INTRODUCTION
Diabetes is a complex multi‐system disease (1). The World Health Organization projects diabetes to increase from 171 million in 2000 to 366 million in 2030 with most increases occurring in Third‐World countries and Aboriginal populations (2). In Canada, in 2008/2009, 200 000 new cases of diabetes were diagnosed; 47.5% of these individuals were obese (3). The correlation of diabetes to obesity is significant, and there is a direct relationship between dietary and lifestyle choices, food intake and activity levels with rates of diabetes 3, 4. With these increasing rates we need to be prepared to support persons with diabetes with prevention strategies and self‐management support.
In Canada, Type 1 and Type 2 diabetes rates are dramatically increasing in direct proportion to obesity rates and the aging population (3). In 2003, the Institute for Clinical Evaluative Sciences reported that 2 million Canadians have diabetes with a yearly estimated cost of $9 billion annually (5). The Public Health Agency of Canada (PHAC) (3) reports an even higher rate of diabetes at 2.4 million of the 34 million Canadians (6).
COMPLICATIONS
Diabetes affects most organs and circulatory systems, yet, the majority of Type 2 diabetes is preventable. Persons with Type 1 and Type 2 diabetes are at risk of developing long‐term foot complications, ulcers and amputations. Complications of diabetes cost the Canadian health care system millions of dollars each year and persons living with diabetes use health care services 2.4 times more than the general population (7). Complications of diabetes include: blindness, end‐stage renal disease, cardiovascular disease and heart attack, and neuropathy. Vascular complications lead to superficial and deep infections, non healing ulcerations of the feet, and amputation(s) of the lower or upper limb 1, 8. With each new case of diabetes we have an increase in complication rates, ulcerations, infections and amputations.
CHRONIC CARE DISEASE MODEL
There is growing recognition that all aspects of diabetes prevention and management, including foot complications, need to be taken into consideration, not only biological factors, but also the psychological and social components. These complex factors must be considered when working with patients and their families.
The Public Health Agency of Canada (PHAC) is aware of the growing need for agencies to adopt and utilise the Chronic Care Disease Model in the development, implementation and evaluation of health care delivery services and programmes to all persons living with chronic diseases including diabetes.
The Chronic Care Disease Model (CCDM) has been ‘proposed as a multitasked, interdependent framework to improve health care delivery’ through the interplay between the healthcare system and the community (10) (Figure 1). One of the core elements of this model is self‐management support, with the goal of empowering patients, families and communities to become involved, informed and active in their care. The PHAC, under the Canadian Diabetes Strategy, is working in partnership with Canadian Association of Wound Care (CAWC) to develop self‐management interactive educational tools (Phase 1), and a Peer‐Led educational programme to encourage self‐management and to empower persons with diabetes to adopt healthy, daily, foot care practices (Phase 2).
Figure 1.
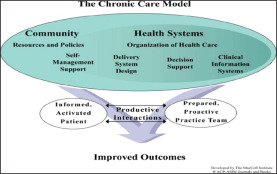
The chronic care model.
Phase 1 –Diabetes, Healthy Feet and You
In 2010 CAWC in partnership with the Public Health Agency of Canada launched the Diabetes, Healthy Feet and You educational and interactive programme and website for persons living with diabetes. The diabetes educational tools can be found online at: http://www.cawc.net/diabetesandhealthyfeet. Brochures for persons with diabetes have been translated into as many as 16 languages.
Phase 2 –PEP Talk: Diabetes, Healthy Feet and You
The Diabetes, Healthy Feet and You initiative has been extended into Phase 2. This phase includes implementation of a Peer Leader educational programme that empowers persons living with diabetes to know and apply good foot care practices. The Peer Leader Education Program (PEP) workshops are called PEP Talk: Diabetes, Healthy Feet and You. The goal of the Peer‐Led workshops is to develop a network of community peer educators and motivate persons with diabetes to change how they care for their feet and potentially prevent foot ulcers. Peer Leaders from each province will facilitate workshops in partnership and with the support of health care professionals. The focus of the programme is to empower persons living with diabetes to ‘discover and use their own innate abilities to gain mastery of their diabetes' and foot care (11).
Peer‐led, self‐management programmes have been identified as having significant benefits to people with diabetes (12). The success of peer‐led programmes is attributed to having support from a person who has experienced the challenges of living with a similar condition, in this case diabetes and its complications. Persons living with diabetes and neuropathy have been identified as the best candidates to facilitate the PEP Talk: Diabetes, Healthy Feet and You workshop (13).
The CAWC educational programme team has used this knowledge to build PEP Talk: Diabetes, Healthy Feet and You programme to be led by volunteer Peer Leaders who live with diabetes and neuropathy; they co‐lead the workshops with volunteer healthcare professionals committed to improving the lives of persons with diabetes. The PEP Talk: Diabetes, Healthy Feet and You programme was developed to incorporate multiple educational strategies including presentations, cognitive strategies, behavioral activities and social interventions that include goal setting, problem solving, group activities and other motivational strategies (1).
The CAWC will continue to work with the Public Health Agency of Canada, Canadian healthcare professionals and persons with diabetes to evaluate the effectiveness of these workshops and increase awareness and knowledge about foot health and foot care with an ultimate goal of reducing the number of preventable foot ulcers and related limb amputations in persons with diabetes.
For more information about the upcoming PEP Talk: Diabetes, Healthy Feet and You– PEP Talk Peer Education Program workshops in your community, please contact Andrea Martin at andrea.martin@cawc.net.

Mariam Botros, M. Gail Woodbury, Janet Kuhnke and Marc Despatis
REFERENCES
- 1. Canadian Diabetes Association. Canadian Diabetes Association 2008 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Toronto: CDA, 2008. [Google Scholar]
- 2. World Health Organization. Media Center: Diabetes Fact Sheet N 312 [WWW document]. URL http://www.who.int/mediacentre/factsheets/fs312/en/ [accessed on 21 March 2012]
- 3. Public Health Agency of Canada (PHAC). Diabetes in Canada: facts and figures from a public health perspective [WWW document]. URL http://www.phac‐aspc.gc.ca/cd‐mc/publications/diabetes‐diabete/facts‐figures‐faits‐chiffres‐2011/chap4‐eng.php [accessed on 21 March 2012] [Google Scholar]
- 4. Canadian Diabetes Association. Foot care: a step toward good health [WWW document]. URL http://www.diabetes.ca/diabetes‐and‐you/living/complications/foot‐care/ [accessed on 21 March 2012]
- 5. Hux JE, Jacka R, Fung K, Rothwell DM. Diabetes and peripheral vascular disease. In: Diabetes in Ontario: An ICES Practice Atlas. Ontario: ICES. URL http://www.ices.on.ca/ [accessed on 21 March 2012] [Google Scholar]
- 6. Statistics Canada. CANSIM: estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual (persons) [WWW document]. URL http://estat.statcan.gc.ca/cgi‐win/CNSMCGI.EXE [accessed on 21 March 2012]
- 7. Canadian Institute for Health Information. Diabetes care gaps and disparities in Canada. Analysis in Brief. Ottawa: CIHI, 2009. [Google Scholar]
- 8. Canadian Association of Wound Care. Diabetes, Healthy Feet and You [WWW document]. URL http://cawc.net/en/index.php/public/feet/ [accessed on 21 March 2012]
- 9. Canadian Diabetes Association. Building competency in education: the essentials. Toronto: Canadian Diabetes Association, 2010. [Google Scholar]
- 10. Chronic Care Model [WWW document]. URL http://www.improvingchroniccare.org/ [accessed on 21 March 2012]
- 11. Funnell M. Patient empowerment. Crit Care Nurs Q, 2004;27:201–4. [DOI] [PubMed] [Google Scholar]
- 12. WHO. Peer support programs in diabetes. Report of the WHO consultations Nov 5‐7 2007[WWW document]. URLhttp://www.who.int/diabetes/publications/Diabetes_final_13_6.pdf [accessed on 29 March 2012]
- 13. Heisler M. Self management and clinical outcomes. Diabetes Spectr 2007;20:214–20. [Google Scholar]


