Abstract
Background:
Long-acting injectable (LAI) antiretroviral therapy (ART) may offer persons living with HIV (PLWH) an attractive alternative to pill-based treatment options, yet acceptability data remain scant, especially in sub-Saharan Africa.
Methods:
We conducted 6 focus group discussions with PLWH, including key stake holder groups, and analyzed data with content analysis.
Results:
Initial reactions to the idea of LAI-ART were often positive. The primary advantages voiced were potential to facilitate improved adherence and alleviate the burden of daily pill-taking while avoiding inadvertent disclosure and HIV stigma. Potential side effects were a particular concern of the women. Most participants preferred clinic-based administration over self-injections at home due to concerns about safety, privacy, and potential need for refrigeration.
Conclusions:
LAI-ART may be acceptable in Kenya, provided injections are infrequent and delivered in a clinic setting. However, HIV stigma, fear of potential side effects, and limited clinical capacity would need to be addressed.
Keywords: long-acting injectable ART, acceptability, HIV/AIDS, qualitative, Kenya, Africa
What Do We Already Know About This Topic?
Long-acting injectable antiretroviral therapy (LAI-ART) appears to be acceptable to some persons living with HIV who have participated in clinical trials in the West.
How Does Your Research Contribute to the Field?
This research provides data on the acceptability of LAI-ART among persons living with HIV in sub-Saharan Africa (Kenya).
What Are Your Research’s Implications Toward Theory, Practice, or Policy?
Efforts to disseminate LAI-ART should prioritize dosing that is infrequent and how clinic-based injections could be administered.
Introduction
Since 2010, the global scale-up of antiretroviral therapy (ART) has contributed to a 50% decline in global annual deaths from AIDS-related illness, from a peak of 1.9 million in 2005 to 940,000 in 2017, highlighting the importance of ART in reducing morbidity and mortality.1 However, UNAIDS has estimated that only 77% of diagnosed persons living with HIV are accessing ART, and only 82% of patients on ART have suppressed viral loads,2 suggesting there is room for improvement in adherence.
In Kenya, one of the countries bearing a disproportionate burden of the HIV pandemic, over 1.4 million adults and children are living with HIV infection, of whom 95.7% are taking ART and 88.4% have achieved viral suppression as of 2018 estimates—a considerable success.3 Unfortunately, treatment disparities have been reported in Kenya among adolescents and young adults, heterosexual men, and key populations such as sex workers, men who have sex with men (MSM), and injection drug users.2,3 Innovative service delivery models have shown that these groups can be reached for treatment,4 but new approaches to optimize ART adherence and retention might be explored.
One novel ART delivery approach involves long-acting antiretroviral agents. While ART using patches or implants is not currently available,, a number of promising long-acting injectable antiretroviral therapy (LAI-ART) products are becoming available or under investigation and could result in effective treatment regimens.5-7 The extent to which LAI-ART products can address non-adherence and poor retention in care will ultimately depend in large part on their acceptability and uptake, yet scant research has addressed this important area, especially outside the United States (U.S.) and Europe.5,8,9
In the first published study of the acceptability of LAI-ART in the U.S., Williams and colleagues surveyed 400 adults on ART at 2 sites, reporting that 73% of participants overall would definitely or probably try LAI-ART: 61% with weekly dosing, 72% every 2 weeks, and 84% monthly.10 However, many were concerned about possible side effects (48%) and needle use (35%), and older individuals were less willing to try injectable treatment.
In our own qualitative research in the U.S., we conducted focus group discussions (FGDs) and in-depth interviews (IDIs) with persons living with HIV infection (PLWH).11 The key attributes of hypothetical LAI-ART regimens linked to acceptability were efficacy (i.e., being at least as effective as pill-based regimens) and having minimal side effects. Fear of needles and dislike of injections dampened enthusiasm for LAI-ART, but these concerns were mitigated if preferences could be met for bodily site of injection, needle size, number of injections and injection volume, and home administration. Certain subgroups seemed more receptive to LAI-ART, including young people and those experiencing adherence challenges.11
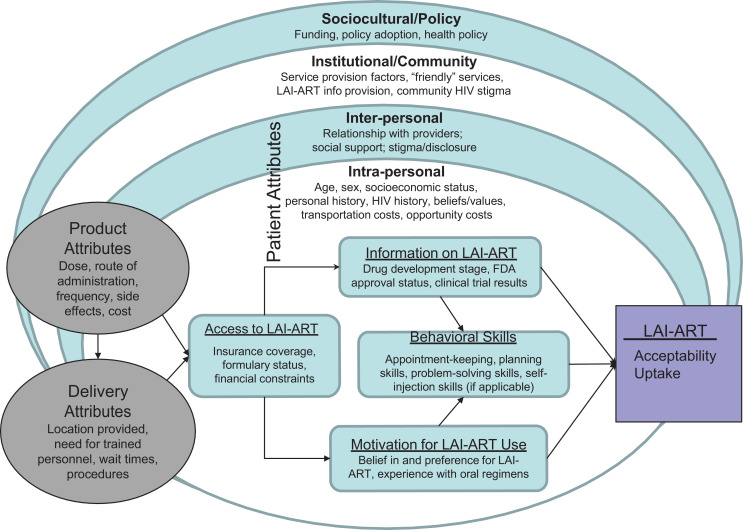
The current study evolves from our program of work on acceptability of LAI-ART,12,13 guided by a multi-level ecological framework that considers factors related to LAI-ART use at intra- and inter-personal, healthcare system, and broader structural and policy levels. As depicted in the Figure 1, product and delivery attributes and access as well as the individual factors of information, motivation, and behavioral (IMB) skills as postulated in the IMB framework14 will likely be key influencers of acceptability and, ultimately, LAI-ART use.
Figure 1.
Ecological model of LAI-ART acceptablity and uptake.
Product formulators need to recognize the inter-connected factors that will affect LAI-ART uptake, adherence, and longer-term persistence — each of which is critical to long-term viral suppression — and devise products that avoid or ameliorate undesirable effects, matching patient preferences to the extent possible. Indeed, identification of modifiable factors will enable the implementation of LAI-ART in a way that maximizes uptake. data that could be used to predict acceptability in different settings would be an invaluable resource for product developers and ultimately contribute to more successful dissemination and uptake of new products.
Sub-Saharan Africa, with the largest burden of HIV in the world, may pose unique barriers and facilitators to product dissemination and uptake but we lack data from African PLWH. In this setting, injections are often used for treatment of infections (e.g., malaria, TB) and for hormonal contraception (e.g., injectable depot-medroxyprogesterone acetate, the most common choice of contraception among women in Kenya). Familiarity with injectable medications may lead to greater acceptability of LAI-ART than in high-income countries. At the same time, HIV stigma and limited access to providers may render the prospect of additional visits for LAI-ART dosing less appealing. To better understand how product and delivery attributes, access, and individual factors may influence patient preferences related to LAI-ART in a resource-limited setting in sub-Saharan Africa, we conducted FGDs with PLWH in Kenya.
Methods
Data Collection
In June 2017, we conducted 6 FGDs with 49 PLWH from key stake holder groups in Kenya: 8 male “youth” (i.e., those under 25 years of age), 8 female youth 7 “adult” men (i.e., those 25 years of age or older), 7 adult women, 11 men who have sex with men (MSM), and 8 female sex workers Participants were recruited from the Coast General Hospital Youth Center, the Ganjoni Comprehensive Care Clinic, the KEMRI Mtwapa HIV Clinic, and the Mombasa Cohort of female sex workers. All sites offer HIV treatment and care according to the Kenyan National Guidelines.
Study and clinic staff assisted with FGD recruitment by contacting patients based on clinic records and inviting them to participate. Participants were eligible if they were a member of one of the key PLWH stakeholder groups, attended clinic at one of the selected study sites, were at least 18 years of age, and were fluent in English or Kiswahili. A FGD for each stake holder group was conducted in a private conference room at our research site, located within Ganjoni Clinic, and facilitated by a Kenyan male social scientist (coauthor GW) with extensive experience conducting qualitative research with PLWH. A female research assistant took detailed notes. FGDs lasted an average of 90 minutes and were digitally audio-recorded. All participants completed a brief demographic questionnaire and received reimbursement (∼USD $5) for transportation.
FGD facilitators followed a semi-structured discussion guide, developed based on literature reviews and interviews with experts in HIV care provision and related research. Discussion guides were designed to elicit participant challenges with ART adherence and views on the potential use of hypothetical LAI-ART regimens. The facilitator began each FGD by asking participants to share their experiences initiating and engaging with current pill-based regimens. Next, participants were asked to provide their initial reactions to the idea of a “new HIV regimen or treatment that does not have to be taken daily and will be given by injection.” Participants were encouraged to share questions and concerns they might have about switching to a LAI-ART regimen, including their thoughts and preferences around dosing frequency, type of injection, and site of administration. Probes explored how strongly side effect profiles, any pain or site reactions associated with an injection, and efficacy relative to pill-based regimens would influence their decisions about switching to LAI-ART. Participants were also asked to identify other attributes influencing LAI-ART acceptability, including factors related to self-administration at home or attendance for clinic-administered injections. No specific details around regimens currently in development were provided during the discussions, and implants, patches, and infusions were not discussed.
Ethical Approval and Informed Consent
Institutional review boards at the University of Washington (51912, 45961, 665), the Kenya Medical Research Institute (2711) and Kenyatta National Hospital/University of Nairobi (P235/5/2013) approved protocols for this study. All participants provided written informed consent prior to enrollment in the study. Participants provided written informed consent.
Data Analysis
FGD recordings were translated and transcribed in a single step. Data were analyzed using a combination of conventional and directed content analysis approaches to identify key attributes of LAI-ART acceptability and feasibility.15 Directed content analysis was used to explore attributes previously shown to be associated with LAI-ART acceptability by our research team,11,12 while conventional content analysis was used to identify novel influences within these specific populations. To support coding, analysis, and data management, we used Dedoose v.7.5.10 software. A codebook was created deductively based on the domains probed in the discussion guide and inductively based on open-ended responses. Co-authors JS, ZM, or KBS independently coded transcripts using an agreed-upon final version of the codebook. Independently coded transcripts were reviewed by a second member of the research team to increase reliability and code application consistency. Any disagreements in code were resolved through group discussion. Following coding and coding review, emergent themes and key influential attributes were identified and compared within and between the population subgroups of PLWH. Demographic characteristics were compared between adult and youth participants using Fisher’s exact tests for categorical variables and Wilcoxon rank-sum tests for continuous variables.
Results
Participants
The Table 1 describes characteristics of the 49 FGD participants according to rsults of the baseline. Overall,, adult (n = 33) and youth (n = 16) participants ranged in age from 19 to 64 years; about half were female and most had some secondary education. About half were unemployed. Most had been diagnosed with HIV and initiated ART at least 6 years ago. About half were on twice-daily ART/co-trimoxazole (Septrin) regimens, and 73% were virally suppressed. Only 2 had experience with self-injections or giving others injections. Surprisingly, about half “somewhat” or “strongly” agreed they hate injections and try to avoid them. There were statistically significant differences between youth and adults participating in the FGDs. Specifically, compared to adults, youth were more educated, lived closer to their clinic, were more likely to report pill-taking twice daily, and were less likely to have an undetectable viral load (see Table 1 for details).
Table 1.
Description of Kenyan Focus Group Discussion Participants (All Living With HIV).
| Characteristics | Youth (n = 16) |
Adults (n = 33) |
All (N = 49) |
p value |
|---|---|---|---|---|
| Female | 8 (50) | 16 (48) | 24 (49) | 1.000 |
| Age in years | 22 (19-24) | 36 (25-64) | 31 (19-64) | <0.001 |
| Highest level of education | 0.003 | |||
| Primary (1-8 years) or less | 1 (7) | 17 (52) | 18 (38) | |
| Secondary (9-12) or more | 14 (93) | 16 (48) | 30 (63) | |
| Employment | 0.286 | |||
| Not working | 11 (69) | 14 (42) | 25 (51) | |
| Working part-time | 4 (25) | 14 (42) | 18 (37) | |
| Working full-time | 1 (6) | 5 (15) | 6 (12) | |
| Monthly income, KES | 0.705 | |||
| 0-9,999 | 4 (67) | 21 (72) | 25 (71) | |
| 10,000-19,999 | 2 (33) | 7 (24) | 9 (26) | |
| 20,000 or more | 0 (0) | 1 (3) | 1 (3) | |
| Lifetime sexual partners | 0.403 | |||
| Mostly or only opposite sex | 8 (89) | 23 (70) | 31 (74) | |
| Mostly or only same sex | 1 (11) | 10 (30) | 11 (26) | |
| Living situation | 0.061 | |||
| Own/family’s house/apartment | 13 (81) | 21 (64) | 34 (69) | |
| Someone else’s house/apartment | 1 (6) | 11 (33) | 12 (24) | |
| No stable living situation | 2 (13) | 1 (3) | 3 (6) | |
| Years since HIV diagnosis | 0.886 | |||
| In the last year | 0 (0) | 2 (6) | 2 (4) | |
| 2-5 years ago | 3 (19) | 4 (12) | 7 (14) | |
| 6-10 years ago | 7 (44) | 16 (48) | 23 (47) | |
| >10 years ago | 6 (38) | 11 (33) | 17 (35) | |
| When initiated HIV medications | 0.071 | |||
| ≤1 year | 0 (0) | 4 (12) | 4 (8) | |
| 2-5 years | 6 (38) | 7 (21) | 13 (27) | |
| 6-10 years | 4 (25) | 17 (52) | 21 (43) | |
| >10 years | 6 (38) | 5 (15) | 11 (22) | |
| # daily pills for HIV-related medications | 0.139 | |||
| 1 | 3 (20) | 9 (27) | 12 (25) | |
| 2 | 2 (13) | 12 (36) | 14 (29) | |
| 3+ | 10 (67) | 12 (36) | 22 (46) | |
| Doses per day of HIV-related medications | 0.011 | |||
| 1 | 2 (13) | 16 (48) | 18 (37) | |
| 2 | 13 (81) | 17 (52) | 30 (61) | |
| 3+ | 1 (6) | 0 (0) | 1 (2) | |
| Primary mode of transport to clinic | 0.861 | |||
| Walk/ride or bicycle | 2 (13) | 7 (21) | 9 (18) | |
| Bus or other public transportation | 13 (81) | 24 (73) | 37 (76) | |
| Taxi/own car | 1 (6) | 2 (6) | 3 (6) | |
| Time to get to clinic | 0.045 | |||
| <30 minutes | 5 (31) | 2 (6) | 7 (14) | |
| 30 minutes to 1 hour | 8 (50) | 18 (55) | 26 (53) | |
| >1 hour | 3 (19) | 13 (39) | 16 (33) | |
| Prescribed any other (non-HIV) medications | 1 (6) | 11 (33) | 12 (24) | 0.073 |
| # days missed 1+ dose of HIV medication (last 30 days) | 0.766 | |||
| None | 10 (67) | 23 (71) | 33 (70) | |
| 1 | 1 (7) | 2 (6) | 3 (6) | |
| 2 | 0 (0) | 2 (6) | 2 (4) | |
| 3+ | 4 (27) | 5 (16) | 9 (19) | |
| HIV medication taken as prescribed (last 30 days) | 1.000 | |||
| Never/Rarely/Sometimes | 4 (25) | 7 (21) | 11 (22) | |
| Usually/Almost always/Always | 12 (75) | 26 (79) | 38 (78) | |
| How well took HIV medications in the way supposed to? (last 30 days) | 0.141 | |||
| Very poor/Poor/Fair | 6 (38) | 5 (15) | 11 (22) | |
| Good/Very good/Excellent | 10 (63) | 28 (85) | 38 (78) | |
| Result of last HIV viral load test | 0.016 | |||
| Undetectable | 3 (38) | 19 (86) | 22 (73) | |
| Detectable | 5 (63) | 3 (14) | 8 (27) | |
| Currently self-inject | 0 (0) | 1 (3) | 1 (2) | 1.000 |
| Any experience with self-injections | ||||
| Never | 15 (100) | 33 (100) | 48 (100) | – |
| Any experience with giving injections to others | ||||
| Never | 16 (100) | 33 (100) | 49 (100) | – |
| Hate getting injections and try to avoid whenever possible | 0.391 | |||
| Strongly/Somewhat agree | 6 (13) | 17 (52) | 23 (47) | |
| Neither agree or disagree | 2 (13) | 1 (3) | 3 (6) | |
| Strongly/Somewhat disagree | 8 (50) | 15 (45) | 23 (47) |
Predominant Themes
Initial participant responses were generally favorable toward LAI-ART but dependent primarily on infrequent dosing and lack of side effects. Some participants expressed dislike or fear of injections, often tied to prior negative experience with injectable medications, which also tempered their enthusiasm for LAI-ART. Side effects such as weight gain attributed to other injectable medications (e.g., contraceptives) were a particular concern for women participants, who linked them to the method of delivery and were thus voiced as a concern for LAI-ART as well. The primary advantages attributed to LAI-ART were its potential to facilitate adherence and alleviate the burden of daily pill-taking. HIV stigma was a pervasive theme, with LAI-ART seen as a way to more easily avoid the inadvertent disclosure that can occur with daily pill-taking. Finally, most participants, if given a choice, would opt for clinic-based administration rather than self-injection at home.
LAI-ART Acceptability Was Dependent on Dosing Frequency, Potential Side Effects and Prior Experience With Injectable Medications
Overall, many participants’ initial reactions to the concept of an injectable formulation of ART were quite favorable, with one participant commenting that an injectable could be “The absolute solution!” Others wanted to know more about the dosing frequency before disclosing any preference. Optimal dosing was considered to be yearly or every 6 months, but many felt that injections required even every 1-3 months would still be preferable to daily pill-taking.
Ah, if it would be a daily injection, I personally would not manage. But if you get injected from January to January I would have preferred…eh, even 6 months. (Adult-M)
I think the syringe should be like the family planning one where you are injected only once in 3 months. (FSW)
I think the injection…should be taken maybe once per month or every other month. The injection is easier that way. (Youth-F)
Although longer dosing intervals were generally favored, a few participants were concerned about how infrequent dosing might inadvertently decrease engagement in care.
I would try the injection but you see everything has an advantage and a disadvantage…the frequency is the problem…when I come here and take the injection and let’s say 3 months or more then I will come to forget that because it is a long time ago. After a month, there is nothing to remind you and I personally may forget. (Adult-M)
Next to dosing intervals, side effects were the most common concern of participants in weighing whether they would consider LAI-ART. Side effects of ART were the source of frequent complaints related to participants’ pill-based regimens, and participants were clear that they would not tolerate an injectable option with worse side effects than those they were already experiencing with pill-based regimens.
If it has no side effects I can even start tomorrow. (Adult-M)
Dislike or fear of injections, as well as past experiences with injectable medications, tempered acceptability. Some participants were clear from the start that no matter the dosing frequency or side effect profile, they were categorically opposed to getting injections.
I am satisfied with the pills and I have no problem swallowing them. I don’t like injections. (FSW)
For some of these participants, negative attitudes toward injections were linked to past experience or knowledge of others taking injectable medications. There was animated discussion of this topic among the FSW, especially regarding changes in fat distribution or physical appearance that were attributed to injections they had received in the past, most likely for contraception.
When we started taking these pills, there are some of us who got fat here and on the nose. You are a slim woman and it adds weight here and her legs swell, so these syringes should not be like those that White people gave us in the past that made our legs dry up and the stomachs had fat and a woman gets big breasts. (FSW)
You see the swelling just comes once the medicine is injected into my body, so when I get to the house my arm has just swollen. So, I would rather just use pills my entire life. (FSW)
Participants who had favorable experiences with injectable versions of other medications were, not surprisingly, more open to LAI-ART.
I am also not afraid of injections and I have the same experience as her because of TB. I was given injections for 30 days and I do not fear them as their process ends fast. It’s only one second or 2 minutes and then it is over. (Youth-F)
Diabetes people inject themselves on the stomach and thighs and I have not seen any side effect so if it won’t bring any side effects, then I think it is okay. (Youth-F)
One female youth talked about another advantage of injections being their (presumed) superior efficacy.
The injection should be more effective. Like when you have malaria, you are given the option of the tabs or the injection and the injections are always more effective. (Youth-F)
LAI-ART Can Improve Adherence by Reducing Daily Pill Burden and Alleviating Stigma
Many participants who were favorably disposed toward injectable ART discussed their challenges adhering consistently to pill-based regimens. Among the 8 FSW, who all responded favorably to injectable ART, 7 admitted to problems taking their pills regularly. The male youth also noted struggling with adherence, which led them to be more favorably inclined toward an injectable version of ART.
It will be nice for the people who forget, as it will be taken maybe once a month and it would have reduced the burden of us forgetting. (Youth-M)
Some participants directly linked their preference for injectable ART to the heavy load of having to take their pill-based regimen. As one FSW said, “They should lighten this burden of ours if they can, and inject us.” Participants noted many challenges to adherence to pill-based regimens, including perceived large size of pills (and their being difficult to swallow), the challenge of arranging their schedules around dosing times, the need to carry pills when traveling, fear of disclosure to others if seen taking pills, challenges traveling to clinics to pick up prescriptions, and continuous stress caused by fear of forgetting pill doses or missing pill times. These concerns were especially prevalent among youth, although voiced in all the FGDs.
I think the injection would be better because the burden of carrying the pills is too much. Maybe you have a sleepover or you have been invited to a party--carrying them while travelling is stressful. (Youth-F)
I would like the injection because I am sure I can travel without the pain of having to take the pills and the constant checking of the time to see if it is time to take the drug. (Adult-F)
Interestingly, one female youth struggling with adherence noted that another advantage of the injections was their ability to track and confirm actual dose-taking.
It will also reduce the lying that we have taken the medication when maybe we haven’t. Because the injection is known and we know what is working…we will not be giving false information when we say that ARTs are not working and maybe we are just not taking the medication ourselves well. (Youth-F)
A pervasive theme of the discussions was stigma, especially its influence on adherence. Many participants thought the major advantage to injectable regimens was in helping them elude the extreme social stigma around HIV, a stigma that led them to conceal their medication-taking in the small, tight-knit communities in which they lived with little privacy.
That is always a secret you have kept. Like for me the only person who knows my secret is my child and even my husband doesn’t know. So maybe you do not know if your neighbor is in that environment and you just take the pill and then they will know…so the injection will help us hide. (Adult-F)
Stigma was especially acute among the youth, who feared inadvertent disclosure of their HIV status to peers. For students in particular, lack of privacy was cited as complicating pill-taking.
So I am currently taking my diploma, and it is a challenge because sometimes I say that I will get out of class early and take them, but I get home late. When I carry them, my classmates keep asking me why I take pills every day. I tell them to mind their own business. (Youth-F)
In addition to the extra adherence challenges noted by youth, participants in the MSM FGD alluded to the double burden of stigma based on HIV and their sexual orientation.
I would say the challenge of the drugs per se, was that I was staying at home. So putting in mind that I have not disclosed to my parents, where it’s not necessary due to the stigma associated with my sexuality, again now introducing HIV it would be like double stigma. So I did not find a way to disclose at home. I had to take initiative and take the drugs but hide them at a friend’s who understands me and also takes the drugs. (MSM)
Clinic Administration of Injections Was Preferred Over Self-Injections at Home
Participants voiced varied opinions regarding where they would prefer to receive ART injections. M most participants, both men and women, favored a provider-administered shot at a clinic over one self-injected at home. Some cited the greater knowledge and competence of clinic-based providers, which would make the commute worthwhile to them.
The chemist can write this for you, do this, do that…But it is important a person goes to be injected in the hospital or by an expert…because anything can happen. When you are alone, what shall you do? Before you think of going to the facility, you are dead. (MSM)
Some thought an injection would entail finding a vein, like with illegal drugs that are injected intravenously, making a trained clinician even more preferable.
I view it like, it’s better for me to come so that the doctor injects me because he is the one that knows where the veins are. (Adult-M)
I would like [the hospital]…because the doctor has training and knows where specifically…I should be injected. I can inject in a wrong place and the medicine reacts in the body. It goes and spoils. It leads to the cancer disease or another disease. I would prefer a doctor. (MSM)
One youth who favored administration at the hospital offered the added advantage that the providers there could help him maintain adherence. Other participants noted that going to a clinic was advantageous because it was more discrete than home administration, which might lead to disclosure of one’s HIV status to others.
I think there will be a problem. We will still have to carry those drugs and take them home, where visitors come and there are kids, so it is better in the health center where they inject us. (Adult-F)
One MSM pointed out legal risk as an additional barrier to home administration, as illicit drug use is criminalized in Kenya and it has been illegal to possess needles and syringes without a prescription until the recent introduction of needle and syringe exchange programs. Another major advantage of clinic-based administration was that it obviated the potential need for refrigeration of the injectable medication.
The medicine should be made to last because not everybody can access refrigeration. Mostly for people in rural areas and us in school it will be a challenge. (Youth-F)
To say the truth if it has to do with placing things in the fridge to an African as poor as me…I see it will be a problem. Let’s say I have a fridge and it spoils and needs repair, Before it is fixed, it will be two months and how about the medicine? (Adult-M)
In the participants’ communities, sometimes a more fortunate neighbor might have refrigeration and might allow storage. Yet, one could not always count on a neighbor’s discretion. Clinic-based administration was also associated with safe and hygienic storage and disposal of needles and syringes. reducing the risk of household members accidentally harming themselves with discarded needles.
Injection is something very risky. Because when I have injected myself and my phone rings, “There is someone who wants to see you outside quickly.” And I have already poked myself and forgotten there are children there. You are a parent, you understand me? You know how children are, big or small. They say, “Daddy does this, let me…” So in my own way, I want a doctor. (Adult-M)
Preference for administration at a clinic persisted even when participants were reminded about the possible burden in terms of time and expense to travel to the clinic. After one such discussion among MSM, which yielded estimates of ½ hour to 2 hours for travel time and 100-400 shillings (US$ 1.50-4.00) in expenses to visit a clinic, the men still preferred clinic administration. Only one MSM, demurring slightly, suggested having a separate clinic for gay men might be a good idea to improve acceptability of clinic-based injections.
Although clinic-based administration was preferred by many in the youth and MSM populations, not every participant would opt for this. The adult men’s group discussed the advantages of home-based injections, and they were inspired by the example of others being able to learn to self-inject.
I have someone with…I do not know if it was diabetes. He was injecting himself, and I asked him about it. He said he doesn’t feel any pain. (Adult-M)
Because you could come here and find there are a lot of people and I had things to do elsewhere. So you waste your time here. And it (the injection) is something you could do yourself. (Adult-M)
In addition, one of the female youth participants thought she could be trained to competently self-inject if needed.
As for difficulty in injection ourselves, actually, as for me I think with constant training and being brought to awareness I think we can, because a 5-year-old diabetes kid can inject herself if trained. Then I think what we have is fear but once we get used to it, it can’t be hard. (Youth-F)
Discussion
This qualitative study on preferences for LAI-ART in a diverse sample of PLWH in coastal Kenya yielded some of the first such data from an African setting. Many of the initial reactions to the idea of an injectable option for ART were positive, even enthusiastic. However, they were tempered by the desire for infrequent dosing (generally no more than monthly). Some participants voiced strong fears and dislike of injections, sometimes based on prior experience. Many women expressed concern about adverse effects that might result from injections, such as weight gain or other bodily changes they had attributed to injectable medications in the past. The main advantages voiced by participants were improved adherence and decreased burden of daily pill-taking (note that about half the participants were on twice-daily HIV/Septrin regimens). In particular, participants described the stigma they experienced related to HIV treatment and were optimistic that LAI-ART, preferably administered in a clinic setting rather than at home, would allow them to live with HIV more discretely. Lack of access to refrigeration for storage and means of hygienic disposal of syringes were raised as barriers to home-based injections.
There are few studies in the literature in which to contextualize our findings, and most of these are from the U.S. or Europe. Compared to our prior U.S.-based findings, Kenyans were less open to home-based injections, more open to injections in general, and more focused on the need for fewer side effects. FGD results were consistent with our expectations that injections would be generally viewed more favorably in Kenya than in the U.S., and with research from the 2012 Kenya AIDS Indicator Survey.16 Of the 13,673 survey participants who answered questions about medical injections, 36% reported receiving one or more injection in the past 12 months and 51% preferred receiving an injection over a pill. Surprisingly, survey responses indicated 47% of participants strongly or somewhat agreed that they “hate getting injections and try to avoid whenever possible.” It is possible the burden of daily dosing was so heavy that some were inclined toward an injectiable ART option even given dislike of needles.
Participants in our Kenyan FGDs generally preferred clinic-based administrations for LAI-ART. They trusted providers to give injections safely and felt that clinic administration would be preferable since it would obviate the need for home storage and disposal of used syringes. Some participants also expressed hope that the clinic might remind them of appointments and find them if they missed injections.
The Kenyan participants in our study had never tried LAI-ART; actual experience with an injectable option of ART may change their views. Reports from PLWH with actual experience using long-acting products are available from the LATTE-2 trial, in which individuals were randomly assigned (2:2:1) to receive 2 injections of long-acting cabotegravir and rilpivirine at 4-week or 8-week intervals or a comparable daily pill-based regimen.17 Across all arms, 97% of 254 participants reported very high treatment satisfaction (5 or 6 on a 6-point scale). While 99% in the injectable treatment arm participants would be highly satisfied to continue their LAI-ART, only 78% in the oral treatment arm would be highly satisfied to continue their oral regimen (no p value given).17 Similarly favorable results were reported from a qualitative study associated with the LATTE-2 trial, in which 39 in-depth interviews were conducted with participants and providers from the U.S. and Spain.18 Despite commonly experienced adverse events (primarily injection site reactions), participants were generally tolerant of the regimen, finding injections convenient, with reduced potential for HIV disclosure and elimination of the “daily reminder of living with HIV.” These findings may allay fears expressed by Kenyans in our study about potential side effects and confirm their hopes that LAI-ART may reduce inadvertent disclosure of daily pill taking.
While provider views were not included in our preliminary work in Kenya, monthly clinic-based injections could be prohibitively expensive in Kenya, where patient volume is large and a differentiated care approach is being scaled up in order to reduce costs and burdens on the health system.19 Improved treatment adherence and overall health might compensate for these costs. Clearly, health system constraints and the cost-effectiveness of LAI-ART relative to the current model of HIV care will be important to incorporate in future work.
Further research might also consider quantitative methods for evaluating acceptability (e.g., conjoint analyses, discrete choice experiments), and incorporate the specific attributes of actual LAI-ART products as they become available. Future research also will need to place LAI-ART in the context of other novel drug administration strategies such as antiretroviral implants.20 Acceptability research should capitalize on opportunities in trials of LAI-ART regimens, using qualitative and quantitative methods as did the LATTE-2 investigators. Such work could provide opportunities to compare anticipated versus actual preferences or vary attributes of the regimens to monitor the impact on preferences and uptake. This work should incorporate findings from the more developed literature on acceptability of and barriers to adherence to long-acting injectable PrEP21,22 and other injectable medications, such as hormonal contraceptives23,24 and treatment for schizophrenia.25
While these preliminary data provided important insights into potential LAI-ART product acceptability and potential facilitators and challenges, this work has some limitations. Our sample was constrained to a relatively small number of PLWH in the coast of Kenya. We did not interview PLWH in other areas of the country or in other African countries; nor did we talk to other stakeholders such as public health officials, policy makers, insurance companies, or pharmaceutical manufacturers. Additionally, as noted, we relied on self-reported preferences instead of actual behavioral assessments and reference to attributes of hypothetical products, rather than specific regimens in development.
In conclusion, our findings revealed the importance of factors at every level of the ecological framework we employed. Product attributes (dosage frequency and potential side effects) and delivery attributes (location for administration) interacted with individual factors (prior experience with injectable medications, experienced stigma) to influence acceptability and likely uptake of LAI-ART. In turn, these factors were affected by broad structural and social barriers and considerations, such as trust in providers, comfort with disclosing HIV status, societal stigma, discrimination in educational settings, and even constraints such as prohibitions against carrying syringes. A “situated,” contextual understanding of PLWH is needed to fully appreciate the likely range of responses to LAI-ART options. Without such an ecological perspective, predictions regarding uptake and planned adjustments in implementation may well miss the mark.
Acknowledgments
We gratefully acknowledge the participation of patients as well as the assistance with recruitment from the clinic staff.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by NIH grants AI120176, AI027757, and MH121424.
ORCID iD: Jane M. Simoni  https://orcid.org/0000-0002-8711-1576
https://orcid.org/0000-0002-8711-1576
Susan M. Graham  https://orcid.org/0000-0001-7847-8686
https://orcid.org/0000-0001-7847-8686
References
- 1. UNAIDS. UNAIDS Data 2018. 2018:1–376. [Google Scholar]
- 2. Joint United Nations Programme on HIV/AIDS, UNAIDS 2017. Ending aids progress towards the 90-90-90 Targets. Glob Aids Updat. 2017:1–198. doi:UNAIDS/JC2900E [Google Scholar]
- 3. National AIDS and STI Control Programme (NASCOP), Preliminary KENPHIA 2018 Report. NASCOP; 2020. [Google Scholar]
- 4. Petersen M, Balzer L, Kwarsiima D, et al. Association of implementation of a universal testing and treatment intervention with HIV diagnosis, receipt of antiretroviral therapy, and viral suppression in east Africa. J Am Med Assoc. 2017;317(21):2196–2206. doi:10.1001/jama.2017.5705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Owen A, Rannard S. Strengths, weaknesses, opportunities and challenges for long acting injectable therapies: insights for applications in HIV therapy. Adv Drug Deliv Rev. 2016;103:144–156. doi:10.1016/j.addr.2016.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kleiner LW, Wright JC, Wang Y. Evolution of implantable and insertable drug delivery systems. J Control Release. 2014;181(1):1–10. doi:10.1016/j.jconrel.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 7. Dabis F, Newell ML, Hirschel B. HIV drugs for treatment, and for prevention. Lancet. 2010;375(9731):2056–2057. doi:10.1016/S0140-6736(10)60838-0 [DOI] [PubMed] [Google Scholar]
- 8. Havlir D, Gandhi M. Implementation challenges for long-acting antivirals as treatment. Curr Opin HIV AIDS. 2015;10(4):282–289. doi:10.1097/COH.0000000000000158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rusconi S, Marcotullio S, Cingolani A. Long-acting agents for HIV infection: biological aspects, role in treatment and prevention, and patient’s perspective. New Microbiol. 2017;40(2):75–79. [PubMed] [Google Scholar]
- 10. Williams J, Sayles HR, Meza JL, et al. Long-acting parenteral nanoformulated antiretroviral therapy: interest and attitudes of HIV-infected patients. Nanomedicine. 2013;8(11):1807–1813. doi:10.2217/nnm.12.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Simoni JM, Beima-Sofie K, Mohamed ZH, et al. Long-acting injectable antiretroviral treatment acceptability and preferences: a qualitative study among US providers, adults living with HIV, and parents of youth living with HIV. AIDS Patient Care STDS. 2019;33(3):104–111. doi:10.1089/apc.2018.0198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Simoni JM, Tapia K, Lee SJ, et al. A conjoint analysis of the acceptability of targeted long-acting injectable antiretroviral therapy among persons living with HIV in the U.S. AIDS Behav. 2019;24(4):1226–1236. doi:10.1007/s10461-019-02701-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dubé K, Simoni J, Louella M, et al. Acceptability of cell and gene therapy for curing HIV infection among people living with HIV in the Northwestern United States: a qualitative study. AIDS Res Hum Retroviruses. 2019;35(7):649–659. doi:10.1089/aid.2019.0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rivet Amico K. A situated-information motivation behavioral skills model of care initiation and maintenance (sIMB-CIM): an IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. J Health Psychol. 2011;16(7):1071–1081. doi:10.1177/1359105311398727 [DOI] [PubMed] [Google Scholar]
- 15. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi:10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 16. Kimani D, Kamau R, Ssempijja V, et al. Medical injection use among adults and adolescents aged 15 to 64 years in Kenya: results from a national survey. J Acquir Immune Defic Syndr. 2014;66(Suppl 1):S57–S65. doi:10.1097/QAI.0000000000000106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Margolis DA, Gonzalez-Garcia J, Stellbrink HJ, et al. Long-acting intramuscular Cabotegravir and Rilpivirine in adults with HIV-1 infection (LATTE-2): 96-week results of a randomised, open-label, phase 2b, non-inferiority trial. Lancet. 2017;390(10101):1499–1510. doi:10.1016/S0140-6736(17)31917-7 [DOI] [PubMed] [Google Scholar]
- 18. Kerrigan D, Mantsios A, Gorgolas M, et al. Experiences with long acting injectable ART: a qualitative study among PLHIV participating in a Phase II study of Cabotegravir + Rilpivirine (LATTE-2) in the United States and Spain. PLoS One. 2018;13(1):1–11. doi:10.1371/journal.pone.0190487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hagey JM, Li X, Barr-Walker J, et al. Differentiated HIV care in sub-Saharan Africa: a scoping review to inform antiretroviral therapy provision for stable HIV-infected individuals in Kenya. AIDS Care. 2018;30(12):1477–1487. doi:10.1080/09540121.2018.1500995 [DOI] [PubMed] [Google Scholar]
- 20. Flexner C. Antiretroviral implants for treatment and prevention of HIV infection. Curr Opin HIV AIDS. 2018;13(4):374–380. doi:10.1097/COH.0000000000000470 [DOI] [PubMed] [Google Scholar]
- 21. Parsons JT, Rendina HJ, Whitfield THF, Grov C. Familiarity with and Preferences for Oral and Long-Acting Injectable HIV Pre-exposure Prophylaxis (PrEP) in a National Sample of Gay and Bisexual Men in the U.S. AIDS Behav. 2016;20(7):1390–1399. doi:10.1007/s10461-016-1370-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Greene GJ, Swann G, Fought AJ, et al. Preferences for Long-Acting Pre-exposure Prophylaxis (PrEP), Daily Oral PrEP, or Condoms for HIV Prevention Among U.S. Men Who Have Sex with Men. AIDS Behav. 2017;21(5):1336–1349. doi:10.1007/s10461-016-1565-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Burke HM, Chen M, Buluzi M, et al. Effect of self-administration versus provider-administered injection of subcutaneous depot medroxyprogesterone acetate on continuation rates in Malawi: a randomised controlled trial. Lancet Glob Heal. 2018;6(5):e568–e578. doi:10.1016/S2214-109X(18)30061-5 [DOI] [PubMed] [Google Scholar]
- 24. Myers JE, Ellman TM, Westhoff C. Injectable agents for pre-exposure prophylaxis: lessons learned from contraception to inform HIV prevention. Curr Opin HIV AIDS. 2015;10(4):271–277. doi:10.1097/COH.0000000000000166 [DOI] [PubMed] [Google Scholar]
- 25. Kane JM, Schooler NR, Marcy P, et al. Patients with early-phase schizophrenia will accept treatment with sustained-release medication (long-acting injectable antipsychotics): results from the recruitment phase of the PRELAPSE trial. J Clin Psychiatry. 2019;80(3):18m12546. doi:10.4088/JCP.18m12546 [DOI] [PubMed] [Google Scholar]