Abstract
We introduced the concept of moist wound healing to extend the limits of fingertip composite grafting. In this retrospective study, we assessed the success of fingertip composite grafting with moist‐exposed ointment dressing, which has been shown to maintain adequate moisture for optimal healing by frequent ointment application without the need for a secondary overlying dressing. We reviewed the outcome of composite graft replacement of 60 amputated fingertips in 56 consecutive patients over a period of 3 years and 3 months. Forty‐two fingertips had survived completely and 18 had failed. Twelve of 15 fingers among patients younger than 15 years of age and 30 of 45 fingers among those 16 years of age and older had survived completely. We believe that our use of antibiotic ointment to maintain a moist environment was an important factor in improving the survival of composite grafts.
Keywords: Composite graft, Fingertip, Moist dressing, Replantation
Introduction
The fingertip is the most commonly damaged part of the body. Its amputation involves the possibility of loss of all its unique functions and severe cosmetic after effects. When traumatic amputation happens, replantation through microscopic vessel reanastomosis is the most secure redemption method because the functional and cosmetic final results are far superior to those obtained with any local or pedicled flap. Because of improvements in our understanding of the vascular anatomy of the distal digit 1, 2, 3) and advances in surgical instrumentation and microvascular surgical technique, replantation of distal digits, even in young children, is no longer technically challenging 3, 4, 5), although it is not usually practical. Microvascular replantation is particularly difficult in a digit distal to the distal palmar arch. If the technique fails, not only is the digit shortened but also all its unique functions are lost. In this case, the only possible way to achieve a full‐length digit with a normal nail complex is to use a composite graft.
Initially, a composite graft is nourished by diffusion, but later on, it survives through revascularisation, like a skin graft does. The success rate of fingertip composite grafts is still very low because the distal regions of grafted fingertips, which cannot be nourished by diffusion, suffer irreversible damage before revascularisation can occur, leading to cellular destruction. As a rule, this technique is feasible only in young children with amputations distal to the lunula and is not advocated for adults because of its low success rate (6, 7). Some authors have reported excellent results with fingertip composite grafting, whereas others have been unable to achieve such success; however, numbers of patients have been small (8, 9). This is why surgeons still regard this technique as uncertain and use it in adults reluctantly and without great hope of success.
It has been demonstrated that good hydration of the external wound is the single most important external factor responsible for optimal wound healing and that moist wounds show more rapid progression to the level of vascularisation of uninjured skin than do dry wounds 10, 11, 12, 13). Furthermore, in human studies, hydration has been shown to improve wound healing (14, 15), and for this retrospective study, we reviewed the cases of patients with fingertip amputations who had undergone composite grafting with application of moist‐exposed dressing to assess the survival rate of the replantation in our institution. Our purpose was to determine whether keeping the wound moist, a simple measure that most surgeons neglect, would improve the traditionally poor results of composite grafting of amputated fingertips.
Patients and methods
Patients
We reviewed the medical records of consecutive patients who had had traumatic amputation of one or more fingertips without concomitant trauma and who had undergone composite grafting between March 1997 and December 1999.
For composite grafting, minimal debridement, which removes only devitalised subcutaneous fat and skin, and minimal diathermy had been used. Under loupe magnification, the skin had been accurately approximated without tension using 5‐0 nylon sutures. The patient's entire arm had then been immobilised with an above‐elbow splint for 2 weeks. Patients had been instructed to elevate the affected hand and to apply topical ofloxacin ophthalmic ointment (Ocuflox®; Samil, Seoul, Korea) once or twice per hour to the reattached fingertip to maintain moisture balance and prevent infection. Ocuflox® has been shown to be effective against a broad range of gram‐positive and gram‐negative bacteria (16). No debridement had been performed for 2 weeks after replantation to avoid altering the delicate vascular supply unless infection or necrosis made it necessary.
For the purpose of this analysis, we classified the level of finger amputation as one of three zones defined in relation to the lunula: zone I, distal to the lunula, the sterile matrix; zone II, at the lunula, the germinal matrix; and zone III, proximal to the lunula (Figure 1). We compared the success rates of the composite grafts according to the age of the patient and the level and type of the amputation. There was no control data in this study, but before introducing this moist‐exposed dressing, we had been doing many kinds of trials such as cooling with or without aluminium foil, bolus dressing and pocketing, but the results were indiscriminately very poor. A review of the literature was conducted with a Medline search. The data comparing fingertip composite graft's survival rate with other treatments are presented in Table 1.
Figure 1.
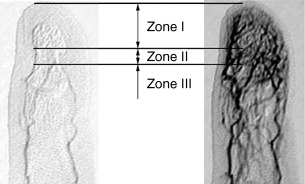
Classifications of fingertip amputation: zone I, distal to the lunula, the sterile matrix; zone II, at the lunula, the germinal matrix; and zone III, proximal to the lunula. Serial angiograms show the distal transverse palmar arch or distal palmar arch lying adjacent to the distal phalangeal bone. From this arch, several arterial branches arise in a longitudinal manner and travel to the tip, where myriad fine vessels arise.
Table 1.
Comparison of clinical results of fingertip composite graft
| Review of the literature | |||||||
|---|---|---|---|---|---|---|---|
| Standard group | Modified group | Milieu‐changing (moist) group | |||||
| Moist‐exposed dressing | Elsahy (7) | Moiemen and Elliot (17) | Brent (18) | Rose et al. (19) | Douglas (9) | Hirase (20) | |
| Number of patients | 56 | 35 | 50 | 3 | 7 | 17 | 11 |
| Mean age | 28 | 5·7 | 17 | Adults | |||
| Number of fingers | 60 | 35 | 50 | 4 | 7 | 17 | 11 |
| Complete survival | 42 | 21 | 11 | 2 | 5 | 15 | 9 |
| Survival rate (%) | 70 | 60 | 22 | 50 | 71·4 | 88·2 | 90·9 |
We judged the success of the composite graft on the basis of clinical notes and photographic records. Sloughing of the outer skin layer in a grafted fingertip makes it hard to assess the survival of a graft (7), but a great advantage of the antibiotic ointment that had been used is its translucency, which allowed visual inspection of the pink wound underneath the outer layer of skin and thus early assessment of the survival of the fingertip (Figure 2). Successful replantation was defined as complete survival of the graft without the need for any additional special handling except when the outer layer of skin had sloughed off or had been removed. Failure of replantation was defined as partial or complete necrosis of the grafted finger. χ2‐testing was used to test for statistical analysis; a P < 0·05 was considered significant.
Figure 2.

Photograph taken 2 weeks after composite grafting shows the pink colour under the outer layer of skin, which eventually sloughed off.
Results
Patients
In total, 56 paediatric and adult patients (43 males and 13 females) whose mean age was 28 years (range 1–60 years) had undergone 60 fingertip composite grafts during the study period. Of these 60 composite grafts, grafting had been successful in 42 and it had failed in 18. Evaluation by age revealed that grafting had been successful in eight of ten fingers among patients less than 6 years old, in four of five fingers among those 6–15 years old and in 30 of 45 fingers among those 16 years of age and older. Assessment by level of amputation showed that grafting had been successful in 23 of 31 fingers amputated in zone I, in eight of 14 fingers amputated in zone II and in 11 of 15 fingers amputated in zone III. Finally, assessment by type of amputation revealed that grafting had been successful in 20 of 24 guillotine‐type, in 20 of 32 crush‐type and in two of four avulsion‐type amputations. No statistically significant differences in graft survival were found in relation to age [P = 0·68, 66·7% (percents of expected count less than five in χ2‐tests)], amputation level (P = 0·79, 55·6%) or type of amputation (P = 0·14, 55·6%).
Discussion
Composite fingertip grafting in children is an accepted, successful procedure, but until now, the same procedure in adults has been considered very challenging. The fingertip, like other terminal portions of the body, i.e. the toe, nasal tip and ear, has a unique vascular system. The vascular anatomy of the fingertip, important not only for microsurgical replantation but also for successful composite grafting, has been reported in detail 1, 2, 3). In addition to the development of microsurgical technique, microscopic vessel reanastomosis has become possible even in the distal transverse palmar arch; however, this is feasible only when the microsurgeon can find the proper vessel. If it is not found or does not exist, attention for composite grafting should be given to the numerous fine vessels arising in the terminal arterial branches (Figure 1). The provision of a moist environment around the reattached fingertip in our patients is presumed to have increased the success rate of inosculation of these fine vessels.
Composite grafting should not be the first approach to fingertip replantation; instead, it should be the solution attempted only after the microsurgeon has been unable to find the proper vessel for microanastomosis. Avoiding damage to the surrounding tissues during the search for the proper vessel should be the primary concern. Damage to the fine vessels arising from two or three vessels of the distal transverse palmar arch branch has serious consequences for the survival of the composite graft. Other important aspects of graft survival are preventing the creation of any dead space through the use of minimal debridement and maintaining a moist dressing for 2 weeks, except in cases of infection or tissue necrosis.
The factors associated with the success of composite grafting have not been fully elucidated. Fingertip composite grafting has been grouped into three approaches in published articles: standard replacements (7, 17), modified replacements (18, 19) and attempts to increase the survival rate by changing the milieu of the graft after surgery (9, 20) (Table 1). Of these three approaches, milieu‐changing has achieved the highest level of success. Douglas (9) reported successful replantation in 15 of 17 amputations at various levels. He meticulously replanted and then kept the dressings wet with normal saline. Hirase (20) used ice water and aluminium foil to retard cellular degeneration and reported complete survival in nine of ten grafts. Ice water and aluminium foil seem most likely to keep the wound moist because the former, as the source of moisture, and the latter prevent evaporation and maintain the moisture. Although the total number of patients in both those studies was small, and the patients' age distribution was not mentioned, the results are far superior to those achieved with the other two approaches (7, 17, 18).
Our use of composite grafting with moist‐exposed dressing could be considered one of these third types of approach. We also achieved high success rates. Furthermore, our technique is even simpler and is more effective at keeping the wound moist. Finally, the total number of patients in our series is the largest reported to date, as far as we know.
We believe there are several reasons why keeping a moist environment is an important factor for composite graft survival. It has been confirmed that wounds reepithelialise more rapidly under moist conditions than they do under dry ones (10, 11, 21, 22). A moist wound environment prevents the development of dermal necrosis, which is the most common finding with exposure to air. An open wound exposed to air for 2–3 hours dehydrates quickly, and in this time, the dermis can become necrotic to a depth of 0·2–0·3 mm (23). The desiccated dermis prevents epithelial cell proliferation, migration and differentiation. In this study, we had kept the reattached fingertip moist with an antibiotic ointment. As a result, shrinkage of the replantation did not occur to any notable degree (Figure 3B). Furthermore, the appearance of turgidity suggested that the implant was hydrated (14, 15), necrotic infection had not developed and fine reepithelialisation was observed underneath the outer keratin layer. Another advantage of a moist environment is that it minimises cellular deformity of the fingertip and keeps fine vessels open until inosculation and neovascularisation can occur and prevents eschar, which may be a cause of mechanical tissue compression that contributes to cellular destruction before new vessels form. The constriction caused by dermal necrosis could be especially great when a circular amputated fingertip becomes dehydrated. A third advantage of a moist environment is that it may increase the rate of angiogenesis. Dyson et al. (10, 24) have stated that wounds maintained in a moist environment presented more endothelial cells and revascularised at a greater rate than did those maintained in a dry environment. After all, vessel inosculation is very important because revascularisation is essential for the survival of composite grafts, and a moist environment is thought to be a positive factor. High survival rate of our composite graft series in a moist environment provides some insight into the counterevidence of increased revascularisation. In one case, the reattached fingertip was removed at the patient's request 2 weeks after surgery. A histological examination showed progress of necrosis in the distal parts but evidence of capillary and fibroblast proliferation in the proximal region (Figure 4). Recently, in an established porcine model, we compared skin composite graft take rates in wet, moist and dry environments. The results showed that the survival rates of wet and moist groups were significantly higher than those of dry group. By postoperative 3 weeks in moist condition, good neovascularisation was observed between the graft and lower portion of the recipient (25). A fourth advantage is that maintaining a moist environment has been shown to reduce inflammation and accelerate the inflammatory phase (12). The pathophysiology of composite graft failure probably involves ischaemia‐induced inflammation with resultant leucocytic infiltration and tissue oedema, leading to thrombosis (26). The antibiotic ointment may have reduced inflammation.
Figure 3.
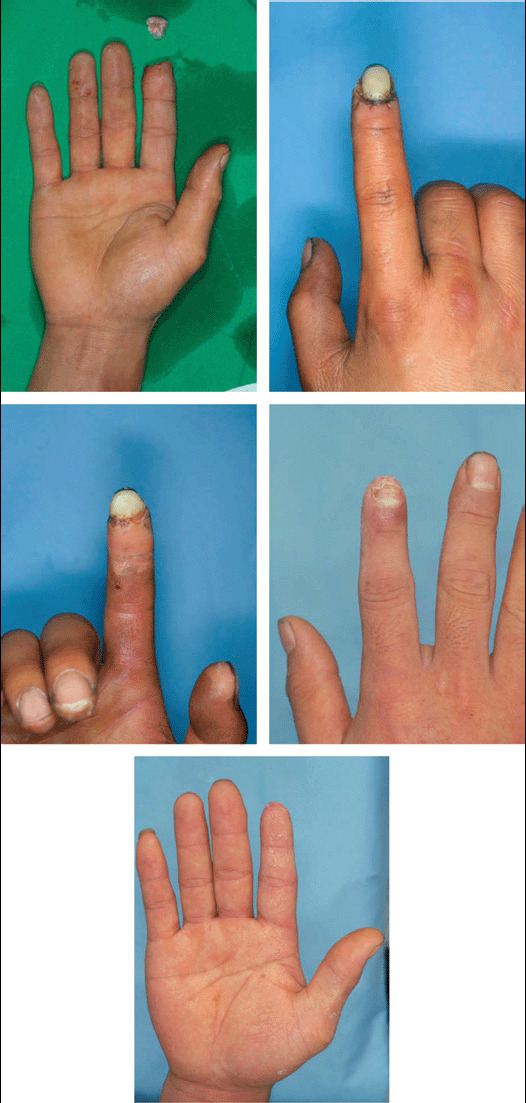
(A) Preoperative photograph of the fingers of a 31‐year‐old patient who had sustained a complete amputation of the right index fingertip in zone III. (B, C) Completion of a fingertip composite grafting. (D, E) The successful graft 3 months after grafting.
Figure 4.
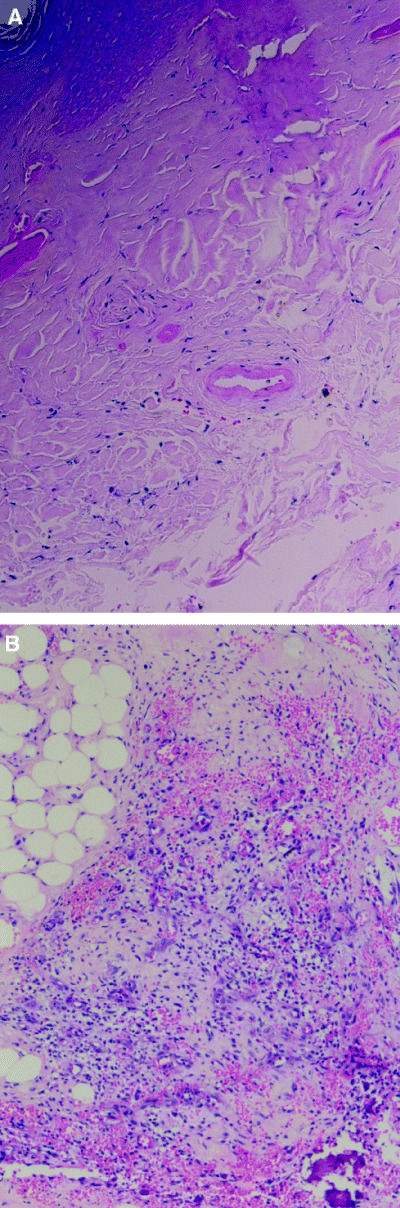
(A) Histologic section shows necrotic change of distal parts and capillary and fibroblasts proliferation of a more proximal part (haematoxylin and eosin ×40). (B) Histologic section showing many capillaries with extravasation of red blood cells under the subcutaneous fat layer (haematoxylin and eosin ×100).
Even successful fingertip composite grafts have some additional problems. First, complete healing takes a long time. After the outer layer of skin falls off in about 2 weeks, the red, single‐layer epithelium is visible. It takes another 2–3 weeks for this to grow thick and attain the colour of normal epidermis. Second, the replantation shrinks over time. If this shrinkage is severe, it can cause a hooked nail deformity. Further research is required on the degree of shrinkage and sensation recovery according to injury type and patient age.
We found a slightly higher complete survival rate in patients who were 6 years of age and younger than we did in those who were 16 years of age and older, but this difference was not statistically significant. We found no significant differences in survival related to amputation level or type statistically but a higher survival rate in guillotine‐type and zone I. Although further follow‐up and more cases are needed before a general statement can be made about the relationship between composite grafts and age, amputation level and amputation type, we believe that the use of moist‐exposed dressings should improve the success rate associated with fingertip composite grafting.
Acknowledgements
We thank professor Chulho Sohn for producing the angiograms and Dr Jungjae Lim and Dr Dongchul Won for expert assistance.
References
- 1. Strauch B, Moura W. Arterial system of fingers. J Hand Surg 1990;15A: 148–54. [DOI] [PubMed] [Google Scholar]
- 2. Smith DO, Oura C, Kimura C, Toshimori K. Arterial anatomy and tortuosity in the distal finger. J Hand Surg 1991;16A: 297–302. [DOI] [PubMed] [Google Scholar]
- 3. Foucher G, Norris RW. Distal and very distal replantations. Br J Plast Surg 1992;45: 199–203. [DOI] [PubMed] [Google Scholar]
- 4. Chen CT, Wei FC, Chen HC et al. Distal phalanx replantation. Microsurgery 1994;15: 77–82. [DOI] [PubMed] [Google Scholar]
- 5. Goldner RD, Stevanovic MV, Nunley JA, Urbaniak JR. Digital replantation at the distal interphalangeal joint and the distal phalanx. J Hand Surg 1989;14A: 214–20. [DOI] [PubMed] [Google Scholar]
- 6. Russel RC. Finger tip injuries. In: McCarthy JG, editor. Plastic Surgery. New York: W.B. Saunders, 1990: 4485–7. [Google Scholar]
- 7. Elsahy NI. When to replant a fingertip after its complete amputation. Plast Reconstr Surg 1977;60: 14–21. [PubMed] [Google Scholar]
- 8. Hirase Y. Postoperative cooling enhances composite graft survival in nasal‐alar and fingertip reconstruction. Br J Plast Surg 1993;46: 707–11. [DOI] [PubMed] [Google Scholar]
- 9. Douglas B. Successful replacement of completely avulsed portions of fingers as composite grafts. Plast Reconstr Surg 1959;23: 213–25. [DOI] [PubMed] [Google Scholar]
- 10. Dyson M, Young S, Pendle CL, Webster DF, Lang SM. Comparison of the effects of moist and dry conditions on dermal repair. J Invest Dermatol 1988;91: 434–9. [DOI] [PubMed] [Google Scholar]
- 11. Vogt PM, Andree C, Breuing K et al. Dry, moist, and wet skin wound repair. Ann Plast Surg 1995;34: 493–500. [DOI] [PubMed] [Google Scholar]
- 12. Breuing K, Eriksson E, Lin PY, Miller DR. Healing of partial thickness porcine skin wounds in a liquid environment. J Surg Res 1992;52: 50–8. [DOI] [PubMed] [Google Scholar]
- 13. Chen WYJ, Rogers AA, Lydon MJ. Characterization of biologic properties of wound fluid collected during early stages of wound healing. J Invest Dermatol 1992;99: 559–64. [DOI] [PubMed] [Google Scholar]
- 14. Jonsson K, Jensen JR, Goodson W et al. Tissue oxygenation, anemia, and perfusion in relation to wound healing in surgical patients. Ann Surg 1991;214: 605–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hartmann M, Jonsson K, Zederfeldt B. Effect of tissue perfusion and oxygenation on accumulation of collagen in healing wounds. Eur J Surg 1992;158: 521–6. [PubMed] [Google Scholar]
- 16. Snyder‐Perlmutter LS, Katz HR, Melia M. Effect of topical ciprofloxacin 0.3% and ofloxacin 0.3% on the reduction of bacterial flora on the human conjunctiva. J Cataract Refract Surg 2000;26: 1620–5. [DOI] [PubMed] [Google Scholar]
- 17. Moiemen NS, Elliot D. Composite graft replacement of digital tips, 2. A study in children. J Hand Surg 1997;22B: 346–52. [DOI] [PubMed] [Google Scholar]
- 18. Brent B. Replantation of amputated distal phalangeal parts of fingers without vascular anastomoses, using subcutaneous pockets. Plast Reconstr Surg 1979;63: 1–8. [DOI] [PubMed] [Google Scholar]
- 19. Rose EH, Norris MS, Kowalski TA et al. The ‘cap’ technique: nonmicrosurgical reattachment of fingertip amputations. J Hand Surg 1989;14A: 513–8. [DOI] [PubMed] [Google Scholar]
- 20. Hirase Y. Salvage of fingertip amputated at nail level: new surgical principles and treatments. Ann Plast Surg 1997;38: 151–7. [DOI] [PubMed] [Google Scholar]
- 21. Winter GD. Formation of the scab and rate of epithelialization of superficial wounds in the skin of the young domestic pig. Nature 1962;193: 293–4. [DOI] [PubMed] [Google Scholar]
- 22. Young SR, Dyson M, Hickman R, Lang S, Osborn C. Comparison of the effects of semi‐occlusive polyurethane dressings and hydrocolloid dressings on dermal repair: 1. Cellular changes. J Invest Dermatol 1991;97: 586–92. [DOI] [PubMed] [Google Scholar]
- 23. Evans RB. An update on wound management. Hand Clin 1991;7: 409–30. [PubMed] [Google Scholar]
- 24. Dyson M, Young SR, Hart J, Lynch JA, Lang S. Comparison of the effects of moist and dry conditions on the process of angiogenesis during dermal repair. J Invest Dermatol 1992;99: 729–33. [DOI] [PubMed] [Google Scholar]
- 25. Won DC, Son DG, Han KH, Park KK. Accelerated healing of composite graft in a wet environment: a pig model. J Korean Soc Plast Reconstr Surg 2003;30: 801–8. [Google Scholar]
- 26. Henrich DE, Logan TC, Lewis RS, Shockley WW. Composite graft survival. Head Neck Surg 1995;121: 1137–42. [DOI] [PubMed] [Google Scholar]


