Abstract
Chronic wound pain is not well understood and the literature is limited. Six of 10 patients venous leg ulcer experience pain with their ulcer, and similar trends are observed for other chronic wounds. Chronic wound pain can lead to depression and the feeling of constant tiredness. Pain related to the wound should be handled as one of the main priorities in chronic wound management together with addressing the cause. Management of pain in chronic wounds depends on proper assessment, reporting and documenting patient experiences of pain. Assessment should be based on six critical dimensions of the pain experience: location, duration, intensity, quality, onset and impact on activities of daily living. Holistic management must be based on a safe and effective mix of psychosocial approaches together with local and systemic pain management. It is no longer acceptable to ignore or inadequately document persistent wound pain and not to develop a treatment and monitoring strategy to improve the lives of persons with chronic wounds. Unless wound pain is optimally managed, patient suffering and costs to health care systems will increase.
Keywords: Holistic management, Local management, Non‐pharmacological methods, Pharmacological wound pain management, Wound pain, Wound pain assessment, Wound pain model
Introduction
In recent years, there has been growing evidence that the experience of living with a chronic wound has a huge impact on a patient’s quality of life 1, 2, 3. One of the consistent findings, particularly in the qualitative work that has been completed, is that pain is one of the symptoms that patients find particularly distressing 4, 5, 6.
A recent study in Canada suggests that the prevalence of pain in patients with venous predominant or mixed venous and arterial ulcers is approximately 50%, with over 50% of these using analgesia as part of their treatment (7). Similar figures have been reported in other studies of leg ulceration 8, 9 as well as in other chronic wound types (Table 1). Health professionals are now starting to recognise the importance of addressing the issue of wound pain, as evidenced by the European Wound Management Association Position Document on pain (10), the dedication of a supplement of Ostomy Wound Management to this topic (April 2003; 11, 12, 13) and the Consensus Document on Minimising Pain at Wound dressing‐related procedures launched at the World Union of Wound Healing Societies meeting (July 2004; 12).
Table 1.
Prevalence studies on leg ulcers including observations on pain and its intensity (PubMed, Cinahl and EMBASE, search concluded by May 2006)
| Author | Wounds types | Investigations | Methods | Participants | Main outcomes |
|---|---|---|---|---|---|
| Ebbeskog et al., 1996 (38) | Leg and foot | Study of demographics of leg ulcer patients in Sweden | Survey, questionnaire | Physicians and nurses completed questionnaires on 294 patients | Leg and foot ulcer prevalence of 0·12%; 92% patients >65 years; 42% venous ulcers (highest prevalence); pain reported by patients: 47% venous; 80% arterial ulcer; 94% mixed ulcer; 48% diabetic ulcer; 51% other ulcer; combined all day and dressing change pain |
| Noonan and Burge 1998 (9) | Venous leg ulcer | Measurement of pain | Nurses interviewing patients; ulcer measurements, pain assessment with Visual Analogue Scale and Visual Rating Scale | 38 venous; 10 arterial ulcer patients | Temporary pain (dressing change): venous 87%; arterial 100%; mixed 86%. Persistent pain: venous 68%; arterial 100%; mixed 71%. 57% patients felt anger about the pain; standing exacerbated pain for all patients; pain disturbed sleep for most patients |
| Hofman et al., 1997 (8) | Venous leg ulcers | Assessment of prevalence, and pain | Prospective study, pain only analysed in venous group as other wound aetiologies were too small in sample size | 140 patients | 64% of venous patients reported 4/5 out of 5 pain; 38% had continuous pain; 64% reported sleep disturbance; 26% had atrophy blanche; periulcer pain was associated with maceration; 61% had pain in ulcer; 43% had pain around the ulcer; 46% had pain elsewhere; 30 out of 37 patients prescribed morphine still had pain of 4 to 5 out of 5 |
| Lindholm et al., 1999 (39) | Chronic wounds and demographics | Study of demographics of leg ulcer patients in Sweden | Survey; structured questionnaire | Physicians and nurses completed questionnaires regarding 694 patients | • Prevalence: leg ulcers (0·14%); pressure ulcers (0·06%) and other wounds (0·04%); pain :48% leg ulcer patients; 46% foot ulcer patients; 37% pressure ulcer patients; 82% arterial patients; 39% venous disease; 24% of type I persons with diabetes; 30% of type II persons with diabetes; 87% of the older adult pressure ulcer patients (80–89 years) |
| Hollinworth and Colllier, 2000 (40) | Chronic leg ulcers | Survey | Questionnaire survey among nurses | 373 nurses returned questionnaires | • Practitioners main consideration: 47% prevention of trauma to the wound; 37% avoiding patient pain; other concerns 16% |
| Charles et al., 2002 (41) | Venous ulcers | Compression bandaging; hydrocolloid dressing evaluation | Clinical trial; 12‐week treatment | 65 patients | 71% of patients had ulcer‐associated pain; 2 weeks with compression bandaging reduced pain to half its entry level; no difference in pain with different dressings |
| Margolis et al., 2002 (42) | Venous leg ulcers | Database analysis | Analysis of general practice databases, UK | 6% of the general practitioners in UK; >65 years; 50 000 eligible for analysis | 1·69% >65 had venous leg ulcers at least one time per year. 1·2 new incidence rate per 100 person years; incidence increased with increasing age |
| Nemeth et al., 2003 (7) | Venous and mixed aetiology | Prevalence measurement | Nurse interviews, cross‐sectional design, three times 1 week, numeric rating scale | 255 participants | 48–55% pain prevalence in venous leg ulcers; pain in all wounds not related to hard‐to‐heal wounds; individuals with pain statistically significant: ↑ osteoarthritis, ↑ foot ulcers, ↓ time of attendance at a leg ulcer service, ↓ SF‐12 mental health component score |
| Nemeth et al., 2004 (43) | Venous leg ulcers | Tracking pain related to compression bandaging | Nurses interviewing patients, pain measurement with numeric rating scale, and short form McGill | 20 patients with venous disease | 85% reported pain at admission; 81% still felt pain after 5 weeks of compression bandaging, but of less severity |
| Goncalves et al., 2004 (44) | Chronic leg ulcers | Describe pain characteristics | Nurse interviews, McGill pain descriptors | 90 patients; mainly of venous origin (87%) | 100% of venous leg ulcer patients had pain; pain descriptors: 83% throb‐bing; 78% drilling; 72% burning; 70% stabbing; evaluative descriptors: 66% nagging; 60% tiring; 50% troublesome |
Few professionals would disagree that decisions regarding patient care should include a strong focus on the management of pain in order to relieve patient suffering. However, effective pain management depends on detailed and accurate assessment and documentation of the patient’s pain experience. The authors have developed a Wound Pain Management Model (WPMM) to assist health care professionals to incorporate wound pain assessment and management into the holistic management of patients with chronic wounds. The first sections of the model place the assessment and management of pain into the context of important aspects of chronic wound management, such as accurate diagnosis and appropriate local wound management. This article concentrates on wound pain assessment and treatment strategies, focusing on persistent chronic pain and on the pain associated with local wound treatment including dressing change.
Wound pain management model
The WPMM (Figure 1) starts from the basic premise that all wounds are painful until proven otherwise (12) but begins by emphasising the importance of good wound assessment leading to accurate wound diagnosis to assist in ensuring that fundamental aspects of underlying pathology are addressed. In addition, many aspects of local wound management, if dealt with swiftly and appropriately, can lead to a reduction in the patient’s pain experience, for example, resolution of infection or reduction in inflammation. Many of these issues are covered comprehensively in the literature 14, 15 and are outside the scope of this study. The focus for the remaining text will be on differentiation of the types of wound pain, wound pain assessment and holistic approaches to wound pain management.
Figure 1.
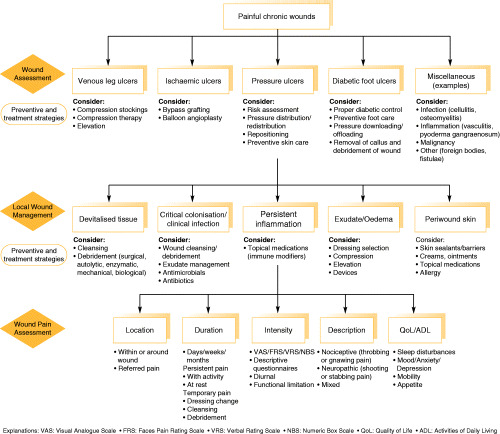
The Wound Pain Management Model is a guide on wound pain assessment and management. The guide consists of four levels that need to be considered simultaneously in order to prevent and treat painful chronic wounds properly. It is therefore recommended to assess and treat both the wound and the pain at the same time.
Types of wound pain
In 1979, the subcommittee for taxonomy of the International Association for the Study of Pain drafted a definition of pain as ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’(11). This definition clearly covers both physical and emotional components of the pain experience and reflects the currently held belief that personal perception mediates the experience of pain, reflected in the definition that ‘pain is what the patient says it is’(16). The need for a universally agreed definition of pain was not just an academic exercise; this definition of pain led to calls for changes in treatment and created pressure to treat pain as a symptom or disorder in its own right. It also highlighted the need to be clear about the different types of pain that patients experience, and the language that we use to describe such pain. Many authors concentrate on distinguishing between ‘acute’ and ‘chronic’ pain 17, 18.
The primary function of acute pain is to warn of injury and prevent tissue damage such as mechanical, thermal and chemical injuries. This is referred to as nociceptive pain. When harmful inputs decrease, pain is usually relieved. Chronic pain differs as it involves both physical and emotional components and is rarely an indication of ongoing damage 18, 19. A wound represents a loss of skin integrity and cut nerve fibres, therefore the resulting pain is due to a combination of nociceptive pain and pain caused by nerve damage (neuropathic pain).
Nociceptive pain has been defined as an appropriate physiological response to a painful stimulus, while neuropathic pain has been defined as an inappropriate response caused by a primary lesion or dysfunction in the nervous system (11). The clinician must be aware that there is a physical and an emotional component of pain. For treatment of the physical component, pain can be divided into nociceptive and/or neuropathic pain as indicated in Table 2. The emotional component of nociceptive and neuropathic pain is comparable and therefore the treatment is similar (20). Both types of pain are most usually seen in combination in patients experiencing chronic wound pain.
Table 2.
Characteristics of nociceptive and neuropathic pain
The World Union of Wound Healing Society’s consensus document describes different elements of the pain experience in terms of ‘operative’, ‘incident’, ‘procedural’ and ‘background’ pain to distinguish the differing parts of the experience of wound pain (12). The debate about the terms used can lead to confusion for the non expert practitioner in the wound care arena. In order to distinguish between the chronic aspects of the wound and the chronic aspects of the pain experience, the WPMM uses the terms ‘temporary’ and ‘persistent’ to clearly differentiate the temporal aspects of the pain experience (in the pain literature, the term ‘chronic pain’ may be used for ‘persistent pain’). These terms may be useful for health professionals at all levels to comprehend and discuss the pain experience with a person with chronic wound, and are outlined in the WPMM in Figure 1.
This conceptualisation incorporates both the ground‐breaking work already completed on patients’ and practitioners’ concerns about experiences of pain at dressing change (21) and research that has shown that wound pain can be persistent (22), with fluctuating bursts of temporary pain at any time (23).
Assessment of wound pain
If wound pain is not assessed and documented, it may be ignored and/or not addressed properly (24). It is important to remember that increased wound pain may be an indicator of wound complications that need treatment and therefore practitioners must constantly reassess the wound as well as the associated pain. The WPMM outlines areas that are important for wound pain assessment including the location, intensity and duration of the pain, as well as listening to the ways in which patients describe their pain and the impact the pain experience has on their activities of daily living. Table 3 outlines a series of questions, together with an explanation of why these questions should be asked. The questions reflect the key components of the model and represent the collective experiences of the groups as useful ways of getting patients to talk about their pain.
Table 3.
Useful questions to ask patients to help assess their wound pain experiences
| Pain assessment | Questions | Explanation |
|---|---|---|
| Location | Where is the pain located: | The localisation of the pain is the first step in determining the cause of the pain and directing appropriate investigations and treatments |
| In the wound bed? | ||
| In the area surrounding the wound? | ||
| Another location in the region of the wound? | ||
| Is the pain unrelated to the wound? | ||
| Duration | How long has the pain been experienced? | A change in the pain suggests the need for a reassessment |
| Is the pain persistent? (At rest or with activities?) | ||
| Is the pain temporary? (Procedurally, at dressing change, during cleansing and debridement) | ||
| Intensity | How strong is chronic wound pain on a scale from 0 to 10? | Pain is subjective and should be treated based on the patient’s symptoms. Pain measurement scales should be used to monitor the development of pain and the patient’s response to treatment |
| 0 = no pain, 10 = worst pain | ||
| Quality | Ask the patients to describe their wound pain. Is it: | It is important to match the treatment of pain to its characteristics; many patients may have both nociceptive and neuropathic pain |
| Aching, throbbing, gnawing, tender (nociceptive) | ||
| Burning, stinging, shooting, stabbing (neuropathic) | ||
| Increased or new onset of pain | Reassess: Has the wound changed? Increased size or other signs and symptoms (increased inflammation, infection, cellulitis, etc.) | If the wound is painful and has signs of critical colonisation/infection, it is important to treat the cause |
| Activities of daily living | Is there anything you do that makes your pain better or worse? | Effective wound pain management involves activities of daily living |
| How does the patients’ chronic wound pain interfere with their: | ||
| Usual activities | ||
| Sleep | ||
| Ability to move around | ||
| Appetite | ||
| Mood |
There are also a number of recognised, validated pain measurement scales [Visual Analogue Scale (VAS), Numeric Box Scale, The Faces Scale, Visual Rating Scale] (25) that can be used to assess pain (25). The use of these validated scales on a regular basis can assist in measuring the impact of pain on sleep, mood state, anxiety levels and activities of daily living (26). The VAS is considered the gold standard for research purposes (25), but there are often situations in which this tool can be particularly difficult to use, such as those with literacy problems or cognitive or communication difficulties. Such circumstances may require the use of a simpler scale, such as the Faces Scale. In some cases, a pragmatic way to assess pain is simply to ask: “Is the pain better, worse or the same?” at each visit; this at least allows for a record of change in pain to be recorded. There will be circumstances in which patients are unable, due to their illness, to self‐assess their pain levels, and in such cases, health care professionals will need to evaluate non verbal communication signs and/or signals to estimate their pain levels (27).
Optimal management of wounds requires holistic assessment. Documentation of the patient’s pain experience is critical and may range from the use of a patient diary (which should be patient driven) to recording pain entirely by the health care professional or caregiver (26). Effective communication between the patient and the health care team is fundamental to this holistic approach. The more frequently the health care professionals measure pain, the greater the likelihood of introducing or changing pain management practices. Ongoing reassessment of pain can be a long process, and the frequency will vary depending on the type of wound and the practice setting.
Local wound pain treatment
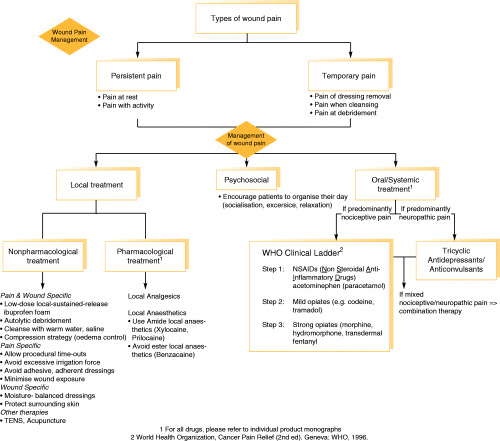
Local pain management should be based on simple principles, starting with the assessment of wound pain together with the underlying cause. This information should be communicated and a mutual decision reached between the health care provider and the patient to design the best combination of wound management and pain control. Local pain management is a natural first step in persistent pain treatment and can be subdivided into non pharmacological and pharmacological treatments. The WPMM outlines these two approaches: pharmacological treatments focus on the use of local and systemic treatments to reduce pain intensity for either persistent or temporary pain, while non pharmacological treatments include a range of strategies that health care professionals can use to minimise the impact of the procedures that they need to carry out to treat the chronic wound.
At present, there are few local options for the treatment of persistent pain, while managing the exudate levels present in many chronic wounds. However, a new foam dressing is available that releases ibuprofen in the presence of exudate (Biatain‐Ibu) (28). A recent review of the effect of non steroidal anti‐inflammatory drugs (NSAIDs) on wound healing has concluded that these drugs are unlikely to interfere with wound healing, with very few side effects when topical application is compared with oral NSAID treatment.
Systemic wound pain treatment
If local treatment does not provide adequate pain reduction, it may be necessary for patients with chronic painful wounds to be prescribed additional systemic treatment for the physical component of their pain. Clinicians should consult with their prescribing colleagues, referring to the World Health Organization (WHO) pain relief ladder (29) of systemic treatment options for guidance. The WPMM outlines the pharmacological options that can be considered depending on whether the patient presents with neuropathic or nociceptive pain, the steps in the WHO ladder reflecting a move towards more powerful drugs that may be necessary. For every pharmacological intervention, there are possible benefits and adverse events that the prescribing clinician will need to consider in conjunction with the wound care treatment team.
Psychosocial wound pain management
Patients often reject, and caregivers are sometimes reluctant to encourage, pharmacological interventions for pain management due to worries about addiction and side effects (24). For some patients, pain signifies that their disease is progressing, or a belief that they should not complain about pain. Alternatively, some patients prefer to deal with the psychosocial aspects of care on a personal basis and reject the interventions of health care professionals, despite an empathic response to their situation (24). Yet, research has demonstrated that psychological factors play an important role in coping, quality of life and disability resulting from chronic pain (30). Although there has been little research on psychological interventions for pain in wound care, a recent randomised controlled trial (RCT) of a community intervention programme documented pain‐level improvements and improved ulcer healing for those with extra focus on information sharing and preventive care for the patient (31). This approach could be a model to help with the considerable emotional aspects of wound pain.
Health care professionals should encourage patients to become involved in appropriate strategies to improve their pain. Options to be considered include coping skills training, behavioural contracts, biofeedback, relaxation and distraction techniques, or social support/self‐help groups. Health care professionals should suggest patients organise their day to include exercise, socialisation, TV, listen actively to music and focussed relaxation. Patients should be encouraged to take more control and improve their ability to cope. Some of these examples are included in the WPMM as part of a holistic approach to managing persistent, chronic wound pain; however, more information is available in the literature (32).
Pharmacological treatment of the neuropathic component of pain revolves around the use of antidepressants, anticonvulsants and opioids; all these drugs have the potential to help with the emotional component of pain (33). The tricyclic antidepressants and the newer serotonin and noradrenaline reuptake inhibitors have also been shown in RCTs to be beneficial for the physical component of both neuropathic and nociceptive pain (19). All provide relief of anxiety and unhappiness, improve sleep and relieve the physical component of pain (34). Anticonvulsant drugs are second‐line mood elevators for anxiety and unhappiness and may also help sleep and relieve the physical component of neuropathic pain 11, 19, 34.
Information on wound pain for health care professionals and patients
Education of patients and carers is an important element in successfully managing chronic wound pain, as patient education and involvement lead to improved outcomes (35). Health care providers need to use simple messages about pain management, given that persistent pain, anxiety, unhappiness and potential depression lead to a negative impact on other types of thinking, including poor concentration, poor memory and failure to complete cognitive tasks (36).
The management of wound pain should focus on discussing the care plan with the patient, and educational initiatives should encourage professionals to find ways to make this possible. A discussion of all the important aspects of education is outside the scope of this study, but in order to maximise the impact of models (such as WPMM) on professional practice, it is important that educational sessions for health care providers are interactive and focus on both pain assessment and management. The authors have developed several tools for practice to support the use of the WPMM [e.g. a pocket guide on wound pain management (37) and a guide to persistent pain management; Figure 2] to provide a useful basis for educational sessions. Professionals should refer to the evidence on strategies to minimise wound pain as part of developing their care packages (12).
Figure 2.
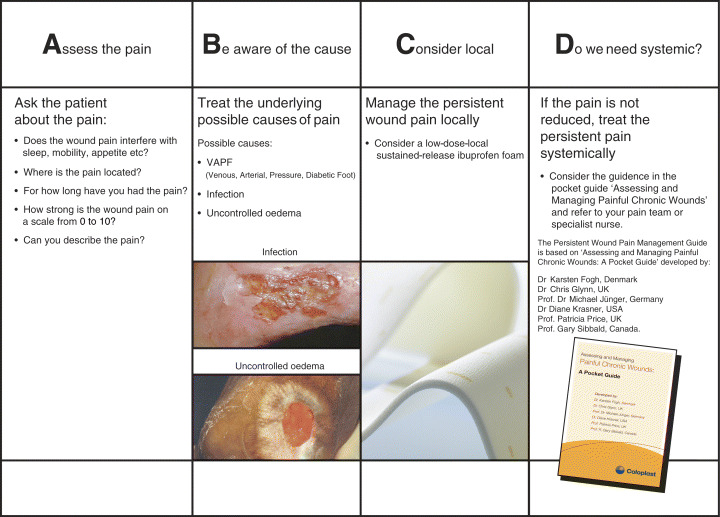
The ABCD guide summarize, in a mnemonic form, four steps to ensure better pain treatment.
Conclusion
Chronic, persistent wound pain occurs frequently in patients with leg ulcers and other types of wounds. Persistent pain dominates patients’ lives but, until recently, has not been a major concern for health care professionals. Many patients, particularly the elderly patients, are reticent to report their pain for fear of being seen as ‘difficult’; therefore, the obligation is for health professionals to ask about their patient’s pain and accurately document their responses. Holistic wound pain management must integrate local wound pain management, systemic pain management and psychosocial approaches. The WPMM has been developed to try to integrate important factors related to wound pain assessment and management, together with relevant factors for the assessment and management of chronic wounds. Each of these areas needs to be reviewed regularly as they overlap considerably in terms of the daily experiences of patients.
Increasingly, health care professionals can select from a range of options to help patient’s effectively manage wound pain. Increased awareness of these options must be raised through coordinated, relevant educational initiatives. It is no longer acceptable to inadequately document persistent wound pain as the aim for wound care practitioners should be to develop a treatment and monitoring strategy to improve the lives of persons with chronic wounds. Unless wound pain is optimally managed, patient suffering and the associated costs to health care system will increase.
Conflicts of interest
All authors are members of the International Pain Advisory Board for Coloplast A/S and have been reimbursed for their services.
References
- 1. Yamada B, Santos V. Quality of life of individuals with chronic venous ulcers. Wounds 2005;17:178–89. [Google Scholar]
- 2. Price P, Harding K. Cardiff Wound Impact Schedule: the development of a condition‐specific questionnaire to assess health‐related quality of life in patients with chronic wounds of the lower limb. Int Wound J 2004;1:10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Persoon A, Heinen MM, Van Der Vleuten CM, De Rooij MJ, Van De Kerkhof PC. Leg ulcers: a review of their impact on daily life. J Clin Nurs 2004;13:341–54. [DOI] [PubMed] [Google Scholar]
- 4. Ribu L, Wahl A. Living with diabetic foot ulcers: a life of fear, restrictions, and pain. Ostomy/Wound Manage 2004;50:57–67. [PubMed] [Google Scholar]
- 5. Hopkins A. Disrupted lives: investigating coping strategies for non‐healing leg ulcers. Br J Nurs 2004;13:556–63. [DOI] [PubMed] [Google Scholar]
- 6. Wilson AB. Quality of life and leg ulceration from the patient’s perspective. Br J Nurs 2004;13:S17–20. [DOI] [PubMed] [Google Scholar]
- 7. Nemeth KA, Harrison MB, Graham ID, Burke S. Pain in pure and mixed aetiology venous leg ulcers: a three‐phase point prevalence study. J Wound Care 2003;12:336–40. [DOI] [PubMed] [Google Scholar]
- 8. Hofman D, Ryan TJ, Arnold F, Cherry GW, Lindholm C, Bjellerup M, Glynn C. Pain in venous leg ulcers. J Wound Care 1997;6:222–4. [DOI] [PubMed] [Google Scholar]
- 9. Noonan L, Burge SM. Venous leg ulcers: Is pain a problem? Phlebology 1998;13:14–9. [Google Scholar]
- 10. European Wound Management Association . EWMA Position document: pain at wound dressing changes [WWW document]. URL http://www.ewma.org. 2002. MEP London Ltd. [accessed on 2 March 2007] [Google Scholar]
- 11. International Association for the Study of Pain (IASP) . Pain terms: a list with definitions and notes on usage. Recommended by the IASP Subcommittee on Taxonomy. Pain 1979;6:249. [PubMed] [Google Scholar]
- 12. World Union of Wound Healing Societies . Principles of best practice: minimising pain at wound dressing‐related procedures. A consensus document [WWW document]. URL http://www.wuwhs.org. 2004. MEP London Ltd. [accessed on 2 March 2007] [Google Scholar]
- 13. Reddy M, Kohr R, Queen D, Keast D, Sibbald RG. Practical treatment of wound pain and trauma: a patient‐centered approach. An overview. Ostomy/Wound Manage 2003;49(4 Suppl):2–15. [PubMed] [Google Scholar]
- 14. Grey J, Harding K. ABC of wound healing. London, UK: BMJ Books, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Krasner D, Sibbald RG, Rodeheaver GT. Chronic wound care: a clinical source book for health care professionals. Malvern, PA: HMP Communications, 2007. [Google Scholar]
- 16. McCaffrey M, Pasero C. Pain: clinical manual. St Louis: Mosby, 1999. [Google Scholar]
- 17. Krasner D. The chronic wound pain experience: a conceptional model. Ostomy/Wound Manage 1995;41:20–5. [PubMed] [Google Scholar]
- 18. Schaible H‐G, Richter F. Pathophysiology of pain. Langenbecks Arch Surg 2004;389:237–43. [DOI] [PubMed] [Google Scholar]
- 19. Finnerup NB, McQuay HJ, Jensen TS, Sindrup SH. Algorithm for neuropathic pain treatment: an evidence based proposal. Pain 2005;118:289–305. [DOI] [PubMed] [Google Scholar]
- 20. Russo MD, Brose MD. Chronic pain. Ann Rev Med 1998;49:123–33. [DOI] [PubMed] [Google Scholar]
- 21. Moffat C, Franks P, Hollingworth H. Understanding wound pain and trauma: an international perspective. EWMA Position Document: pain at dressing change [WWW document]. URL http://www.ewma.org/. 2002. [accessed on 2 March 2007]
- 22. Ebbeskog B, Ekman S‐L. Elderly people’s experiences. The meaning of living with venous leg ulcer. EWMA J 2001;1:21–3. [DOI] [PubMed] [Google Scholar]
- 23. Flanagan M, Vogensen H, Haase L. Case series investigating the experience of pain in patients with chronic venous leg ulcers treated with a foam dressing releasing ibuprofen. World Wide Wounds 2006. [WWW document]. URL http://www.worldwidewounds.com/2006/april/Flanagan/Ibuprofen‐Foam‐Dressing.html [accessed on 2 March 2007]
- 24. Schofield P. Pain management for older people in care homes: a pilot study. Br J Nurs 2006;15:509–14. [DOI] [PubMed] [Google Scholar]
- 25. Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, Kerns RD, Stucki G, Allen RR, Bellamy N, Carr DB, Chandler J, Cowan P, Dionne R, Galer BS, Hertz S, Jadad AR, Kramer LD, Manning DC, Martin S, McCormick C, McDermott MP, McGrath P, Quessy S, Rappaport BA, Robbins W, Robinson J, Rothman M, Royal MA, Simon L, Stauffer JW, Stein W, Tollett J, Wernicke J, Witter J. Topical review and recommendations Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113:9–19. [DOI] [PubMed] [Google Scholar]
- 26. Osterbrink J. Der Deutsche Schmerzstandard und seine Auswirkungen auf die Pflege. Die Schwester, der Pfleger 2003;42:758–64. [Google Scholar]
- 27. Ferris FD, Balfour HM, Bowen K, Farley J, Hardwick M, Lamontagne C, Lundy M, Syme A, West PJ. A model to guide patient and family care: based on nationally accepted principles and norms of practice. J Pain Symptom Manage 2002;24:106–23. [DOI] [PubMed] [Google Scholar]
- 28. Jørgensen B, Friis GJ, Gottrup F. Pain and quality of life for patients with venous leg ulcers: proof of concept of the efficacy of Biatain‐Ibu, a new pain reducing wound dressing. Wound Repair Regen 2006;14:233–9. [DOI] [PubMed] [Google Scholar]
- 29. World Health Organization . Cancer pain relief. Geneva, Switzerland: WHO, 1996. [Google Scholar]
- 30. Turk DC, Okifuji A. Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol 2002;70:678–90. [DOI] [PubMed] [Google Scholar]
- 31. Edwards H, Courtney M, Finlayson K, Lindsay E, Lewis C, Shuter P, Chang A. Chronic venous leg ulcers: effect of a community nursing intervention on pain and healing. Nurs Stand 2005;19:47–54. [DOI] [PubMed] [Google Scholar]
- 32. Price P. The psychology of pain and its application to wound management. In: White R, Harding K, editors. Trauma and pain in wound care. London: Wounds UK, 2006:162–79. [Google Scholar]
- 33. Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Seattle, WA: IASP Press, 1994. [Google Scholar]
- 34. McQuay HJ, Moore RA. Antidepressants and chronic pain. BMJ 1997;314:763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Haynes RB, Yao X, Degani A, Kripalani S, Garg A, McDonald HP. Interventions to enhance medication adherence. Cochrane Database Syst Rev 2005. (4) CD000011. [DOI] [PubMed] [Google Scholar]
- 36. Dufton BD. Cognitive failure and chronic pain. Int J Psychiatry Med 1989;19:291–7. [DOI] [PubMed] [Google Scholar]
- 37. Fogh K, Glynn C, Jünger M, Krasner D, Price P, Sibbald R. Assessing and managing painful chronic wounds: a pocket guide. Humlebæk, Denmark: Coloplast A/S, 2006. [Google Scholar]
- 38. Ebbeskog B, Lindholm C, Öhman S. Leg and foot ulcer patients. Epidemiology and nursing care in an urban population in south Stockholm, Sweden. Scand J Prim Health Care 1996;14:238–43. [DOI] [PubMed] [Google Scholar]
- 39. Lindholm C, Bergsten A, Berglund E. Chronic wounds and nursing care. J Wound Care 1999;8:5–10. [DOI] [PubMed] [Google Scholar]
- 40. Hollinworth H, Colllier M. Nurses’ views about pain and trauma at dressing changes: results of a national survey. J Wound Care 2000;9:369–73. [DOI] [PubMed] [Google Scholar]
- 41. Charles H, Callicot C, Mathurin D, Ballard K, Hart J. Randomised, comparative study of three primary dressings for the treatment of venous ulcers. Br J Community Nurs 2002;7(6 Suppl): 48–54. [DOI] [PubMed] [Google Scholar]
- 42. Margolis DJ, Bilker W, Santanna J, Baumgarten M. Venous leg ulcer: incidence and prevalence in the elderly. J Am Acad Dermatol 2002;46:381–6. [DOI] [PubMed] [Google Scholar]
- 43. Nemeth KA, Harrison MB, Graham ID, Burke S. Understanding venous leg ulcer pain: results of a longitudinal study. Ostomy Wound Manage 2004;50:34–46. [PubMed] [Google Scholar]
- 44. Goncalves ML, VLCdG Santos, CAdM Pimenta, Suzuki É, Komegae KM . Pain in chronic leg ulcers. J Wound, Ostomy Continence Nurs 2004;31:275–83. [DOI] [PubMed] [Google Scholar]
- 45. Godfrey H. Understanding pain. Part 1: physiology of pain. Br J Nurs 2005;14:846–52. [DOI] [PubMed] [Google Scholar]
- 46. Mangwendeza A. Pain in venous leg ulceration: aetiology and management. Br J Nurs 2002;11:1237–42. [DOI] [PubMed] [Google Scholar]


