Abstract
Oral Candida colonisation is higher in tobacco smokers as compared to non‐smokers; however, it remains unknown whether smokeless tobacco chewers are susceptible to increased oral Candida colonisation. The aim was to determine the oral Candida carriage and species prevalence amongst habitual gutka‐chewers and non‐chewers in a cohort from Karachi, Pakistan. Forty‐five gutka‐chewers and 45 non‐chewers were included. Information regarding age, sex, duration of gutka‐chewing habit, daily frequency of gutka consumption, duration of holding gutka in the mouth, daily frequency of tooth‐brushing and tongue brushing was collected using a questionnaire. Oral yeast samples were collected by scraping the dorsum of the tongue and bilateral buccal mucosa with a sterile cotton swab. Identification of yeast species was performed using standard techniques. Tongue lesions were identified and recorded. Unstimulated whole salivary flow rate (UWSFR) was also measured. There was no significant difference in the mean age, UWSFR and oral Candida carriage among gutka‐chewers and non‐chewers. Individuals were chewing gutka since 4·4 years and were consuming five gutka sachets daily. Candida albicans (C. albicans) was the most common yeast species isolated from 57·8% gutka‐chewers and 64.4% non‐chewers. In 24.4% gutka‐chewers and 22·2% non‐chewers, two candidal strains (C. albicans and Candida tropicalis) were isolated. In conclusion, the present results indicated no significant difference in oral Candida carriage in habitual gutka‐chewers and non‐chewers.
Keywords: Candida; Gutka; Smokeless tobacco
Introduction
Oral fungal organisms, predominantly Candida albicans (C. albicans) are isolated commonly from the oral cavities of healthy humans (1). The precise carriage rate of oral Candida species in healthy individuals has been difficult to estimate; however, a range from 17% to 75% has been reported (2). Various factors that govern the rate of oral candidal carriage include increasing age, female sex, immunosuppression, steroid therapy and tabagism have been reported to augment oral candidal colonisation 1, 2, 3, 4, 5, 6, 7, 8. It has been proposed that contents of tobacco (such as nicotine, polycyclic aromatic hydrocarbons, polonium, nitrosodietheinal amine and nitrosoprolin) act as nutrients for Candida species thereby facilitating their proliferation (9). This may be one explanation for the findings reported in one study (10) in which colonisation with oral Candida was reported to be significantly higher in tobacco‐smokers as compared to non‐smokers.
Tobacco‐chewing is a cultural practice in many Southeast Asian countries including Bangladesh, India, Pakistan and Sri Lanka 11, 12, 13, 14, 15. Gutka is a form of smokeless tobacco that is mainly a blend of powdered tobacco, areca‐nut (fruit of Areca catechu) and slaked lime (aqueous calcium hydroxide) 12, 13. Other components of gutka include fragrance compounds including menthol, musk ketones and sandalwood. It is commercially sold with various brand names in glittery sachets (Figure 1). Gutka is placed in the mouth initially and masticated gently. It is then held against the buccal mucosa over a long period of time and chewed gently and sucked intermittently on a relatively continual basis. When desired, the contents may either be swallowed or expectorated (12). As powdered tobacco is the major source of nicotine in gutka, it was hypothesised that habitual gutka‐chewers harbor increased levels of oral Candida species compared with individuals not using tobacco in any form. To our knowledge (from indexed literature), oral carriage of Candida species in habitual gutka‐chewers has not yet been investigated.
Figure 1.
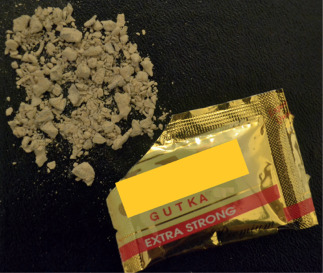
Gutka commercially available in colourful and glittery sachets.
The aim of this study was to identify carriage of oral Candida, and the prevalence of this species amongst habitual gutka‐chewers and non‐chewers.
Methods
Ethical guidelines
This study was approved by the research ethics review board of the Engineer Abdullah Bugshan Research Chair for Growth Factors and Bone Regeneration, King Saud University, Riyadh, Saudi Arabia in accordance with the Declaration of Helsinki (2000). It was mandatory for subjects to have read and signed the consent form before being included in this study.
Exclusion criteria
The exclusion criteria encompassed the following: (i) tobacco smoking (16); (ii) alcohol consumption (16); (iii) exclusive areca‐nut chewing (13); (iv) individuals currently using or those having used antibiotics, steroids and/or non‐steroidal anti‐inflammatory drugs within the past 3 months (16); (v) self‐reported systemic disorders such as diabetes mellitus, hepatitis B, hepatitis C, infection with human immunodeficiency virus and acquired immunodeficiency syndrome (16); and (vi) individuals who reported to be wearing partial and/or complete dentures 1, 16.
Study participants
Habitual gutka‐chewers were defined as individuals who reported that they have been chewing at least one sachet of gutka daily and exclusively since at least 1 year (12). Individuals who reported to have never used tobacco in any form were designated as ‘non‐chewers' (12).
Questionnaire
Information regarding age, sex, duration of gutka‐chewing habit, daily frequency of gutka consumption (number of gutka sachets consumed daily), duration of retaining gutka in the mouth (in minutes), daily frequency of tooth‐brushing and tongue brushing was collected using a standardised questionnaire.
Measurement of unstimulated whole salivary flow rate
For collection of unstimulated whole saliva samples, participants (gutka‐chewers and non‐chewers) were seated comfortably on a chair in a bent‐forward position and requested to spit (without swallowing) for five continuous minutes into a gauged measuring cylinder. Unstimulated whole salivary flow rate (UWSFR) was expressed in millilitres per minute (ml/ minute).
Collection of oral Candida samples and culture
Oral Candida samples were collected as described elsewhere (1). In summary, subjects were instructed to avoid eating and drinking for at least 2 hours before collection of microbiological samples. Each sample was collected by scraping the dorsum of the tongue and bilateral buccal mucosa with a sterile cotton swab (Biomérieux S.A., Montalieu‐Vercieu, France) (1). The swabs were immediately returned to the containment tube after sampling.
Candida strains were cultured in Sabouraud dextrose agar (Becton, Dickinson and Company, Sparks, MD) at 37 °C to quantify the colony‐forming units in the oral cavities of gutka‐chewers and controls 5, 6. The cultures were inspected after 24 hours and until 7 days of incubation for yeast growth. The cultures were subjected to speciation.
Identification of oral yeast samples
Identification of oral yeast species was performed using a yeast identification system (API 32‐C System bioMériux yeast identification programme, Lyon, France) (1). If identification was not possible with the API 32‐C system, the yeast isolate was subjected to molecular identification.
For DNA isolation, yeast cells were suspended in 200 µl sterile polymerase chain reaction (PCR)‐grade water and genomic DNA was prepared using MagNA pure (Roche Diagnostics GmbH, Mannheim, Germany) a DNA preparation robot (17). For DNA sequencing and PCR analysis, a region (about 500 bp) of 18S ribosomal ribonucleic acid gene was amplified by PCR using universal primers and ampliTaq Gold DNA polymerase. Primers and free nucleotides from the PCR products were then removed by using QIAquick PCR purification kit (250) (Qiagen, GmbH, Hilden, Germany). The purified PCR products were processed for DNA sequencing by BigDye Terminator Cycle Sequencing using capillary electrophoresis technology in ABI 310 Genetic Analyzer (Applied Biosystems, Foster City, CA). Both strands of PCR amplified DNA fragments were sequenced to avoid error of sequencing (18). The DNA sequence was analysed by a software and searched in the Blast DNA database for yeast identification and typing 19, 20.
Tongue lesions
A clinical diagnosis of tongue lesions (fissured tongue, geographic tongue, coated tongue, hairy tongue and median rhomboid glossitis) was made using standardised World Health Organization criteria 21, 22, 23, 24, 25.
Statistical analysis
Statistical analysis was performed using a software program (SPSS Version 18., Chicago, IL). Level of significance between the groups (gutka‐chewers and non‐chewers) was determined using Mann–Whitney U‐test). P values less than 0 ·05 were considered statistically significant.
Results
Characteristics of the study population
Forty‐five gutka‐chewers (42 males and 3 females) and 45 non‐chewers (41 males and 4 females) volunteered to participate in this study. There was no significant difference in the mean age of gutka‐chewers (33·6 years) and non‐chewers (35 years). Individuals indicated that they had been chewing gutka habitually for a mean duration of 4·4 years and consumed an average of five gutka sachets daily. Gutka‐chewers placed this smokeless tobacco in their mouth for an average of 6·2 minutes before either swallowing or spitting‐out the remnants. These results are shown in Table 1.
Table 1.
Characteristics of the study population
| All individuals (n = 90) | ||
|---|---|---|
| Gutka‐chewers (n = 45) | Non‐chewers (n = 45) | |
| Mean age in years (range) | 33·6 (28–36) | 35 (26–37) |
| Mean duration of gutka‐chewing habit in years (range) | 4·4 (3–6) | – |
| Mean daily consumption of gutka (range) | 5(4–7) | – |
| Mean duration of placement of gutka in the mouth in minutes (range) | 6·2 (5–10) | – |
| Oral hygiene maintenance | ||
| Once daily (percentage) | 37·7% | 31·1% |
| Twice daily (percentage) | 62·3% | 68·9% |
| Three times or more (percentage) | – | – |
| Sometimes | – | – |
| Tongue brushing | ||
| Once daily (percentage) | – | – |
| Twice daily (percentage) | – | – |
| Three times or more (percentage) | – | – |
| Sometimes | 4·4% | 20% |
Unstimulated whole salivary flow rate
The mean UWSFR in gutka‐chewers and non‐chewers was 0·56 ml/minute (range 0·5–0·64 ml/minute) and 0·54 ml/ minute (range 0·5‐0·6 ml/minute) respectively. There was no significant difference in UWSFR between gutka‐chewers and non‐chewers.
Oral hygiene maintenance
Most of the gutka‐chewers (62·3%) and non‐chewers (68·9) reported that they brushed their teeth twice daily. Twenty percent of non‐chewers and 4·4% gutka‐chewers reported that they occasionally scraped the dorsum of tongue with a toothbrush following brushing (Table 1).
Oral Candida carriage in habitual gutka‐chewers and non‐chewers
Overall, there was no significant difference in the oral carriage rate of Candida between gutka‐chewers and non‐chewers, with carriage rates of 57·8% and 64·4%, respectively (Table 2). Candida tropicalis was isolated from 4·4% gutka‐chewers and 6·7% non‐chewers. Strains of C. albicans and C. tropicalis existed together in 24·4% gutka‐chewers and 22·2% non‐chewers (Table 2). C. parapsilosis was isolated from three gutka‐chewers (6·6%) and one (2·2%) non‐chewer. There were no Candida species isolated from three gutka‐chewers (6·6%) and five (11·1%) non‐chewers (Table 2).
Table 2.
Oral candida species isolated from habitual gutka‐chewers and non‐chewers
| All individuals (n = 90) | Total participants (%) (n = 90) | ||
|---|---|---|---|
| Gutka‐chewers (%) (n = 45) | Non‐chewers (%) (n = 45) | ||
| Candida albicans | 26 (57·8) | 29 (64·4) | 55 (61·1) |
| Candida tropicalis | 2 (4·4) | 3 (6·7) | 5 (5·6) |
| Candida albicans + Candida tropicalis | 11 (24·4) | 10 (22·2) | 21 (23·3) |
| Candida parapsilosis | 3 (6·7) | 1 (2·2) | 4 (4·4) |
| Candida glabrata | – | – | – |
| Candida krusei | – | – | – |
| Candida gullerimondi | – | – | – |
| Candida dublinensis | – | – | – |
| Candida lusitaniae | – | – | – |
| No Candida species isolated | 3 (6·7) | 2 (4·4) | 5 (5·6) |
Clinical examination: lesions on the tongue
Based on clinical assessments, there was no difference in the prevalence of oral lesions between the two test populations and in fact, none of the subjects had oral lesions.
Discussion
The present results suggest that gutka‐chewers and non‐chewers carry similar levels of Candida in their mouths. Overall, the rate of carriage for oral Candida reported in our study population (61·1%) was similar to that reported from other parts of the world 5, 6, 21, 22.
A number of factors including the dry oral environment due to a reduced salivary flow rate have also been reported to augment oral candidal proliferation 25, 26, 27, 28. According to the present results, the salivary flow rates in both groups were within the normal range. Hence the phenomenon of increased oral yeast carriage rate in this cohort with no apparently discernible risk factors warrant further studies with a larger population. A possible explanation for this may be associated with the patient selection criteria adopted in this study. It is known that advancing age, habitual tobacco‐smoking, chronic denture‐wearing, xerostomia and systemic diseases (such as poorly‐controlled diabetes mellitus and acquired immune deficiency syndrome) promote oral candidal proliferation 1, 25, 27, 28, 29. Although the exact mechanism by which tobacco‐smoking augments oral candidal colonisation remains unclear, it has been hypothesised that aromatic hydrocarbons in tobacco smoke are utilised by oral Candida species that in turn increases their proliferation 9, 30. Chronic denture‐wearing has been reported to obstruct salivary flow from minor salivary glands thereby resulting in low pH, which facilitates oral candidal proliferation (27). Since tobacco smoking, denture wearing and systemic diseases are significant risk factors for proliferation of oral Candida, such individuals were excluded from the present investigation. In addition, participants of this study were relatively young individuals and exhibited normal salivary flow rates thereby further reducing the risk for proliferation/infection with Candida. The findings reported here are in accordance with the studies reported by others 5, 6 where oral candida species were investigated among habitual betel‐nut (an integral ingredient of gutka) chewers and non‐chewers. Hence, the phenomenon of increased oral yeast carriage rate in this cohort with no apparently discernible risk factors warrant further studies with a larger population.
In general, the current study indicates that gutka chewing has no significant effect on oral carriage of Candida species, although the high overall oral yeast carriage rate in the population (∼61%) may be the reason that we could not uncover such a difference, if any. Of the more than 20 species of Candida, C. albicans with an arsenal of superior virulence attributes is widely accepted as the major commensal flora of the oral cavity, with C. tropicalis and Candida glabrata closely following 5, 6. This is confirmed in our study as C. albicans and C. tropicalis were the most common oral yeast species isolated from both gutka‐chewers and non‐chewers.
In this study, no tongue lesions were observed in either study group. It is notable that the mean duration of the gutka‐chewing habit reported here was nearly 4 years and these individuals generally placed gutka in their oral vestibules for approximately 6 minutes. It seems that chewing gutka for less than 10 minutes and a short history of gutka‐chewing habit does not contribute to increases in infection with cultivable candidal organisms found on oral mucosal surfaces. In a previous study (12), gutka‐chewers with periodontal disease had been addicted to the chewing abuse for approximately a decade and had been placing gutka in the buccal vestibule for around 20 minutes before either swallowing or spitting it out. Therefore, it might be argued that in individuals with a long history of gutka‐chewing and retaining it in the buccal vestibule for significantly longer durations it may lead to significantly higher counts of Candida as well as tongue lesions as compared to controls subjects who do not use tobacco in any form. However, further studies are warranted in this regard.
Oral Candida has been isolated from dental plaque (29). Oral candidal colonisation has been reported to be higher in individuals with poor oral health (e.g. those with high plaque scores and gingival bleeding indices) as compared to those with good oral hygiene. In this study, most of the gutka‐chewers and non‐chewers reported that they brush their teeth twice daily and sometimes perform tongue scraping following tooth brushing. A satisfactory oral health status in gutka‐chewers and non‐chewers may have also contributed to the findings reported here whereas there did not appear to be any differences in oral colonisation of candida for either group. The above notwithstanding it is still possible that gutka‐chewers and non‐chewers with poor oral health might demonstrate a variation in oral candidal carriage and requires additional study. Moreover, it cannot be over‐emphasised that other methods for quantification of clinically meaningful colonisation with oral candidal should be used for analyses of samples (e.g. cytological smears).
Conclusion
Within the limits of this study, it is concluded that there is no significant difference in the levels of Candida in the mouths of either gutka‐chewers or non‐chewers.
Acknowledgements
The authors declare that they have no conflict of interest and there was no external source of funding for this study.
Author Contribution
FJ performed the mycological investigations, wrote the manuscript, performed the statistical analysis and revised the manuscript. HCT wrote the manuscript and revised it prior to submission. GN wrote the manuscript and revised it prior to submission. NN wrote the manuscript and participated in discussions throughout the study period. LPS wrote the manuscript and revised it prior to submission. KA‐H wrote the manuscript and revised it prior to submission. All authors read and approved the final manuscript.
References
- 1. Javed F, Klingspor L, Sundin U, Altamash M, Klinge B, Engström PE. Periodontal conditions, oral Candida albicans and salivary proteins in type 2 diabetic subjects with emphasis on gender. BMC Oral Health 2009;9:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nittayananta W, Jealae S, Winn T. Oral Candida in HIV‐infected heterosexuals and intravenous drug users in Thailand. J Oral Pathol Med 2001;30:347–54. [DOI] [PubMed] [Google Scholar]
- 3. Tsang PC, Samaranayake LP. Oral manifestations of HIV infection in a group of predominantly ethnic Chinese. J Oral Pathol Med 1999;28:122–127. [DOI] [PubMed] [Google Scholar]
- 4. Ellepola AN, Samaranayake LP. Inhalational and topical steroids, and oral candidosis: a mini review. Oral Dis 2001;7:211–6. [PubMed] [Google Scholar]
- 5. Reichart PA, Samaranayake LP, Samaranayake YH, Grote M, Pow E, Cheung B. High oral prevalence of Candida krusei in leprosy patients in Northern Thailand. J Clin Microbiol 2002;40:4479–4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reichart PA, Khongkhunthian P, Samaranayake LP, Yau J, Patanaporn V, Scheifele C. Oral Candida species and betel quid‐associated oral lesions in Padaung women of Northern Thailand. Mycoses 2005;48:132–6. [DOI] [PubMed] [Google Scholar]
- 7. Baboni FB, Barp D, Izidoro AC, Samaranayake LP, Rosa EA. Enhancement of Candida albicans virulence after exposition to cigarette mainstream smoke. Mycopathologia 2009;168:227–35. [DOI] [PubMed] [Google Scholar]
- 8. de Azevedo Izidoro AC, Semprebom AM, Baboni FB, Rosa RT, Machado MA, Samaranayake LP, Rosa EA. Low virulent oral Candida albicans strains isolated from smokers. Arch Oral Biol 2012;57:148–53. [DOI] [PubMed] [Google Scholar]
- 9. Hsia CC, Sun TT, Wang YY, Anderson LM, Armstrong D, Good RA. Enhancement of formation of the esophageal carcinogen benzylmethylnitrosoamine from its precursors by Candida albicans . Proc Natl Acad Sci USA 1981;78:1878–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ellepola AN, Khan ZU, Joseph B, Chandy R, Philip L. Prevalence of Candida dubliniensis among oral Candida isolates in patients attending the Kuwait University Dental Clinic. Med Princ Pract 2011;20:271–6. [DOI] [PubMed] [Google Scholar]
- 11. Ranasinghe AW, Warnakulasuriya KA, Johnson NW. Low prevalence of expression of p53 oncoprotein in oral carcinomas from Sri Lanka associated with betel and tobacco chewing. Eur J Cancer B Oral Oncol 1993;29B:147–50. [DOI] [PubMed] [Google Scholar]
- 12. Javed F, Altamash M, Klinge B, Engström PE. Periodontal conditions and oral symptoms in gutka‐chewers with and without type 2 diabetes. Acta Odontol Scand 2008;66:268–273. [DOI] [PubMed] [Google Scholar]
- 13. Javed F, Chotai M, Mehmood A, Almas K. Oral mucosal disorders associated with habitual gutka usage: a review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:857–64. [DOI] [PubMed] [Google Scholar]
- 14. Joshi U, Modi B, Yadav S. A study on prevalence of chewing form of tobacco and existing quitting patterns in urban population of Jamnagar, Gujarat. Indian J Community Med 2010;35:105–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rahman MA, Spurrier N, Mahmood MA, Rahman M, Choudhury SR, Leeder S. Is there any association between use of smokeless tobacco products and coronary heart disease in Bangladesh? PLoS One 2012;7:e30584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Javed F, Näsström K, Benchimol D, Altamash M, Klinge B, Engström PE. Comparison of periodontal and socioeconomic status between subjects with type 2 diabetes mellitus and non‐diabetic controls. J Periodontol 2007;78:2112–9. [DOI] [PubMed] [Google Scholar]
- 17. Knepp JH, Geahr MA, Forman MS, Valsamakis A. Comparison of automated and manual nucleic acid extraction methods for detection of enterovirus RNA. J Clin Microbiol 2003;4:3532–3536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jalal S, Ciofu O, Høiby N, Gotoh N, Wretlind B. Molecular mechanisms of fluoroquinolone resistance in Pseudomonas aeruginosa isolates from cystic fibrosis patients. Antimicrob Agents Chemother 2000;44:710–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jonasson J, Olofsson M, Monstein HJ. Classification, identification and subtyping of bacteria based on pyrosequencing and signature matching of 16S rDNA fragments. APMIS 2002;110:263–72. [DOI] [PubMed] [Google Scholar]
- 20. Gharizadeh B, Norberg E, Löffler J, et al. Identification of medically important fungi by the Pyrosequencing technology. Mycoses 2004;47:29–33. [DOI] [PubMed] [Google Scholar]
- 21. Kramer IR, Pindborg JJ, Bezroukov V, Infirri JS. Guide to epidemiology and diagnosis of oral mucosal diseases and conditions. World Health Organization. Community Dent Oral Epidemiol 1980;8:1–26. [DOI] [PubMed] [Google Scholar]
- 22. Samaranayake LP, MacFarlane TW, editors. Oral candidosis. Bristol, UK: Wright, 1990. [Google Scholar]
- 23. Terai H, Shimahara M. Atrophic tongue associated with Candida. J Oral Pathol Med 2005;34:397–400. [DOI] [PubMed] [Google Scholar]
- 24. Gönül M, Gül U, Kaya I, Koçak O, Cakmak SK, Kiliç A, Kiliç S. Smoking, alcohol consumption and denture use in patients with oral mucosal lesions. J Dermatol Case Rep 2011;5:64–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Al‐Hezaimi K, Javed F, Ali TS, Al‐Askar M, Al‐Rasheed A. Rapidly progressive periodontal disease associated with human immunodeficiency virus. J Coll Physicians Surg Pak 2012;22:186–8. [PubMed] [Google Scholar]
- 26. Ueta E, Tanida T, Doi S, Osaki T. Regulation of Candida albicans growth and adhesion by saliva. J Lab Clin Med 2000;136:66–73. [DOI] [PubMed] [Google Scholar]
- 27. Aizen E, Feldman PA, Madeb R, et al. Candida albicans colonization of dental plaque in elderly dysphagic patients. Isr Med Assoc J 2004;6:342–5. [PubMed] [Google Scholar]
- 28. Tanida T, Ueta E, Tobiume A, Hamada T, Rao F, Osaki T. Influence of aging on candidal growth and adhesion regulatory agents in saliva. J Oral Pathol Med 2001;30:328–35. [DOI] [PubMed] [Google Scholar]
- 29. Tanida T, Okamoto T, Okamoto A, Wang H, Hamada T, Ueta E, Osaki T. Decreased excretion of antimicrobial proteins and peptides in saliva of patients with oral candidiasis. J Oral Pathol Med 2003;32:586–94. [DOI] [PubMed] [Google Scholar]
- 30. Jung HJ, Hwang IA, Sung WS, Kang H, Kang BS, Seu YB, Lee DG. Fungicidal effect of resveratrol on human infectious fungi. Arch Pharm Res 2005;28:557–60. [DOI] [PubMed] [Google Scholar]


