Abstract
Recent clinical research has generated interest in the use of sacral wound dressings as preventive devices for patients at risk of ulceration. This study was conducted to identify the modes of action through which dressings can add to pressure ulcer prevention, for example, shear and friction force redistribution and pressure distribution. Bench testing was performed using nine commercially available dressings. The use of dressings can reduce the amplitude of shear stress and friction reaching the skin of patients at risk. They can also effectively redirect these forces to wider areas which minimises the mechanical loads upon skeletal prominences. Dressings can redistribute pressure based upon their effective Poisson ratio and larger deflection areas, providing greater load redistribution.
Keywords: Poisson's ratio, Dressing prophylaxis, Force dispersion, In vitro force measurement, Point load deflection, Pressure ulcer, Pressure ulcer prevention, Shear
Introduction
Continuing risk of developing pressure ulcers drives both clinical and in vitro research into practices, risk mechanisms, mitigation methods and skin protection policies and procedures. Clinically, a number of recent studies have followed up on the primary report by Brindle 1 that the use of wound dressings is an effective addition to standard preventive measures 2, 3, 4. In vitro work by Gawlitta et al. 5 has shown that the force delivered to tissue, in the form of distorting stress, is much more damaging in the loading excursion than ischaemia and the resulting cellular anoxia.
The combination of clinical success in the prevention of ulceration using dressings prophylactically and the new work describing the mechanisms of tissue destruction in ulceration drive a significant question: What are the mechanisms of action by which the dressing modifies the pressure, friction or shear forces applied to the tissue that explain this successful intervention? Here, we review bench test results performed by us and reported elsewhere as well as new considerations in the results of this bench work to understand the performance impact of the dressings used, the features of the dressings available and the relative value of these features in providing physical intervention to ulceration. This is done with particular focus on the elements of recent review as risk factors for ulceration 6.
Materials and Methods
Dressings tested
Nine commercially available dressings were tested in at least triplicates; descriptions of dressing construction are provided in Table 1. Dressings of similar sizes were chosen as much as possible between manufacturers; however, because of differences in dressing design, intended function and manufacturer offerings, we were unable to eliminate differences in size variation of the dressings. All Testing was performed under ISO test laboratory environmental controls 7.
Table 1.
Description of dressing construction
| Dressing # | Dressing name | Size (cm) | Area of dressing pad (cm2) | Thickness (cm) | Number of layers | Adhesive | Absorbent layer | Adhesive on absorbent layer |
|---|---|---|---|---|---|---|---|---|
| 1 | Versiva XC | 24·7 × 20·7 | 145·59 | 0·22 | 4 | Acrylic | Foam covered by hydrofibre™ | No |
| 2 | Allevyn Sacrum | 22 × 22 | 206·6 | 0·40 | 3 | Acrylic | Hydrocellular foam | Yes |
| 3 | Allevyn Sacrum | 17 × 17 | 94·53 | 0·40 | 3 | Acrylic | Hydrocellular foam | Yes |
| 4 | Allevyn Plus Sacrum | 17 × 17 | 95·99 | 0·59 | 3 | Acrylic | Hydrocellular foam | Yes |
| 5 | Allevyn Gentle Border Heel | 23 × 23 | 200·48 | 0·55 | 3 | Silicone | Hydrocellular foam | Yes |
| 6 | Optifoam Sacrum | 15·2 × 16·5 | 47·98 | 0·26 | 2 | Acrylic | Foam | No |
| 7 | Biatain Adhesive Foam (sacral dressing) | 23 × 23 | 130·32 | 0·42 | 3 | Acrylic | Foam | No |
| 8 | Mepilex Border Sacrum | 20 × 20 | 117·79 | 0·36 | 5 | Silicone | Foam | Yes |
| 9 | Mepilex Border Sacrum | 23 × 23 | 237·63 | 0·36 | 5 | Silicone | Foam | Yes |
Friction and shear testing using steel sled
This test was conducted using the BS 3424‐10:1987 8 method to measure the friction of a dressing surface. The method was modified to include use of a ground steel sled with an angled face to simulate a bony structure sliding over the dressing surfaces and was sized to represent the ischial tuberosity. The method is described elsewhere in the literature. From the friction outputs, the shear stresses experienced by the patient and at the surface of dressing were calculated. We believe that this method is a better representation of the use case than others in the literature 9.
Friction and shear testing using shear displacement method
A 6‐mm thick glycerin gel overlay was used to simulate the elastic properties of skin. A Molten Predia shear sensor (Molten Corp., Hiroshima, Japan) was used to measure shear and normal pressure at the glycerin gel surface. A dressing was placed over the sensor. A foam sled wrapped with a cotton sheet and secured by a steel frame was positioned over the dressing/Predia sensor/glycerin gel assembly (Figure 1). The foam sled was weighed to apply 10·3 mmHg (1·4 kPa, 0·2 psi) pressure to the dressing surface. The structure was placed on a test plane parallel to the plane of a Chatillon LF Plus computerised test stand. The sled was pulled at a rate of 50 mm/minute over the dressing. Shear was measured as Newtons of lateral force during displacement of the body analogue across the support surface. Normal pressure was also recorded during the test as mmHg between the surfaces.
Figure 1.

Set‐up of shear displacement method.
Human subject validation of shear displacement
The shear sensor was attached to the sacrum of a male human volunteer weighing 95·3 kg and wearing only an underwear and a cotton hospital gown. The volunteer was positioned on a viscoelastic mattress covered with a cotton bed sheet for 60 seconds, and the peak shear force was recorded as the head of the bed was raised from supine to a 45° angle.
Point load deflection and Poisson's ratio testing
This test used a 13‐mm diameter glass rod indenter compressed against a dressing backed with a glycerin gel layer and 60 mm of foam. The test measured the load deflection. From the area of deflection and the peak load, the Poisson's ratio was calculated as the ratio of the lateral strain to the axial strain 10. For all intensive purposes, the foam base and the glycerin gel layers were assumed to be isotropic materials and the loading was perfectly axial. The test method described by Call and coworkers 11 is discussed here.
Results
Friction and shear results using steel sled
Coefficient of friction values were calculated for the outer surface of the dressings. The static and dynamic friction values for each dressing can be seen in Figure 2. The shear stresses were calculated from the friction data as a function of surface area for both the patient and the dressings, and the difference was calculated to produce the shear that had to be delivered to the patient. These values can be seen in Figure 3. Note that the Versiva XC dressing did not have an adhesive layer on the foam, resulting in a very low difference in shear between the patient's side and the outer surface of the dressing.
Figure 2.
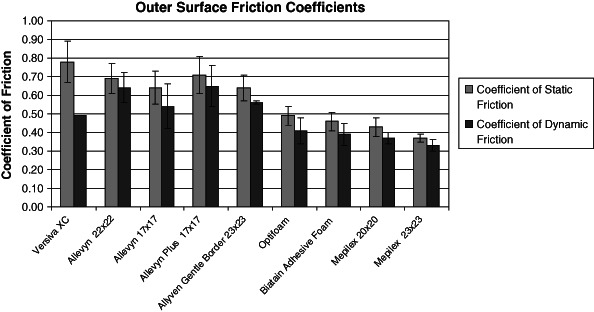
Dressing coefficient of friction (α = 0·05).
Figure 3.
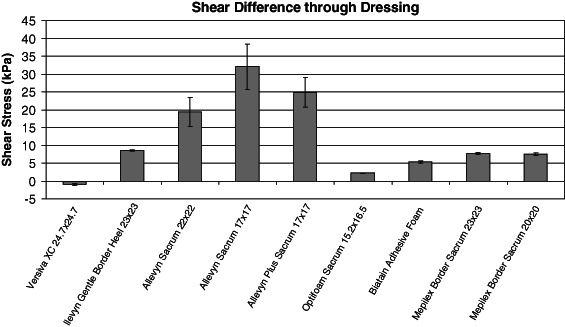
Shear stress delivered to the patient (α = 0·05).
Friction and shear testing using shear displacement method
The shear displacement method performed using the Molnlycke Border Sacrum dressing resulted in significant reduction in shear from the undressed control (Figure 4). Similar peak shear values were obtained between the human subject and the bench test, providing a validation of the model (Figure 5).
Figure 4.
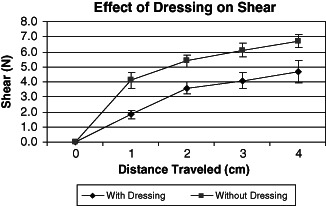
Effect of dressing on shear (α = 0·05).
Figure 5.
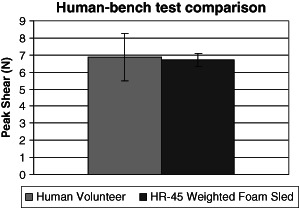
Human subject and bench test validation (α = 0·05).
Point load deflection and Poisson's ratio results
The point load deflection testing measured the force at maximum deflection on each dressing and compared it to a control without a dressing. These results can be seen in Figure 6. Additionally, the Poisson's ratio was calculated for each dressing and can be seen in Figure 7. The deflection area of each trial was measured and compared with the contact area of the padding for each dressing and the control. The results can be seen in Figure 8. Variability in this data was so low that error bars for α = 0·05 are indistinguishable from the bars in the graph.
Figure 6.
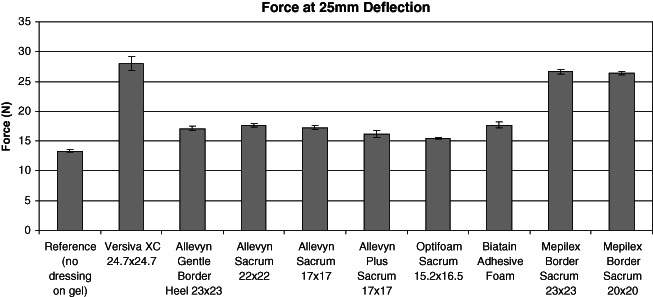
Point load at maximum deflection for nine dressings and control (no dressing) (α = 0·05).
Figure 7.
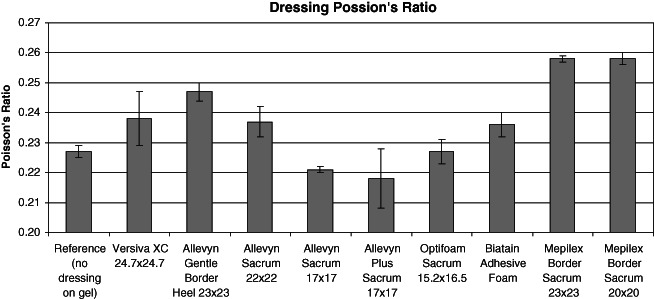
Poisson's ratio for nine dressings and control (no dressing) (α = 0·05).
Figure 8.
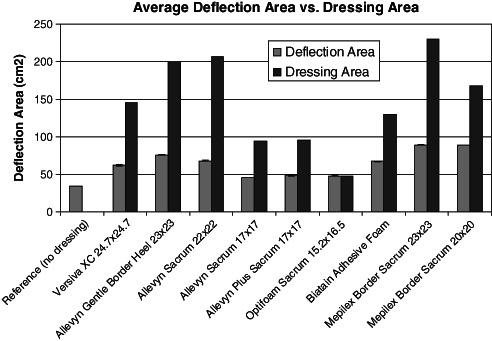
Dressing deflection area and contact area (α = 0·05).
Discussion
Testing philosophy or perspective is critical to this experimental design. The tests used to characterise a dressing's protective effect must reflect the typical case and the proper model of risk mitigation so as to make the approach valid. For example, the use of a very low friction dressing surface might appear to reduce friction at the point of concern. However, in reality, an area of very low friction created at the sacrum following the presence of low friction dressing changes the body's static versus dynamic balance in maintaining body position in bed. Too much friction between the dressing and the support surface may apply large stresses to the tissue, whereas too little friction causes the body to slide. This could result in movement, increasing the risk to tissue when it reaches the elastic limit of the skin at an accelerated rate. However, the safer tissue conservation approach would be to distribute the shear force over as large an area as possible and to the tissue outside the area of risk. Therefore, tests must be used that not only characterise friction of dressings but also characterise the safe mitigation of those friction forces.
Characterisation of dressing architecture shows that there are a number of variables that appear in the body of dressings available in the industry. These variables play a significant role in mitigating forces applied to the dressing‐on‐the‐skin structure (Table 1). Horizontal layers translate forces in a lateral direction. Foams used in construction, absorb forces when the foam elastically compresses. Thickness or loft creates the opportunity for cushioning and cross‐sectional shear translation that absorbs shear force before it is delivered to the underlying skin. Thickness combined with the presence or absence of lateral structure layers redirect pressure in a Poisson fashion, resulting in the area under the dressing being impacted by the force larger than the area of force application on the outside of the dressing. This cone‐shaped influence spreads the force to surrounding tissue and away from the points of the bony prominences. Dressings may protect the skin by increasing the load‐bearing area of the underlying tissue 5. A high Poisson's ratio indicates that the dressing disperses the load over a greater area. It is to be noted that a piece of cork will produce a Poisson's ratio of 0·0, whereas a piece of rubber will produce a ratio of 0·5 10. The dressings on glycerin gel and foam body analogue produced Poisson ratios in the range of 0·20–0·26, falling within the range of expected isotropic material (0·25) 10.
Dressing adhesive strength drives shear difference through the dressing (Figure 3), which plays an important role in the mechanisms of ulcer prevention. When a nurse applies the dressing to a patient, adequate adhesion is required to maintain positioning (12,13); too low adhesion allows the dressing to move or release from the skin, whereas too high adhesion causes cell stripping or disruption of the granulation bed in the case of wound healing. Silicone adhesive is elastic in nature and absorbs shear and protects the skin by elastic deformation. When adhered to the skin, the dressing displaces forces as an assembly to the area outside and away from the area of risk being protected by the dressing. When the shear force exceeds the designed adhesive strength the dressing will release from the skin and effectively absorb the shear that would have damaged tissue.
Our results indicate that dressings can mitigate shear and friction forces' impact on the underlying test surfaces representing the skin. The dressings tested were all of different sizes and various forms of construction (i.e. adhesion at the absorbent layer). Our results suggest that a number of different variables influence the shear delivered to the patient. It is observed that the presence of a dressing significantly reduces the shear delivered to the skin through five different force mitigating features: (i) shear displaced outside the dressing area; (ii) silicone adhesive elastically absorbs shear; (iii) bulk modulus absorbs shear; (iv) multiple layers create a displacement plane absorbing shear and (v) cross‐sectional distortion absorbs shear.
This article does not address the impact of microclimate that the dressing plays in the prevention of pressure ulceration. Additional work has been performed and can be reviewed in another work 14.
Conclusions
Dressings can be used to enhance but not replace pressure ulcer prevention strategies. Understanding the potential risks and benefits allows the prevention of misapplication of dressings. It is appropriate to create guidance documents to educate nurses and caregivers in the proper application of dressings in the prophylaxis of pressure ulcers.
The use of Mepilex and Allevyn dressings can provide reduction in frictional forces away from critical areas. The use of Mepilex dressings provides mitigation of shear forces observed at critical areas on the patient. The dressings can transfer the shear away from critical areas or actually absorb some of the stresses within the construction of the dressing.
The use of dressings with horizontal fabric structures, such as the Mepilex, provides a greater pressure distribution that is ideal for transferring load over a greater area. It was observed that the size of the dressing does play a role in the outcome of these tests. This is based on the test forces being applied to a dressing structure that reacts to the loading as a cohesive unit, redistributing the test load over the responding area of the dressing. Therefore, the use of proper sizing is also very important.
References
- 1. Brindle CT. Outliers to the Braden scale: identifying high risk ICU patients and the results of prophylactic dressing use. World Council Enterost Therap J 2009;30:11–8. [Google Scholar]
- 2. Chaiken N. Reduction of sacral pressure ulcers in the intensive care unit using a silicone bordered foam dressing. J Wound Ostomy Continence Nurs 2012;39:143–5. [DOI] [PubMed] [Google Scholar]
- 3. Walsh NS, Blanck AW, Smith L, Cross M, Andersson L, Polito C. Use of a sacral silicone border foam dressing as one component of a pressure ulcer prevention program in an intensive care unit setting. J Wound Ostomy Continence Nurs 2012;39:146–9. [DOI] [PubMed] [Google Scholar]
- 4. Santamaria N, Gertz M, Sage S, McCann J, Freeman A, Vassiliou T, DeVincentis S, Ng AW, Manias E, Liu W, Knott J. A randomised controlled trial of the effectiveness of soft silicone foam multi‐layer dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients. Int Wound J 2013. DOI: 10.1111/iwj.12101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gawlitta D, Li W, Oomens CW, Baaijens FP, Bader DL, Bouten CV. The relative contributions of compression and hypoxia to development of muscle tissue damage: an in vitro study. Ann Biomed Eng 2007;35:273–84. [DOI] [PubMed] [Google Scholar]
- 6.Wounds International. Pressure ulcer prevention. Pressure, shear, friction and microclimate in context. London: Wounds International, 2010. URL http://www.woundsinternational.com/pdf/content_8925.pdf [accessed on 11 December 2012].
- 7.International Organization for Standardization. Standard atmospheres for conditioning and/or testing—specifications. ISO 554‐1976 (E).
- 8.British Standards Institution. Testing coated fabrics—Part 10: methods 12A and 12B determination of surface drag. BS 3424‐10:1987.
- 9. Ohura T, Takahashi M, Ohura N. Influence of external forces (pressure and shear force) on superficial layer and subcutis of porcine skin and effects of dressing materials: are dressing materials beneficial for reducing pressure and shear force in tissues? Wound Repair Regen 2008;16:102–7. [DOI] [PubMed] [Google Scholar]
- 10. Callister WD. Materials science and engineering, 6th edn. Hoboken: John Wiley & Sons, Inc, 2003:121–2. [Google Scholar]
- 11. Ferguson‐Pell M, Hirose H, Nicholson G, Call E. Thermodynamic rigid cushion loading indenter: a buttock‐shaped temperature and humidity measurement system for cushioning surfaces under anatomical compression conditions. J Rehabil Res Dev 2009;46:945–56. [DOI] [PubMed] [Google Scholar]
- 12. Reger SI, Ranganathan VK, Sahgal V. Support surface interface pressure, microenvironment, and the prevalence of pressure ulcers: an analysis of the literature. Ostomy Wound Manage 2007;53:50–8. [PubMed] [Google Scholar]
- 13. Ohura N, Icholka S, Nakasuka T, Shlbata M. Evaluating dressing materials for the prevention of shear force in the treatment of pressure ulcers. J Wound Care 2005;14:401–4. [DOI] [PubMed] [Google Scholar]
- 14. Call E, Pedersen J, Bill B, Oberg C, Ferguson‐Pell M. Microclimate impact of prophylactic dressings using in vitro body analog method. Wounds 2013;25:94–103. [PubMed] [Google Scholar]


