Abstract
All penetrating neck wounds are potentially dangerous and require emergency treatment because there are important vessels, nerves and organs in the neck. We present the case of a patient who had an unusual penetrating neck injury caused by a broken windshield, noticed accidentally. Because fragments of windshield glass consist of sharp material, and the neck contains vital structures, such penetrating neck injury may cause life‐threatening complications. Radiological examinations should be offered before the management of all neck wounds. The risk of retained foreign bodies and related complications can be prevented by using fluoroscopy during surgical exploration of the neck.
Keywords: Fluoroscopy, Neck, Penetrating trauma, Windshield, Zone II
Introduction
Penetrating neck injuries are presented in 5–10% of all trauma cases. Multiple vital structures of the neck can be divided into four groups, including (i) the air passages: trachea, larynx and lung; (ii) vascular structures: carotid, jugular, subclavian, innominate and aortic arch vessels; (iii) gastrointestinal structures: pharynx and oesophagus and (iv) neurological structures: cranial nerves, peripheral nerves, brachial plexus and spinal cord, which are vulnerable to injury in the neck (1). Many kinds of material can cause penetrating trauma to the neck, such as a knife, shotgun, pencil and fragments of glass 1, 2, 3). We present the case of a patient who had an unusual penetrating neck injury caused by a broken windshield, noticed accidentally.
Case report
A 50‐year‐old woman was admitted in the emergency room with a 4‐cm incisional wound and small face lacerations related to a car accident. The wound was located on the right submandibular region horizontally and extended to a deep layer of the neck (Figure 1). There was no active bleeding or haematoma. She did not have any trauma, injury or wound in the other locations of her body except for the neck wound. She was fully conscious. Neurological and other systemic physical evaluations were normal. An X‐ray examination of the neck was performed before suturing of the wound for fear of cervical dislocation or fracture, although there was no evidence of blunt trauma of the head and neck area. The X‐ray showed multiple radiopaque foreign bodies in the deep location of zone II of the neck (Figure 2A,B). In the otolaryngological examination, there was no tenderness, subcutaneous emphysema, dysphagia, dyspnea, haematemesis, haemoptysis, hoarseness or Horner's syndrome. Vocal cords were mobile in the indirect laryngoscopy. Function of the hypoglossal and spinal accessory nerves were also normal.
Figure 1.

The wound located on the right submandibular region horizontally and extended deep layer of the neck.
Figure 2.
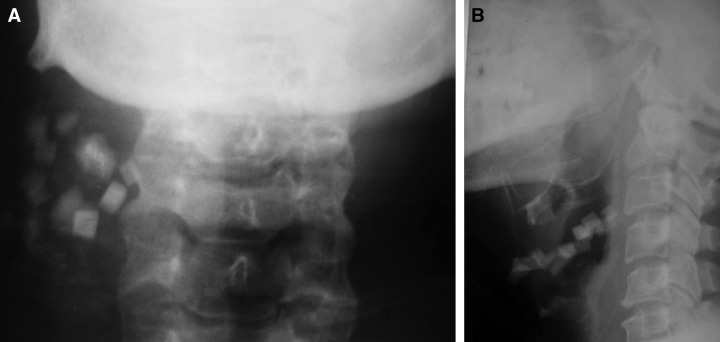
The X‐ray shows multiple radiopaque foreign bodies in the deep location of zone II of the neck. (A) A‐P X‐ray, (B) lateral X‐ray.
The patient was taken to the operating room. Multiple glass fragments were seen in the wound. An incision lengthening the wound ends was made from the mastoid tip to the midline of the neck for definitive exploration. The fragments were located from the subplatysmal area to the deep cervical fascia (Figure 3). The vagus nerve, the common carotid artery, jugular vein and hypoglossal nerve were identified. The fragments were found around these vessels and nerves, but there was not any injury on the carotid sheath, jugular vein, vagus or hypoglossal nerves. There was also no bleeding or haematoma in the zone II area. Fifteen glass fragments of windshield were removed carefully. Complete removal of glass fragments was checked by undertaking fluoroscopy of the neck, intraoperatively, and another two small fragments of windshield were seen in the deep locations of the neck and then removed (Figure 4). The wound was closed primarily. Postoperative recovery was uneventful, and she was discharged on the seventh day. Subsequent magnetic resonance (MR) angiography did not show any abnormality at 6 months after injury.
Figure 3.
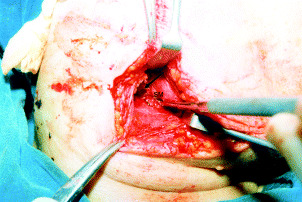
A sharp fragment (black arrow) near the common carotid artery is seen. SM, submandibular gland.
Figure 4.

Seventeen sharp glass fragments.
Discussion
All penetrating neck wounds are potentially dangerous and require emergency treatment because of the presence of vessels, nerves and organs in the neck. The neck is divided into two major triangles by sternocleidomastoid (SCM) muscle, the anterior and posterior. The anterior cervical triangle contains submandibular, submental, superior and inferior carotid triangles. The submandibular triangle is outlined by the two converging bellies of the digastric muscle and the inferior margin of the mandible. The submandibular triangle contains the submandibular gland, lymphatic structures, parts of the anterior facial vein and facial artery, and the marginal mandibular branch of the facial nerve. The carotid triangle is outlined the posterior belly of the digastric muscle, the omohyoid muscle and SCM. The carotid triangle carotid artery, jugular vein, hypoglossal and vagus nerves (4). Although there are many classifications of the neck, the neck also can be divided into three major zones to aid in the decision making for diagnostic tests and timing of surgery including zones I, II and III (1). Zone I is located below the cricoid cartilage of the larynx. The bony thorax and clavicle act to protect zone I from injury. Zone III is located above the angle of the mandible. The mandibular ramus may provide some protection to vital structures in ‘zone III’ as internal carotid artery, internal jugular veins and cranial nerves (1). The level of the zone II is located between angle of the mandible and cricoid cartilage. Although zones I and III are protected by bones, penetrating trauma of these area is more dangerous than in zone II because of proximity thorax and skull base (1). The vital structures in the zone II are not protected by bone, and the risk of injury is different to that in zones I and III.
Angiography is the useful diagnostic technique for both the evaluation of the vital vessels and the evaluation of the relationship between foreign bodies and vessels (1, 5). Angiography is offered in injuries of the zones I and III, while angiography or exploration could be selected in injuries of the zone II (5, 6). It was demonstrated that there was no significant difference between clinical examination and angiography for the detection of vascular injury in zone II penetrating neck injuries (6). It is an invasive diagnostic tool, and allergic reactions can occur. Indication for an angiogram in zone II injures included a stable patient who has persistent haemorrhage and neurological deficits, such as Horner's syndrome indicating sympathetic nerve plexus injury or hoarseness indicating a recurrent laryngeal nerve injury (1). However, non invasive diagnostic tools such as computed tomography, MRI, MR angiography and Doppler examination give more information about the exact location of the foreign bodies and relationship between foreign bodies and vessels. The present case had penetrating neck injury in zone II. There was no active bleeding or haematoma in the wound, but a skin wound of 4 cm was present. Therefore, we preferred exploration in order to evaluate vascular and nerves structures and remove sharp foreign bodies.
Currently, old glass, which can easily break into small pieces, is not being used for windshields in cars. New windshield glass is more resistant than old windshield glass (7). All modern glass in common use is radiopaque. Even glass fragments as small as 1 mm can be detected by direct X‐ray (2). Foreign bodies can be difficult to visualise because of opacity of the cervical spine, especially in the midline lesions (3). Therefore, a lateral and an Anterior‐Posterior (A‐P) X‐ray must be taken. The plain X‐rays including lateral and A‐P X‐rays showed multiple radiopaque foreign bodies in the deep location of zone II of the neck (Figure 2A,B). When exploration of the wound was performed, multiple windshield glass fragments were seen just around carotid sheath, jugular vein, vagus nerve and hypoglossal nerve (Figure 3). Although there were 17 sharp fragments in the wound, she had only one entrance wound for all these fragments. A large glass fragment of windshield could have entered through the wound and then broken into small pieces in the deep layers of the neck. Any remaining foreign bodies in the wound may have caused early and late complications, such as infection, wound dehiscence, cosmetic deformity and salivary fistula. Also, foreign bodies that pose a risk to injuring vital structures on removal and act as a tampon arresting the bleeding from a vital organ or vessel can still remain deep in the tissue (2). If the foreign body or bodies are composed of sharp material, they may lead to complications in the early and late periods. In the present case, fluoroscopy was used to confirm complete removal of the glass fragments, because there was a risk of retained sharp foreign bodies.
In conclusion, even patients who have a small incision in the neck may have a large number of foreign bodies in the wound. Because the fragment of windshield glass was very sharp material and the neck includes vital structures, penetrating neck injury by broken windshield glass may cause life‐threatening complications. Radiological examination should be offered before the management of all the neck wounds for fear of foreign bodies, especially in an accident of an old model car. During surgical exploration of the neck to remove foreign bodies, if necessary, there is a risk of multiple retained foreign bodies. Risk of retained foreign bodies and related complications can be prevented by using fluoroscopy during surgical exploration of the neck.
References
- 1. Maisel HM, Hom DB. Penetrating trauma to the neck. In: Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Richardson MA, Schuller DE, editors. Otolaryngology Head Neck Surgery. St Louis: Mosby, 1998:1707–20. [Google Scholar]
- 2. Rothschild MA, Karger B, Schneider V. Puncture wounds caused by glass mistaken for with stab wounds with a knife. Forensic Sci Int 2001;121:161–5. [DOI] [PubMed] [Google Scholar]
- 3. Pickles JM. Retropharyngeal abscess complicating a neck wound (a case report). J Laryngol Otol 1988;102:552–3. [DOI] [PubMed] [Google Scholar]
- 4. Lingeman RE. Surgical Anatomy. In: Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Richardson MA, Schuller DE, editors. Otolaryngology Head Neck Surgery. St Louis: Mosby, 1998:1673–85. [Google Scholar]
- 5. Miller RH, Duplechain JK. Penetrating wounds of the neck. Otolaryngol Clin North Am 1991;24:15–29. [PubMed] [Google Scholar]
- 6. Jarvik JG, Philips GR III, Schwab CW, Schwartz JS, Grossman RI. Penetrating neck trauma: sensitivity of clinical examination and cost‐effectiveness of angiography. AJNR Am J Neuroradiol 1995;16: 647–54. [PMC free article] [PubMed] [Google Scholar]
- 7. Sances A Jr, Carlin FH, Kumaresan S, Enz B. Biomedical engineering analysis of glass impact injuries. AJNR Am J Neuroradiol 1995; 16:647–54. [DOI] [PubMed] [Google Scholar]


