
The purpose of this study was to investigate the difference in time to closure of wounds surgically excised with hydrosurgery system (VERSAJET) and those surgically excised using conventional surgical techniques. In addition, quantitative bacteriology, cost per operating procedure and procedure time were investigated. Regarding the impact on bacterial load, previous research found that the use of hydrosurgery system (VERSAJET) promoted a more efficient debridement, leading to decreased postoperative wound infections and increased success with the take rate of skin grafts. These findings suggest a potential correlation between the use of the hydrosurgery system (VERSAJET) and a reduction in postoperative bacterial count 10. However, our study found no significant differences between hydrosurgical system (VERSAJET) and conventional surgical debridement techniques when examining stable wound closure or bacterial reduction. It is possible that bacterial fallout associated with hydrosurgery affected the results, and careful consideration must be taken to reduce perioperative bacterial contamination in future trials 11.
Contrary to our findings, previous research supports the cost‐effectiveness of the hydrosurgery system (VERSAJET). These studies make several assertions. First, hydrosurgery system (VERSAJET) reduced the number of necessary debridement procedures as well as the number of postoperative complications 12. Minimising the number of surgical procedures needed to achieve optimal wound environment may result in an overall estimated savings of $1900 per patient for the cost of debridement 13. Second, debridement time can be reduced by nearly 40%, which may lead to savings in operating time and thus, more patients can be scheduled for operating sessions 14. Third, decreased use of pulse lavage may garner additional savings because a separate irrigation procedure is not necessary for the hydrosurgery system (VERSAJET) 14. Finally, the hydrosurgical approach minimised hospitalisation and healing time, resulting in total savings despite the high monetary expense of the disposable handpiece 14.
These studies, however, fail to consider medical billing policies in assessing cost‐effectiveness. The cost of operating room labour largely depends on whether the staff is hourly or salaried 15. If the operating room staff is paid a salary regardless of when the procedure is completed, then the patient would experience no cost‐benefits if debridement time is reduced by several minutes. In the case of hourly labour costs, it is also possible that a patient may be billed for a full hour of operative time even if the procedure takes less than an hour to complete. Additionally, it is difficult to assess whether shortened debridement time would increase daily scheduled sessions. Doing so would require documentation that decreased debridement time made it possible to treat an additional patient in a session that was originally scheduled for only one patient. In addition, the hydrosurgery (VERSAJET) console can be considered a capital item, so its overall value in cost‐effectiveness will depend on the number of surgeries each surgeon performs 14. The cost per procedure may increase if the console is under‐used 9.
In our pilot study, we compared the hydrosurgery system to the conventional surgical debridement techniques and found no significant differences when examining stable wound closure, bacterial reduction or procedural expenses. Future research sampling a larger population is required in order to demonstrate the efficacy and cost‐effectiveness of the treatment. In addition, this is a single‐centre study and creating a multicentre study would yield more reliable results in prospective studies. Polymerase chain reaction can be utilised in forthcoming research in order to test the impact of hydrosurgery on bacterial burden in the wound.
Regarding the health economics of this study, prior experiences will provide more insight into data collection as well as potential issues of capturing economic data for this type of study. A questionnaire designed to collect feedback from the surgeons who are using the hydrosurgery debridement method will be valuable suggestion.
Conclusion
There were no differences in time to stable wound closure or bacterial reduction between hydrosurgery and conventional debridement. The hydrosurgery system (VERSAJET) did offer advantages in terms of operative times and intraoperative blood loss, and was cost‐neutral, despite the handpiece cost.
Acknowledgments
No member of the research team, writers or editors has any conflict of interests, financial or intellectual, in any form, with this publication and/or study. This study was funded by Smith and Nephew Inc.
References
- 1. Fonder MA, Lazarus GS, Cowan DA, Aronson‐Cook B, Kohli AR, Mamelak AJ. Treating the chronic wound: a practical approach to the care of nonhealing wounds and wound care dressings. J Am Acad Dermatol 2008;58:185–206. [DOI] [PubMed] [Google Scholar]
- 2.Healthcare Cost & Utilization Project (HCUP) Agency for Healthcare Research and Quality. 2004 National Statistics. URL http://www.ahrq.gov/data/hcup/ [accessed on 11 January 2012]
- 3.Centers for Medicare and Medicaid Services (CMS) MEDPAR inpatient hospital national data for fiscal year 2005.
- 4. Steed DL, Donohoe D, Webster MW, Lindsley L. Effect of extensive debridement and treatment on the healing of diabetic foot ulcers. J Am Coll Surg 1996;183:61–4. [PubMed] [Google Scholar]
- 5. Falanga V. The chronic wound: impaired healing and solutions in the context of wound bed preparation. Blood Cells Mol Dis 2004;32:88–94. [DOI] [PubMed] [Google Scholar]
- 6. Nusbaum AG, Gil J, Rippy MK, Warne B, Valdes J, Claro A, Davis SC. Effective method to remove wound bacteria: comparison of various debridement modalities in an in vivo porcine model. J Surg Res 2012;176:701–7. URL [http://www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/DRG05.pdf] [DOI] [PubMed] [Google Scholar]
- 7. Panuncialman J, Falanga V. The science of wound bed preparation. Surg Clin North Am 2009;89:611–26. [DOI] [PubMed] [Google Scholar]
- 8. Cornell RS, Meyr AJ, Steinberg JS, Attinger CE. Débridement of the noninfected wound. J Vasc Surg 2010;52(3 Suppl):31S–6S. [DOI] [PubMed] [Google Scholar]
- 9. Sainsbury DCG. Evaluation of the quality and cost‐effectiveness of VersajetÒ hydrosurgery. Int Wound J 2009;6:24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gurunluoglu R. Experience with waterjet hydrosurgery system in wound debridement. World J Emerg Surg 2007;2:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bowling FL, Stickings DS, Edwards‐Jones V, Armstrong DG, Boulton AJM. Hydrodebridement of wounds: effectiveness in reducing wound bacterial contamination and potential for air bacterial contamination. J Foot Ankle Res. 2009;2:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Granick M, Boykin J, Gamelli R, Schultz G, Tenenhaus M. Toward a common language: surgical wound bed preparation and debridement. Wound Repair Regen 2006;14(Suppl 1):S1–10. [DOI] [PubMed] [Google Scholar]
- 13. Granick MS, Posnett J, Jacoby M, Noruthun S, Ganchi PA, Datiashvili RO. Efficacy and cost‐ effectiveness of a high‐powered parallel waterjet for wound debridement. Wound Repair Regen 2006;14:394–7. [DOI] [PubMed] [Google Scholar]
- 14. Caputo WJ, Beggs DJ, DeFede JL, Simm L, Dharma H. A prospective randomised controlled clinical trial comparing hydrosurgery debridement with conventional surgical debridement in lower extremity ulcers. Int Wound J 2008;5:288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Macario A. What does one minute of operating room time cost? J Clin Anesth 2010;22:233–6. [DOI] [PubMed] [Google Scholar]


