Abstract
This study aimed to determine the predictive accuracy and factors deteriorating blanchable erythema. A prospective cohort study was conducted in a 832‐bed university hospital in Japan. Skin condition, risk factors, care plans and practices were measured everyday for 4 weeks by direct assessments and chart review by research staff. Blanchable erythema developed in 62 (24·9%) and a pressure ulcer in 8 (3·2%) patients. Six of the 62 blanchable erythema patients worsened to pressure ulcer of either stage I or II. Calculating the accuracy of blanchable erythema for predicting pressure ulcer development, sensitivity was 75%, specificity 77% and positive likelihood ratio 3·26. The factors found to deteriorate blanchable erythema were K‐scale ‘pressure’ and inadequate support surface management to a patient whose condition was deteriorating. These results suggested that the value of positive likelihood ratio means small effect to the clinical use. However, if adequate support surface management were implemented to blanchable erythema patients, the incidence of pressure ulcer would probably fall to 0·8%.
Keywords: Blanchable erythema, Cohort study, Pressure ulcer, Risk factors
Introduction
Recently, early identification of pressure ulcer has been emphasised, because it can prevent skin alteration progressing to skin loss. Several studies focused on non blanchable erythema as the early identification of pressure ulcer and investigated the factors for developing into more severe pressure ulcers 1, 2, 3. Researchers consider that persistent redness over a bony prominent area, especially blanchable erythema is the first clinical sign of pressure ulcer development. Detecting the blanchable erythema is expected to provide appropriate care to prevent even stage I pressure ulcer, i.e. non blanchable erythema development at this stage. There have been a few studies on whether the blanchable erythema can predict the pressure ulcer development.
Incidence of blanchable erythema and deterioration rate to pressure ulcer were reported in a randomised clinical trial comparing support surfaces on surgical patients (4). This study adopted conditions that were manipulated for experimental purposes and enrolled a limited group of subjects. In another study, incidence rate of erythema and pressure ulcer development were reported according to incontinence severity (5). Erythema could also have been a sign of incontinence‐related contact dermatitis. Therefore, development of blanchable erythema, which is assumed to be caused by pressure could not be accurately evaluated. Moreover, no studiy has clarified the factors related to the deterioration of blanchable erythema.
The purpose of this study was to determine the predictive accuracy of blanchable erythema and prospectively identify the factor related to their deterioration.
Materials and methods
Research design
This was a prospective cohort study. The research team consisted of a total of 12 individuals, including two WOC nurses, two university faculty members who specialised in wound care and nine Masters course students who majored in wound care and routinely observed skin conditions. Researchers were trained in skin observation and survey methods prior to the initiation of the study.
Setting and subjects
Subjects consisted of patients who were admitted to six wards in a university hospital with 832 beds (Ishikawa, Japan) between February and April 2005. Six wards were ICU, surgical recovery room, gastroenterological surgery and medicine, internal medicine and cardiovascular and respiratory surgery. These were selected, as three had the highest percentages of bedridden patients, and the other three had the lowest percentages. All subjects were required to be free of pressure ulcers at the beginning of the study and spent most of the day in bed.
Accuracy of blanchable erythema for predicting pressure ulcer development
A pair of researchers directly observed the skin condition of subjects daily, and recorded the presence of blanchable erythema and pressure ulcers, location, date of development and date of healing. To assess for blanchability, researchers pressed firmly on the skin with a finger and lifted the finger and looked for blanching (sudden whitening of the skin), followed by prompt return of colour to the area. Pressure ulcers were defined by using the National Pressure Ulcer Advisory Panel classification (6). Based on this observation record, the probability of blanchable erythema resulting in pressure ulcer development was calculated in terms of sensitivity, specificity and positive likelihood ratio and diagnostic accuracy was examined. In the statistical methods, diagnostic probabilities (sensitivity, specificity and positive likelihood ratio) were used to calculate. The LR is used to assess how good a diagnostic test is.
Deteriorating factors involved in the progress from blanchable erythema to pressure ulcer
Data collected included demographic information; diagnoses; a K‐score for predicting pressure ulcer risk; care processes related to pressure ulcer prevention (skin integrity assessment, pressure ulcer risk assessment, use of support surfaces, maintenance of support surfaces, repositioning schedule, maintain the head of the bed at 30°C or below, protect for the skin over the extreme bony prominence, documentation of pressure ulcer risk and care plan, skin care, nutritional assessment and management). The Kanazawa University Pressure Ulcer Predictive Scale (K‐scale) assesses the following two risk factor groups: underlying risk factors and trigger factors. Of these two factors, former involved immobility, bony prominence and malnutrition and the latter involved interface pressure, skin moisture and shear. Each risk factor is answered with Yes or No, and one point given for a Yes answer and zero point for No answer. Potential scores range from 0 to 6. The higher the score is, the higher is the risk. K‐scale is used at a patient’s admission to the health‐care facility and whenever a significant change occurs in the patient’s general health and status. This scale has undergone testing in elderly and reliability and validity have been established (7).
These data were collected by the direct observation and medical and nursing record review. Subjects who had blanchable erythema, which resulted in pressure ulcer development, were classified as the deteriorated group and those who had no pressure ulcer development were classified as the healed group. We compared each type of data between the two groups.
Ethical considerations
The purpose of the present study was explained to the director of nursing in the hospital both orally and in writing and permission for conducting the study was obtained. After informed consent was obtained, the patients were included in the study. In case of difficulty in verbal communicating, consent was obtained from his/her family. When investigating the skin, we confirmed the medical condition of the patients. The study protocol conformed to the ethical guidelines of the Japan Ministry of Health, Labour and Welfare. Development of pressure ulcers of stage I and above and other problems were reported to staff nurses for the safety of patients.
Statistics
To compare each parameter between the healed and the deteriorated groups, the chi‐squared test and Mann‐Whitney U test were performed using SPSS II for Windows for statistical analysis. P < 0·05 was considered statistically significant.
Results
Incidence of blanchable erythema and consequences
The total number of inpatients during the survey period was 493. A total of 15 were excluded from the subject group; eight patients with pressure ulcers and seven because of deterioration of medical condition of the patients. Among the remaining 478, 229 were able to walk and 249 spent most of each shift in bed (Figure 1). Among these 249 bedridden subjects, blanchable erythema was observed in 62 (24·9%), six of whom (9·7%) developed pressure ulcer, (stage I, n = 3; stage II, n = 3). All pressure ulcers were partial thickness wounds and eventually healed. On the other hand, among the 187 patients without blanchable erythema, pressure ulcer development was observed in two (1·1%; stage I, n = 1; stage II, n = 1). These ulcers also eventually healed (Figure 1). Hence, of the 249 bedridden patients, pressure ulcer development was observed in a total of eight (3·2%).
Figure 1.
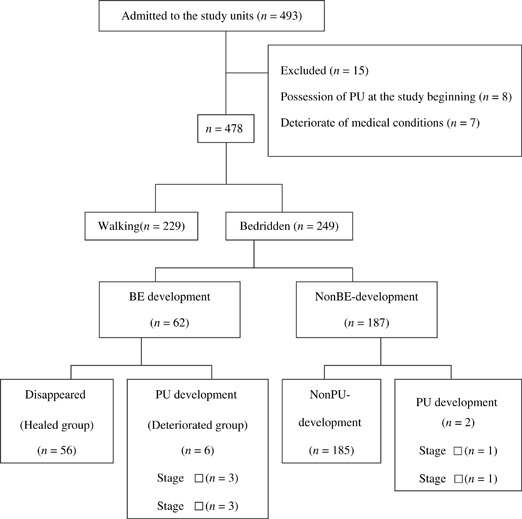
Flow of patients through the study PU, pressure ulcer; BE, blanchable erythema.
Accuracy of blanchable erythema for predicting pressure ulcer development
Based on the 2 × 2 contingency table, sensitivity, specificity and positive likelihood ratio were 75%, 77%, and 3·26, respectively (Table 1).
Table 1.
Accuracy of BE as a predictor of PU development
| PU development | Non PU development | Total | |
|---|---|---|---|
| With BE | 6 | 56 | 62 |
| Without BE | 2 | 185 | 187 |
| Total | 8 | 241 | 249 |
BE, blanchable erythema; PU, pressure ulcer.
Deteriorating factors
No significant differences were observed regarding demographic information and diagnoses (Table 2). However, the number of patients who had a risk under the item ‘pressure’, which is one of the triggering factors in the K‐scale for predicting pressure ulcer development, was significantly higher in the deteriorated group (Table 3) (χ2=4·277, P = 0·039). Inadequate maintenance of support surfaces was observed in all six patients in the deteriorated group (χ2=0·228, P = 0·015; Table 4).
Table 2.
Deteriorating factors to pressure ulcer in demographic information
| Deteriorating factors | Deteriorated group n = 6 | Healed group n = 56 | U value | P value |
|---|---|---|---|---|
| Age 1 | 69 (21–78) | 74 (12–90) | 134.5 | 0.425 |
| χ2 value | P value | |||
| Gender | ||||
| Male | 5 | 31 | 1.742 | 0.187 |
| Female | 1 | 25 | ||
| Diagnosis | ||||
| Cardiovascular disease | 1 | 21 | ||
| Orthopaedic disease | 4 | 12 | ||
| Digestive disease | 0 | 14 | ― | |
| Respiratory disease | 0 | 3 | ||
| Urological disease | 1 | 1 | ||
| Others | 0 | 5 | ||
Values represent mediam with range.
Statistical analysis could not be conducted because of small samples.
Table 3.
Deteriorating factors to pressure ulcer in k‐scale
| Sub scale | Deteriorated group n = 6 | Healed group n = 56 | χ value | P value | ||
|---|---|---|---|---|---|---|
| Risk factors | ||||||
| Yes | No | Yes | No | |||
| Immobility | 5 | 1 | 29 | 27 | 2.178 | 0.140 |
| Bony Prominence | 3 | 3 | 11 | 45 | 2.857 | 0.091 |
| Malnutrition | 2 | 4 | 38 | 18 | 2.822 | 0.093 |
| Pressure | 5 | 1 | 22 | 34 | 4.277 | 0.039 |
| Moisture | 0 | 6 | 19 | 37 | 2.935 | 0.087 |
| Shear | 2 | 0 | 39 | 17 | 2.510 | 0.113 |
Table 4.
Inappropriate selection of support surfaces
| Deteriorated group n = 6 | Healed group n = 56 | χ value | P value | |
|---|---|---|---|---|
| Appropriate | 0 | 30 | 0.228 | 0.015 |
| Inappropriate | 6 | 26 | ||
Discussion
Despite the potential important clinical implications of persistent redness, identification and diagnosis of these lesions may be difficult for nurses. This study was unique in that pairs of researchers, who specialised in wound care and were not involved in management of the hospital wards surveyed, directly observed the skin of 249 bedridden patients every day. The present study provided highly reliable data, which thoroughly followed the course of blanchable erythema from development to outcome in 62 patients. Furthermore, the present study was noteworthy in revealing the factors affecting the course of blanchable erythema in its deterioration to pressure ulcer. Knowing the clinical course of blanchable erythema is essential for their appropriate management and to reduce the pressure ulcer incidence rate.
Consequences of blanchable erythema
Detection of non blanchable erythema has been reported the effectiveness for prevention of partial thickness wound‐type pressure ulcer development 1, 2, 8. Rates of non blanchable erythema deterioration to stage II and deeper were 35·5% among the bedridden elderly in Japan (1) and 59·8% among surgical inpatients (2). On the other hand, the rates of blanchable erythema deterioration were 4·8% in our study. These results suggested that detecting the blanchable erythema is more effective for prevent the pressure ulcer development of stage II and deeper. Although some have suggested that it is difficult to distinguish between blanchable erythema and healthy skin 9, 10, 11, non blanchable erythema is defined as a stage I pressure ulcer in the Agency for Health Care policy and Research classification(12) and skin integrity is already impaired at this stage. Therefore, in order to avoid impairment to the patients’ health, it was considered necessary to provide pressure ulcer prevention care, which also targets non blanchable erythema.
The sensitivity, specificity and positive likelihood ratio for the probability of blanchable erythema resulting in pressure ulcer were 75%, 77% and 3·26, respectively. This sensitivity and specificity indicated high diagnostic accuracy. On the basis of our results, the value of positive likelihood ratio means small effect to the clinical use (LR 3·26)(13). However, it appears meaningful in this university hospital with eight cases of pressure ulcer development and the incidence rate was 3·2%. If nurses had detected blanchable erythema and provided pressure ulcer prevention care, it might be possible to reduce the incidence of pressure ulcer from 3·2% to 0·8%. Thus, detection of blanchable erythema is assumed to be useful for prevention of pressure ulcer development.
Deteriorating factors of blanchable erythema to pressure ulcer
Based on the univariate analysis, it was assumed that the factors that were involved in pressure ulcer development were ‘pressure’ on the K‐scale and ‘inappropriate selection of support surfaces’. ‘Pressure’ can become a risk factor when pressure redistribution care cannot be provided to the patients regularly by the nurses or caregiver because of deterioration of medical condition of the patients, such as shock or increased pain. Therefore, it was assumed that appropriate position change was not provided upon development of blanchable erythema and that this resulted in pressure ulcer development. It was also assumed that nurses’ ignorance of support surface selection in the care programme. Necessity of educational programme to understand the selection of support surface in the care programme.
Limitation and further research
As only six subjects had blanchable erythema that progressed to pressure ulceration in the present study, it is necessary to extend the survey period and to increase the number of cases by conducting surveys at other facilities. Moreover, most of the patients of this study were postoperative patients who had indwelling urinary catheters and no faecal incontinence. Further study of incontinent subjects with moisture problems that contribute to pressure ulcer development by macerating the skin is needed.
Conclusion
Based on these results, the accuracy of blanchable erythema for predicting pressure ulcer development, sensitivity was 75%, specificity 77% and positive likelihood ratio 3·26. The factors found to deteriorate blanchable erythema were K‐scale ‘pressure’ and inadequate support surface management to a patient whose condition was deteriorating. It was considered important to confirm appropriate use and selection of support surfaces if patients develop blanchable erythema, even in the absence of moisture as a risk factor, in order to prevent development of pressure ulcers including stage I pressure ulcers.
References
- 1. Sato M, Sanada H, Konya C, Sugama J, Nakagami G. Prognosis of stage I pressure ulcers and related factors. Int Wound J 2006;3:355–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nixon J, Granny G, Bond S. Skin alterations of intact skin and risk factors associated with pressure ulcer development in surgical patients: A cohort study. J Nurs Stud. 2007;5:655–663. [DOI] [PubMed] [Google Scholar]
- 3. Linddgre M, Malmquvist L‐A, Sjoberg F, Ek A‐C. Alterd skin blood perfusion in areas with non blamchable erythema: an explorative study Int Wound J 2006;3:215–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Russell L, Reynolds T, Park C, Rithalia S, Gonsalkorale M, Birch J, Torgerson D, Iglesias C. Randomized clinical trial comparing 2 support surfaces results of the prevention of pressure ulcers study. Adv Skin Wound Care 2003;16:317–27. [DOI] [PubMed] [Google Scholar]
- 5. Schnelle J‐F, Adamson G‐M, Cruise P‐A, Samarrai N‐A, Sarbaugh F‐C, Uman G, Ouslander J‐G. Skin disorders and moisture in incontinent nursing home residents: intervention implications. JAGS 1997;45:1182–8. [DOI] [PubMed] [Google Scholar]
- 6. Wound Ostomy and Continence Nurses Society . Guideline for prevention and management of pressure ulcers. Glenview, IL, Wound, Ostomy and Continence Nurses Society, 2003. [DOI] [PubMed] [Google Scholar]
- 7. Okuwa M, Sanada H, Sugama J, Konya C, Matui Y, Koshimura J, Nagakawa T. The reliability and validity of the K scale for predicting pressure ulcer development for elderly. Jpn J Press Ulcers 2001;3:7–13. [Google Scholar]
- 8. Allman R‐M, Goode P‐S, Patric M‐M, Burst N, Bartolucci A‐A. Pressure ulcer risk factors among hospitalized patients with activity limitation. JAMA 1995;273:865–70. [PubMed] [Google Scholar]
- 9. Bates‐Jensen BM, Sussman C: Tools to measure wound healing. In: Bates‐Jensen BM, Sussman C, editors. Wound care, 2nd edn. Maryland: Aspen publishers, 2001:147–8. [Google Scholar]
- 10. Russell R: Pressure ulcer classification, defining early skin damage. Brit J Nurs 2002;11:S33–41. [DOI] [PubMed] [Google Scholar]
- 11. Witowski JA, Parish LC.: Histopathological of the decubitus ulcer. J Acad Dermatol 1982;6:1014–21. [DOI] [PubMed] [Google Scholar]
- 12. Agency for Health Care Policy and Research (AHCPR) . Pressure sores in adults: prediction and prevention. Clinical Practice Guidelines, No. 3. Rockville, MD: U.S. Department of Health and Human Services, 1992. [Google Scholar]
- 13. Indra R, Patil S‐S, Joshi R, Pai M, Kalantri S‐P. Accuracy of physical examination in the diagnosis of hypothyroidism:a cross‐sentinal, double‐blind study. JPGM 2004;50:7–10. [PubMed] [Google Scholar]


