Abstract
Hepatocellular carcinoma (HCC), the most common primary hepatic tumor, metastasizes in more than 50% of cases. However, metastasis of HCC to the submandibular glands is very rare. HCC rarely metastasizes to the salivary glands; only six cases of metastasis to the parotid gland have been reported in the English-language literature. Moreover, only one case of metastasis of HCC to the submandibular glands has been reported to date, and the affected patient died of hepatic failure. This clinical report describes a 55-year-old man who had undergone two surgeries for liver cancer and subsequently presented with a 2-week history of a right submandibular mass. We performed dissection of the right submandibular triangle, and metastatic HCC of the submandibular gland was diagnosed. Although HCC metastases to the oral cavity have been reported, this is only the second case of HCC metastasis to the submandibular gland. Fine-needle aspiration biopsy is recognized as a simple, direct approach for morphologic diagnosis of salivary gland lesions; however, histological and immunohistochemical examination of the surgical specimen remains necessary.
Keywords: Hepatocellular carcinoma, submandibular gland, metastasis, hepatic failure, histopathology, case report
Introduction
Hepatocellular carcinoma (HCC), the most common primary hepatic tumor, metastasizes in more than 50% of cases. Metastases are commonly found in the lungs, peritoneum, adrenal glands, and bone, although a few reports have described metastases in the heart, ovaries, nasal cavity, skin, and pharynx. HCC rarely metastasizes to the salivary glands. Moreover, only one case of HCC metastasis to the submandibular glands has been reported to date, and the affected patient died of hepatic failure. Metastasis to the salivary glands, which is always a late manifestation of HCC, can be easily misdiagnosed as benign mass. We herein describe a patient in whom investigation of a right submandibular mass revealed metastatic HCC.
Case report
In 2011, a 55-year-old man was admitted to the hospital because of a 2-week history of a right submandibular mass without persistent pain. The patient had undergone two surgeries for stage 3 liver cancer in 2003 and 2006. Postoperative interventions were performed 12 times for disease relapse. Nine months before the current presentation, computed tomography (CT) had revealed metastases in the right lung and lower left thoracic ribs.
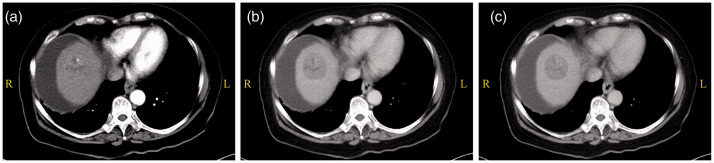
Three-phase contrast-enhanced abdominopelvic CT revealed a mass in the right lobe of the liver. The mass showed enhancement in the arterial phase and a typical wash-out pattern with heterogeneous low attenuation in the portal and delayed phases; these findings are relevant to the clinical diagnosis of HCC (Figure 1).
Figure 1.
Hepatocellular carcinoma was seen in the right lobe of the liver on abdominal computed tomography. The mass showed obvious heterogeneous enhancement in the arterial phase and a typical wash-out pattern in the portal and delayed phases. (a) Arterial phase. (b) Portal phase. (c) Delayed phase.
R, right; L, left.
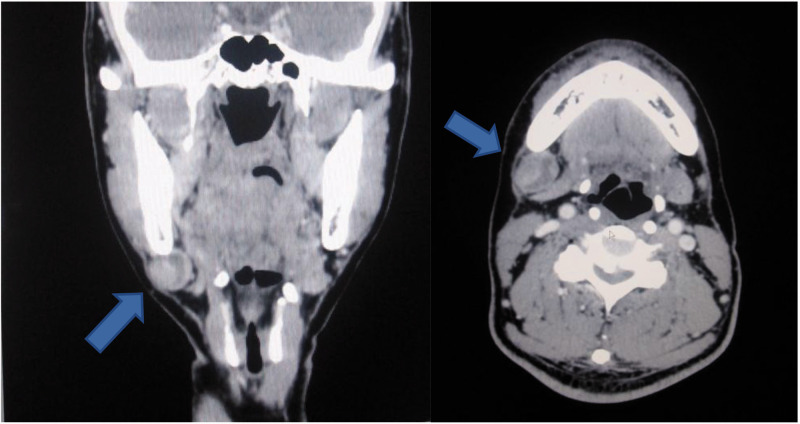
Clinical examination revealed a 2- × 2-cm soft and well-defined mass in the right submandibular region. CT showed a 20-mm round and well-defined enhancing nodular lesion with no remarkable lymph node enlargement. Therefore, a lymphatic tumor of the submandibular gland was considered (Figure 2).
Figure 2.
Computed tomography showed a 20-mm round and well-defined enhancing nodular lesion under the right jaw (arrows) with no other remarkable lymph node enlargement.
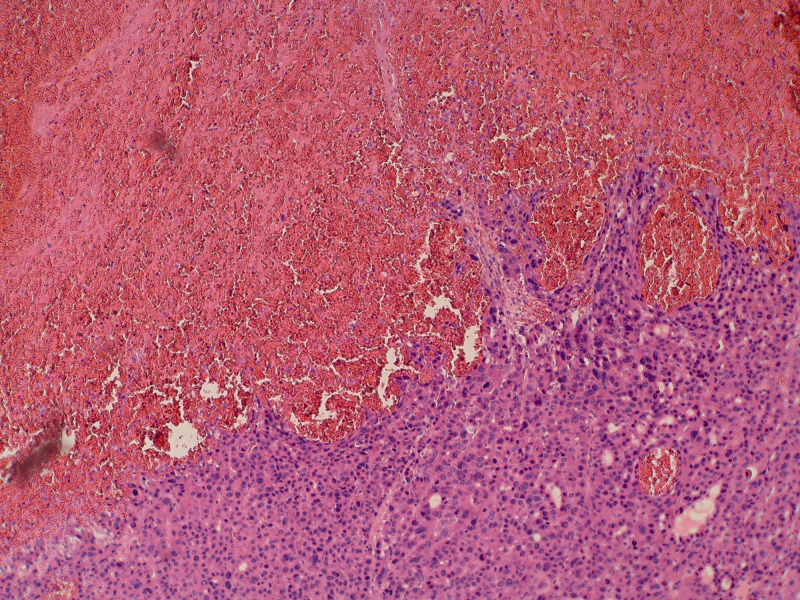
Initial laboratory investigations showed no obvious contraindications for general anesthesia. The operation (dissection of right submandibular triangle + adjacent flap repair) was performed 1 week after admission (Figure 3). No postoperative complications were observed, and the patient was discharged from the hospital in good condition. The histopathological examination revealed invasion of the hepatoma carcinoma cells into the submandibular gland tissue. A photomicrograph of a hematoxylin- and eosin-stained slide (×100) showed severe nuclear anaplasia and pleomorphism (Figure 4). The patient died of liver failure 6 months after the operation.
Figure 3.
Resection of the 20-mm tumor and right submandibular gland.
Figure 4.
Photomicrograph of the oral mass exhibiting nuclear anaplasia and pleomorphism (hematoxylin and eosin, ×100).
Discussion
Extrahepatic metastasis of HCC is a relatively common malignancy. However, metastasis to the oral cavity and jaws is seldom observed. The most commonly invaded sites in such cases include the mandibles and the gingiva. Metastatic involvement of the salivary glands is uncommon, accounting for 10% to 16% of all salivary gland malignancies excluding lymphomas. These metastases usually originate from head and neck malignancies, but metastases from primary cancer outside the head and neck region are also possible. However, only 20% of such metastases originate from infraclavicular sites (usually the lungs, kidneys, or breasts) and even more rarely originate from gastrointestinal or genitourinary primary sites.1 To the best of our knowledge, the present report describes only the second case of HCC metastasizing to the submandibular glands.
The treatment of submandibular gland tumors remains challenging because the exact nature of the lesion is often unknown before or at the time of surgery. The disease is advanced by the time HCC has metastasized to the oral cavity. Fine-needle aspiration (FNA) biopsy is a simple, direct approach for morphologic diagnosis of salivary gland lesions and can maintain the integrity of the tumor. Despite the accuracy, specificity, and sensitivity of FNA biopsy, however, there may be differences between cellular morphology and histopathology.2 FNA of salivary gland lesions presents one of the most challenging diagnoses in cytopathology.3 In general, FNA of some salivary glands, such as the parotid gland, has moderate sensitivity and high specificity in differentiating malignant from benign disease. The advantage of this technique is that it can be performed in the outpatient setting with minimal recovery time and a low risk of complications.4 Although the classification standardization of salivary FNA findings should be improved, FNA has become a commonly performed diagnostic test in the initial evaluation of some salivary masses.
Basically, there are two pathways leading from the liver to the maxillofacial region. Metastases from the liver to the maxillofacial area initially reach the lungs via the hepatic artery and the portal vein,5 and they subsequently reach the maxillofacial area. Vitale et al.2 reported a case involving metastatic HCC in the parotid region without lung metastasis. The study suggested that HCC can spread into Batson’s plexus (a connection between the azygos and hemiazygos veins and the vertebral venous plexus), bypassing the filtration through the lungs. In the present case, however, the metastasis had already invaded the patient’s lungs, leading to a poor prognosis. The submandibular gland metastasis in this case might have occurred via the lymphatic route, although the exact route is unclear because metastatic HCC was found in the lymph nodes of the submandibular gland.
Although these findings are rare, HCC is considered the origin of submandibular masses in patients with a history of HCC.
Footnotes
Ethics approval: The requirement for ethics approval was waived because the patient’s data were de-identified.
Consent to participate: Written informed consent was obtained from the patient prior to the study.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by the National Natural Science Foundation of China [grant no. 31400859].
ORCID iD: Danping Ruan https://orcid.org/0000-0002-3113-9692
References
- 1.Romanas MM, Cherian R, McGregor DH, et al. Hepatocellular carcinoma diagnosed by fine-needle aspiration of the parotid gland. Diagn Cytopathol 2004; 30: 401–405. [DOI] [PubMed] [Google Scholar]
- 2.Vitale AR, Compilato D, Coletti G, et al. Metastatic hepatocellular carcinoma of the parotid region without lung metastasis: a case report. Int J Oral Maxillofac Surg 2009; 38: 696–698. [DOI] [PubMed] [Google Scholar]
- 3.Moore FR, Bergman S, Geisinger KR. Metastatic hepatocellular carcinoma mimicking acinic cell carcinoma of the parotid gland: a case report. Acta Cytol 2010; 54: 889–892. [PubMed] [Google Scholar]
- 4.Liu CC, Jethwa AR, Khariwala SS, et al. Sensitivity, specificity, and posttest probability of parotid fine-needle aspiration: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2016; 154: 9–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teshigawara K, Kakizaki S, Sohara N, et al . Solitary mandibular metastasis as an initial manifestation of hepatocellular carcinoma. Acta Med Okayama 2006; 60: 243–247. [DOI] [PubMed] [Google Scholar]