Abstract
Clinical experience with a new electrical stimulation (ES) technique, the wireless micro current stimulation (WMCS), for the treatment of chronic wounds is described. WMCS transfers the current to any surface wound from a distance, by using oxygen's and nitrogen's ability to exchange electrons. We studied 47 patients with hard‐to‐heal wounds. Patients with venous, arterial and mixed leg ulcers were predominant; other aetiologies such as diabetic foot lesions, pressure ulcers, vasculitis and pyoderma were also included. WMCS treatment protocol specified treatment twice or thrice per week, for 45–60 minutes per session, with 1·5 μA current intensity. Standard wound care was applied to all patients, including compression bandages, if necessary. Clear progress of wound healing, even after 2 weeks, was observed in all cases. The mean reduction of the wound surface after WMCS treatment was 95% in 8 weeks. Complete healing was achieved within 3 months for the majority of the cases. No clinical side effects were observed. WMCS technology significantly accelerated wound healing for patients with hard‐to‐heal wounds of different aetiologies. This new therapy offers multiple advantages compared with the previous methods of ES, as it is contactless, free of pain and very easy to use.
Keywords: Chronic wounds, Diabetic foot, Electrical stimulation, Leg ulcer, Wireless micro current stimulation
Introduction
Electrical stimulation (ES) is a well proven method for accelerating wound healing in the treatment of chronic wounds 1. Numerous studies show positive effects of ES at cellular and molecular level 2, 3, 4. Briefly, it increases blood flow and the oxygen content in the wounded tissues, promotes angiogenesis, stimulates the synthesis of collagen, activates the reepithelialisation by directed migration of keratinocytes and reduces oedema and pain 1, 2, 4, 5, 6, 7. A great number of clinical data confirms the benefits of ES in order to shorten the process of wound healing and reduce pain, especially in the case of hard‐to‐heal chronic wounds 5. In addition, ES is the only method for the treatment of chronic wounds, with the highest grade of evidence (level Ia) 8, 9, 10. Despite these facts, ES is not still widely known and, therefore, rarely used. A possible explanation for this apparent lack of popularity might be the fact that ES is used in many different ways and, therefore, is not standardised yet.
ES application for the treatment of wounds adopts the physiological fact that skin and corneal epithelia act as batteries and have electric potentials. When an injury/wound occurs in the epithelium, an electric leak occurs that short‐circuits the skin battery, allowing current to flow out of the wound, giving the ‘current of injury’. This change sends signals to the healing epithelial cells to migrate into the wound, initiating the body's own healing processes 1, 2. After the healing of the epithelial layer, no more current flow is detectable. As part of a wound healing disorder the current flow changes and may even subside completely. ES is applied as an external method to restart the wound‐healing process by mimicking the ‘current of injury’.
ES is traditionally performed by applying on the tissue pin or dressing electrodes connected by cables to a current‐generating device. In contrast, wireless micro current stimulation (WMCS) technology is an innovative, simple, non‐invasive, pain‐free method to transfer current wirelessly to the wound by using oxygen's and nitrogen's ability to donate electrons. The charged particles create a direct current (DC) of very low intensity. With no physical contact to the wound thanks to its spray effect, it offers a radical advantage compared with other currently used ES techniques 11, 12, 13, 14. The application of WMCS in medical cases has already been reported 11, 12, 13, 14. However, we here present its application in a relatively large number of patients for the first time and we suggest the potentially beneficial effect of its usage as a first‐line therapy for hard‐to‐heal wounds.
Materials and methods
The WMCS device (Wetling, Fredensborg, Denmark) was used in the therapies. It works by transferring distantly low‐intensity electric current to the patients. The patient has to be part of an electrical circuit and, for this reason, has to be connected with the device through a wrist strap wire as shown in Figure 1 (usually placed on the patient's intact skin, far away from the wound, e.g. in case of leg ulcers it is normally placed at the wrist joint) 11.
Figure 1.
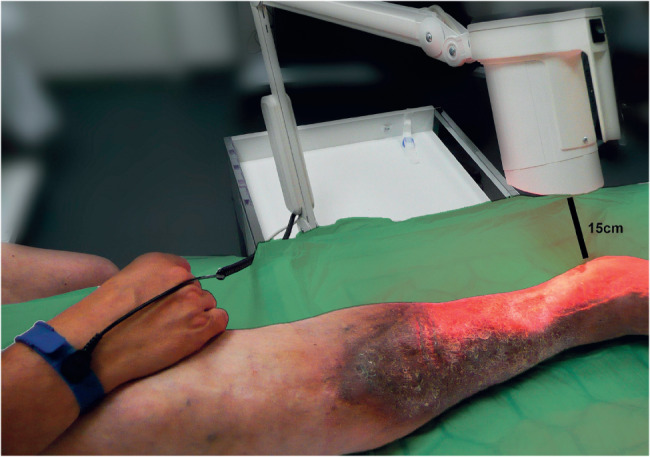
Instrumentation set‐up.
A control box permits the adjustment of the current (1·5–4·0 μA) and treatment duration. The intensity was set to 1·5 μA for all the therapies and the distance from the head of the device to any wound was 12–15 cm. The treatment surface covered is about 400 cm2, which can be increased by moving away the head of the device from the wound. If the head of the device is too far from the wound area for the transferred electric effect to reach the patient, there is a continuous warning tone. The charged particles create a DC of very low intensity.
Two wound centres, one in Aalen (Germany) and the second in Thun (Switzerland), developed this therapy and used the ‘treatment algorithm of chronic wounds with WMCS therapy’ as shown in Figure 2.
Figure 2.
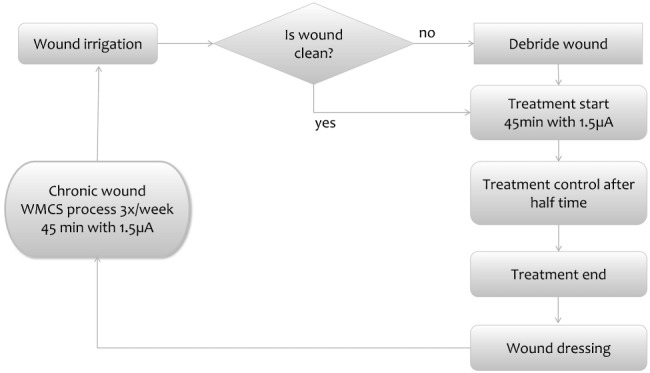
Treatment algorithm of chronic wounds with wireless micro current stimulation (WMCS) therapy.
The recommended treatment time is set to 45 minutes, so it is important that the patient lies or sits comfortably because the wound position relative to the WMCS device should remain steady throughout the treatment. All the participants were outpatients, were informed about the treatment and agreed to participate.
Before starting WMCS therapy, the wounds were examined and the wound cause was treated optimally. All principles of modern wound care or management were applied (pain management, examination of the skin surrounding the wound, taking a swab in case of infection and evaluating wound exudates). In both wound centres the WMCS therapy was combined with compression therapy in the case of venous leg ulcers, while in pressure ulcers it was combined with decompression as much as possible. Normally hydroactive wound dressings were used, including silver dressings; advanced wound therapeutics (growth factors, protease modulating matrix dressings, etc.) were avoided. All stages of wound healing were treated. Both appropriate cotreatment of the underlying diseases and sufficient pain therapy were deemed very important. In our experience, the only contraindication for WMCS was the presence of an acute inflammation or of a severely infected wound. Before starting WMCS therapy necrotic tissue was removed completely as well as fibrin or other coverings. Only patients with so called ‘hard‐to‐heal wounds’ were treated, which means that the wound existed for a long time and did not respond to standard wound treatment. Pictures of the wound were taken regularly with a digital camera and the wound area was measured in mm2 by using Synedra View 3® (Synedra Information Technologies GmbH, Innsbruck, Austria).
In both wound centres 47 patients were treated during the period of July 2011 to December 2012; patient age ranged 39–91 years (mean 72 years), and 22 were men and 25 women. These were patients with venous, arterial and mixed leg ulcers (28 patients), diabetic foot lesions (6 patients), pressure ulcers (3 patients), posttraumatic lesions (3 patients), decubitus (2 patients), pyoderma (2 patients), vasculitis (1 patient) and ulcer martorell (1 patient). The most common underlying diseases were diabetes mellitus, peripheral arterial disease, chronic venous insufficiency, coronary heart disease, hypertension and lymph oedema. The duration of the lesions before starting WMCS therapy was between 3 months and 11 years (median 10 months).
Check‐up of the patients was performed at the start, after 2 weeks (day 14–16), 4 weeks (day 28–35), 6 weeks (day 42–50), 8 weeks (day 56–60) and 12 weeks (day 84), sometimes even later. The mean duration of treatment was 45 days. The area of ulcers at the beginning of treatment was 50–4225 mm2 (mean 743 mm2, median 278 mm2).
All patients were treated by a specialised wound nurse; at least once a week the patients had a consultation with the respective physician. Sterile gauze was mainly used as wound dressing. In case of dressing changes after ≥2 days, hydroactive wound dressings were used.
Results
Findings
One to two weeks after WMCS therapy, a clear progression of wound healing was observed for all patients with the main observation being the restarting of wound healing with an extensive reduction of the wound area. In most cases, within 3 months or even less, complete healing could be achieved. Even in so‐called ‘non‐treatable patients’ a progression of the wound healing was shown when using the WMCS therapy. Severe side effects or complications did not appear during or after treatment; no burns or any other severe complication were reported by the patients. In very rare individual cases, a short, very smooth, burn filling was reported, but analgesics or other medications were never required. In these cases, a light redness of the tissue surrounding the wound was observed, which disappeared within a few hours.
In the first two (female) patients in Aalen Wound Centre, the WMCS therapy was terminated after three and six sessions, respectively, as the preexisting intense infection of the long‐standing and very painful leg ulcers did not improve and the patients refused further treatment. In Thun Wound Centre, in one case the WMCS therapy was not successful also due to a severe wound infection; in three very old patients no improvement was observed because of a fixed fibrin layer which was covering the wound completely and could not be removed without surgery.
In all other cases an essential improvement of the arterial blood flow could be seen independent of the cause of ulcer; the same was also observed in patients with a severe arterial occlusive disease or a diabetic microangiopathy and/or macroangiopathy. In addition, a clear reduction of bacterial burden was observed, even after just a few days of treatment. After only one session of treatment a contraction of the wound edge was observed. High rates of treatment (three times a week) resulted in a proportionally faster improvement of the wound situation and an earlier success was achieved. Patients who complained about wound pain during the change of the dressings prior to using WMCS, could bear the WMCS therapy and the following dressing changes without any pain. This shows that WMCS therapy reduces wound pain substantially.
The analysis performed by using digital wound area measurement of all patients before starting WMCS therapy showed an average area reduction of 17·1 ± 19·4% per month. After WMCS therapy, the monthly wound area reduction was 41·1 ± 27·3% (P = 0·0215). When cases with a clinical benefit were analysed, the corresponding values were 17·6 ± 20·3% and 55·7 ± 16·9% (P = 0·0071, Figure 3). It is observed that the WMCS therapy caused a threefold acceleration of the wound healing process. The mean reduction of the wound area after 8 weeks of treatment with WMCS was 95% (Figure 4).
Figure 3.
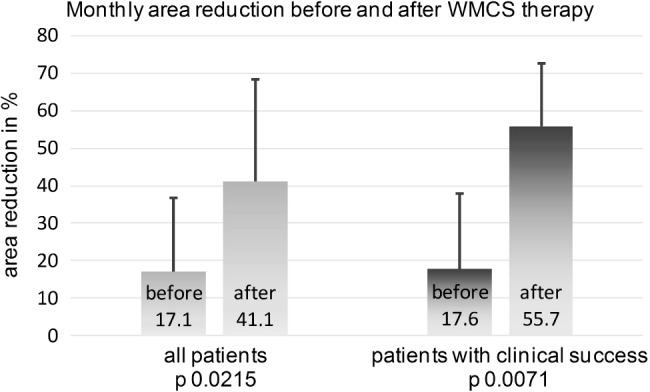
Monthly area reduction in percent before and after wireless micro current stimulation (WMCS) therapy.
Figure 4.
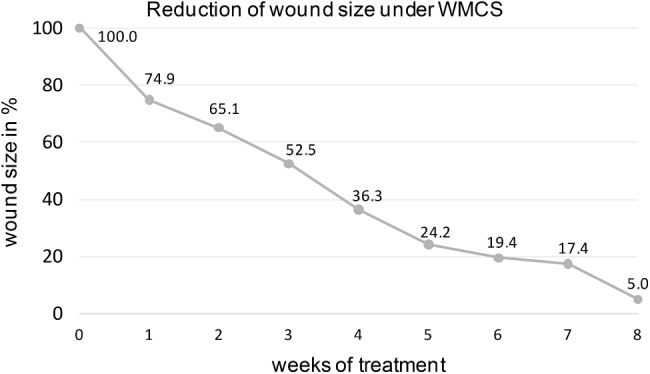
Reduction of wound size (%) in all patients under wireless micro current stimulation (WMCS).
Case Studies
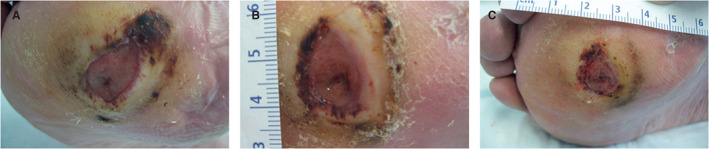
Patient 1: male, 84 years, peripheral artery disease stage IV
A vascular patient with no prospect for arterial reconstruction or interventional procedure to improve the arterial blood flow. Accompanying diseases, such as anaemia, hyperuricaemia, renal failure stage III and chronic venous insufficiency, were treated optimally. Modern wound dressings had been used for long time without improving the wound situation. There was no alternative for the treatment of the leg ulcer, which appeared 15 months ago (Figures 5 and 6).
Figure 5.

Wound at (A) treatment start (875 mm2), (B) after 4 weeks (630 mm2) and (C) after 10 weeks (251 mm2).
Figure 6.
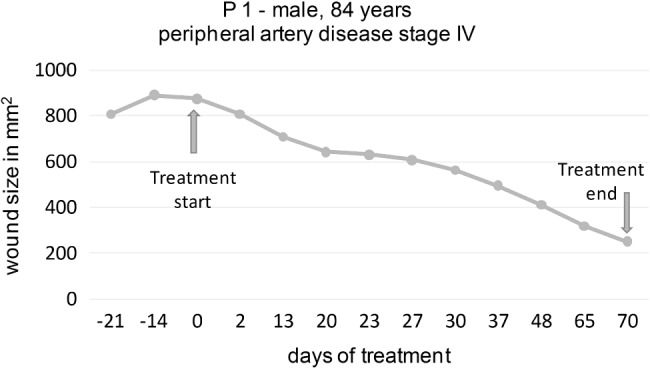
Reduction of wound size (mm2) under wireless micro current stimulation (WMCS) in patient 1.
Patient 2, male, 74 years, diabetic foot
A diabetic foot patient with an increasing pressure ulcer plantar at the forefoot, accompanied by an extreme deformation of the right foot (club foot or talipes equinovarus), adjusted however by using insoles. It was not possible to achieve a sufficient decompression. Accompanying diseases, such as diabetes mellitus and a severe arterial occlusive disease, were treated optimally (Figures 7 and 8).
Figure 7.
Wound at (A) treatment start (164 mm2), (B) after 6 weeks (140 mm2) and (C) after 16 weeks (120 mm2).
Figure 8.
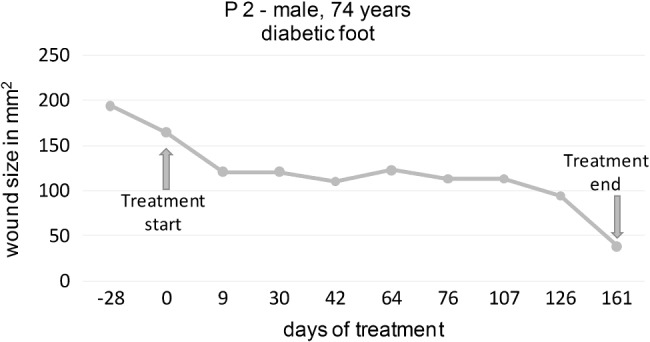
Reduction of wound size (mm2) under wireless micro current stimulation (WMCS) in patient 2.
Patient 3, female, 86 years, venous leg ulcer
A patient with a hard‐to‐heal ulcer of the right lower leg persisting for 7 months owing to a severe post thrombotic syndrome. No diabetes or peripheral artery disease was diagnosed. All previous therapies, including compression bandages, vacuum‐assisted wound closure and zinc paste bandage had failed. The WMCS therapy started in combination with strong short stretch bandages (Figures 9 and 10).
Figure 9.

Wound at (A) treatment start (525 mm2), (B) after 4 weeks (265 mm2) and (C) after 16 weeks (190 mm2).
Figure 10.
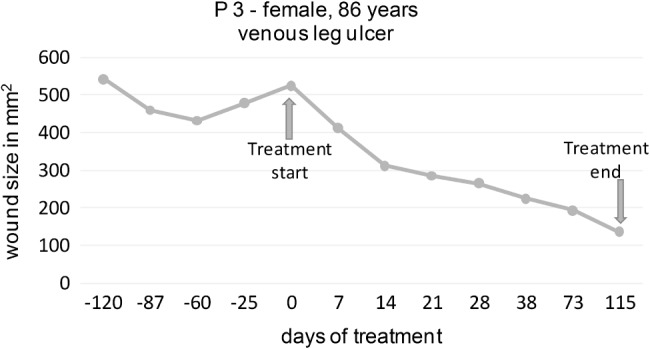
Reduction of wound size (mm2) under wireless micro current stimulation (WMCS) in patient 3.
Discussion
ES in the form of WMCS is an excellent method to significantly accelerate the process of wound healing. WMCS has a huge potential to treat hard‐to‐heal wounds as well as to heal chronic wounds in general. Therefore, we see the use of WMCS in pressure ulcers, venous‐, arterial‐ and mixed‐leg ulcers and diabetic foot ulcers, especially in cases of existing severe accompanying diseases. An extraordinary inflammation and infection of the wound should be treated by fully tested antibiotics before starting the WMCS treatment. Necrotic tissue and coverings must be removed before WMCS is started.
Generally, contraindications for WMCS are pregnancy, any implanted electrical device, any treatment with metal ion‐containing wound‐care products, malignancy close to the wound, epilepsy or other neuro‐excitatory diseases and overshoot‐granulation (rough) tissue of the wound.
The WMCS therapy has multiple advantages in comparison to previous methods of ES and other common methods in the treatment of chronic wounds (Table 1).
Table 1.
Advantages of the WMCS method
| Non‐invasive contactless treatment |
| Free of pain |
| Excellent tolerability – treatment with no essential side effects |
| First positive effects can be seen already 1 week after starting treatment |
| Treatment can be carried out in combination with other applied methods |
| Reduced risk of infections |
| Different areas are treatable in one session – time saving for patients and medical staff |
| Device easy in its transportation and application |
WMCS, wireless micro current stimulation.
After our experiences, an obvious improvement or a clear progression of healing of chronic wounds and a significant reduction of pain (even within 1–2 weeks of the first application) when using the WMCS method were observed. Further testing and comparative controlled studies are necessary to confirm this.
Acknowledgements
The WMCS device was provided free of charge by Wetling Denmark.
The authors have declared no conflicting interests to publish this manuscript.
References
- 1. Kloth LC. Electrical stimulation for wound healing: a review of evidence from in vitro studies, animal experiments, and clinical trials. Int J Low Extrem Wounds 2005;4:23–44. [DOI] [PubMed] [Google Scholar]
- 2. Zhao M, Song B, Pu J, Wada T, Reid B, Tai G, Wang F, Guo A, Walczysko P, Gu Y, Sasaki T, Suzuki A, Forrester JV, Bourne HR, Devreotes PN, McCaig CD, Penninger JM. Electrical signals control wound healing through phosphatidylinositol‐3‐OH kinase‐γ and PTEN. Nature 2006;442:457–60. [DOI] [PubMed] [Google Scholar]
- 3. Cho MR, Thatte HS, Lee RC, Golan DE. Integrin‐dependent human macrophage migration induced by oscillatory electrical stimulation. Ann Biomed Eng 2000;28:234–43. [DOI] [PubMed] [Google Scholar]
- 4. Bourguignon GJ, Bourguignon LY. Electric stimulation of protein and DNA synthesis in human fibroblasts. FASEB J 1987;1:398–402. [DOI] [PubMed] [Google Scholar]
- 5. Goldman RJ, Brewley BI, Golden MA. Electrotherapy reoxygenates inframalleolar ischemic wounds on diabetic patients: a case series. Adv Skin Wound Care 2002;15:112–20. [DOI] [PubMed] [Google Scholar]
- 6. Zhao M, Pu J, Forrester JV, McCaig CD. Membrane lipids, EGF receptors, and intracellular signals colocalize and are polarized in epithelial cells moving directionally in a physiological electric field. FASEB J 2002;16:857–9. [DOI] [PubMed] [Google Scholar]
- 7. Ong P, Laatsch L, Kloth L. Antibacterial effects of a silver electrode carrying microamperage direct current in vitro. J Clin Electrophysiol 1994;6:14–8. [Google Scholar]
- 8. Junger M, Arnold A, Zuder D, Stahl HW, Heising S. Local therapy and treatment costs of chronic, venous leg ulcers with electrical stimulation (Dermapulse): a prospective, placebo‐controlled, double blind trial. Wound Repair Regen 2008;16:480–7. [DOI] [PubMed] [Google Scholar]
- 9. Houghton PE, Kincaid CB, Lovell M, Campbell KE, Keast DH, Woodbury MG, Harris KA. Effect of electrical stimulation on chronic leg ulcer size and appearance. Phys Ther 2003;83:17–28. [PubMed] [Google Scholar]
- 10. Herberger K, Kornek T, Debus ES, Diener H, Augustin M. Electrotherapy of chronic wounds: evidence of clinical effectiveness and benefit. Wound Manage 2011;2:86–93. [Google Scholar]
- 11.Wirsing P, Habrom A. Can WMCS (wireless microcurrent stimulation) improve the treatment of chronic wounds? EWMA Conference 2012, No P149.
- 12.Blatti M, Friedli S, Zehender T. Use of a new method of electrostimulation in‐hard‐to‐heal wounds. EWMA Conference 2012, No P244.
- 13. Castana O, Dimitrouli A, Argyrakos T, Theodorakopoulou E, Stampolidis N, Papadopoulos E, Pallantzas A, Stasinopoulos I, Poulas K. Wireless electrical stimulation: an innovative powerful tool for the treatment of a complicated chronic ulcer. Int J Low Extrem Wounds 2013;12:18–21. [DOI] [PubMed] [Google Scholar]
- 14. Ramadhinara A, Poulas K. Use of wireless microcurrent stimulation for the treatment of diabetes‐related wounds: 2 case reports. Adv Skin Wound Care 2013;26:1–4. [DOI] [PubMed] [Google Scholar]


