Abstract
Aim
The present study was carried out as a comparative observational study in order to determine the effect of prophylactic dressing on the prevention of skin injuries due to the use of personal protective equipment (PPE) in health care workers (HCWs) working with COVID-19 patients. In addition, the effect of nasal strip on the prevention of discomfort in breathing with mask was also investigated.
Materials and methods
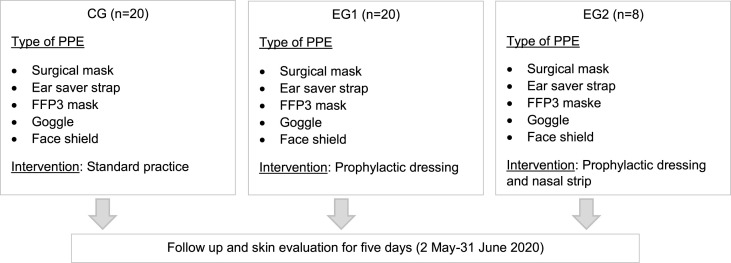
The present study was carried out with 48 HCWs (Control Group-CG, n = 20; Experimental Group 1-EG1, n = 20; Experimental Group 2-EG2, n = 8) who use PPE on the face region and work with COVID-19 patients. Data was collected with Data Collection Form developed by researchers. In participants in CG, normal procedures of the institution in using PPE were followed. In EG1, prophylactic dressing was used on risky areas on the face. In EG2, nasal strip sticky on one side was used in addition to prophylactic dressing. The evaluation of the facial skin was made once a day by a researcher with expertise in wound management.
Results
Groups were similar in terms of demographic characteristics of participants. Overall rate of skin injuries associated with PPE use was 47.9%. Skin injuries developed in all participants in CG (n = 20), and in two and one participants in EG1 and EG2 respectively, with significant difference between groups. The most common skin injuries were Stage 1 pressure injury (29.2%), blanchable erythema of intact skin (27.1%) and itching (18.8%). No participant in EG2 reported discomfort in breathing (n = 8). Significant difference was found between groups in favor of EG2 in terms of experiencing discomfort in breathing (p < 0.001).
Conclusions
In the present study, it was established that using prophylactic dressing under PPE prevents skin injuries on the facial skin and using nasal strip prevents discomfort in breathing with mask. In view of these results, it was recommended that prophylactic dressing should be used under PPE.
Keywords: Personal protective equipment, Pressure injuries, Skin injuries, COVID-19, Prophylactic dressing
1. Introduction
Skin is the largest organ of our body protecting the body from outside agents and has important functions. Various internal and external factors such as mechanic, chemical and physical trauma, surgical intervention, long term pressure, ischemia, and acute and chronic diseases may impair the integrity of structures making up the skin. Impairment in skin integrity may present with abrasions, skin tears, infection, rash, discoloration, and open ulcer [3,25]. One of the autonomous responsibilities of the nurse is the maintenance of the skin and tissue integrity. Pressure injuries (PIs) are one of the issues that are documented most commonly in the literature in the framework of this responsibility [2,23,30].
A special sub-group of PIs includes device-related pressure injuries (DRPIs). DRPIs can be defined as injuries resulting from pressure, friction and shear caused by devices designed and used for diagnostic or therapeutic purposes in health care [4,7]. Non-medical devices and objects, which have contact with skin and tissues may also cause DRPIs. The injury is consistent with the shape of the device used. Characteristics of devices (e.g. materials used in their composition, size, shape, region used, duration of use) also play crucial part [7,9]. International Consensus Document (2020) [9] states that main etiological factor for development of DRPIs is frictional force caused by medical devices or other objects in contact with skin and mucosa [9]. In addition to frictional force, accompanying sustained shear leads to skin and tissue damage [11]. It is suggested that DRPIs should be classified using a recognized classification system [6,7].
Although DRPIs are common problem in different health care settings, interestingly literature on this issue is more focused on patients, and data are more limited than that on PIs in general [28]. Also, DRPIs were not commonly investigated in health care workers (HCWs) until the breakout of COVID-19 pandemic in Wuhan region of China in December 2019, which spread uncontrollably all over the world, but from then on, it became a very conspicious issue on media with various skin manifestations on the face of HCWs and all people became aware of its presence. It was also reported that in HCWs giving care to constantly increasing intensive care patients diagnosed with COVID-19 and trying to protect them from DRPIs, the rate of DRPIs associated with personal protective equipment (PPE) use was extremely high [10,15,16].
In the multi-centered cross-sectional survey study of Jiang et al. (2020) [15] in China (n = 4.306), the rate of PPE associated skin injuries was found to be 42.8%. In their study, types of skin injuries were categorized into PIs (30.0%), moisture-associated skin damage (10.8%) and skin tears (2.0%), and regions of injury were reported to be nasal bridge (30.1%), cheek (28.3%), ear (25.3%) and forehead (14.8%). In the same study, the distribution of PIs was 81.1% Stage 1 PI, 18.3% Stage 2 PI, and 0.6% Deep Tissue PI respectively [15]. Lam et al. (2020) [19] in Malaysia (n = 5), reported PI cases on nasal bridge (Stage 1 PI, n = 4 and Stage 3, n = 1) associated with N95 mask use in HCWs who work in intensive care units [19].
It was stated that HCWs encounter other skin problems in associated with PPE use such as surgical mask, N95 mask, FFP2 mask, FFP3 mask, face shield, goggle, gloves employed for infection control [8,10,14,15]. For example, in a study performed on HCWs in an acute care hospital in Singapur in 2003 during SARS epidemic (n = 322), it was reported that regular use of N95 mask led to problems such as acne (59.6%), itching on the face (51.4%) and rash (35.8%) [8]. In the descriptive survey study of Hu et al. (2020) [14] in a state hospital in China, during COVID-19 pandemic (n = 61), it was reported that of HCWs who use N95 mask, 68.9% experienced injury on nasal bridge and 27.9% itching on the face [14]. Atzori et al. (2020) [1] in a dermatology clinic in Italy during COVID-19 pandemic, reported that they experienced an increased number of consultations for contact dermatitis and skin injuries by HCWs. In this report, the most affected sites included the nasal bridge, hands, cheek, periocular and perioral regions. Most common sypmtoms were dryness, itching and stinging sensations [1].
However, it can be observed that there was not much progress in the development of protective materials between two epidemics, although loss of integrity of skin due to PPE use renders HCWs more susceptible to infection. In addition, working in PPE for hours and fear of getting COVID-19 infection and transmitting it to loved ones leads to further stress, exerting negative impact on defense systems of HCWs [10,35]. HCWs experience many other problems in addition to skin injuries such as fogging in goggles and face shields, excessive sweating, discomfort in breathing, and having difficulty in meeting basic needs such as nutrition and excretion [16,32,35]. Therefore, professional organizations developed training documents and algorhythms to protect HCWs from PPE associated DRPIs and others skin problems in many countries [10,20,27]. The Wound Management Association of Turkey (WMA-T) and Wound Ostomy Continence Nurses Society of Turkey (WOCNS-T) prepared a mutual algorhythm [34] and shared it with all HCWs across the country. The most important challenge in this issue is the fact that evidence-based interventions and recommendations are limited, and the knowledge in the literature is based on expert opinions. Recommendations mostly are based on the interpretation of the information on etiology and development mechanism of DRPIs in the context of PPE [10,20,27].
The mechanisms playing part in the etiology of PPE associated DRPIs are as follows; the face mask materials, with their comparatively stiff flange and straps and the near rigid goggle frames mechanically indent and damage facial skin. In addition, continuous static and dynamic frictional forces, cause notable shearing in skin and subdermal tissues. Finally, excessive sweating and accumulating moisture on the facial skin due to work stress caused by heavy work load and working with PPE leads the stratum corneum to soften and increase co-efficient of friction. Another factor is that mask and goggles used are produced in standard size and do not fit all HCWs with different facial size and shapes [10,12,16,31]. Moreover, they have not been designed for long term use [33,35]. Therefore, HCWs may adjust PPE too tightly in order to keep them in place [12].
For the prevention of PPE associated DRPIs, it has been recommended that before putting on medical mask sensitive face regions should be cleaned and dried, skin moisture should be maintained. If the equipment will remain in place for a long period of time, barrier skin wipe/protectant should be applied to face in order to prevent friction [10,20,27,35]. Although its has been stated in DRPIs International Consensus Document (2020) [9] that placement of prophylactic dressings under stiff devices will decrease the risk of DRPIs [9]. It was demonstrated that if these prophylactic dressings are placed under devices after being cut to shape, they reduce skin deformations formed by the contact between the skin and the device [31]. In the laboratory study of Peko Cohen et al. (2019) [29], they examined by using finite element method the effect of the prophylactic dressings cuts under the non-invasive ventilation mask against compressive and frictional forces. They reported that the use of prophylactic dressing cuts was biomechanically effective in reducing exposure of facial tissues to elevated mechanical loads [29].
However, at present there are no ready to use specific prophylactic dressings, whose biomechanical characteristics have been tested in laboratories in wound care industry. Using available wound dressings for this aim utilizing some of their characteristics such as (flexibility, decreasing pressure by functioning as a pillow, preventing friction, being cut according to face contours, being applied without harming sensitive regions, removing heat and moisture from skin, positive contribution to microclimate will contribute to their being tested and to the production of special prophylactic dressings directly aiming the prevention of DRPIs. Yet, the difficulty of well structured and designed experimental studies with HCWs working at the front line of COVID-19 pandemic struggle is obvious. Furthermore, universities and research centers are closed or work limitedly, which also hinder such studies. Considering these difficulties, Gefen and Ousey (2020) [13], stated that due to growing need to maintain skin integrity during global emergency public health crises, such as COVID-19 pandemic, HCWs should be considered to use interventions that have been proven to work through laboratory evidence and clinical experience [13].
In addition to the aforementioned literature, our observations indicated that HCWs working in diagnosis, treatment and care of COVID-19 are in need of information and support regarding the prevention of skin injuries developing on the face region after long term intensive use of PPE and of breathing difficulties they experience. Considering that studies on this issue will contribute to the development of prevention strategies in daily clinical routine and new technological products, we attempted to investigate the effect of a kit, which we produced with prophylactic dressing, ear saver strap and nasal strip, and termed as ‘‘face protection kit for HCWs'’ on the prevention of PPE associated skin injuries and PIs. An important contribution of the present study to the literature may be that the effect of nasal strip on comfortable breathing of HCWs with mask was evaluated.
2. Materials and methods
2.1. Study design
The present study was designed as a comparative observational study in order to determine the effect of face protection kit (prophylactic dressing, nasal strip and ear saver strap) on the prevention of facial skin injuries and PIs associated with PPE use and breathing comfort in HCWs working in the diagnosis, treatment and care of COVID-19 patients.
2.2. Hypotheses of the study
-
1.
Using prophylactic dressing and ear saver strap exerts effect on the prevention of skin injuries and PIs associated with PPE use in HCWs.
-
2.
Using prophylactic dressing, nasal strip and ear saver strap exerts effect on the prevention of skin injuries and PIs and in helping HCWs to breathe more comfortably.
2.3. Participants
Purposeful sampling method was used in the determination of study participants. 48 HCWs (Control Group-CG, n = 20; Experimental Group 1-EG1, n = 20; Experimental Group 2-EG2, n = 8) who worked in the diagnosis, treatment and care of COVID-19 patients in a training and research hospital in Ankara with 250 bed capacity and volunteered to enter the study. HCWs were randomly allocated to groups by the reseacher using their work shift list.
2.4. Ethical considerations
Prior to the study, ethical permission was obtained from Republic of Turkey Ministry of Health, Scientific Researches Platform, with the approval dated May 02, 2020 and numbered 2020-05-02T09_49_46. Participants volunteering to participate in the study were informed and their verbal consent was obtained.
2.5. Data collection tool
In the collection of data, Data Collection Form developed by researchers in view of the literature was used [9,17,26]. Data Collection Form consists of two parts. In the first part, questions on demographic characteristics of HCWs and their experiences and opinions regarding PPE were asked (7 questions). In the second part of the form, types and location of skin injuries associated with PPE were questioned. In this part, skin injuries were tabulated. In the left column, type of injury and in the right column, description, explanation and location of injury (forehead, nasal bridge, right cheek, left cheek, right ear, left ear, chin, posterior part of the head) were shown. Skin injuries were grouped as follows; blanchable erythema of intact skin, rash, itching, skin lesions (papule, pustule etc.) and PIs. PIs were classified according to National Pressure Injury Advisory Panel (NPIAP) PI staging system as Stage 1 PI, Stage 2 PI, Stage 3 PI, Stage 4 PI, Unstageable PI, Deep Tissue PI. With an additional question, the satisfaction level of HCWs in associated with PPE were evaluated with Visual Analogue Scale (VAS) between 1 and 10 point (1:I am not satisfied at all and 10: I am very satisfied).
2.6. Implementation and data collection method
The study was carried out between May 2-June 31, 2020. HCWs working actively in diagnosis, treatment and care of COVID-19 patients and using PPE on their face region were randomly allocated into the study groups. In the first page of Data Collection Form, an explanation was offered to the participants including information on the aim of study, volunteer participation, the fact that they can withdraw from the study whenever they want and communication information for contact with researchers.
Participants in CG followed normal procedures of the institution when using PPE. No special training or intervention was offered to CG. Since the routine procedure of the institution included the utilization of ear saver strap (Ear Saver Strap for Mask, Genç Kalıp Plastik Limited Company, Manisa/Turkey) in order to prevent friction on ears caused by mask ties and to support complete fitting of the mask on the face, they used only this device (Fig. 1 ).
Fig. 1.

Ear saver strap.
Participants in EG1 used prophylactic dressing (Mepilex® Lite and Mepilex® Lite Border with Safetac® technology, Mölnlycke Health Care AB/Sweden) along with ear saver strap. Prophylactic dressing was used in accordance with the instructions of the manufacturer [22] and with DRPIs prevention algorhythm [34] after being cut to shape by participants themselves at a width and length corresponding to their own facial measurements.
Participants in EG2 used nasal strip with sticky one side on nasal region (Breathe Right® nasal strips, GlaxoSmithKline, London/UK), and prophylactic dressing cut to shape and ear saver strap on the other parts of the face (Fig. 2 ).
Fig. 2.
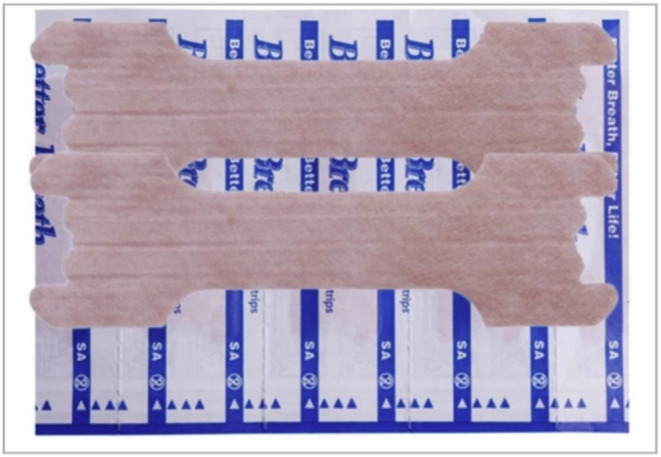
Nasal strips.
Participants in the EG1 and EG2 were given PPE associated DRPIs prevention algorhythm developed by WMA-T and WOCNS-T [34] and were asked to protect their skin accordingly. Participants were informed individually for applying prophylactic dressing to the regions on their face, which have contact with PPE (forehead, nasal bridge, cheeks and chin) in order that they can cut dressing in accordance with the instructions of the manufacturer [22] and algorhythm [34] and with specimens of cut dressings in practice guidelines issued on this subject [20]. Prophylactic dressings were cut to shape were applied to the face of participants involving forehead, chin, nasal bridge and cheeks prior to the use of PPE (mask, face shield, goggle).
All participants in the study used goggle, face shield, surgical mask and FFP3 mask together as standard PPE. Evaluation of the facial skin in participants from all three groups was made by a researcher with expertise in wound management once daily at the end of work shift or whenever it was convenient for the participant and recorded in Data Collection Form. When PI was detected at the evaluation, it was classified according to NPIAP PI staging system [7,26]. Each HCW was followed up for at least 24 h and for maximum five days (Fig. 3 ).
Fig. 3.
Research scheme.
2.7. Data analysis
In the analysis of data, IBM SPSS Statistics for Windows, Version 26.0 (Armonk, NY: IBM Corp., 2019) software was used. In descriptive statistics, categorical data were expressed with frequency and percentage, and continuous numerical data with mean and standard deviation. Whether the data were distributed normally was evaluated with Shapiro-Wilk Test. In the comparison between study groups, continuous numerical data, which are not normally distributed were evaluated with Kruskal-Wallis Test [5,24] and categorical data with Likelihood Ratio [21]. p value of <0.05 was considered statistically significant.
3. Results
3.1. Characteristics of the study participants
Of overall 48 participants in the study, 89.6% (n = 43) was female and 72.9% (n = 35) was nurse while 18.8% (n = 9) was physician. All participants worked in a in-patient clinic and/or out-patient clinic serving COVID-19 patients. Their mean age was x̄ = 34.21 ± 6.02, and mean duration of work was x̄ = 12.5 ± 5.55 years. There was no difference between the groups in terms of demographic characteristics of the participants (Table 1 ).
Table 1.
Demographic characteristics of the study participants.
| Demographic characteristics | CG |
EG1 |
EG2 |
Overall |
Test |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | Value | p | |
| Sex | ||||||||||
| Male | 4 | 20.0 | 1 | 5.0 | 0 | 0.0 | 5 | 10.4 | a4.121 | 0.127 |
| Female | 16 | 80.0 | 19 | 95.0 | 8 | 100.0 | 43 | 89.6 | ||
| Occupation | ||||||||||
| Nurse | 13 | 65.0 | 15 | 75.0 | 7 | 87.5 | 35 | 72.9 | a8.140 | 0.420 |
| Physician | 5 | 25.0 | 3 | 15.0 | 1 | 12.5 | 9 | 18.8 | ||
| c Other | 2 | 10.0 | 2 | 10.0 | 0 | 0.0 | 4 | 8.0 | ||
| x̄ ± SD | x̄ ± SD | x̄ ± SD | x̄ ± SD | |||||||
| Mean age (years) | 33.30 ± 6.87 | 35.15 ± 5.60 | 34.13 ± 4.99 | 34.21 ± 6.02 | b0.764 | 0.682 | ||||
| Mean duration of work (years) | 11.50 ± 6.08 | 12.55 ± 5.53 | 12.75 ± 4.62 | 12.15 ± 5.55 | b0.392 | 0.822 | ||||
Likelihood Ratio.
Kruskal-Wallis Test.
Others (Emergency medicine technician, auxiliary support personnel and medical secretary).
3.2. Experiences of the study participants with PPE
Mean duration of PPE use was x̄ = 3.79 ± 1.18 h. No significant difference was found between CG (x̄ = 3.5 ± 0.88), EG1 (x̄ = 4.0 ± 1.58) and EG2 (x̄ = 4.0 ± 0.00) with respect to mean duration of PPE use (p = 0.361). 97.9% of the participants reported that they experienced fogging in goggle and face shield, 97.9% perspiration and moisture on mask, and 81.3% discomfort in breathing. None of the participants in EG2 (n = 8) experienced discomfort in breathing (p < 0.001). Mean satisfaction scores with PPE were x̄ = 5.04 ± 2.44 (CG x̄ = 2.40 ± 1.23, EG1 x̄ = 6.80 ± 0.69 and EG2 x̄ = 7.25 ± 0.70). There was significant difference between groups, which was in favor of experimental groups (p < 0.001) in terms of satisfaction score (Table 2 ).
Table 2.
Distribution of the informations on PPE use in health care workers.
| Informations on PPE use | CG |
EG1 |
EG2 |
Overall |
Test |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | Value | p | |
| Problems experienced with PPE | ||||||||||
| Fogging in goggles | 19 | 95.0 | 20 | 100.0 | 8 | 100.0 | 47 | 97.9 | a1.781 | 0.410 |
| Fogging in face shield | 19 | 95.0 | 20 | 100.0 | 8 | 100.0 | 47 | 97.9 | a1.781 | 0.410 |
| Perspiration and moisture | 19 | 95.0 | 20 | 100.0 | 8 | 100.0 | 47 | 97.9 | a1.781 | 0.410 |
| Discomfort in breathing | 19 | 95.0 | 20 | 100.0 | 0 | 0.0 | 39 | 81.3 | a38.387 | <0.001 |
| No problem experienced | 1 | 5.0 | 0 | 0.0 | 0 | 0.0 | 1 | 2.1 | a1.781 | 0.410 |
| Number of participants with skin injuries associated with PPE | 20 | 100.0 | 2 | 10.0 | 1 | 12.5 | 23 | 47.9 | a47.427 | <0.001 |
| Number of participants with multiple skin injuries associated with PPE | 16 | 80.0 | 0 | 0.0 | 0 | 0.0 | 16 | 33.3 | a41.089 | <0.001 |
| x̄ ± SD | x̄ ± SD | x̄ ± SD | x̄ ± SD | |||||||
| Mean number of skin injuries associated with PPE | 2.45 ± 0.24 | 0.10 ± 0.06 | 0.13 ± 0.12 | 1.08 ± 1.18 | a55.678 | <0.001 | ||||
| Mean duration of PPE use (hours) | 3.5 ± 0.88 | 4.0 ± 1.58 | 4.0 ± 0.00 | 3.79 ± 1.18 | b2.036 | 0.361 | ||||
| Mean satisfaction score of PPE | 2.40 ± 1.23 | 6.80 ± 0.69 | 7.25 ± 0.70 | 5.04 ± 2.44 | b35.476 | <0.001 | ||||
Likelihood Ratio.
Kruskal-Wallis Test (Bonferroni correction p<0.001).
3.3. Characteristics of the skin injuries
The rate of skin injuries associated with PPE use in all participants was 47.9% (n = 23). While skin injury developed in all participants in CG (n = 20), the corresponding rate was 10.0% (n = 2) in EG1 and 12.5% (n = 1) in EG2 with significant difference between groups (p < 0.001). 33.3% (n = 16) of participants had multiple skin injuries, all being in CG (Table 2). Types of skin injuries were determined to be Stage 1 PI (29.2%, n = 14), blanchable erythema of intact skin (27.1%, n = 13), papule and pustule type skin lesions (12.5%, n = 6), Stage 2 PI without exposed dermis (8.3%, n = 4), Stage 2 PI with exposed dermis (6.3%, n = 3) and rash (6.3%, n = 3). 18.8% (n = 9) of the participants reported itching on the skin (Table 3 ).
Table 3.
Distribution of types of skin injuries associated with PPE use.
| Information on skin injuries | CG |
EG1 |
EG2 |
Overall |
Test |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | Value | p | |
| Types of skin injuries | ||||||||||
| Stage 1 PI | 14 | 70.0 | 0 | 0.0 | 0 | 0.0 | 14 | 29.2 | a33.515 | <0.001 |
| Blanchable erythema of intact skin | 11 | 55.0 | 2 | 10.0 | 0 | 0.0 | 13 | 27.1 | a15.543 | <0.001 |
| Itching | 8 | 40.0 | 0 | 0.0 | 1 | 12.5 | 9 | 18.8 | a13.379 | 0.001 |
| Skin lesions (papule, pustule etc.) | 6 | 30.0 | 0 | 0.0 | 0 | 0.0 | 6 | 12.5 | a11.735 | 0.003 |
| Stage 2 PI (without exposed dermis) | 4 | 20.0 | 0 | 0.0 | 0 | 0.0 | 4 | 8.3 | a7.520 | 0.023 |
| Stage 2 PI (with exposed dermis) | 3 | 15.0 | 0 | 0.0 | 0 | 0.0 | 3 | 6.3 | a5.536 | 0.063 |
| Rash | 3 | 15.0 | 0 | 0.0 | 0 | 0.0 | 3 | 6.3 | a5.536 | 0.063 |
| Anatomical regions of skin injuries | ||||||||||
| Nasal bridge | 19 | 95.0 | 2 | 10.0 | 0 | 0.0 | 21 | 43.8 | a44.846 | <0.001 |
| Right cheek | 17 | 85.0 | 0 | 0.0 | 0 | 0.0 | 17 | 35.4 | a45.490 | <0.001 |
| Left cheek | 17 | 85.0 | 0 | 0.0 | 0 | 0.0 | 17 | 35.4 | a45.490 | <0.001 |
| Forehead | 5 | 25.0 | 0 | 0.0 | 0 | 0.0 | 5 | 10.4 | a9.584 | 0.008 |
| Chin | 3 | 15.0 | 0 | 0.0 | 0 | 0.0 | 3 | 6.3 | a5.536 | 0.063 |
| Posterior part of the head | 0 | 0.0 | 0 | 0.0 | 1 | 12.5 | 1 | 2.1 | a3.693 | 0.158 |
Likelihood Ratio.
Stage 1 PI 70.0% (n = 14, p < 0.001), blanchable erythema of intact skin 55.0% (n = 11, p < 0.001), papule and pustule type skin lesions 30.0% (n = 6, p = 0.003), Stage 2 PI without exposed dermis 20.0% (n = 4, p = 0.023) were observed only in participants of CG, with significant difference between groups. Stage 2 PI with exposed dermis and rash occurred at the rate of 15.0% (n = 3, p = 0.063) solely CG participants (Table 3).
Anatomical regions of skin injuries were nasal bridge (43.8%, n = 21), right cheek (35.4%, n = 17), left cheek (35.4%, n = 17), forehead (10.4%, n = 5), chin (6.3%, n = 3) and posterior part of the head (2.1%, n = 1) respectively (Table 3).
4. Discussion
DRPIs are common problem that develop as a result of the use of medical and non-medical devices, which have contact with skin and mucosa. However, during COVID-19 pandemic period, with high risk of contamination, DRPIs occurred commonly in HCWs responsible for the diagnosis, treatment and care of these patients, which made it further important to prevent them. DRPIs, which are mostly reported on head and face region depending on the type of devices [9,18], are encountered most commonly on the face region due to the use of PPE [15,16].
In the present study, the rate of skin injuries associated with PPE use was reported to be 47.9% (n = 23) among HCWs (n = 48). Skin injuries developed in all participants in CG (n = 20), while they developed in two participants in EG1 and one participant in EG2. Mean number of skin injuries was approximately 2.5 times higher in CG group than that in other groups. The types of skin injuries were Stage 1 PI, blanchable erythema of intact skin, itching, papule or pustule type skin lesions, Stage 2 PI without exposed dermis, Stage 2 PI with exposed dermis and rash respectively.
Although the methodology of studies in the literature are not uniform, our findings are consistent with other studies in terms of rates and types of skin injuries. In the descriptive study of Foo et al. [8] in 2003 during SARS epidemic, in an acute care hospital in Singapur (n = 322), rash on the face was reported in 35.8% (n = 39) of HCWs using N95 mask [8]. In the survey study of Hu et al. [14] in a state hospital in China (n = 61), it was reported that 27.9% (n = 17) of HCWs using N95 mask experienced itching on the face [14]. Atzori et al. (2020) [1] in a dermatology clinic in Italy reported an increased number of cases of contact dermatitis and skin injuries associated with PPE use [1]. In the multi-center study of Jiang et al. [15] in China (n = 4.306), it was stated that of PPE associated skin injuries, maximum 30.0% (n = 1.293) was PIs being followed by moisture-associated skin damage (10.8%, n = 465) and skin tears (2.0%, n = 86). In the same study, the distribution of PIs was Stage 1 PI (81.1%, n = 1.049), Stage 2 PI (18.3%, n = 236) and Deep Tissue PI (0.6%, n = 8) respectively. Also, it was established that 27.4% (n = 386) of participants had two or more types of skin injuries and 76.8% (n = 1.080) of participants had skin injuries in two or more anatomical regions [15]. In the report of Lam et al. (2020) [19] in Malaysia, PI cases on nasal bridge (n = 5) associated with N95 mask use have been reported [19].
Considering development mechanisms of DRPIs [7,9,10], findings of skin injuries are not surprising. PPEs such as surgical mask, N95 mask, FFP2 mask, FFP3 mask, goggle, face shield, which are used to provide contact and droplet isolation in entrance ports such as mouth, nose and eye [33], exert pressure, friction and shear forces on the face, posterior part of the ear and head where they have contact. Moreover, the fact that these regions have especially sensitive skin where acne and dermatitis problems are common further increases the risk of skin injuries [10,35]. In addition, moisture, which remains under mask and can not be removed and accumulates on the skin causing it to soften, may be an important factor reducing tissue tolerance. Besides these, although HCWs have symptoms such as pain, pressure, and itching under and around PPE, they are forced to maintain contact of skin with these devices for mostly over 2 h until the end of shift owing to the concern about contamination. In the present study, mean duration of constant PPE use was near 4 h, which is almost two times as high as the period stated in international guidelines for relieving the tissue from this load [7,9,10].
Despite its limitations, the results of the present study indicated that using prophylactic dressing contributed to decrease the skin injuries on the face region associated with PPE use, significantly. Due to prophylactic dressing cut to shape and applied to nasal bridge, forehead, chin and cheeks, and ear saver strap, which decrease injuries associated with friction and pressure caused by mask ties, the number of participants with skin injuries in EG1 (n = 2) and EG2 (n = 1) were very few compared to CG (n = 20). This result was obtained with the effect of prophylactic dressings absorbing the moisture, and protecting the fragile skin from friction and pressure exerted by PPE. In studies on the issue, it was stated that prophylactic dressings may help to prevent DRPIs thanks to these characteristics [7,10,35]. In addition, in the present study, unlike other reports in the literature [15,16], no skin injury associated with mask ties was observed in the posterior ear region due to friction. We believe that, this results from the effect of ear saver strap preventing tightness and friction produced by mask ties.
One of the most important result of the present study was that using Breathe Right® nasal strips (GlaxoSmithKline, London/UK) helped to decrease discomfort in breathing during mask use, which is one of the problems associated with PPE use that making a contribution to the solution of this problem. We found this result clinically relevant. In the present study, fogging in goggle, fogging in face shield, perspiration and moisture on the face are problems experienced by almost all participants irrespective of their group. Similar problems were observed in other studies as well [16,31]. However, discomfort in breathing was experienced in all participants except one in groups CG and EG1, while in EG2, which used Breathe Right®, none of the participants experienced this problem (n = 8). The sample size was small, and physiological mechanism of this effect was not investigated, but it can be stated that Breathe Right® nasal strips, which were produced for keeping nostrils open and are stuck on nasal dorsum may have exerted this effect by keeping nostrils open, producing nasal dilatation in people who have nasal obstruction and decreasing nasal congestion associated with flu and allergies.
Mean satisfaction scores associated with PPE was found to be highest in EG2 (x̄ = 7.25 ± 0.70), and mean satisfaction scores of EG2 and EG1 (x̄ = 6.80 ± 0.69) were found to be three times higher than those in CG (x̄ = 2.40 ± 1.23). This result may be attributed to the effect of prophylactic dressing and nasal strip decreasing skin injuries and contributing to more comfortable breathing in experimental groups.
5. Conclusions
The results of this observational study, which was aimed to determine the effect of prophylactic dressing, nasal strip and ear saver strap on the prevention of PPE associated skin injuries on the facial skin and on comfortable breathing with masks in HCWs (CG, n = 20; EG1, n = 20 and EG2, n = 8) working with COVID-19 patients demonstrated that PPE associated skin injuries developed almost in half of HCWs (47.9%). In addition, the rate of skin injures was found to be ten times lower in experimental groups in which prophylactic dressing was used than in CG. In EG2 in which Breathe Right® nasal strips were used in addition to prophylactic dressing, none of the participants experienced any discomfort in breathing with mask.
Skin injuries detected in associated with PPE use Stage 1 PI, blanchable erythema of intact skin, itching, papule or pustule type skin lesions, Stage 2 PI without exposed dermis, Stage 2 PI with exposed dermis and rash respectively. The anatomical regions, where skin injuries associated with PPE developed were nasal bridge, right cheek, left cheek, forehead, chin and posterior part of the head respectively. Mean satisfaction score of PPE was three times higher in experimental groups in which prophylactic dressing and nasal strip were used than that in CG.
In view of these results, it was recommended that prophylactic dressing should be utilized in HCWs using PPE in order to prevent skin injuries on the face region, and that PPE kits, which are ergonomical and ready to use and do not cause breathing problems, should be produced in order that health, safety and work comfort of HCWs can be taken into account as much as patients safety. In addition, it is thought that randomized controlled studies, which will be carried out on this issue with larger patient samples, will contribute to the development of institutional evidence-based policies and practice standards involving skin protection strategies. It is also recommended that industry, health care professionals, professional organizations, and regulatory agencies work in collaboration to manufacture skin-friendly and more ergonomic PPE.
Study limitations
It is thought that low number of participants in the study groups may limit the generalizibility of results to the general population.
Statements of
“ What is already known about the topic?”
-
•
Experiences and informations on skin problems associated with medical and non-medical devices in the literature are usually concerned with the patients.
-
•
Skin problems experienced by HCWs associated with PPE use increase during pandemic periods.
-
•
Following COVID-19 pandemic, intensive and long term PPE use by HCWs for infection control have led the skin injuries to be experienced.
-
•
It is important to prevent skin injuries and PIs associated with PPE use for the safety of HCWs.
“What this paper adds?”
-
•
Skin injuries on the face region develop at high rates in HCWs who use PPE.
-
•
Prophylactic dressing placed under PPE after being cut to shape, prevents development of pressure, friction and moisture-associated skin injuries and PIs on the skin contacting equipment used.
-
•
Using Breathe Right® nasal strips under mask may contribute to the prevention of breathing problems in HCWs.
-
•
More ergonomical and skin-friendly PPE with higher protective effect are required in order to increase satisfaction and safety of HCWs.
Funding
No grant or financial support was obtained from a private or official institution or non-profit organization for the study. Mepilex® Lite and Mepilex® Lite Border with Safetac® technnology wound dressings were donated by Mölnlycke Health Care.
Contributions
Aybala Yıldız contributed to study design, data collection, data analysis and writing of manuscript. Ayişe Karadağ contributed to study design, data analysis and writing of manuscript. Alp Yıldız contributed to study design and data collection. Vildan Çakar contributed to data entrance, data analysis and writing of manuscript. All authors approved the content of the prepared manuscript.
Declaration of competing interest
Authors have no conflict of interest to declare.
Acknowledgements
The authors sincerely thank all partcipants in the study and administrators of the institution allowing this study to be carried out.
References
- 1.Atzori L., Ferreli C., Atzori M.G., Rongioletti F. COVID-19 and impact of personal protective equipment use: from occupational to generalized skin care need [published online ahead of print, 2020 May 16] Dermatol Ther. 2020 doi: 10.1111/dth.13598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayello E.A., Sibbal R.G. Pressure ınjuries: nursing-sensitive indicator or team- and systems-sensitive indicator? Adv Skin Wound Care. 2019;32(5):199–200. doi: 10.1097/01.ASW.0000557754.10070.88. [DOI] [PubMed] [Google Scholar]
- 3.Beitz J.M. Wound healing. In: Carmel J.E., Colwell J.C., Goldberg M.T., editors. Wound, ostomy and continence nurses society core curriculum: wound management. first ed. Lippincott Williams & Wilkins; 2016. pp. 24–37. [Google Scholar]
- 4.Black J., Kalowes P. Medical device-related pressure ulcers. Chron Wound Care Manag Res. 2015;(3):91–99. [Google Scholar]
- 5.Dwivedi A.K., Mallawaarachchi I., Alvarado L.A. Analysis of small sample size studies using nonparametric bootstrap test with pooled resampling method. Stat Med. 2017;36:2187–2205. doi: 10.1002/sim.7263. [DOI] [PubMed] [Google Scholar]
- 6.Edsberg L.E., Black J.M., Goldberg M., McNichol L., Moore L., Sieggreen M. Revised National Pressure Ulcer Advisory Panel pressure injury staging system: revised pressure injury staging system. J Wound, Ostomy Cont Nurs. 2016;43(6):585–597. doi: 10.1097/WON.0000000000000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haesler Emily., editor. European pressure ulcer advisory Panel, national pressure injury advisory Panel and Pan pacific pressure injury alliance. Prevention and treatment of pressure ulcers/injuries: clinical practice guideline. EPUAP/NPIAP/PPPIA; 2019. [Google Scholar]
- 8.Foo C.C.I., Goon A.T.J., Leow Y.H., Goh C.L. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome: a descriptive study in Singapore. Contact Dermatitis. 2006;55(5):291–294. doi: 10.1111/j.1600-0536.2006.00953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gefen A., Alves P., Ciprandi G. Device related pressure ulcers: SECURE prevention. J Wound Care. 2020;29(Sup2a):1–52. doi: 10.12968/jowc.2020.29.Sup2a.S1. [DOI] [PubMed] [Google Scholar]
- 10.Gefen A., Ousey K. Update to device-related pressure ulcers: SECURE prevention. COVID-19, face masks and skin damage. J Wound Care. 2020;29(5):245–259. doi: 10.12968/jowc.2020.29.5.245. [DOI] [PubMed] [Google Scholar]
- 11.Gefen A. Skin Tears, medical face masks, and coronavirus. Wound Manag. Prevent. 2020 Apr;66(4):6–7. [Google Scholar]
- 12.Gefen A., Ousey K. Prevention of skin damage caused by the protective equipment used to mitigate COVID-19. J Wound Care. 2020 Jun 12;29(6):311. doi: 10.12968/jowc.2020.29.6.311. [DOI] [PubMed] [Google Scholar]
- 13.Gefen A., Ousey K. Prevention of skin damage caused by the protective equipment used to mitigate COVID-19: monthly update. J Wound Care. 2020 Jul 12;29(7):379. doi: 10.12968/jowc.2020.29.7.379. [DOI] [PubMed] [Google Scholar]
- 14.Hu K., Fan J., Li X. The adverse skin reactions of health care workers using personal protective equipment for COVID-19. Medicine. 2020;99:24. doi: 10.1097/MD.0000000000020603. e20603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jiang Q., Song S., Zhou J. The prevalence, characteristics, and prevention status of skin injury caused by personal protective equipment among medical staff in fighting COVID-19: a multicenter, cross-sectional study. Adv Wound Care. 2020 doi: 10.1089/wound.2020.1212. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jiang Q., Liu Y., Wei W. The prevalence, characteristics, and related factors of pressure injury in medical staff wearing personal protective equipment against COVID-19 in China: a multicentre cross sectional survey. Int Wound J. 2020:1–10. doi: 10.1111/iwj.13391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karadağ A., Hanönü S., Eyikara E. A prospective, descriptive study to determine nursing interventions in the prevention of medical device-related pressure injuries. Ostomy/Wound Manag. 2017 Oct;63(10):34–41. [PubMed] [Google Scholar]
- 18.Kayser S.A., VanGilder C.A., Ayello E.A., Lachenbruch C. Prevalence and analysis of medical device-related pressure injuries: results from the International Pressure Ulcer Prevalence Survey. Adv Skin Wound Care. 2018;31:276–285. doi: 10.1097/01.ASW.0000532475.11971.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lam U.N., Md Mydin Siddik N.S.F. N95 respirator associated pressure ulcer amongst COVID-19 health care workers [published online ahead of print, 2020 May 12] Int Wound J. 2020 doi: 10.1111/iwj.13398. 10.1111/iwj.13398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.LeBlanc K., Heerschap C., Butt B., Bresnai-Harris J., Wiesenfeld L. NSWOCC; 2020. Prevention and management of personal protective equipment skin injury: update.www.nswoc.ca/ppe Available from: [Google Scholar]
- 21.McHugh M.L. The Chi-square test of independence. Biochem Med. 2013;23(2):143–149. doi: 10.11613/BM.2013.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Medical device related pressure injury guide-Mepilex® Lite. https://www.molnlycke.com/SysSiteAssets/master-and-local-markets/documents/master/wound-care-documents/mepilex-dressings/mepilex-lite-cutting-guide-pdf.pdf Last accessed: July 15, 2020.
- 23.Mitchell A. Adult pressure area care: preventing pressure ulcers. Br J Nurs. 2018;27(18):1050–1052. doi: 10.12968/bjon.2018.27.18.1050. [DOI] [PubMed] [Google Scholar]
- 24.Morgan C.J. Use of proper statistical techniques for research studies with small samples. Am J Physiol Lung Cell Mol Physiol. 2017;313:L873–L877. doi: 10.1152/ajplung.00238.2017. [DOI] [PubMed] [Google Scholar]
- 25.Mufti A., Ayello E.A., Sibbal R.G. Anatomy and physiology of the skin. In: Carmel J.E., Colwell J.C., Goldberg M.T., editors. Wound, ostomy and continence nurses society core curriculum: wound management. first ed. Lippincott Williams & Wilkins; 2016. pp. 3–23. [Google Scholar]
- 26.Haesler Emily., editor. National pressure ulcer advisory Panel, European pressure ulcer advisory Panel, and Pan pacific pressure injury alliance. Prevention and treatment of pressure ulcers: clinical practice guideline. Cambridge Media; Osborne Park, Western Australia: 2014. [Google Scholar]
- 27.National Pressure Ulcer Advisory Panel NPIAP protecting facial skin under PPE N95 face masks info-graphic. https://cdn.ymaws.com/npiap.com/resource/resmgr/position_statements/NPIAP_-_Mask_Injury_Infograp.pdf Last accessed: July 15, 2020.
- 28.Padula C.A., Paradis H., Goodwin R., Lynch J., Hegerich-Bartula D. Prevention of medical device-related pressure injuries associated with respiratory equipment use in a critical care unit. A quality improvement project. J Wound, Ostomy Cont Nurs. 2017;44(2):138–141. doi: 10.1097/WON.0000000000000311. [DOI] [PubMed] [Google Scholar]
- 29.Peko Cohen L., Ovadia-Blechman Z., Hoffer O., Gefen A. Dressings cut to shape alleviate facial tissue loads while using an oxygen mask. Int Wound J. 2019 Jun;16(3):813–826. doi: 10.1111/iwj.13101. Epub 2019 Mar 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Samuriwo R., Dowding D. Nurses' pressure ulcer related judgements and decisions in clinical practice: a systematic review. Int J Nurs Stud. 2014;51(12):1667–1685. doi: 10.1016/j.ijnurstu.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 31.Smart H., Opinion F.B., Darwich I. Preventing facial pressure injury for health care providers adhering to COVID-19 personal protective equipment requirements. Adv Skin Wound Care. 2020;33:1–9. doi: 10.1097/01.ASW.0000669920.94084.c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tabah A., Ramanan M., Laupland K.B. Personal protective equipment and intensive care unit healthcareworker safety in the COVID-19 era (PPE-SAFE): an international survey. J Crit Care. 2020;59:70–75. doi: 10.1016/j.jcrc.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19). Interim guidance. 2020. https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf March 19. Last accessed: July 15, 2020.
- 34.Wound Management Association of Turkey and Wound Ostomy Continence Nurses Society of Turkey Recommendations for preventing medical device-related pressure injuries. 2020. http://yarabakimidernegi.org.tr/rehber.pdf April 14. Last accessed: August 18, 2020.
- 35.Yan Y., Chen H., Chen L. Consensus of Chinese experts on protection of skin and mucous membrane barrier for healthcare workers fighting against coronavirus disease 2019. Dermatol Ther. 2020 doi: 10.1111/dth.13310. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]