Abstract
Meniscal tears treated with partial meniscectomies have been shown to significantly increase contract pressures within the tibiofemoral joint, and a complete focal meniscal deficiency may render the entirety of the meniscus functionally incompetent. Although various techniques of meniscal transplantation have been described, these techniques may require the excision of a considerable amount of healthy meniscal tissue. Furthermore, failures continue to frequently occur. Therefore, attempts to restoring normal knee kinematics and biomechanical forces are essential. Segmental meniscus allograft transplantations may offer the advantage of a robust repair by both maintaining knee biomechanics and biology while maximizing preservation of native meniscal tissue. Also, most meniscal deficiency involves only a portion of the meniscus, and thus we developed this technique to segmentally transplant only the deficient portion. The purpose of this Technical Note is to describe a technique of segmental medial meniscus allograft transplantation in a patient with focal medial meniscus deficiency.
Technique Video
This video outlines the step-by-step illustration of anterior cruciate ligament reconstruction and segmental medial meniscus transplant in a patient with focal medial meniscus deficiency. We perform this technique by first performing a diagnostic arthroscopy, which reveals the region of full-thickness segmental meniscus deficiency. After debridement, a spinal needle is passed from outside-in to determine the location of the defect and to pass a shuttling suture to eventually shuttle the prepared meniscus transplant into the defect. Next, the meniscus allograft is prepared by marking both the posterior and anterior aspects, and the desired length of transplant is measured. The 20-mm allograft of meniscus is excised from the donor meniscus. Preparation of the graft consists of No. 2 nonabsorbable sutures around the periphery of the graft. A total of 5 sutures are passed around the periphery in a vertical mattress configuration. A midline incision and a medial parapatellar arthrotomy are performed to accomplish both the proximal tibia osteotomy and the 2 osteochondral allograft plugs. The same arthrotomy is used to shuttle the meniscus graft. Once the allograft is positioned intraarticularly, the 5 vertical mattress sutures are passed through the capsule using a needle-shuttling device. The anterior and posterior regions of the graft are then incorporated into native tissue using No. 2 nonabsorbable sutures. The transplant is further anchored anteriorly to the tibia with a single 2.9-mm suture anchor placed at the periphery of the tibia. The final construct was intact to probing and stable.
Intact menisci are important for normal knee kinematics and load-bearing characteristics.1, 2, 3, 4, 5, 6, 7, 8 Meniscal tears and subsequent partial meniscectomy have been shown to significantly increase articular cartilage contact pressures in the tibiofemoral joint, leading to degenerative changes.5,7,9 Numerous studies have documented the poor clinical outcomes that occur subsequent to partial and complete meniscectomy.2,4,9, 10, 11, 12
To prevent knee arthritis after partial or complete meniscal excision, focus has turned to restoring normal knee kinematics and biomechanical forces through meniscal transplantation and/or meniscal scaffold insertion (Table 1).5,9,13, 14, 15, 16, 17, 18, 19, 20 Biomechanical characteristics of knees with meniscal allograft transplantation have been reported to resemble native knee-loading characteristics. However, in some patients, significant amounts of native meniscal tissue with proprioceptive capacity must be excised to perform a complete meniscal transplantation.14, 15, 16, 17, 18, 19, 20 Furthermore, survival rates greater than 10 years for meniscal transplantation have been reported to be only 52%.21 In some instances, meniscal scaffolds have been used for focal meniscal deficiency, but despite favorable short-term results, scaffolds have not yielded long-term regeneration of functional meniscal tissue or prevented osteoarthritis.22,23 Implantation of a segmental meniscal allograft in this setting has the potential to more closely replicate native knee biomechanics and biology while preserving as much native tissue as possible (Table 1).14,24
Table 1.
Advantages and Disadvantages of Segmental Meniscus Allograft Transplantation
| Advantages | Disadvantages |
|---|---|
| Intact portions of the meniscus are not sacrificed | Technique is limited to focal meniscal deficiency; not suitable for patients with global meniscal deficiency |
| Restoration of contact pressure and area within the medial compartment at time zero | Long-term clinical results not yet available |
| Preserved mechanoreceptors within the native meniscus may improve proprioception and joint homeostasis | Risk of failure at the allograft-native meniscal interface |
| The segmental meniscal transplant may be firmly secured with suture anchors at the junction of allograft-native meniscus | There is a possibility that the meniscus may become overtethered when using suture anchors in the lateral compartment |
The purpose of this Technical Note is to present the surgical technique for segmental medial meniscus allograft transplantation in a patient with focal medial meniscus deficiency.
Surgical Technique
Indications
Segmental meniscal transplant may be indicated in symptomatic patients with a focal meniscal defect, as may be seen after a prior meniscectomy. Contraindications include uncorrected alignment, unaddressed ligamentous instability, and bipolar chondral defects within the compartment. A proper physical examination should verify that the patient’s pain corresponds with the findings of imaging and arthroscopy, such that a patient is not unnecessarily subjected to a procedure with a lengthy recovery without benefit.
Patient Evaluation
Prior to proceeding with any form of meniscal transplant, the authors obtain long-leg standing alignment films and magnetic resonance imaging (MRI), and they perform a primary staging arthroscopy and debridement. Alignment, meniscal status, chondral lesions, and ligamentous status are assessed, such that these may be addressed concurrently to prevent additional modes of meniscal failure. Commonly, patients with focal deficiency may have undergone several prior surgeries. A complete surgical history should be obtained. In the setting of prior ligamentous reconstruction, physical exam, MRI, and arthroscopy should verify intact ligaments and a stable knee. Close inspection of the adjacent cartilage should be performed, as coexisting chondral lesions may be commonly encountered. Long-leg standing alignment films may also demonstrate malalignment; this requires correction to avoid overloading the area of transplanted meniscus.
Surgical Technique
Our surgical technique is presented in Video 1. MRI and arthroscopy performed prior to the procedure demonstrated an intact anterior cruciate ligament graft. A segmental medial meniscal defect was identified, as were associated chondral lesions of the medial femoral condyle, and significant varus malalignment. Accordingly, a segmental medial meniscal transplant was planned to be performed concordantly with a valgus-producing opening-wedge high tibial osteotomy (HTO), as well as medial femoral condyle osteochondral allografting (MFC OCA).
Diagnostic Arthroscopy
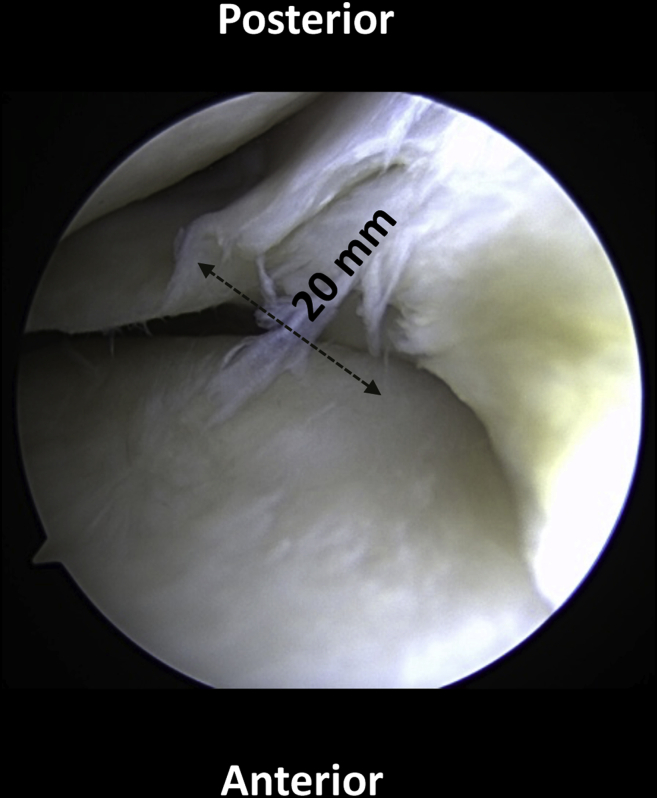
Before the segmental meniscal transplantation, a standard diagnostic arthroscopy is performed. This essential step is performed to ensure that there has been no additional meniscal loss or damage that would compromise the segmental allograft transplant (Table 2). When that the area of meniscal deficiency is found to excurse beyond the middle body of the meniscus, a total meniscal transplant may be indicated. In the case presented, diagnostic arthroscopy was performed via 2 standard subcutaneous anteroinferior portals through a central, midline incision used for both the HTO and MFC OCA. The meniscal defect was measured to be 20 mm, which was believed to be within the acceptable range for a segmental transplant (Fig 1). As a caveat: if an HTO is to be performed, this is completed prior to addressing the meniscus, whereas OCA is completed after the segmental meniscal transplant.
Table 2.
Pearls and Pitfalls of Segmental Meniscus Allograft Transplantation
| Pearls | Pitfalls |
|---|---|
| Use spinal needle to identify anterior and posterior extents of the defect for careful arthrotomy planning | Prevent additional modes of meniscal failure by concurrently addressing malalignment, ligamentous deficiency, or cartilage lesions |
| Prepass sutures through the graft to aid with inside-out repair to capsule | Careful measurement must be performed along the periphery of the defect to prevent undersizing of the graft |
| Use arthroscopic knot pusher to aid in gentle reduction of the graft into position of the defect | Failure to obtain an adequate bite of posterior meniscal remnant may cause suture pullout when shuttling graft into place |
| Use anchor (such as 3.0-mm shoulder labrum anchors) fixation for secure attachment to tibial plateau | |
| Meticulous preparation to native unaffected meniscus with accurate sizing via arthroscopic ruler |
Fig 1.
Diagnostic arthroscopy viewing from the anterolateral portal shows a radial degenerative tear of the meniscus with healthy meniscus anterior and posterior to it. Rather than performing a near-total meniscectomy, a segmental portion can be removed and prepared for a segmental transplantation. The patient is positioned supine on the operating room table.
Arthrotomy and Meniscal Remnant Excision
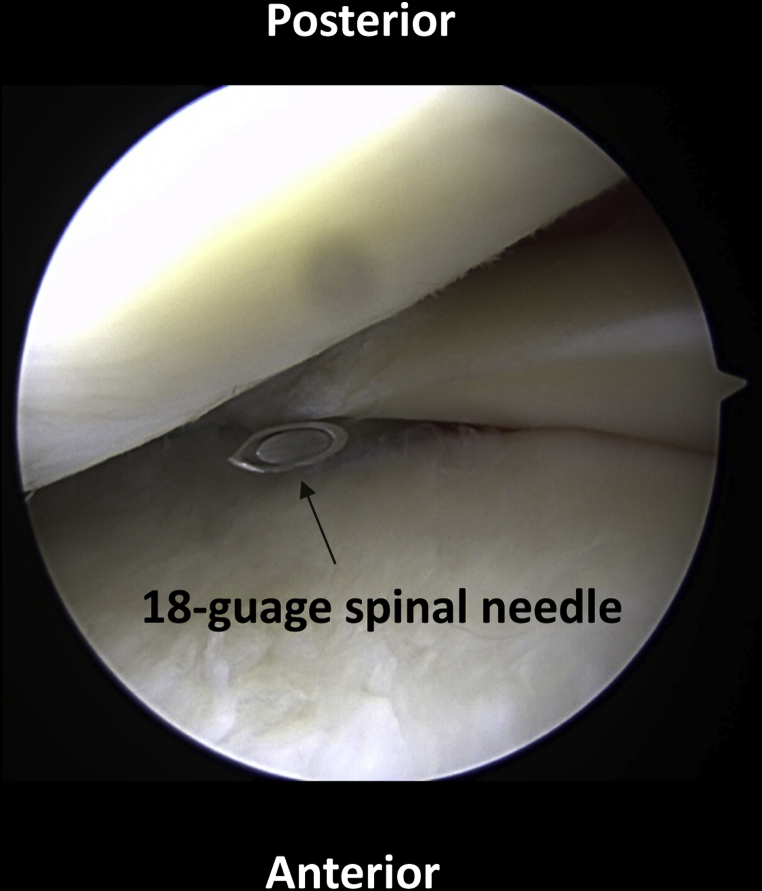
The area of meniscal deficiency is then identified in an outside-in fashion using an 18-gauge spinal needle (Fig 2, Table 2). Two needles are used to approximate both the anterior and posterior extents of the defect. Particular attention must be paid to the posterior extent of the defect, and the arthrotomy must be performed in a location where the posterior remnant will be accessible. An approximately 3-cm arthrotomy is made medially within the knee capsule near the anterior aspect of the defect. The joint capsule is opened to reveal the deficient meniscus of the medial body. A No. 15 blade is used to excise the identified meniscal remnant, with careful dissection to avoid injury to the intact meniscus. The defect is again measured around the peripheral rim of the deficient meniscus, ensuring that the graft will be of proper size when prepared. After careful verification of the deficient area to be transplanted, the allograft is prepared on the back table.
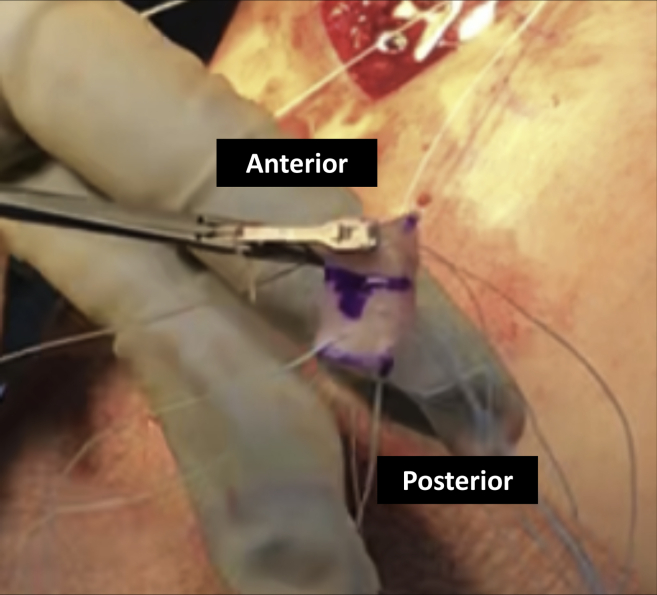
Fig 2.
With the arthroscope in the anterolateral portal, a spinal needle is used for localization of the segmental transplant location. A small medial parapatellar arthrotomy is made.
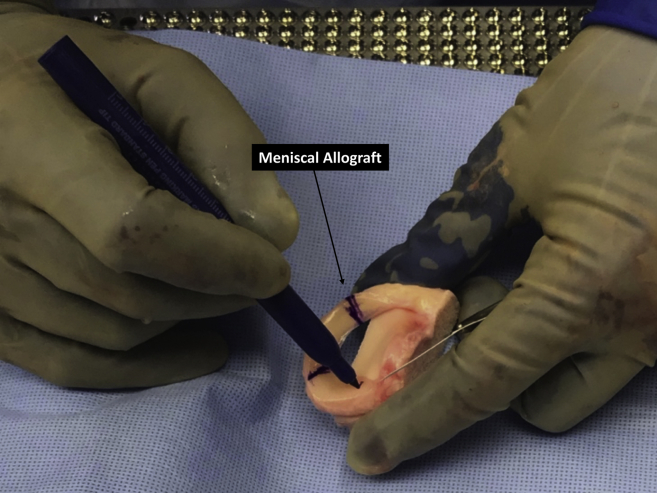
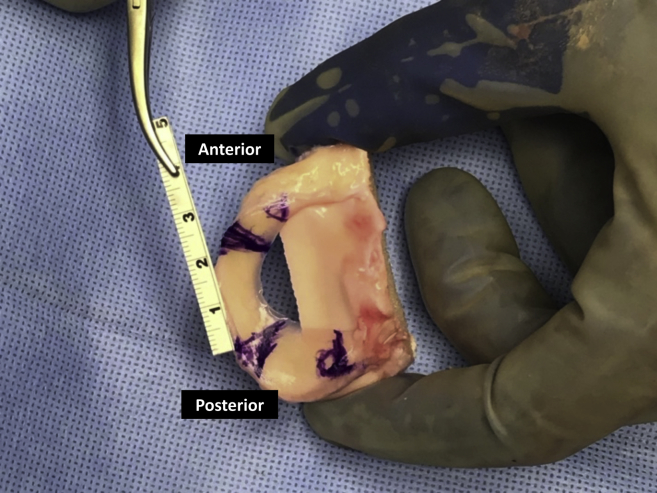
Segmental Allograft Preparation
The meniscal allograft is sized on the back table (Fig 3). In the presented case, this was performed by taking a 2-cm wedge from the body of a cadaver meniscus. This segment is marked with a sterile ruler, so that anterior and posterior and tibial sides are evident (Fig 4). After confirmation of measurements, the segmental allograft is excised from the donor using a No. 15 blade (Fig 5). Subsequently, 5 vertical mattress sutures are placed around the periphery of the meniscal graft in preparation for future passage through the capsule (Fig 6, Table 2). We find a self-passing arthroscopic suture device to be ideal for this task. In addition, 2 sutures are placed in the posterior remnant of the native meniscus; care must be taken to obtain an adequate capture of the intact meniscus, as these sutures will eventually be used to shuttle the graft into place. These sutures are then passed through the corresponding posterior aspect of the graft (Fig 7).
Fig 3.
After preparation of the recipient site is complete and the defect measured, the allograft meniscus is marked to the same size on the back table.
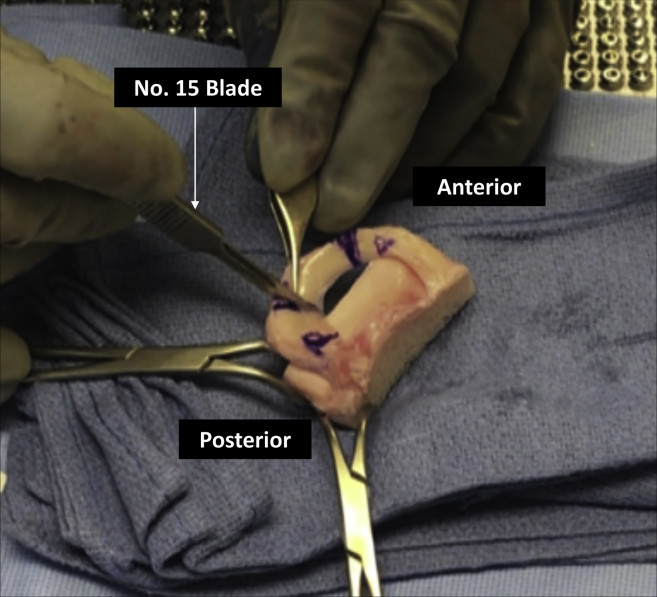
Fig 4.
The allograft meniscus is measured along its periphery, verifying appropriate size for the segmental transplant. This measurement should equal the measured defect size at the periphery of the focal defect.
Fig 5.
The allograft meniscus is cut to the appropriate size for the segmental transplantation. A No. 15 blade is used, while the assistant carefully stabilizes the graft.
Fig 6.
While still on the back table, 5 vertical mattress sutures are then passed through the peripheral portion of the meniscus in preparation for the later outside-in repair over the capsule, as well as through the native meniscus. The authors find the use of an arthroscopic suture passer to be ideal for this task. In addition, 2 sutures were placed in the posterior aspect of the intact meniscus for repair.
Fig 7.
The graft is then moved to the operating table. The sutures that were already passed through the native meniscus are then passed with an arthroscopic suture passer through the posterior portion of the segmental transplant.
Graft Delivery and Fixation
The allograft meniscus is then passed through the medial arthrotomy and parachuted down the sutures previously attached to the posterior meniscus remnant, using an arthroscopic knot pusher and tension slide technique (Fig 8, Table 2). These sutures are tied to securely affix the segmental allograft transplant posteriorly via a horizontal mattress (side-to-side nature meniscus). Following this, a self-passing suture device is used to pass the sutures from the graft periphery through the capsule for an inside-out-type repair. These meniscocapsular sutures approximate the meniscal graft to the capsule and along the course of the periphery of the graft. Finally, the graft is evaluated arthroscopically, and an additional high-strength suture is used to affix the graft to anteriorly. This is again performed with a self-passing suture device in a mattress fashion. Afterward, a knotless anchor is placed to secure the meniscus anteriorly to the tibial plateau (Table 2). Again, the meniscus is evaluated arthroscopically for stability and continuity with the remnants of the anterior and posterior meniscus (Fig 9). An additional repair of the arthrotomy site is the performed with figure-of-8 absorbable sutures.
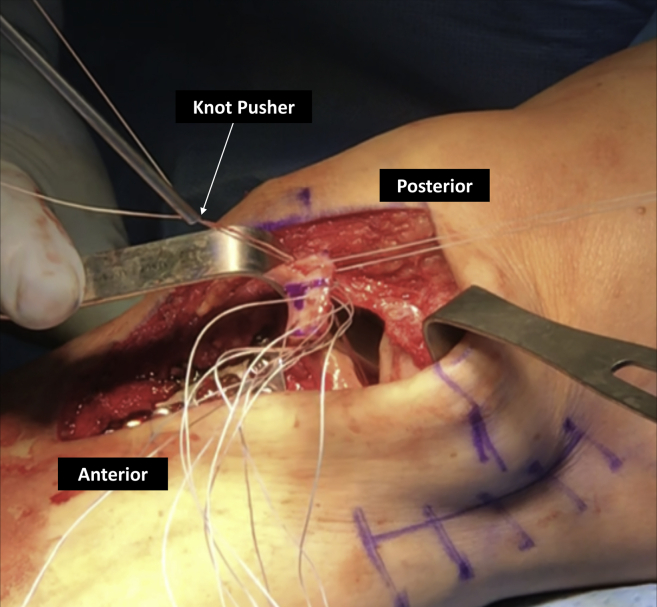
Fig 8.
An arthroscopic knot pusher is used to pass the meniscus through the medial arthrotomy and tensioned down, delivering the meniscus into the defect using a tension slide technique. The knee may be flexed as needed to facilitate delivery. An arthroscopic suture passer is then used to repair the meniscal graft to the capsule along the course of the arcuate ligaments. Additional inverted mattress sutures were then placed at the anterior rim of the meniscus. For further fixation, a 3-mm SutureTak knotless anchor (Arthrex, Naples, FL, U.S.A.) was placed anteriorly.
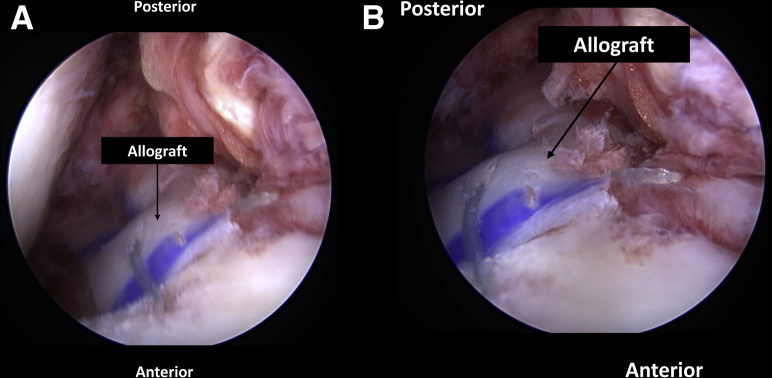
Fig 9.
Final arthroscopic images viewed from the anterolateral portal after (A) suture fixation through the capsule, as done in an outside in meniscal repair. (B) Sutures are also seen tied to the adjacent anterior and posterior native meniscus
Discussion
As our understanding of normal meniscus function has increased, so too have our efforts to preserve the menisci. Several biomechanical studies have demonstrated that partial medial meniscectomy creates altered tibiofemoral compartment pressures and loading characteristics.1,2,4,5,10,16,25,26 Given these findings, several authors have gone to great lengths to study methods of meniscus preservation, including meniscal repair,6,7,9,13,18 meniscal allograft transplantation,5,14, 15, 16, 17, 18,20,24 and meniscal scaffold transplantation.21,22,27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37
Most meniscal treatment algorithms support meniscal repair whenever meniscal tissue is amenable.38 However, focal meniscal loss is not an uncommon result of failed meniscal repair or in tear patterns when repair is not possible. In these cases, meniscal allograft transplantation is a viable option, although current meniscal allograft transplantation techniques can be challenging and include complete excision of the native meniscus. In some cases, this includes excision of healthy native meniscal tissue adjacent to the focal meniscal deficiency.
Several studies have reported that various intra-articular components, including menisci, are sensate, capable of generating neurosensory signals that reach spinal, cerebellar, and higher central nervous system levels.39, 40, 41, 42, 43 It is believed that these neurosensory signals result in conscious perception and are important for normal knee joint function and maintenance of tissue homeostasis (Table 1).44 One concern with performing a total meniscectomy for meniscal allograft transplantation is that it effectively removes all meniscal mechanoreceptors in that compartment, including Ruffini endings, Pacinian corpuscles, and Golgi tendon organs, which aid in proprioception and joint homeostasis.39, 40, 41
Given these findings, attention has been turned to meniscal preservation through segmental meniscal scaffolds. Meniscal scaffolds generally come in 2 varieties, a collagen-based implant28,30, 31, 32, 33, 34, 35,37 and a polyurethane-based scaffold.21,22,27,29,36 The 2 available implants are the Collagen Meniscal Implant (CMI; Ivy Sports Medicine, Gräfelfing, Germany) and Actifit polyurethane scaffold (Actifit; Orteq Ltd, London, UK). Rates of success have been variable with both scaffold implants, with failure rates ranging from 0% to 38% at 4 years.22 Long-term results have been less predictable. It has been reported that meniscal scaffolds may become nonfunctional due to fragmentation, shrinkage, and extrusion, which may result in failure to increase articular cartilage coverage, reduce peak pressure, and achieve a balanced load distribution.22
Nyland et al.24 first evaluated segmental meniscus allograft transplantation in a bovine knee cadaveric model, looking for an alternative to meniscal scaffolds. They found that segmental meniscal allograft transplantation in bovine knees restored native knee contact pressures in the tibiofemoral joint. Unpublished biomechanical data from the senior authors’ institution have demonstrated that segmental medial meniscus allograft transplantation in human knees restores medial compartment mean contact pressure and mean contact area. Although further investigation is needed, these data suggest that segmental medial meniscus transplantation may be a reasonable treatment alternative for patients with focal medial meniscus deficiency.
Limitations of this technique include the lack of long-term follow-up after segmental meniscal transplant. Moreover, this technique may not be suitable for treatment of patients with large areas of meniscal deficiency; these patients may be better served with a traditional meniscal transplant. Otherwise, limitations mirror those seen with complete meniscal transplant. Patients with frank arthritic changes within the compartment of interest or bipolar chondral lesions may not be suitable candidates. Specific risks of segmental meniscal transplant include the possibility that the allograft may not integrate with the native meniscus. When using suture anchors to secure the meniscus to the tibial plateau, there is also a theoretical possibility of overtethering the meniscus, particularly in the lateral compartment.
The purpose of this Technical Note is to present the surgical technique for segmental medial meniscus allograft transplantation in a patient with focal medial meniscus deficiency.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video outlines the step-by-step illustration of anterior cruciate ligament reconstruction and segmental medial meniscus transplant in a patient with focal medial meniscus deficiency. We perform this technique by first performing a diagnostic arthroscopy, which reveals the region of full-thickness segmental meniscus deficiency. After debridement, a spinal needle is passed from outside-in to determine the location of the defect and to pass a shuttling suture to eventually shuttle the prepared meniscus transplant into the defect. Next, the meniscus allograft is prepared by marking both the posterior and anterior aspects, and the desired length of transplant is measured. The 20-mm allograft of meniscus is excised from the donor meniscus. Preparation of the graft consists of No. 2 nonabsorbable sutures around the periphery of the graft. A total of 5 sutures are passed around the periphery in a vertical mattress configuration. A midline incision and a medial parapatellar arthrotomy are performed to accomplish both the proximal tibia osteotomy and the 2 osteochondral allograft plugs. The same arthrotomy is used to shuttle the meniscus graft. Once the allograft is positioned intraarticularly, the 5 vertical mattress sutures are passed through the capsule using a needle-shuttling device. The anterior and posterior regions of the graft are then incorporated into native tissue using No. 2 nonabsorbable sutures. The transplant is further anchored anteriorly to the tibia with a single 2.9-mm suture anchor placed at the periphery of the tibia. The final construct was intact to probing and stable.
References
- 1.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus: Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 2.Cox J.S., Nye C.E., Schaefer W.W., Woodstein I.J. The degenerative effects of partial and total resection of the medial meniscus in dogs' knees. Clin Orthop Relat Res. 1975;109:178–183. doi: 10.1097/00003086-197506000-00026. [DOI] [PubMed] [Google Scholar]
- 3.Ichiba A., Kishimoto I. Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients under 40 years old. Arch Orthop Trauma Surg. 2009;129:409–415. doi: 10.1007/s00402-008-0786-4. [DOI] [PubMed] [Google Scholar]
- 4.Koh J.L., Yi S.J., Ren Y., Zimmerman T.A., Zhang L.Q. Tibiofemoral contact mechanics with horizontal cleavage tear and resection of the medial meniscus in the human knee. J Bone Joint Surg Am. 2016;98:1829–1836. doi: 10.2106/JBJS.16.00214. [DOI] [PubMed] [Google Scholar]
- 5.Lee B.S., Bin S.I., Kim J.M. Articular cartilage degenerates after subtotal/total lateral meniscectomy but radiographic arthrosis progression is reduced after meniscal transplantation. Am J Sports Med. 2016;44:159–165. doi: 10.1177/0363546515612076. [DOI] [PubMed] [Google Scholar]
- 6.Marzo J.M., Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37:124–129. doi: 10.1177/0363546508323254. [DOI] [PubMed] [Google Scholar]
- 7.Muriuki M.G., Tuason D.A., Tucker B.G., Harner C.D. Changes in tibiofemoral contact mechanics following radial split and vertical tears of the medial meniscus an in vitro investigation of the efficacy of arthroscopic repair. J Bone Joint Surg Am. 2011;93:1089–1095. doi: 10.2106/JBJS.I.01241. [DOI] [PubMed] [Google Scholar]
- 8.Seitz A.M., Lubomierski A., Friemert B., Ignatius A., Durselen L. Effect of partial meniscectomy at the medial posterior horn on tibiofemoral contact mechanics and meniscal hoop strains in human knees. J Orthop Res. 2012;30:934–942. doi: 10.1002/jor.22010. [DOI] [PubMed] [Google Scholar]
- 9.Faucett S.C., Geisler B.P., Chahla J. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: Clinical and economic effectiveness. Am J Sports Med. 2019;47:762–769. doi: 10.1177/0363546518755754. [DOI] [PubMed] [Google Scholar]
- 10.Edd S.N., Netravali N.A., Favre J., Giori N.J., Andriacchi T.P. Alterations in knee kinematics after partial medial meniscectomy are activity dependent. Am J Sports Med. 2015;43:1399–1407. doi: 10.1177/0363546515577360. [DOI] [PubMed] [Google Scholar]
- 11.Johnson R.J., Kettelkamp D.B., Clark W., Leaverton P. Factors affecting late results after meniscectomy. J Bone Joint Surg Am. 1974;56:719–729. [PubMed] [Google Scholar]
- 12.Papalia R., Del Buono A., Osti L., Denaro V., Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: A systematic review. Br Med Bull. 2011;99:89–106. doi: 10.1093/bmb/ldq043. [DOI] [PubMed] [Google Scholar]
- 13.Buckley P.S., Kemler B.R., Robbins C.M. Biomechanical comparison of 3 novel repair techniques for radial tears of the medial meniscus: The 2-tunnel transtibial technique, a "hybrid" horizontal and vertical mattress suture configuration, and a combined "hybrid tunnel" technique. Am J Sports Med. 2019;47:651–658. doi: 10.1177/0363546518816949. [DOI] [PubMed] [Google Scholar]
- 14.Jang S.H., Kim J.G., Ha J.G., Shim J.C. Reducing the size of the meniscal allograft decreases the percentage of extrusion after meniscal allograft transplantation. Arthroscopy. 2011;27:914–922. doi: 10.1016/j.arthro.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade R.F., Wills N.J., Spiridonov S.I., Perkinson S. A prospective outcomes study of meniscal allograft transplantation. Am J Sports Med. 2010;38:1804–1812. doi: 10.1177/0363546510368133. [DOI] [PubMed] [Google Scholar]
- 16.Noyes F.R., Barber-Westin S.D. Long-term survivorship and function of meniscus transplantation. Am J Sports Med. 2016;44:2330–2338. doi: 10.1177/0363546516646375. [DOI] [PubMed] [Google Scholar]
- 17.Riboh J.C., Tilton A.K., Cvetanovich G.L., Campbell K.A., Cole B.J. Meniscal allograft transplantation in the adolescent population. Arthroscopy. 2016;32:1133–1140.e1131. doi: 10.1016/j.arthro.2015.11.041. [DOI] [PubMed] [Google Scholar]
- 18.Rosso F., Bisicchia S., Bonasia D.E., Amendola A. Meniscal allograft transplantation: A systematic review. Am J Sports Med. 2015;43:998–1007. doi: 10.1177/0363546514536021. [DOI] [PubMed] [Google Scholar]
- 19.Padalecki J.R., Jansson K.S., Smith S.D. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42:699–707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 20.Waterman B.R., Rensing N., Cameron K.L., Owens B.D., Pallis M. Survivorship of meniscal allograft transplantation in an athletic patient population. Am J Sports Med. 2016;44:1237–1242. doi: 10.1177/0363546515626184. [DOI] [PubMed] [Google Scholar]
- 21.Shin Y.S., Lee H.N., Sim H.B., Kim H.J., Lee D.H. Polyurethane meniscal scaffolds lead to better clinical outcomes but worse articular cartilage status and greater absolute meniscal extrusion. Knee Surg Sports Traumatol Arthrosc. 2018;26:2227–2238. doi: 10.1007/s00167-017-4650-3. [DOI] [PubMed] [Google Scholar]
- 22.Houck D.A., Kraeutler M.J., Belk J.W., McCarty E.C., Bravman J.T. Similar clinical outcomes following collagen or polyurethane meniscal scaffold implantation: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26:2259–2269. doi: 10.1007/s00167-018-4838-1. [DOI] [PubMed] [Google Scholar]
- 23.Ruprecht J.C., Waanders T.D., Rowland C.R. Meniscus-derived matrix scaffolds promote the integrative repair of meniscal defects. Sci Rep. 2019;9:8719. doi: 10.1038/s41598-019-44855-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nyland J., Campbell K., Kalloub A., Strauss E.J., Kuban K., Caborn D.N.M. Medial meniscus grafting restores normal tibiofemoral contact pressures. Arch Orthop Trauma Surg. 2018;138:361–367. doi: 10.1007/s00402-017-2849-x. [DOI] [PubMed] [Google Scholar]
- 25.Lee S.J., Aadalen K.J., Malaviya P. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34:1334–1344. doi: 10.1177/0363546506286786. [DOI] [PubMed] [Google Scholar]
- 26.Bedi A., Kelly N.H., Baad M. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92:1398–1408. doi: 10.2106/JBJS.I.00539. [DOI] [PubMed] [Google Scholar]
- 27.Efe T., Getgood A., Schofer M.D. The safety and short-term efficacy of a novel polyurethane meniscal scaffold for the treatment of segmental medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc. 2012;20:1822–1830. doi: 10.1007/s00167-011-1779-3. [DOI] [PubMed] [Google Scholar]
- 28.Buma P., van Tienen T., Veth R. The collagen meniscus implant. Expert Rev Med Devices. 2007;4:507–516. doi: 10.1586/17434440.4.4.507. [DOI] [PubMed] [Google Scholar]
- 29.de Groot J.H. Polyurethane scaffolds for meniscal tissue regeneration. Med Device Technol. 2005;16:18–20. [PubMed] [Google Scholar]
- 30.Gastel J.A., Muirhead W.R., Lifrak J.T., Fadale P.D., Hulstyn M.J., Labrador D.P. Meniscal tissue regeneration using a collagenous biomaterial derived from porcine small intestine submucosa. Arthroscopy. 2001;17:151–159. doi: 10.1053/jars.2001.20959. [DOI] [PubMed] [Google Scholar]
- 31.Genovese E., Angeretti M.G., Ronga M. Follow-up of collagen meniscus implants by MRI. Radiol Med. 2007;112:1036–1048. doi: 10.1007/s11547-007-0204-y. [DOI] [PubMed] [Google Scholar]
- 32.Rodkey W.G., DeHaven K.E., Montgomery W.H., III Comparison of the collagen meniscus implant with partial meniscectomy: A prospective randomized trial. J Bone Joint Surg Am. 2008;90:1413–1426. doi: 10.2106/JBJS.G.00656. [DOI] [PubMed] [Google Scholar]
- 33.Rodkey W.G., Steadman J.R., Li S.T. A clinical study of collagen meniscus implants to restore the injured meniscus. Clin Orthop Relat Res. 1999;367:281–292. doi: 10.1097/00003086-199910001-00027. [DOI] [PubMed] [Google Scholar]
- 34.Stabile K.J., Odom D., Smith T.L. An acellular, allograft-derived meniscus scaffold in an ovine model. Arthroscopy. 2010;26:936–948. doi: 10.1016/j.arthro.2009.11.024. [DOI] [PubMed] [Google Scholar]
- 35.Steadman J.R., Rodkey W.G. Tissue-engineered collagen meniscus implants: 5- to 6-year feasibility study results. Arthroscopy. 2005;21:515–525. doi: 10.1016/j.arthro.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 36.Verdonk R., Verdonk P., Huysse W., Forsyth R., Heinrichs E.L. Tissue ingrowth after implantation of a novel, biodegradable polyurethane scaffold for treatment of partial meniscal lesions. Am J Sports Med. 2011;39:774–782. doi: 10.1177/0363546511398040. [DOI] [PubMed] [Google Scholar]
- 37.Grassi A., Zaffagnini S., Marcheggiani Muccioli G.M., Benzi A., Marcacci M. Clinical outcomes and complications of a collagen meniscus implant: A systematic review. Int Orthop. 2014;38:1945–1953. doi: 10.1007/s00264-014-2408-9. [DOI] [PubMed] [Google Scholar]
- 38.Karia M., Ghaly Y., Al-Hadithy N., Mordecai S., Gupte C. Current concepts in the techniques, indications and outcomes of meniscal repairs. Eur J Orthop Surg Traumatol. 2019;29:509–520. doi: 10.1007/s00590-018-2317-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Assimakopoulos A.P., Katonis P.G., Agapitos M.V., Exarchou E.I. The innervations of the human meniscus. Clin Orthop Relat Res. 1992;275:232–236. [PubMed] [Google Scholar]
- 40.Day B., Mackenzie W.G., Shim S.S., Leung G. The vascular and nerve supply of the human meniscus. Arthroscopy. 1985;1:58–62. doi: 10.1016/s0749-8063(85)80080-3. [DOI] [PubMed] [Google Scholar]
- 41.Zimny M.L. Mechanoreceptors in articular tissues. Am J Anat. 1988;64:883–888. doi: 10.1002/aja.1001820103. [DOI] [PubMed] [Google Scholar]
- 42.O’Connor B.L., McConnaughey J.S. The structure and innervation of cat knee menisci, and their relation to a “sensory hypothesis” of meniscal function. Am J Anat. 1978;153:431–442. doi: 10.1002/aja.1001530306. [DOI] [PubMed] [Google Scholar]
- 43.Kennedy J.C., Alexander I.J., Hayes K.C. Nerve supply of the human knee and its functional importance. Am J Sports Med. 1982;10:329–335. doi: 10.1177/036354658201000601. [DOI] [PubMed] [Google Scholar]
- 44.Dye S.F., Vaupel G.L., Dye C.C. Conscious neurosensory mapping of the internal structures of the human knee without intraarticular anesthesia. Am J Sports Med. 1998;26:773–777. doi: 10.1177/03635465980260060601. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video outlines the step-by-step illustration of anterior cruciate ligament reconstruction and segmental medial meniscus transplant in a patient with focal medial meniscus deficiency. We perform this technique by first performing a diagnostic arthroscopy, which reveals the region of full-thickness segmental meniscus deficiency. After debridement, a spinal needle is passed from outside-in to determine the location of the defect and to pass a shuttling suture to eventually shuttle the prepared meniscus transplant into the defect. Next, the meniscus allograft is prepared by marking both the posterior and anterior aspects, and the desired length of transplant is measured. The 20-mm allograft of meniscus is excised from the donor meniscus. Preparation of the graft consists of No. 2 nonabsorbable sutures around the periphery of the graft. A total of 5 sutures are passed around the periphery in a vertical mattress configuration. A midline incision and a medial parapatellar arthrotomy are performed to accomplish both the proximal tibia osteotomy and the 2 osteochondral allograft plugs. The same arthrotomy is used to shuttle the meniscus graft. Once the allograft is positioned intraarticularly, the 5 vertical mattress sutures are passed through the capsule using a needle-shuttling device. The anterior and posterior regions of the graft are then incorporated into native tissue using No. 2 nonabsorbable sutures. The transplant is further anchored anteriorly to the tibia with a single 2.9-mm suture anchor placed at the periphery of the tibia. The final construct was intact to probing and stable.
This video outlines the step-by-step illustration of anterior cruciate ligament reconstruction and segmental medial meniscus transplant in a patient with focal medial meniscus deficiency. We perform this technique by first performing a diagnostic arthroscopy, which reveals the region of full-thickness segmental meniscus deficiency. After debridement, a spinal needle is passed from outside-in to determine the location of the defect and to pass a shuttling suture to eventually shuttle the prepared meniscus transplant into the defect. Next, the meniscus allograft is prepared by marking both the posterior and anterior aspects, and the desired length of transplant is measured. The 20-mm allograft of meniscus is excised from the donor meniscus. Preparation of the graft consists of No. 2 nonabsorbable sutures around the periphery of the graft. A total of 5 sutures are passed around the periphery in a vertical mattress configuration. A midline incision and a medial parapatellar arthrotomy are performed to accomplish both the proximal tibia osteotomy and the 2 osteochondral allograft plugs. The same arthrotomy is used to shuttle the meniscus graft. Once the allograft is positioned intraarticularly, the 5 vertical mattress sutures are passed through the capsule using a needle-shuttling device. The anterior and posterior regions of the graft are then incorporated into native tissue using No. 2 nonabsorbable sutures. The transplant is further anchored anteriorly to the tibia with a single 2.9-mm suture anchor placed at the periphery of the tibia. The final construct was intact to probing and stable.