Abstract
Objectives:
A decision tree analysis helps determine the complex characteristics of the groups that are closely connected with specific outcomes. Using a decision tree analysis, the purpose of this secondary analysis was to examine the associations of type II diabetes mellitus (DM) to depressive symptoms among midlife women from four major racial/ethnic groups in the U.S. while identifying the complex characteristics of the women that were closely linked to depressive symptoms.
Methods:
The data from two larger Internet survey studies were used for this analysis. The data from a total of 164 women (62 with type II diabetes and 102 without diabetes) were included. The data were collected using several instruments to measure background characteristics, health and menopausal status, and depressive symptoms (the Depression Index for Midlife Women). The data analysis was conducted using independent t-tests, Mann-Whitney U tests, and decision tree analyses.
Results:
The total numbers and total severity scores of depressive symptoms were significantly higher in those with DM compared with those without DM (p<.05). There were significant differences in the total numbers and total severity scores of depressive symptoms by menopausal status and race/ethnicity (p<.05). DM was a significant factor that influenced the total severity scores of depressive symptoms among midlife women in peri- or post- menopausal stages who were born outside the U.S. and among midlife women in their pre-menopausal stage (p<.05).
Conclusions:
This study indicated several combined characteristics of midlife women at high risk for depressive symptoms that could provide directions for future interventions.
Keywords: Depressive Symptoms, Diabetes Mellitus, Middle Aged, Women, Menopause
Introduction
Many epidemiologic studies have consistently indicated that depression and type II diabetes mellitus (DM) co-occur about two times as frequently as could be predicted only by chance.1 In a meta-analysis including eleven studies,2 the incidence rate of depression was 24 % higher among those with DM. Furthermore, the association between depression and DM is reportedly bidirectional.3,4 In another meta-analysis, those with depression were found to be at a 37 % increased risk of developing DM after controlling multiple influencing factors.5 In a meta-analysis by Mezuk et al.4, they found that the incident rate of depression increased among those with DM (OR 1.15; 95 % CI 1.02–1.30).
Menopausal transition could add another dimension to the associations between DM and depressive symptoms. Indeed, researchers have reported that the prevalence rate of DM goes up during women’s menopausal transition.3 Menopause has been reported as an important time point for changes in many aspects of midlife women’s life.1 A major physiological change during women’s menopausal transition is hormonal changes (estrogen and progesterone),2 which results in changes in their glucose metabolism and insulin sensitivity.3 Menopausal hormonal changes, especially in changes in estrogen and progesterone, could affect the responses of cells to insulin,3 and the hormonal changes subsequently result in changes in blood sugar. Subsequently, menopausal transition uniquely places midlife women at high risk of DM.
The changes in hormones, furthermore, could affect midlife women’s psychological symptoms as well.2, 3 Indeed, depression is one of the most frequently reported symptoms among midlife women during their menopausal transition.6,7 In Freeman et al.’s study,8 those in late menopausal transition had more depressive symptoms compared with pre-menopausal women. Many factors including negative attitudes toward menopausal transition (e.g., concerns about getting ill, worries about getting old, feeling the loss of femininity) were reported to increase the risk of depression among midlife women during menopausal transition.6,7
Despite these findings of the studies on the association of DM to symptoms experienced during the menopausal transition,6,7,9 the associations between DM and depressive symptoms need to be further explored while considering multiple influencing factors. Decision tree analyses are known to be instrumental in determining selective combined characteristics that are directly associated with specific outcomes of interests.10 Thus, a decision tree analysis is frequently used to identify future target groups for an intervention. However, very few studies on the association between DM and depressive symptoms among midlife women have been conducted using a decision tree analysis. For instance, when the PUBMED database was searched without a time limit using keywords of diabetes, depressive symptoms, midlife women, and decision tree, only one article11 was retrieved, but the article was about metabolic syndrome among hypertensive women in the age of menopause.
The purpose of this study was to examine the associations of DM to depressive symptoms among midlife women from four major racial/ethnic groups in the U.S. while considering multiple co-variates and to identify the combined characteristics of the women (including DM) that were closely linked to depressive symptoms. The specific aims were to:
Explore differences in the total numbers and total severity scores of depressive symptoms between midlife women with DM and without DM (Aim 1).
Explore differences in the total numbers and total severity scores of depressive symptoms by menopausal status and race/ethnicity (Aim 2).
Explore the associations of DM to the total numbers and total severity scores of depressive symptoms while considering multiple influencing factors (Aim 3).
Identify the combined characteristics of the women (including DM) that were closed linked to depressive symptoms (Aim 4).
The UCSF symptom management model14 was used to theoretically guide the analysis. The model has three major domains including “person,” “health and illness,” and “environments.” The model has three major concepts including “symptom experience,” “symptom management strategies,” and “outcomes.” In this study, differences in depressive symptoms as “symptom experience” were explored between those with DM and without DM (“health and illness”; Aim 1). Then, differences in depressive symptoms (“symptom experience”) by menopausal status and race/ethnicity were explored (“health and illness” and “person”; Aim 2). Finally, the association between DM (“health and illness”) to depressive symptoms (“symptom experience”) were explored after considering multiple influencing factors (“person,” “health and illness,” and “environments”; Aims 3 and 4).
Methods
This study was approved by the institutional review boards of the researchers’ institutions.
Samples and Settings
For this secondary analysis, the data from two Internet survey studies were used. The parent Internet survey studies aimed to determine racial/ethnic differences in menopausal symptom experience and attitudes toward physical activity among midlife women.15, 16 Among the participants of the two original studies, the cases that met the following criteria were selected for this analysis: midlife women who self-reported as Hispanic, Non-Hispanic (N-H) White, N-H African American or N-H Asian, who were aged between 40 to 60 years, and who could read and write in English. The data with over 10% missing data were excluded. Then, among 1,054 participants who met all the criteria (512 in one study and 542 in the other study), only 164 women (62 with DM and 102 without DM) who answered the questions on DM and depressive symptoms were selected for this analysis. The sample size of 164 was adequate to achieve Aims 1 to 4. Based on the calculations using G-power 3.1.9.4 program, the aims could be addressed with no less than 130 cases with an assumed small effect size of 0.25 (based on the literature12), a power of 90%, and an alpha level of 0.05.
Instruments
The data included in this analysis were collected using multiple measurements on background characteristics, health and menopausal status (including the status of diagnosed DM), and the Depression Index for Midlife Women (DIMW).
Questions on background characteristics and health and menopausal status.
To obtain the data on background characteristics and health and menopausal status, multiple questions were used. Background characteristics included age, marital status, education, employ status, family income, social support, level of acculturation (language, music, foods, customs, and close friends), race/ethnicity, country of birth, number of children, and family income. Health status included body mass index (BMI) and diagnosed diseases, including diabetes. BMI (kg/m2) was classified by the Centers for Disease Control and Prevention (CDC)’s guidelines: normal (18.5–24.9 kg/m2); overweight (25.0–29.9 kg/m2); and obese (≥30.0 kg/m2). Menopausal status was decided using seven questions on the last menstrual cycle, menstrual regularity, and menstrual flow. Those who had their menstruation in the past 3 months with no change in regularity were considered as pre-menopausal. Those who had their menstrual bleeding in the past 3 months with increased changes in cycle length over the past year were considered as early peri-menopausal. Those who had their menstruation in the past 12 months but not in the past 3 months were considered as late peri-menopausal. In this study, early and late peri-menopausal women were lumped into one peri-menopausal group because of small numbers of participants in each category. Those with no menstruation in the past year were considered as post-menopausal.
The Depression Index for Midlife Women (DIMW).
To measure depressive symptoms, the DIMW was used. The DIMW is a subscale of the Midlife Women’s Symptom Index (MSI).13 The MSI has 73 items on physical, psychological, and psychosomatic symptoms that midlife women could experience during their menopausal transition. The DIMW was developed by reviewing the signs and symptoms of depression from the National Institutes of Mental Health document.14 A total of 17 items of the MSI were adopted for the DIMW because they were the signs and symptoms of depression. Each item of the DIMW included two parts: (a) a prevalence part on a dichotomous scale (1 = yes; 0 = no) and (b) a severity part on a 6-point Likert scale (0 = no symptom ~ 5 = extremely). For data analyses, the total numbers and the total severity scores of depressive symptoms were calculated by adding all items (ranged 0~17) and by adding the severity scores of all 17 items (ranged 0~85), respectively. Higher total numbers and higher total severity scores meant more prevalent and more severe symptoms. Cronbach’s alphas of the DIMW in this study were .89 (the prevalence part) and .92 (for the severity part). All the item-to-total correlations were above .20 among 17 items.
Data Collection Procedures
For the original Internet survey studies, project websites were arranged while following the recommendations by the HIPAA and the SANS/FBI. When a midlife woman stopped by the project websites, she was requested to review the informed consent sheets that were uploaded on the project websites. Then, if she wanted to participate in the study, she was required to consent to participate in the study by clicking “I agree to participate in the study.” After the consent process, she was checked against the inclusion and exclusion criteria. When she met all the criteria, she was directly linked to the Internet survey sites and asked to enter her answers to the questions on the Internet surveys.
Data Analysis
The deidentified data were analyzed using the IBM SPSS (version 26.0) software program (IBM Corporation, Armonk, NY). This secondary analysis excluded the data with over 10% missing data; subsequently, the data from a total of 164 women were included. First, the data on background characteristics, health and menopausal status, and depressive symptoms were analyzed through frequencies, percentages, and other descriptive statistics. Independent t tests were used to assess differences in the total numbers and total severity scores of depressive symptoms by DM (Aim 1). Then, the differences in depressive symptoms by menopausal status and racial/ethnicity were assessed using Mann-Whitney U tests because the sample size in each sub-group was less than 30 (Aim 2). The associations between DM and total numbers and severity scores of depressive symptoms were analyzed using multiple regression analyses. The complex characteristics associated with the total numbers and severity scores of depressive symptoms were identified through decision tree analyses (algorithm = chi-squared automatic interaction detection; Aim 3); background characteristics, health status, and menopausal status were controlled as influencing factors in multiple regression analyses and decision tree analyses. In the decision tree analyses, the following rules were set: the least number of cases was 2% for the parent node and 1% for the child node, and the largest tree depth of the model was 3. The decision tree model was validated through a 10-fold cross-validation. Adjustment for multiple testing was done using Bonferroni method. All the analyses in this study were done with an alpha level of .05.
Results
Background Characteristics and Health and Menopausal Status
Table 1 summarize the participants’ background characteristics and health and menopausal status by DM status. Table 2 summarize the participants’ background characteristics and health and menopausal status by race/ethnicity in those with DM and in those without DM. The average age was 49.9 years (SD=±5.5), and 69.5% of the participants were married or living with a partner. Almost all of them had partial college or higher education (98.2%), 72.6% were employed, and 45.1% did not have difficulties in meeting their essential needs (e.g., housing, foods) with their family income. About 38.4% had poor social support, over 50% were overweight or obese, and over 50% preferred vegetables or fruits to other types of foods. Their race/ethnicity included: Hispanic (26.2%), Asian (24.4%), African American (22.6%), and White (26.8%). About 74.4% were born in the U.S. Their menopausal status was pre-menopausal (19.5%), peri-menopausal (34.8%), and post-menopausal (45.7%). About 53.0% had 1 or 2 children, and 37.8% had a DM diagnosis.
Table 1.
Background characteristics and health and menopausal status by DM Status.
| Total (n=164) | DM | ||||
|---|---|---|---|---|---|
| No (n=102) | Yes (n=62) | t or x2 (p) | |||
| M±SD or n (%) | M±SD or n (%) | M±SD or n (%) | |||
| Age | 49.9±5.5 | 49.2±5.3 | 51.0±5.9 | −2.03 (.044) | |
| Marital status | Single/Non-married/Separated | 50 (30.5) | 28 (27.5) | 22 (35.5) | 1.17 (.279) |
| Married/Partnered | 114 (69.5) | 74 (72.5) | 40 (64.5) | 0.03 (.872) | |
| Education | ≤ High school graduate | 3 (1.8) | 2 (2.0) | 1 (1.6) | |
| ≥ Partial college | 161 (98.2) | 100 (98.0) | 61 (98.4) | ||
| Employment status | No | 45 (27.4) | 31 (30.4) | 14 (22.6) | 1.18 (.277) |
| Yes | 119 (72.6) | 71 (69.6) | 48 (77.4) | ||
| Family incomea | Very hard | 31 (18.9) | 21 (20.6) | 10 (16.1) | 3.65 (.161) |
| Somewhat | 59 (36.0) | 31 (30.4) | 28 (45.2) | ||
| Not hard | 74 (45.1) | 50 (49.0) | 24 (38.7) | ||
| Social supportb | None of time | 22 (13.4) | 13 (12.7) | 9 (14.5) | 0.12 (.990) |
| A little of the time | 41 (25.0) | 26 (25.5) | 15 (24.2) | ||
| Some of the time | 40 (24.4) | 25 (24.5) | 15 (24.2) | ||
| Most of the time | 61 (37.2) | 38 (37.3) | 23 (37.1) | ||
| Body Mass Indexc | Normal | 66 (40.2) | 56 (54.9) | 10 (16.1) | 32.27 (<.001) |
| Overweight | 35 (21.3) | 23 (22.5) | 12 (19.4) | ||
| Obese | 63 (38.4) | 23 (22.5) | 40 (64.5) | ||
| Preferred foods | Vegetables | 49 (29.9) | 35 (34.3) | 14 (22.6) | 4.97 (.291) |
| Fruits | 37 (22.6) | 19 (18.6) | 18 (29.0) | ||
| Grains | 19 (11.6) | 12 (11.8) | 7 (11.3) | ||
| Dairy products | 15 (9.1) | 11 (10.8) | 4 (6.5) | ||
| Meats | 44 (26.8) | 25 (24.5) | 19 (30.6) | ||
| Race/ethnicity | Hispanic | 43 (26.2) | 17 (16.7) | 26 (41.9) | 16.18 (.001) |
| Asian | 40 (24.4) | 65 (31.4) | 8 (12.9) | ||
| African American | 37 (22.6) | 22 (21.6) | 15 (24.2) | ||
| White | 44 (26.8) | 31 (30.4) | 13 (21.0) | ||
| The country of birth | Outside the U.S. | 42 (25.6) | 30 (29.4) | 12 (19.4) | 2.05 (.152) |
| U.S. | 122 (74.4) | 72 (70.6) | 50 (80.6) | ||
| Menopausal statusd | Pre-menopausal | 32 (19.5) | 23 (22.5) | 9 (14.5) | 2.86 (.240) |
| Peri-menopausal | 57 (34.8) | 31 (30.4) | 26 (41.9) | ||
| Post-menopausal | 75 (45.7) | 48 (47.1) | 27 (43.5) | ||
| Number of children | None | 27 (16.5) | 14 (13.7) | 13 (21.0) | 2.07 (.355) |
| 1–2 | 87 (53.0) | 58 (56.9) | 29 (46.8) | ||
| More than 3 | 50 (30.5) | 30 (29.4) | 20 (32.3) | ||
Abbreviations: M=mean; SD=standard deviation; U.S.=United States; DM=diabetes mellitus
Difficulties in meeting the basic needs (e.g., housing, foods, clothes) with family income.
The availability of social support.
Normal=18.5–24.9 kg/m2/ overweight=25.0–29.9 kg/m2/ obese=≥30.0 kg/m2.
Pre-menopausal=those who had their menstruation in the past 3 months with no change in regularity/ Peri-menopausal=those who had their menstrual bleeding in the past 3 months with increased changes in cycle length over the past year and those who had their menstruation in the past 12 months but not in the past 3 months/ post-menopausal=those with no menstruation in the past year.
Table 2.
Background characteristics and health and menopausal status by race/ethnicity in those with DM and those without DM.
| DM | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No (n=102) | Yes (n=62) | |||||||||
| Hispanic (n=17) | Asian (n=32) | African American (n=22) | White (n=31) | X2 (p) | Hispanic (n=26) | Asian (n=8) | African American (n=15) | White (n=13) | X2 (p) | |
| M±SD or n (%) | M±SD or n (%) | |||||||||
| Age | 48.9±4.0 | 49.7±6.3 | 48.3±4.8 | 49.5±5.1 | 59.36 (.499) | 50.0±5.9 | 51.9±5.9 | 50.4±6.6 | 53.2±4.7 | 72.11 (.086) |
| Marital status | ||||||||||
| Single/Non-married/Separated | 8 (47.1) | 3 (9.4) | 9 (40.9) | 8 (25.8) | 10.58 (.014)a | 9 (34.6) | 2 (25.0) | 7 (46.7) | 4 (30.8) | 1.34 (.726) |
| Married/Partnered | 9 (52.9) | 29 (90.6) | 13 (59.1) | 23 (74.2) | 17 (65.4) | 6 (75.0) | 8 (53.3) | 9 (69.2) | ||
| Education | ||||||||||
| ≤ High school graduate | 2 (11.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5.41 (.026)a | 0 (0.0) | 1 (12.5) | 0 (0.0) | 0 (0.0) | 4.53 (.129) |
| ≥ Partial college | 15 (88.2) | 32 (100.0) | 22 (100.0) | 31 (100.0) | 26 (100.0) | 7 (87.5) | 15 (100.0) | 13 (100.0) | ||
| Employment status | ||||||||||
| No | 4 (23.5) | 14 (43.8) | 5 (22.7) | 8 (25.8) | 4.00 (.262) | 4 (15.4) | 3 (37.5) | 3 (20.0) | 4 (30.8) | 2.35 (.504) |
| Yes | 13 (76.5) | 18 (56.2) | 17 (77.3) | 23 (74.2) | 22 (84.6) | 5 (62.5) | 12 (80.0) | 9 (69.2) | ||
| Family incomeb | ||||||||||
| Very hard | 4 (23.5) | 5 (15.6) | 4 (18.2) | 8 (25.8) | 10.13 (.119) | 4 (15.4) | 0 (0.0) | 0 (0.0) | 6 (46.2) | 13.79 (.032)a |
| Somewhat | 6 (35.3) | 6 (18.8) | 5 (22.7) | 14 (45.2) | 13 (50.0) | 4 (50.0) | 7 (46.7) | 4 (30.8) | ||
| Not hard | 7 (41.2) | 21 (65.6) | 13 (59.1) | 9 (29.0) | 9 (34.6) | 4 (50.0) | 8 (53.3) | 3 (23.1) | ||
| Social supportc | ||||||||||
| None of time | 3 (17.6) | 6 (18.8) | 2 (9.1) | 2 (6.5) | 7.86 (.553) | 6 (23.1) | 1 (12.5) | 2 (13.3) | 0 (0.0) | 8.02 (.533) |
| A little of the time | 3 (17.6) | 6 (18.8) | 6 (27.3) | 11 (35.5) | 7 (26.9) | 1 (12.5) | 3 (20.0) | 4 (30.8) | ||
| Some of the time | 6 (35.3) | 9 (28.1) | 3 (13.6) | 7 (22.6) | 3 (11.5) | 2 (25.0) | 5 (33.3) | 5 (38.5) | ||
| Most of the time | 5 (29.4) | 11 (34.4) | 11 (50.0) | 11 (35.5) | 10 (38.5) | 4 (50.0) | 5 (33.3) | 4 (30.8) | ||
| Body Mass Indexd | ||||||||||
| Normal | 7 (41.2) | 26 (81.3) | 7 (31.8) | 16 (51.6) | 18.46 (.004)a | 3 (11.5) | 4 (50.0) | 0 (0.0) | 3 (23.1) | 20.78 (<.001)a |
| Overweight | 4 (23.5) | 5 (15.6) | 7 (31.8) | 7 (22.6) | 5 (19.2) | 3 (37.5) | 0 (0.0) | 4 (30.8) | ||
| Obese | 6 (35.3) | 1 (3.1) | 8 (36.4) | 8 (25.8) | 18 (69.2) | 1 (12.5) | 15 (100.0) | 6 (46.2) | ||
| Preferred foods | ||||||||||
| Vegetables | 5 (29.4) | 16 (50.0) | 5 (22.7) | 9 (29.0) | 12.64 (.379) | 4 (15.4) | 3 (37.5) | 5 (33.3) | 2 (15.4) | 11.85 (.362) |
| Fruits | 2 (11.8) | 6 (18.8) | 3 (13.6) | 8 (25.8) | 10 (38.5) | 1 (12.5) | 1 (6.7) | 6 (46.2) | ||
| Grains | 2 (11.8) | 4 (12.5) | 2 (9.1) | 4 (12.9) | 3 (11.5) | 1 (12.5) | 1 (6.7) | 2 (15.4) | ||
| Dairy products | 4 (23.5) | 2 (6.3) | 3 (13.6) | 2 (6.5) | 1 (3.8) | 3 (37.5) | 2 (13.3) | 1 (7.7) | ||
| Meats | 4 (23.5) | 4 (12.5) | 9 (40.9) | 8 (25.8) | 8 (30.8) | 0 (0.0) | 6 (40.0) | 2 (15.4) | ||
| The country of birth | ||||||||||
| Outside the U.S. | 3 (17.6) | 26 (81.3) | 0 (0.0) | 1 (3.2) | 61.96 (<.001)a | 4 (15.4) | 7 (87.5) | 1 (6.7) | 0 (0.0) | 21.58 (<.001)a |
| U.S. | 14 (82.4) | 6 (18.8) | 22 (100.0) | 30 (96.8) | 22 (84.6) | 1 (12.5) | 14 (93.3) | 13 (100.0) | ||
| Menopausal statuse | ||||||||||
| Pre-menopausal | 3 (17.6) | 6 (18.8) | 5 (22.7) | 9 (29.0) | 31.05 (<.001)a | 4 (15.4) | 0 (0.0) | 3 (20.0) | 2 (15.4) | 10.62 (.078) |
| Peri-menopausal | 8 (47.1) | 0 (0.0) | 13 (59.1) | 10 (32.3) | 10 (38.4) | 1 (12.5) | 6 (40.0) | 9 (69.2) | ||
| Post-menopausal | 6 (35.3) | 26 (81.2) | 4 (18.2) | 12 (38.7) | 12 (46.2) | 7 (87.5) | 6 (40.0) | 2 (15.4) | ||
| Number of children | ||||||||||
| None | 5 (29.4) | 1 (3.1) | 5 (22.7) | 3 (9.7) | 14.09 (.022)a | 5 (19.2) | 2 (25.0) | 4 (26.7) | 2 (15.4) | 2.81 (.866) |
| 1–2 | 6 (35.3) | 23 (71.9) | 8 (36.4) | 21 (67.7) | 11 (42.3) | 5 (62.5) | 7 (46.6) | 6 (46.2) | ||
| More than 3 | 6 (35.3) | 8 (25.0) | 9 (40.9) | 7 (22.6) | 10 (38.5) | 1 (12.5) | 4 (26.7) | 5 (38.4) | ||
p<.05
Difficulties in meeting the basic needs (e.g., housing, foods, clothes) with family income.
The availability of social support.
Normal=18.5–24.9 kg/m2/ overweight=25.0–29.9 kg/m2/ obese=≥30.0 kg/m2.
Pre-menopausal=those who had their menstruation in the past 3 months with no change in regularity/ Peri-menopausal=those who had their menstrual bleeding in the past 3 months with increased changes in cycle length over the past year and those who had their menstruation in the past 12 months but not in the past 3 months/ post-menopausal=those with no menstruation in the past year.
Differences in Depressive Symptoms by DM (Aim 1)
The average total numbers of depressive symptoms were 6.2 (SD=±4.8) in total sample, 7.3 (SD=±4.6) in those with DM, and 5.5 (SD=±4.8) in those without DM. The average total severity scores of depressive symptoms were 19.4 (SD=±17.2) in total sample, 24.3 (SD=±17.3) in those with DM, and 16.4 (SD=±16.6) in those without DM. Those with DM had significantly higher total numbers of depressive symptoms than those without DM (t=−2.39, p = .018). Those with DM had significantly higher total severity scores of depressive symptoms than those without DM (t=−2.90, p = .004).
Differences in Depressive Symptoms by Menopausal Status (Aim 2)
The differences in the total numbers and total severity scores of depressive symptoms between those with DM and without DM by menopausal status are summarized in Table 3. Among post-menopausal women, those with DM had significantly higher total numbers of depressive symptoms than those without DM (U = 466.50, p = .045). Among pre-menopausal (U = 57.00, p = .047) and post-menopausal women (U = 414.50, p = .010), those with DM had significantly higher total severity scores of depressive symptoms than those without DM.
Table 3.
Differences in depressive symptoms between those with DM and those without DM by menopausal status and race/ethnicity.
| Total Numbers | Total Severity Scores | |||||
|---|---|---|---|---|---|---|
| n, M±SD | n, M±SD | n, M±SD | n, M±SD | |||
| Menopausal Stautsb | ||||||
| Pre-menopausal | 23, 1.2±1.2 | 9, 2.4±2.5 | 68.50 (.145) | 23, 2.5±2.4 | 9, 8.2±9.1 | 57.00 (.047)a |
| Peri-menopausal | 31, 6.7±3.2 | 26, 6.7±3.5 | 400.50 (.968) | 31, 19.6±10.7 | 26, 20.7±12.2 | 382.00 (.736) |
| Post-menopausal | 48, 6.8±5.5 | 27, 9.5±4.8 | 466.50 (.045)a | 48, 21.1±19.8 | 27, 33.1±18.6 | 414.50 (.010)a |
| Race/Ethnicity | ||||||
| Hispanic | 17, 6.1±4.8 | 26, 8.0±4.6 | 167.50 (.183) | 17, 17.6±15.2 | 26, 26.7±19.2 | 155.00 (.101) |
| Asian | 32, 3.1±3.5 | 8, 8.3±5.5 | 63.00 (.026)a | 32, 8.0±9.9 | 8, 27.4±19.1 | 60.50 (.022)a |
| African American | 22, 6.3±4.3 | 15, 6.0±4.1 | 157.50 (.815) | 22, 19.2±15.8 | 15, 19.3±12.9 | 157.00 (.804) |
| White | 31, 7.0±5.5 | 13, 6.8±4.6 | 199.50 (.959) | 31, 22.5±20.2 | 13, 23.4±17.1 | 186.50 (.699) |
Abbreviations: M=mean; SD=standard deviation; DM=diabetes mellitus
p<.05
Pre-menopausal=those who had their menstruation in the past 3 months with no change in regularity/ Peri-menopausal=those who had their menstrual bleeding in the past 3 months with increased changes in cycle length over the past year and those who had their menstruation in the past 12 months but not in the past 3 months/ post-menopausal=those with no menstruation in the past year.
Differences in Depressive Symptoms by Racial/ethnicity (Aim 2)
The differences in the total numbers and total severity scores of depressive symptoms between those with DM and without DM by race/ethnicity are summarized in Table 3. Only among Asian women, those with DM had significantly higher total numbers (U=63.00, p=.026) and total severity scores (U=60.50, p=.022) of depressive symptoms than those without DM.
Factors Associated with Total Numbers and Total Severity Scores of Depressive Symptoms (Aim 3)
Menopausal status and country of birth were significantly associated with total numbers and total severity scores of depressive symptoms (p<.001). DM was significantly associated with the total severity scores of depressive symptoms (ß=.16, p=.026) (Table 4).
Table 4.
Factors associated with the total numbers and total severity scores of depressive symptoms.
| Numbers | Severity Scores | |||
|---|---|---|---|---|
| ß | p | ß | p | |
| Age | −.06 | .406 | −.03 | .684 |
| Marital status (ref: married/partnered) | ||||
| Single/Non-married/Separated | .04 | .612 | .04 | .579 |
| Education (ref: ≥ partial college) | ||||
| ≤ High school graduate | .13 | .054 | .06 | .350 |
| Employment status (ref: yes) | ||||
| No | −.03 | .676 | .01 | .920 |
| Family income (ref: not hard) | ||||
| Somewhat | .02 | .793 | .07 | .365 |
| Very hard | .05 | .502 | .08 | .293 |
| Social support (ref: most of the time) | ||||
| None of time | .02 | .784 | .03 | .724 |
| A little of the time | .15 | .056 | .13 | .086 |
| Some of the time | −.03 | .675 | −.01 | .909 |
| Body Mass Index (ref: normal) | ||||
| Overweight | .01 | .939 | .01 | .849 |
| Obese | −.05 | .602 | −.04 | .658 |
| Preferred foods (ref: vegetables) | ||||
| Fruits | .02 | .826 | .03 | .691 |
| Grains | −.13 | .082 | −.12 | .113 |
| Dairy products | .04 | .554 | .07 | .335 |
| Meats | .04 | .572 | .03 | .683 |
| Race/ethnicity (ref: Hispanic) | ||||
| Asian | −.08 | .482 | −.10 | .391 |
| African American | −.39 | .699 | −.02 | .806 |
| White | .46 | .645 | .05 | .551 |
| The country of birth (ref: outside the U.S.) | ||||
| U.S. | .41 | .002b | .40 | .002b |
| Menopausal status (ref: pre-menopausal) | ||||
| Peri-menopausal | .43 | <.001c | .34 | <.001c |
| Post-menopausal | .87 | <.001c | .85 | <.001c |
| Number of children (ref: none) | ||||
| 1–2 | .01 | .952 | −.02 | .820 |
| More than 3 | .01 | .931 | −.04 | .678 |
| DM (ref: no) | ||||
| Yes | .13 | .076 | .16 | .026a |
| Adjusted R2 | .39 | .39 | ||
| p | <.001 | <.001 | ||
Abbreviations: U.S.=United States; DM=diabetes mellitus
p<.05,
p<.005,
p<.001
Combined Characteristics Associated with Total Numbers of Depressive Symptoms (Aim 4)
Figure 1 illustrates the findings on the combined characteristics that influenced the total numbers of depressive symptoms from the decision tree analyses. The mean total number of depressive symptoms was 6.2 (SD=±4.8; Node 0). Through the decision tree analyses, the following three groups were identified to have higher total numbers of depressive symptoms than the mean total numbers. First, those who were in their post- or peri-menopausal status, Asian, and single/non-married/separated had higher total numbers of depressive symptoms than the mean number (Node 8; M=11.3, SD= ±3.8). Second, those in their post-menopausal status who were African American, Hispanic or White had higher total numbers than the mean total number (Node 5; M=10.4, SD=±4.7). Finally, those in their peri-menopausal status who were African American, Hispanic or White had higher total numbers than the mean total number (Node 6; M=6.6, SD=±3.2). In other words, in the decision tree analyses, DM was not a significant factor that influenced the total numbers of depressive symptoms (p<.050). All the variables that were shown on the decision tree (see Figure 1) were statistically significant factors influencing the total numbers of depressive symptoms (p<.050).
Figure 1.
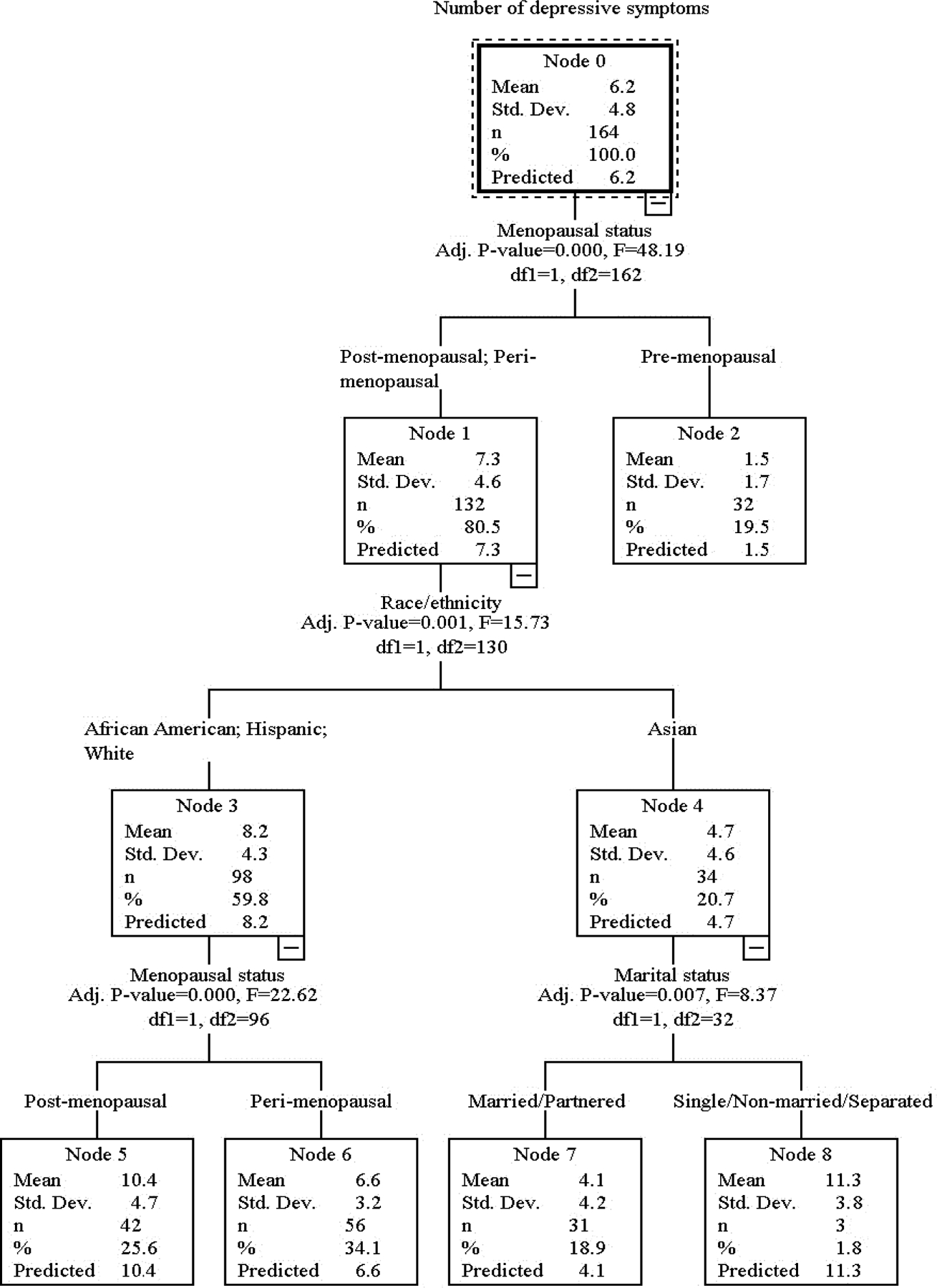
The decision tree on the total number of depressive symptoms.
Combined Characteristics Associated with Total Severity Scores of Depressive Symptoms (Aim 3)
Figure 2 illustrates the findings on the combined characteristics that influenced the total severity scores of depressive symptoms from the decision tree analyses. The mean total severity score of depressive symptom was 19.4 (SD=±17.2; Node 0). Through the decision tree analyses, the following three groups were identified to have higher total severity scores of depressive symptoms than the mean total severity score. First, those in their post-menopausal status who were born in the U.S. had higher total severity scores of depressive symptoms (Node 7; M=37.5, SD=±18.4) than the mean total severity score. Second, those in post- or peri-menopausal status who were born outside the U.S. and had the diagnosis of DM had higher total severity scores of depressive symptoms (Node 9; M= 30.5, SD=±18.8) than the mean total severity score. Third, those in peri-menopausal status who were born in the U.S. had higher total severity scores of depressive symptoms (Node 8; M=20.1, SD=±11.3) than the mean total severity score. In other words, in the decision tree analyses, DM was a significant factor that influenced the total severity scores of depressive symptoms among midlife women in peri- or post- menopausal stages who were born outside the U.S. and among midlife women in their pre-menopausal stage (p<.050). All the variables that were shown on the decision tree (see Figure 2) were statistically significant factors influencing the total severity scores of depressive symptoms (p<.050).
Figure 2.
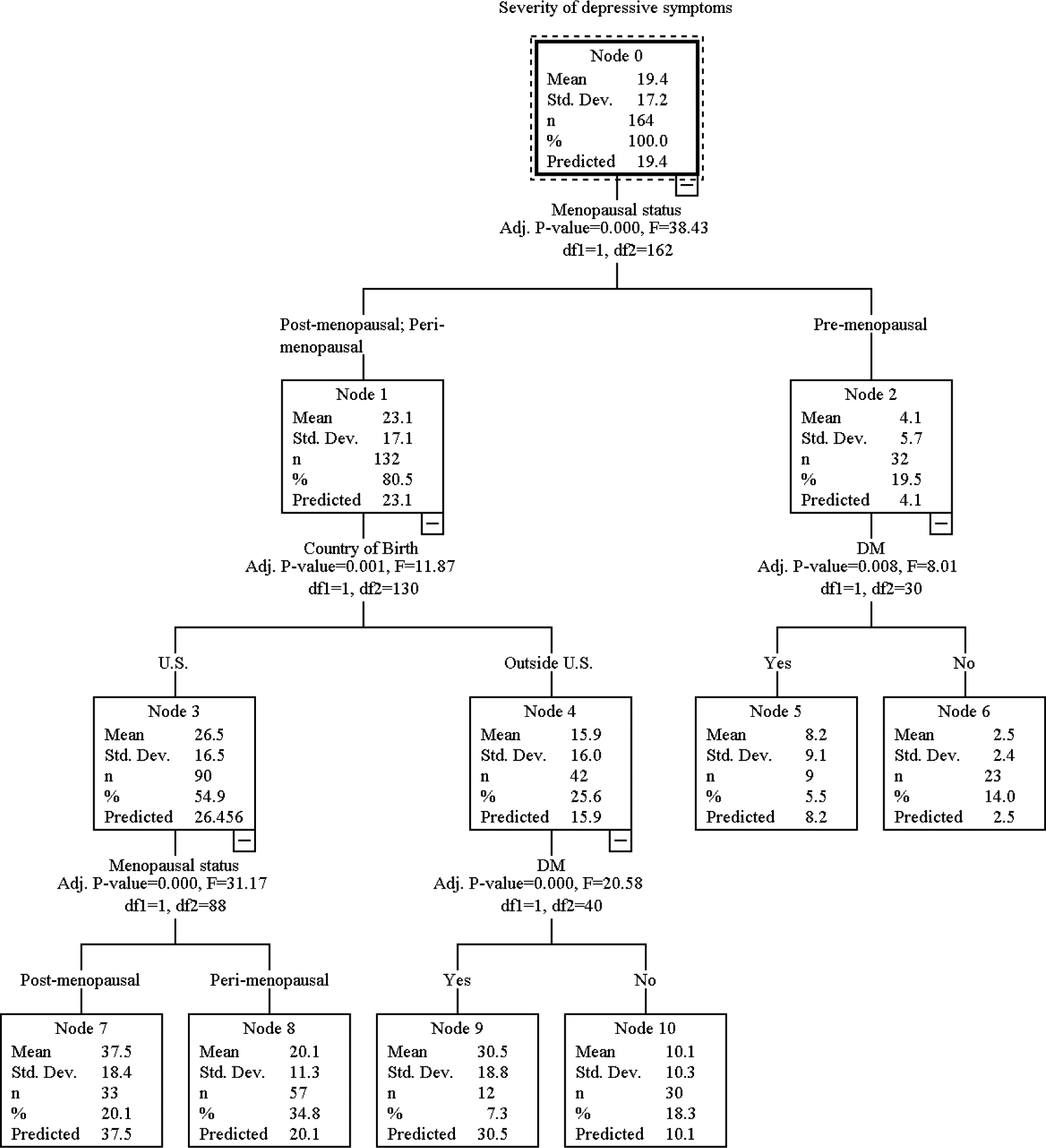
The decision tree on the total severity scores of depressive symptoms.
Discussion
This study indicated significant associations between DM and depressive symptoms among four racial/ethnic groups of midlife women in the U.S. Midlife women with DM had higher total numbers and total severity scores of depressive symptoms compared with those without DM (Aim 1). Among midlife women who were in their post-menopausal stage, those with DM had significantly higher total numbers of depressive symptoms than those without DM (Aim 2). Among those who were in their peri-menopausal and post-menopausal stages, those with DM reported higher total severity scores of depressive symptoms than those without DM (Aim 2). Only among Asian midlife women, those with DM had higher total numbers and total severity scores of depressive symptoms compared with those without DM (Aim 2). The multivariable-adjusted analyses indicated that DM was significantly associated with the total severity scores of depressive symptoms (Aim 3). After considering multiple factors influencing depressive symptoms of midlife women, decision tree analyses indicated specific combined characteristics of midlife women who had higher total numbers and total severity scores of depressive symptoms than the mean total number and mean total severity score (Aim 4).
The finding that midlife women with DM had higher total numbers and total severity scores of depressive symptoms than those without DM is consistent with the current literature on the associations of DM to depressive symptoms. Studies supported that the incidence rate of depression was higher in those with DM compared with those without DM,2 and depressive symptoms were linked to an increased risk of DM.15 As mentioned above, the literature suggested bidirectional relationships between DM and depression.3,4,16 Yet, in this secondary analysis, the direction of the relationship between DM and depressive symptoms could not be determined because this was a secondary analysis of the data that were collected through two cross-sectional studies.
The finding that there were significant differences in the total numbers and total severity scores of depressive symptoms by menopausal status also agrees with the current literature. As mentioned above, the relationships between DM and depressive symptoms could be significantly influenced by menopausal transition; the incidence rate of DM increases in midlife women during their menopausal transition.3 Indeed, menopausal transition brings about drastic changes in many aspects of daily life.1 The changes include hormonal changes (estrogen and progesterone)2 and subsequent changes in glucose metabolism and insulin sensitivity.3 As mentioned above, these changes are known to influence cells’ responses to insulin3 and changes in blood sugar, which uniquely increases the risk of DM among midlife women. Furthermore, these changes influence psychological symptoms of midlife women,2, 3 including depressive symptoms.6,7 The literature supported that those in postmenopausal stage had higher prevalence rate of depressive symptoms compared with those in pre-menopausal stage.8 The findings from this analysis were consistent with all these findings in the literature.
The finding that the differences in depressive symptoms between those with DM and those without DM existed only in Asian midlife women has rarely been reported in the literature. The literature indicated that Asian women were less likely to have psychological symptoms during their menopausal transition compared with other racial/ethnic groups.17–20 Also, Asian populations in general reportedly had the stigma attached to psychological symptoms including depressive symptoms, which frequently made them underreport their psychological symptoms.21–25 Thus, one plausible reason for this finding would be: although Asian midlife women in general are less likely to report their psychological symptoms during menopausal transition,17–20 Asian midlife women with DM might feel more comfortable to report their depressive symptoms due to their diagnosed physical disease (DM). The literature indicated that Asians tended to express psychological distress as physical complaints, and they tended to be more comfortable about reporting their physical complaints than psychological complaints.26,27 Yet, this finding might have occurred by chance.
Decision tree analyses could give directions for development of future interventions by determining specific combinations of variables that needed to be considered in deciding the target groups of the interventions.10 Decision tree analyses also help determine the mechanisms through which various factors affect the outcome(s) of interests by producing “the rules for inferences” that could connect “parent nodes” to “child nodes.”10 Thus, the findings from the decision tree analyses could help identify target groups of planned interventions. In the decision tree analyses, DM was a significant factor that influenced the total severity scores of depressive symptoms among those in their peri- or post-menopausal stages who were born outside the U.S. Also, in the decision tree analyses, DM was a significant factor that influenced the total severity scores of depressive symptoms among those in their pre-menopausal stage. Thus, the diagnosis of DM needs to be considered in development of interventions to decrease the severity of depressive symptoms among these two specific groups of midlife women.
The findings from the decision tree analyses supported that future interventions to reduce the total numbers of depressive symptoms would need to target three specific groups: (a) midlife women in their post- or peri-menopausal stages who are Asian and single/non-married/separated; (b) midlife women in their post-menopausal stage who are African American, Hispanic or White; and (c) midlife women in their peri-menopausal stage who are African American, Hispanic or White. The findings from the decision tree analyses also supported that future interventions to reduce the total severity scores of depressive symptoms would need to target three specific groups: (a) midlife women in their post-menopausal stage who are born in the U.S.; (b) midlife women in their post- or peri-menopausal stage who are born outside the U.S. and have the diagnosis of DM; and (c) midlife women in their peri-menopausal stage who are born in the U.S. However, in the literature, virtually none is known about these specific findings mainly due to a lack of studies on depressive symptoms of midlife women using a decision tree analysis.
There were several limitations in this study. First of all, the sample size and variables were pre-determined because the data from the parent studies were secondarily analyzed. Second, there were only eight Asian women with DM, which would require a careful interpretation of the findings related to Asian women. Third, the findings for Aims 1 and 2 were from unadjusted analyses. Fourth, there existed potential selection bias because the participants of the parent studies were required to have access to the Internet. Fifth, no objective validation of the self-reported data was obtained. Finally, the causality between DM and depressive symptoms could not be determined because the parent studies were cross-sectional studies.
Conclusions
This study indicated significant associations between DM and depressive symptoms among four racial/ethnic groups of midlife women in the U.S. Based on the findings, the following suggestions are made for future research and practice. First of all, further longitudinal studies with larger samples are necessary to confirm the findings reported in this study and to determine potential causal associations between DM and depressive symptoms. As described above, this study had some limitations because this was a secondary analysis, and the data came from two cross-sectional studies. Second, the differences in depressive symptoms between those with DM and those without DM need to be further investigated in individual racial/ethnic groups. As discussed, the differences were identified only among Asian women. Third, more investigations are also essential in determining the associations of multiple co-variates to depressive symptoms of midlife women with DM because the variables included in this study were pre-determined by the parent studies. Finally, the association between DM and depressive symptoms needs to be considered in future practice with midlife women while considering multiple influencing factors. Depressive symptoms need to be closely assessed when working with midlife women with DM, and some strategies to manage depressive symptoms need to be provided to midlife women with DM while considering multiple influencing factors including menopausal status, race/ethnicity, marital status, and the country of birth.
Supplementary Material
Sources of Funding:
This is a secondary analysis of the quantitative data from two larger studies that were funded by the National Institute of Health (NIH/NINR/NIA, 1R01NR008926 and NIH/NINR/ NHLBI, R01NR010568).
Footnotes
Financial Disclosures/Conflict of Interest: None reported.
References
- 1.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–1078. 10.2337/diacare.24.6.1069 [DOI] [PubMed] [Google Scholar]
- 2.Nouwen A, Winkley K, Twisk J, et al. European Depression in Diabetes (EDID) Research Consortium. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53(12):2480–2486. 10.1007/s00125-010-1874-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Golden SH, Lazo M, Carnethon M, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299(23):2751–2759. 10.1001/jama.299.23.2751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31(12):2383–2390. 10.2337/dc08-0985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knol MJ, Twisk JWR, Beekman ATF, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49(5):837–845. 10.1007/s00125-006-0159-x [DOI] [PubMed] [Google Scholar]
- 6.Judd FK, Hickey M, Bryant C. Depression and midlife: are we overpathologising the menopause? J Affect Disord. 2012;136(3):199–211. 10.1016/j.jad.2010.12.010 [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29(2–3):85–96. [DOI] [PubMed] [Google Scholar]
- 8.Freeman EW, Sammel MD, Liu L, Gracia CR, Nelson DB, Hollander L. Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry. 2004;61(1):62–70. 10.1001/archpsyc.61.1.62 [DOI] [PubMed] [Google Scholar]
- 9.NIMH. Depression. Available at: https://www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed October 24, 2020.
- 10.Arroyo C, Hu FB, Ryan LM, et al. Depressive Symptoms and Risk of Type 2 Diabetes in Women. Diabetes Care. 2004;27(1):129–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sartorius N Depression and diabetes. Dialogues Clin Neurosci. 2018;20(1):47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Avis NE, Stellato R, Crawford S, et al. Is there a menopausal syndrome? Menopausal status and symptoms across racial/ethnic groups. Soc Sci Med 1982. 2001;52(3):345–356. [DOI] [PubMed] [Google Scholar]
- 13.Im E-O, Lee BI, Chee W, Dormire S, Brown A. A National Multiethnic Online Forum Study on Menopausal Symptom Experience. Nurs Res. 2010;59(1):26–33. 10.1097/NNR.0b013e3181c3bd69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Im E-O, Lee B, Chee W, Brown A, Dormire S. Menopausal Symptoms Among Four Major Ethnic Groups in the U.S. West J Nurs Res. 2010;32(4):540–565. 10.1177/0193945909354343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Im E-O. Symptoms experienced during menopausal transition: Korean women in South Korea and the United States. J Transcult Nurs. 2003;14(4):321–328. [DOI] [PubMed] [Google Scholar]
- 16.Augsberger A, Yeung A, Dougher M, Hahm HC. Factors influencing the underutilization of mental health services among Asian American women with a history of depression and suicide. BMC Health Serv Res. 2015;15:542. 10.1186/s12913-015-1191-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernstein KS, Park S-Y, Shin J, Cho S, Park Y. Acculturation, discrimination and depressive symptoms among Korean immigrants in New York City. Community Ment Health J. 2011;47(1):24–34. 10.1007/s10597-009-9261-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park S-Y, Bernstein KS. Depression and Korean American immigrants. Arch Psychiatr Nurs. 2008;22(1):12–19. 10.1016/j.apnu.2007.06.011 [DOI] [PubMed] [Google Scholar]
- 19.Lee HB, Han H-R, Huh B-Y, Kim KB, Kim MT. Mental health service utilization among Korean elders in Korean churches: preliminary findings from the Memory and Aging Study of Koreans in Maryland (MASK-MD). Aging Ment Health. 2014;18(1):102–109. 10.1080/13607863.2013.814099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen JA, Hung GC-L, Parkin S, Fava M, Yeung AS. Illness beliefs of Chinese American immigrants with major depressive disorder in a primary care setting. Asian J Psychiatry. 2015;13:16–22. 10.1016/j.ajp.2014.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kamiński B, Jakubczyk M, Szufel P. A framework for sensitivity analysis of decision trees. Cent Eur J Oper Res. 2018;26(1):135–159. 10.1007/s10100-017-0479-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


