ABSTRACT
Compression bandaging is a major cornerstone in the treatment of chronic venous insufficiency. Its efficacy considerably depends on the applied pressure and it is therefore largely dependent on the individual applying the system. The sub‐bandage pressure was measured under three consecutive compression bandages applied by 21 nurses before and after training and the introduction of a pressure monitor (Kikuhime®, MediTrade, Denmark). A questionnaire was used to evaluate the self‐rating before and after the intervention. Before intervention, a questionnaire showed the confidence of the nurses in reaching sufficient sub‐bandage pressure levels. However, 34·9% of all bandages were shown to be insufficient before intervention (< 20 or ≥ 60 mmHg) and only 17·5% after intervention, representing a statistically significant improvement through intervention. Of the insufficient bandages, 77·3% were applied by nurses with more than 10 years of working experience. Furthermore, the mean sub‐bandage pressure in active standing position, a marker for the working pressure, was improved form 38·7 to 64·3 mmHg after intervention. Continuous awareness and training are necessary to maintain sufficient compression bandaging. The availability of a pressure monitor was helpful to reach this goal. Long work experience and self‐rating alone is not sufficient to maintain adequate quality in compression bandaging.
Keywords: Bandages, Compression, Pressure monitor, Varicose ulcer, Working pressure
INTRODUCTION
Compression therapy is recognised as a major cornerstone in the treatment of venous insufficiency, increasing healing rates of venous leg ulcers 1, 2, 3. Insufficient compression therapy can lead to delayed healing. Compression enhances the venous outflow and reduces oedema by increasing the interstitial pressure of soft tissues 4, 5.
The comparison between different compression systems is difficult because internationally agreed standards are lacking. Compression classes differ from one country to another. Furthermore, a consensus is missing on how to define good, adequate or poor compression bandaging and on how to measure it. In the UK, performance indicators for compression bandages have been developed (6). In a recent consensus meeting, a new classification system for compression bandages with four pressure ranges was recommended. The compression pressure of < 20 mmHg has been categorised as mild, 20 to < 40 mmHg as medium, 40 to < 60 mmHg as strong and ≥ 60 mmHg as very strong (7). It was shown that high compression is more effective than low 1, 3. Compression bandaging of 35–45 mmHg sub‐bandage pressure at the ankle was shown in several studies to be safe and effective 7, 8, 9, 10, 11. Furthermore, short stretch bandages show an average pressure loss of 25% within 30–60 minutes 12, 13.
A broad range of different short stretch and long stretch as well as single layer and multilayer compression bandage systems are used. Multilayer compression bandaging has been proposed as the gold standard in the treatment of venous leg ulcers (14). However, non inferiority of other compression devices compared with short stretch compression bandages was reported (15). In another study, the effects of high pressure compression stocking plus thrombosis stockings was found to be more effective than short stretch bandages (16).
Application of compression bandages remains inevitable in phases of high wound secretion or in the initial phase of oedema treatment. Despite the fact that the efficacy of compression bandaging highly depends on the skills of the individual applying it, the use of objective devices to proof that the bandage is sufficiently applied are not a standard in training.
Different studies show that training and the use of a pressure monitor optimise compression bandaging skills of nurses; however, study design and definition of adequate or insufficient compression in the studies published differ in each study 9, 17, 18, 19, 20.
In the presented prospective study, the sub‐bandage pressure before and after introduction of a pressure monitor and training was measured. Pressure under bandages applied by nurses with short, medium and long professional experience was evaluated. Compression bandaging with pressure of < 20 or ≥ 60 mmHg was rated as insufficient and pressure between 35 and 45 mmHg was rated as optimal. The self‐rating questionnaire was correlated with the pressure measurement.
METHODS
From the Department of Dermatology, University Medical Center Freiburg, Germany, 21 qualified nurses were included in the study. All participating nurses were working in a specialist dermatology clinic. All participants gave informed consent. During their daily working routine, all nurses frequently applied high‐compression bandages for treatment of lymph oedema and venous insufficiency.
Self‐report questionnaire
A self‐report questionnaire was used to collect information on confidence and self‐perceived competence in the application of compression bandages. The questionnaire was completed before the first sub‐bandage pressure measurement and the introduction of the pressure monitor. Confidence about adequate pressure under the compression bandage was rated on a 1–10 scale (1 very confident and 10 unconfident). After the intervention, the nurses were asked to assess the usefulness of the pressure monitor based on a 1–10 scale (1 very useful and 10 useless).
Compression bandaging
The nurses were asked to apply a compression bandage with short stretch bandages (Pütter Bandages, Hartmann, Germany) in the same way as they did in everyday high‐compression bandaging task. The number of compression bandages, the width of the bandage and the technique was chosen by the participant: two to three bandages were applied using different multilayer compression techniques. Every nurse applied three consecutive compression bandages with the same technique and the same amount of bandages. External factors like differences in curvature or surface are prone to influence the results of the measurements (21). To ensure compatibility of the measurements taken, the leg of the same volunteer was used throughout the study and the pressure sensor was always placed under the short stretch bandages. In the training phase, pressure between 35 and 45 mmHg was rated to be optimal. This sub‐bandage pressure is in agreement with the recent consensus document recommending a sub‐bandage pressure ’around 40 mmHg of the supine subject' to be aimed (7).
Statistical methods
Data approximately normal in distribution were analysed using the t‐test for paired samples in order to determine the probability that pre‐ and post‐educational pressures have the same distribution. A P‐value less than 0·05 was considered significant. In addition, Fisher's exact test for small sample sizes has been applied to the analysis of categorised pressures in a contingency table (mild/very strong, < 20 or ≥60 mmHg versus medium/strong, 20 to < 60 mmHg), regarding a P‐value of less than 0·05 as significant. Statistical analysis has been performed using SPSS version 16 (Chicago, Illinois, USA).
Box plots are drawn for descriptive statistics using five‐number summaries, that is, sample minimum, lower quartile, median, upper quartile and sample maximum.
Measurement
Baseline measurements were performed before theoretical and practical training took place. The result of the sub‐bandage pressure measurement was not unfolded before the third consecutive measurement. Training was performed and the participants were instructed to use the pressure monitor. For consolidation of the training, couples within the team were formed and the participants were asked to use the bandage pressure monitor in the following weeks at each other. The Kikuhime® sub‐bandage pressure measuring device by MediTrade was used in the study. A 30 × 38 mm pad was placed about 12 cm above the inner ankle at the medial aspect of the lower leg where the tendon changes into the muscular part of the gastrocnemius muscle. This point is known as the B1 point according to the recent consensus report (7). The body mass index of the volunteer was within normal ranges.
The supine position measures the achieved pressure in inactivity, the ’resting pressure’. The active standing position on the assessed leg is expected to correlate with the pressure in action, the ’working pressure’12, 22.
The measurement was repeated about 10–14 weeks after the training and the introduction of the pressure monitor.
RESULTS
Baseline measurements showed that 34·9% of the compression bandages were applied with insufficient pressure of < 20 mmHg in supine position, no bandages were applied with pressure ≥ 60 mmHg (Table 1; 1, 2). After intervention only 4·8% of the bandages showed insufficient mild pressure; however, 12·7% were ≥ 60 mmHg (Table 2; 1, 2). The decrease of bandages with insufficient mild sub‐bandage pressure is visualised in Figure 1 left columns. In total, 17·5% of the bandages showed insufficient sub‐bandage pressure after intervention. Pre‐ and post‐educational resting pressure distribution (Figure 3) was significantly different (t‐test, P < 0 · 0001). The proportion of medium/strong versus mild/very strong sub‐bandage pressure calculated by Fisher's exact test was as well significant (P < 0 · 05). Pressure distribution in standing position (Figure 4) was also significantly different (P < 0 · 0001), where Fisher's exact test showed a significantly different proportion (P < 0 · 0001). Medium to strong sub‐bandage pressure (20 to < 60 mmHg) was achieved in 65% before intervention and in 82·6% after intervention (1, 2). Optimal sub‐bandage pressure, defined as 35–45 mmHg, was increased from 9·5% before intervention to 31·7% after intervention (Figure 2A,B).
Table 1.
The sub‐bandage pressure in resting position before training and the introduction of a pressure monitor
| Total | 0–2 years work experience | 3–10 years work experience | Above 10 years work experience | |
|---|---|---|---|---|
| Mild < 20 mmHg | 22 (34·9%) | 2 (16·7%) | 3 (14·3%) | 17 (56·7%) |
| Medium 20 to < 40 mmHg | 36 (57·1%) | 8 (66·7%) | 16 (76·2%) | 12 (40·0%) |
| Strong 40 to < 60 mmHg | 5 (7·9%) | 2 (16·7%) | 2 (9·5%) | 1 (3·3%) |
| Very strong ≥ 60 mmHg | 0 (0·0%) | 0 (0·0%) | 0 (0·0%) | 0 (0·0%) |
| Total | 63 (100·0%) | 12 (100·0%) | 21 (100·0%) | 30 (100·0%) |
Figure 1.
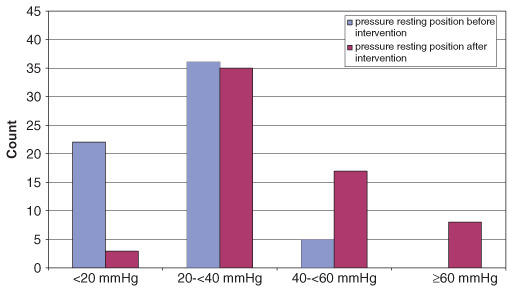
Sub‐bandage pressure before (blue) and after (purple) intervention. The study shows a drastic decrease of insufficient mild sub‐bandage pressure (< 20 mmHg) after intervention.
Figure 2.
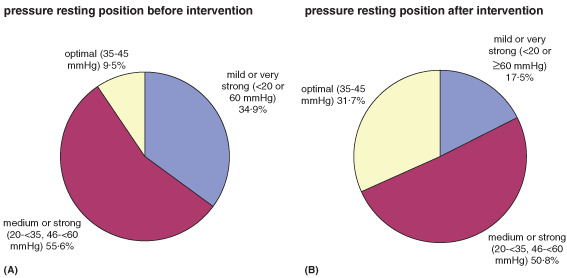
Optimal, medium or strong and mild or very strong sub‐bandage pressure before (A) and after (B) intervention, showing an increase of optimal sub‐bandage pressure from 9·5% before intervention to 31·7% after intervention and a decrease of mild or very strong sub‐bandage pressure from 34·9% to 17·5%.
Table 2.
The sub‐bandage pressure in resting position after training and the introduction of a pressure monitor
| Total | 0–2 years work experience | 3–10 years work experience | Above 10 years work experience | |
|---|---|---|---|---|
| Mild < 0 mmHg | 3 (4·8%) | 0 (0·0%) | 2 (9·5%) | 1 (3·3%) |
| Medium 20 to < 40 mmHg | 35 (55·6%) | 4 (33·3%) | 7 (33·3%) | 24 (80·0%) |
| Strong 40 to < 60 mmHg | 17 (27·0%) | 5 (41·7%) | 7 (33·3%) | 5 (16·7%) |
| Very strong ≥ 60 mmHg | 8 (12·7%) | 3 (25·0%) | 5 (23·8%) | 0 (0·0%) |
| Total | 63 (100·0%) | 12 (100·0%) | 21 (100·0%) | 30 (100·0%) |
Figure 3.
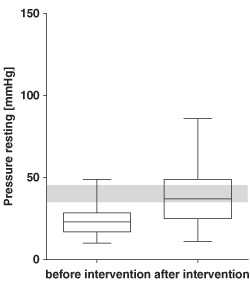
Box plot showing mean sub‐bandage pressure in supine position before (left) and after (right) intervention with the optimal range marked in grey.
Figure 4.

Box plot showing mean sub‐bandage pressure in active standing position, representing a good marker for the ‘working pressure’ before (left) and after (right) intervention with the optimal range marked in grey.
Before intervention, 17 of 22 insufficient bandages (77·7%) were applied by nurses having work experience above 10 years (Table 1) and after intervention only 1 of 11 insufficient bandages was applied by this group (Table 2).
The participants applied three consecutive compression bandages showing a mean intra‐individual variation of 6·9 mmHg in supine and 12·2 mmHg in active position.
The mean sub‐bandage pressure in supine position was recorded to be 23·9 mmHg before and 39·1 mmHg after the intervention (Figure 3). In active position, the optimal range was defined between 50 and 70 mmHg (5). The mean sub‐bandage pressure in active position, representing a good marker for the working pressure, was found to be at 38·7 mmHg before and 64·3 mmHg after the intervention (Figure 4).
Self‐assessment
Confidence about adequate pressure under the compression bandage was rated in average 3·72 points on a 1–10 scale (1 very confident and 10 unconfident) at baseline measurement. The assessment was taken before the first pressure measurements and the training interventions, showing that the nurses were over all confident to apply the adequate pressure with the compression bandages. After intervention and introduction of the pressure monitor the rating reached 3·29 points. The usefulness of the pressure monitor was rated in average 2·55 points on a 1–10 scale (1 very useful and 10 useless).
DISCUSSION
Compression is recognised as the single most effective treatment for venous leg ulcerations 2, 3. Healing is accelerated and recurrence of ulcerations is prevented by effective compression (1). The efficacy of compression bandaging highly depends on the skills of the individual applying it 18, 19. For the individual applying the compression bandage, however, it often remains uncertain whether the sub‐bandage pressure is adequate.
The introduction of objective devices to measure sub‐bandage pressure in combination with training showed improvement in the bandaging skills of nurses in former studies. Taylor et al. (19) reported to have improved the percentage of compression bandages with ’adequate’ and ’good’ compression levels from 50% to 81% by means of training using a pressure monitor for feedback. Similar results of training have been described by Hafner (8), Reynolds (18) and Nelson et al. (20). In our study, we were able to show that the effects of training and the use of a pressure monitor with inelastic bandages are comparable with the results presented in former studies in which elastic type bandages were used 18, 20.
However, the observed training effect could also be as a result of the ’Hawthorne effect', as participants were under observation and therefore in the centre of attention during the application of the compression bandages. Reports show that participants are prone to fall back into old habits under regular conditions (23). In this study, the follow‐up measurement was therefore performed 10–14 weeks after intervention and after extended training with the pressure monitor in the everyday setting, showing medium or strong sub‐bandage pressure (20–60 mmHg) in 82·6% after intervention. The long interval between introduction of the pressure monitor and the follow‐up reduces the influence of short‐term effects in this study. To maintain sustainable compression bandage quality, ongoing training and supervision is necessary.
Furthermore, the definition of adequate and optimal compression levels is still a matter of debate and differed in each study. In the present study, the optimal sub‐bandage pressure was defined between 35 and 45 mmHg in supine position, a widely accepted range for sufficient and save compression, which was also recommended in the recent consensus document on compression bandaging (7). The intervention leads to an increase in optimal sub‐bandage pressure (9·5% before intervention to 31·7% after intervention); 31·7% of bandages with optimal sub‐bandage pressure 10–14 weeks after intervention do not represent a fully satisfying result indicating that ongoing training is necessary to further improve the percentage. However, the number of insufficient compression bandages was reduced after training and introduction of a pressure monitor in the everyday routine (34·9% before intervention and 17·5% after intervention).
At baseline measurement, participants were asked to apply compression bandages in the way they do it in their everyday work regardless of the application technique. The participants chose the number of bandages needed and the technique by themselves. In between, two to three short stretch bandages were chosen and different multilayer bandaging techniques were applied. The participants were asked to perform three consecutive compression bandages using the same amount of bandages and the same compression technique (intra‐individual consistency). The sub‐bandage pressure measured in this study can be expected to represent sub‐bandage pressure similar to the pressure applied to patients in the everyday work, because the nurses were asked to use the same technique and the same amount of bandages as they do in everyday work.
The questionnaire showed that after the training the nurses chose a higher number of bandages to apply compression, indicating that the training and experience with an objective device lead to changed technique. The presented results underline that continuous training embedded in the everyday work is helpful to maintain adequate sub‐bandage pressure in everyday work.
In contrast to former studies measuring only one compression bandage applied by each participant, we were able to reduce the influence of outliers by asking to apply three consecutive compression bandages before and after intervention.
A mean intra‐individual variation of 6·9 mmHg in supine position and 12·2 mmHg in active position was measured underlining that even with training it remains difficult to reach a specific sub‐bandage pressure.
Most striking was the fact that in this study population before intervention 77·3% of the inadequate compression bandages were applied by nurses with work experience of more than 10 years. Long work experience does not necessarily stand for adequate sub‐bandage pressure. In the present study population especially this group was at risk to apply insufficient bandaging and therefore continuous awareness and training is essential to maintain sufficient sub‐bandage pressure.
Partsch et al. (12) show an average pressure loss of 25% within 30–60 minutes under compression bandages, depending on the materials used and the rate at which the oedema is reduced. After 3 hours, about 56% of the original sub‐bandage pressure remains (13). For this reason, Partsch (5) recommends to aim at achieving an initial sub‐bandage pressure of about 50 mmHg above the ankle or even higher when inelastic materials are used. The training phase therefore focused on adequate sub‐bandage pressure, the ability to detect ischemia and skills to prevent critically high compression. By introduction of an objective pressure monitor for practical training and by further theoretical training, these issues were addressed. The insufficient low sub‐bandage pressure (< 20 mmHg) was reduced from 34·9% before intervention to 4·8% after intervention. However, eight bandages (12·7%) were applied with a pressure above 60 mmHg after intervention. This might be because of the fact that the nurses felt secure to detect signs of ischemia after the training.
Many investigations in the past have measured sub‐bandage pressures in supine position only, although the ’working pressure’ is of much greater importance for the efficacy of a compression bandage. The measurement in active standing position can be expected to correlate with the ’working pressure’. The optimal ’working pressure’ is still a matter of debate. Partsch et al. 5, 10 show that 50–70 mmHg pressure are necessary to occlude veins in the upright position. In this study, the mean sub‐bandage pressure in active standing position increased from 38·7 mmHg before to 64·3 mmHg after the intervention. To be able to measure sub‐bandage pressure in resting (supine) as well as in active position, the sensor had to be placed 12 cm above the ankle to detect muscle‐dependent difference in compression 12, 22. The presented results give further information about sub‐bandage pressure in active position during muscular activity compared with measurement in supine position.
The correlation of the self‐assessment questionnaires and the actual sub‐bandage pressures measured show that in this population the nurses rate their competence regarding the sub‐bandage pressure in average 3·72 points on a 1–10 scale (1 very confident and 10 unconfident) at baseline measurement and therefore felt safe to apply adequate pressure. The self‐rating before intervention does not correlate well with the actual results of insufficient sub‐bandage pressure in 34·9%. On average after intervention 3·29 points were given, indicating that the nurses felt overall confident to apply sufficient sub‐bandage pressure. The results clearly show that self‐assessment and self‐control without an objective device to measure the pressure are not sufficient to evaluate bandaging skills.
CONCLUSION
Specific training programmes can help to improve confidence and competence concerning the application of compression bandages. Self‐rating alone is not sufficient to maintain adequate quality in compression therapy. A pressure monitor gives direct feedback on sub‐bandage pressure, an important aspect of an efficient compression bandage. All participants rated the use of a pressure monitor as a helpful or very helpful instrument for the training. Continuous awareness and ongoing training for nurses with short but also long work experience are essential to maintain adequate sub‐bandage pressure and therefore effective compression bandages in the everyday routine.
REFERENCES
- 1. Nelson EA, Bell‐Syer SE, Cullum NA. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev 2000;4:CD002303. [DOI] [PubMed] [Google Scholar]
- 2. Cullum N, Nelson EA, Fletcher AW, Sheldon TA. Compression for venous leg ulcers. Cochrane Database Syst Rev 2001;2:CD000265. [DOI] [PubMed] [Google Scholar]
- 3. Fletcher A, Cullum N, Sheldon TA. A systematic review of compression treatment for venous leg ulcers. BMJ 1997;315:576–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Damstra RJ, Brouwer ER, Partsch H. Controlled, comparative study of relation between volume changes and interface pressure under short‐stretch bandages in leg lymphedema patients. Dermatol Surg 2008;34:773–8; discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 5. Partsch H. Compression therapy of venous leg ulcers. Haemodynamic effects depend on interface pressure and stiffness. EWMA J 2006;6:16–20. [Google Scholar]
- 6. Clark M. Compression bandages: principles and definitions. In: Understanding compression therapy. EWMA Position Document; 2003;5–7. http://ewma.org/fileadmin/user_upload/EWMA/pdf/Position_Documents/2003/Spring_2003_English.pdf. [Google Scholar]
- 7. Partsch H, Clark M, Mosti G, Steinlechner E, Schuren J, Abel M, Benigni JP, Coleridge‐Smith P, Cornu‐Thénard A, Flour M, Hutchinson J, Gamble J, Issberner K, Juenger M, Moffatt C, Neumann HA, Rabe E, Uhl JF, Zimmet S. Classification of compression bandages: practical aspects. Dermatol Surg 2008;34:600–9. [DOI] [PubMed] [Google Scholar]
- 8. Hafner J, Botonakis I, Burg G. A comparison of multilayer bandage systems during rest, exercise, and over 2 days of wear time. Arch Dermatol 2000;136:857–63. [DOI] [PubMed] [Google Scholar]
- 9. Hafner J, Luthi W, Hanssle H, Kammerlander G, Burg G. Instruction of compression therapy by means of interface pressure measurement. Dermatol Surg 2000;26:481–6; discussion 7. [DOI] [PubMed] [Google Scholar]
- 10. Partsch B, Partsch H. Calf compression pressure required to achieve venous closure from supine to standing positions. J Vasc Surg 2005;42:734–8. [DOI] [PubMed] [Google Scholar]
- 11. Blair SD, Wright DD, Backhouse CM, Riddle E, McCollum CN. Sustained compression and healing of chronic venous ulcers. BMJ 1988;297:1159–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Partsch H. The static stiffness index: a simple method to assess the elastic property of compression material in vivo. Dermatol Surg 2005;31:625–30. [DOI] [PubMed] [Google Scholar]
- 13. Larsen A, Futtrup I. Watch the pressure—It drops. EWMA J 2004;4:625–39. [Google Scholar]
- 14. Palfreyman SJ, Lochiel R, Michaels JA. A systematic review of compression therapy for venous leg ulcers. Vasc Med 1998;3:301–13. [DOI] [PubMed] [Google Scholar]
- 15. Jünger M, Partsch H, Ramelet A, Zucarelli F. Efficacy of ready‐made tubular compression device versus short‐stretch compression bandages in the treatment of venous leg ulc. Wounds 2004;16:313–20. [Google Scholar]
- 16. Partsch H, Horakova MA. Compression stockings in treatment of lower leg venous ulcer. Wien Med Wochenschr 1994;144:242–9. [PubMed] [Google Scholar]
- 17. Feben K. How effective is training in compression bandaging techniques? Br J Community Nurs 2003;8:80–4. [DOI] [PubMed] [Google Scholar]
- 18. Reynolds S. The impact of a bandage training programme. J Wound Care 1999;8:55–60. [DOI] [PubMed] [Google Scholar]
- 19. Taylor AD, Taylor RJ, Said SS. Using a bandage pressure monitor as an aid in improving bandaging skills. J Wound Care 1998;7:131–3. [DOI] [PubMed] [Google Scholar]
- 20. Nelson EA, Ruckley CV, Barbenel JC. Improvements in bandaging technique following training. J Wound Care 1995;4:181–4. [DOI] [PubMed] [Google Scholar]
- 21. Rotsch C, Oschatz H, Möhring U, Rohrer C. Objektiver Vergleich von Kompressionsdrucksystemen für die Kompressionstherapie. Orthopädie-Technik 2005;11:789–93. [Google Scholar]
- 22. Partsch H, Clark M, Bassez S, Benigni JP, Becker F, Blazek V, Caprini J, Cornu‐Thénard A, Hafner J, Flour M, Jünger M, Moffatt C, Neumann M. Measurement of lower leg compression in vivo: recommendations for the performance of measurements of interface pressure and stiffness: consensus statement. Dermatol Surg 2006;32:224–32; discussion 33. [DOI] [PubMed] [Google Scholar]
- 23. Polit D, Beck C. Essentials of nursing research. Philadelphia: Lippincott Williams & Wilkins, 2001. [Google Scholar]


