Abstract
Irreparable posterior-superior rotator cuff tear is encountered quite often in clinical practice. Bridging the tendon defect with various materials is reasonable. However, optimal bridging structures and techniques are still being pursued. We introduce a rotator cuff bridging technique, rooting rotator cuff reconstruction. In this technique, autogenous tendon is used to make grafts. On the medial side, the graft tendons are suspended on the rotator cuff tendon. On the lateral side, the graft tendons are placed into tunnels through the tuberosities. The most critical steps of this technique are properly fabricating the humeral tunnels and suspending the graft tendons onto the rotator cuff tendon. We believe this technique will shed light on rotator cuff reconstruction.
Technique Video
Rotator Cuff Reconstruction for Irreparable Posterior-Superior Rotator Cuff Tear. 1. This procedure is performed on the right shoulder. The arthroscope is placed through the midlateral portal. One bone tunnel–aiming device is placed through an accessory anterolateral portal. 2. Tunnel I is created through the lesser tuberosity, at the anterior edge of the bicipital groove. Tunnel II is created through the greater tuberosity, at the posterior edge of the bicipital groove. Guide sutures are placed through the tunnels. 3. The arthroscope is placed through the posterior-lateral portal. The bone tunnel–aiming device is placed through an accessory lateral portal. 4. Tunnel III is created through the middle part of the greater tuberosity. Tunnel IV is created through the posterior part of the greater tuberosity. Guide sutures are placed in the tunnels. 5. The superior fossa portal is created. A suture retriever is placed through the supraspinatus. The guide suture in tunnel IV is retrieved through the supraspinatus. 6. The supraspinatus graft is passed through the supraspinatus into tunnel IV. The superior part of the graft is pulled into tunnel III. 7. A suture retriever is placed through the infraspinatus. The guide suture in tunnel II is retrieved through the infraspinatus. 8. The infraspinatus graft is passed through the infraspinatus into tunnel II. The superior part of the graft is pulled into tunnel I. 9. The scope is placed into the anterior subdeltoid space. The 2 ends of the infraspinatus graft are fixed by tying the sutures over the bone bridge. 10. The scope is placed into the lateral subdeltoid space. The 2 ends of the supraspinatus grafts are fixed with a knotless suture anchor.
Irreparable posterior-superior rotator cuff tears (IPSRCTs) are common pathologies related to shoulder pain and dysfunction. Although many methods address IPSRCTs,1, 2, 3 a method that has predictable results still needs to be explored.4 Rotator cuff reconstruction means using a structure or structures to bridge the rotator cuff and the greater tuberosity and restore the force chain of the defect rotator cuff. Various bridging structures, which include autograft, allograft, xenograft, and synthetic patch, have been reported.5,6 The optimal bridging structures and techniques are still being pursued.
In this article, we introduce a rotator cuff reconstruction technique named rooting rotator cuff reconstruction. In this technique, we bridge the rotator cuff with autogenous tendon graft, suspend the grafts on the rotator cuff tendons for medial connections, and place the graft tendons into transhumeral tunnels for lateral connection. We use the word rooting because on the lateral side, the bridging structures root into bone tunnels instead of being pressed onto the bone surface. This technique is indicated for IPSRCT with a usable posterior-superior rotator cuff (Table 1).
Table 1.
Terms Regarding Irreparable Posterior-Superior Rotator Cuff Tear With Usable Posterior-Superior Rotator Cuff
| 1. Posterior-superior rotator cuff tear. |
| Posterior-superior rotator cuff tear is defined in our clinical practice as a tear that involves mainly the supraspinatus and infraspinatus. When the superior part of the subscapularis or teres minor is also involved but is reparable, the entire tear is also defined as a posterior-superior rotator cuff tear. |
| 2. Irreparable posterior-superior rotator cuff tear. |
| Irreparable posterior-superior rotator cuff tear is defined when, after routine rotator cuff release and lateralization, as well as footprint medialization, the tendon-footprint overlap at the apex of the rotator cuff defect is less than 5 mm, in case of a large or massive U- or V-shaped rotator cuff tear. |
| 3. Single usable or unusable rotator cuff in rotator cuff tear. |
| The usability of a single rotator cuff (the supraspinatus or infraspinatus) is evaluated according to atrophy and fatty infiltration evaluated on magnetic resonance images, as well as the tendon length evaluated during operation. When rotator muscle atrophy is over two-thirds or fatty infiltration is grade IV, or the tendon length is less than 5 mm, the torn rotator cuff is defined as unusable. When rotator muscle atrophy is less than two-thirds, fatty infiltration is grade III or less, and the tendon length is 5 mm or greater, the torn rotator cuff is defined as usable. |
| 4. Usable and unusable entire posterior-superior rotator cuff in posterior-superior rotator cuff tear. |
| When the supraspinatus or the infraspinatus is usable, the entire posterior-superior rotator cuff is defined as usable. When both the supraspinatus and infraspinatus are unusable, the entire posterior-superior rotator cuff is defined as unusable. |
Surgical Procedure
The operation is performed in the lateral decubitus position with the arm in 30-degree abduction. Combined conditions are first addressed though routine portals. Rotator cuff release and footprint medialization are first performed. When the rotator cuff is defined as irreparable and rotator cuff reconstruction is finally indicated (Table 1), the rotator cuff is pulled slightly lateral to detect its potential amplitude of lateral excursion without obvious tension, as a reference for final tension of the structure.
Preparing the Tendon Grafts
A 2- to 3-cm-long longitudinal incision is made 2 cm proximal to the posterior styloid of the distal fibula. The peroneus longus tendon (PLT) is harvested from the incision and cut into 2 segments with a length of 10 to 12 cm of each segment. Both ends of each tendon segment are sutured with No. 2 ultra-high molecular weight polyethylene sutures (Smith & Nephew, Andover, MA, U.S.A.) in a whip-stitch style (Fig 1, Table 2).
Fig 1.
Two tendon grafts made from the peroneus longus tendon.
Table 2.
Step-by-Step Surgical Procedure of Rotator Cuff Reconstruction for Irreparable Posterior-Superior Rotator Cuff Tear
|
|
|
|
|
|
|
|
|
|
|
Creating Humeral Tunnels Through the Tuberosities
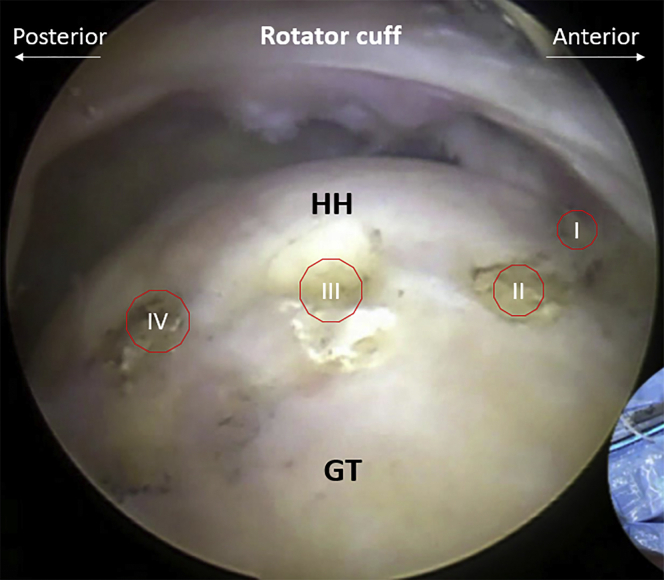
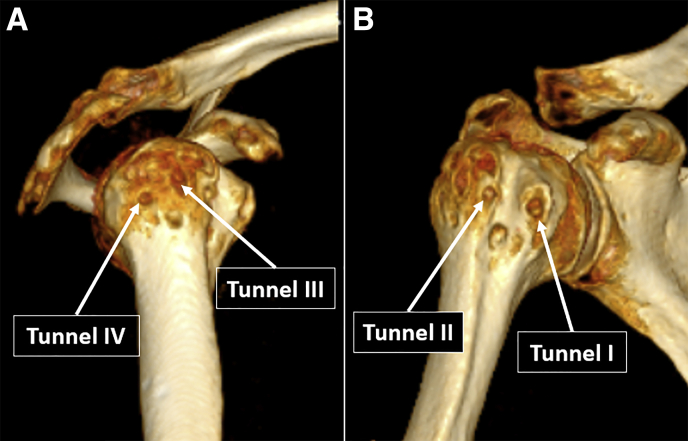
A 7-mm offset point-to-point tibial tunnel aiming device, which is usually used for anterior cruciate ligament reconstruction of the knee, is used to create humeral tunnels through the tuberosities (Video 1). Four longitudinal tunnels, which are arranged from the anterior to the posterior side and named tunnels I, II, III, and IV, respectively, are fabricated through the tuberosities. Tunnels I and II are located at the medial and lateral sides of the bicipital groove, respectively; tunnels III and IV pass through the middle and posterior part of the greater tuberosity. The proximal orifices of the humeral tunnels are located at the cartilage edge and arranged sequentially from the anterior to posterior side (Fig 2). The lateral orifices of the humeral tunnels are located approximately 3 cm distal to the tip of the corresponding tuberosities (Fig 3). The tunnels are 0.5 mm smaller than the tendon.
Fig 2.
The location of the proximal orifices of the humeral tunnels (arthroscopic subacromial view of right shoulder through the midlateral portal). GT, greater tuberosity; HH, humeral head.
Fig 3.
Postoperative computed tomography of the right shoulder indicating distal offices of tunnels III and IV (A) and tunnels I and II (B).
The arthroscope is placed into the subacromial space through the midlateral portal. One switching stick is placed into the anterior subdeltoid space to elevate the anterior deltoid. One accessory anterolateral portal is fabricated to put the hook of the tunnel-aiming device into the subacromial space and set at the desired location near the cartilage edge (Fig 4). A K-wire is placed through the tunnel-aiming pin and the anterior deltoid to the anterior edge of the bicipital groove. When the desired location of the distal orifice of the tunnel is confirmed, the K-wire and a cannulated drill are drilled in sequentially to create tunnel I. One guide suture is placed through the tunnel. Then, tunnel II is created in the same way, and one guide suture is placed (Fig 5).
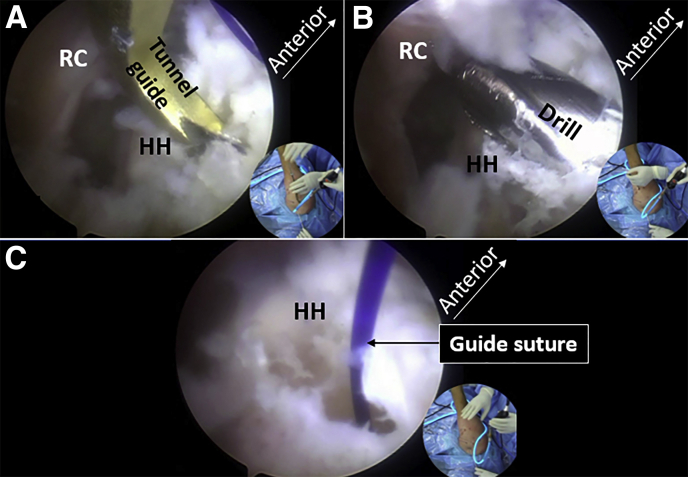
Fig 4.
Fabricating tunnel I (arthroscopic subacromial and subanterior deltoid view of right shoulder through the midlateral portal). (A) Setting the tip of the tunnel-aiming device at the desired location of the proximal orifice of tunnel I. (B, C) Drilling the K-wire through the lesser tuberosity. (D) Creating a tunnel by drilling over the K-wire. (E) Placing the guide suture into the canulated drill. HH, humeral head; RC, rotator cuff.
Fig 5.
Fabricating tunnel II (arthroscopic subacromial view of right shoulder through the midlateral portal). (A) Creating the tunnel with a drill. (B) Placing a guide suture through the tunnel. HH, humeral head; RC, rotator cuff.
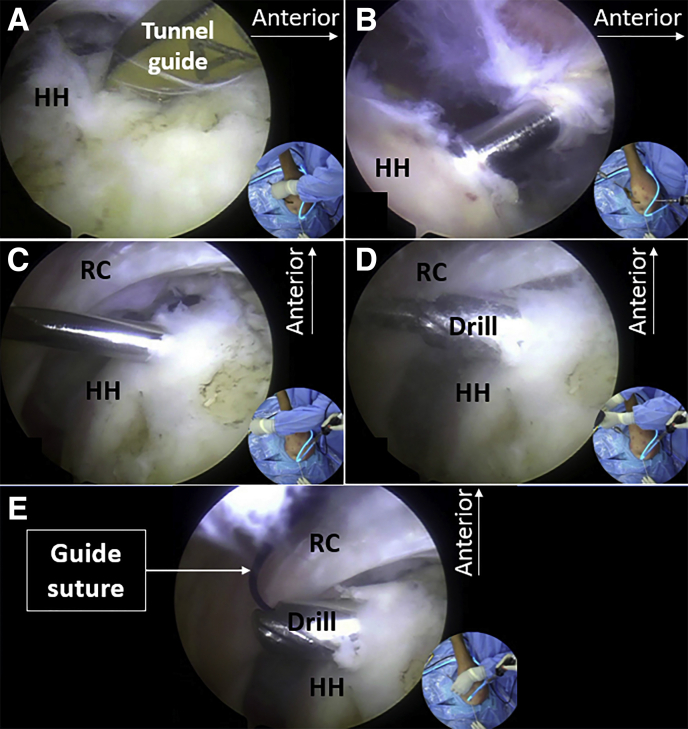
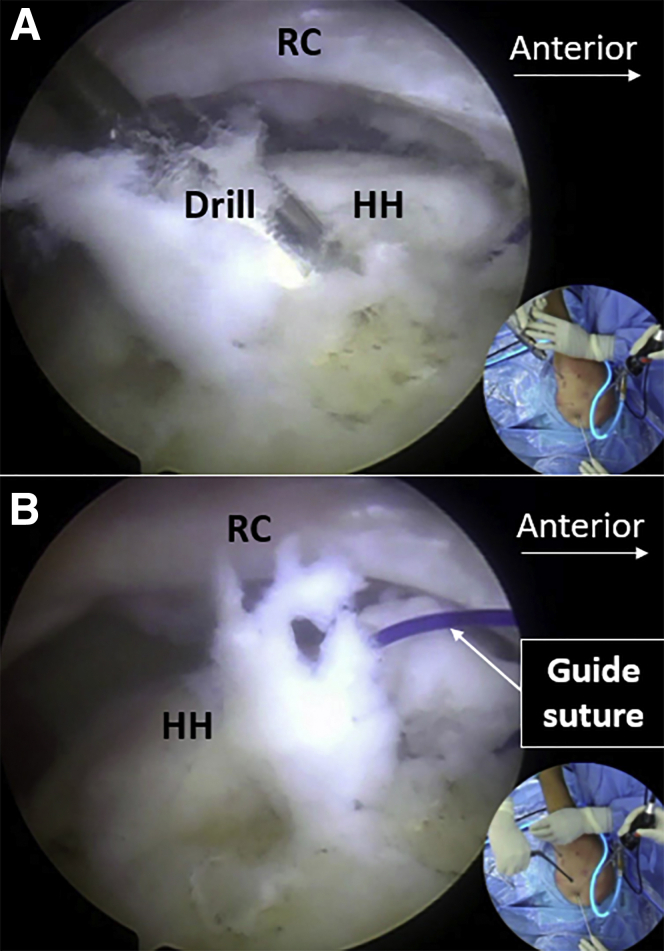
The arthroscope is placed through the posterior-lateral portal to the subacromial space, and the tunnel-aiming device is placed through the midlateral portal or an accessory lateral portal and set at the desired location near the cartilage edge. A K-wire is placed through the lateral deltoid to the lateral side of the proximal humerus. When the desired location of the distal orifice of the tunnel is confirmed, the K-wire and a cannulated drill are drilled in sequentially. In this way, tunnels III and IV are created, with one guide suture placed in each tunnel (Figs 6 and 7).
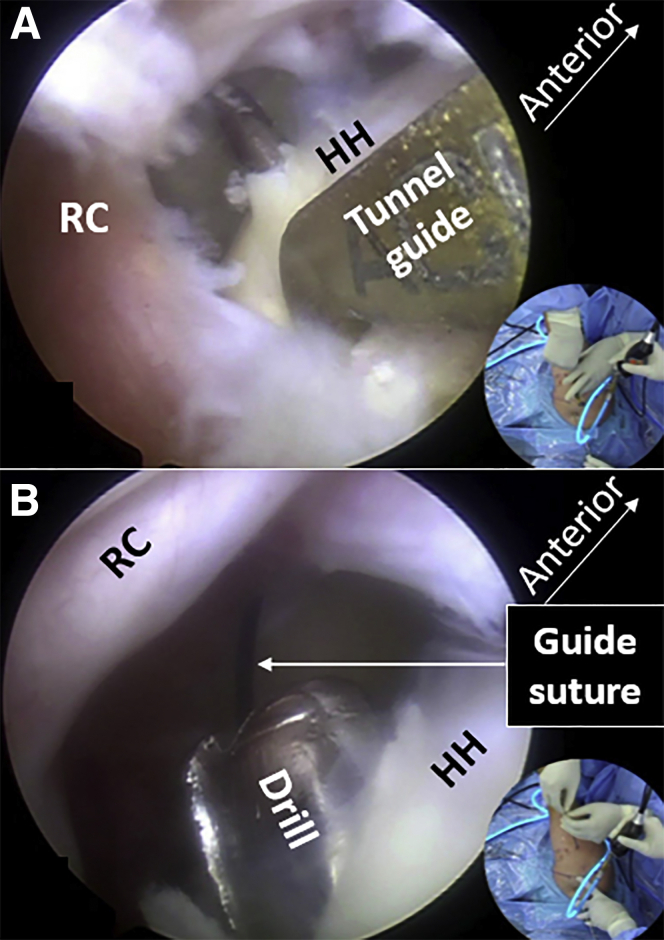
Fig 6.
Fabricating tunnel III (arthroscopic subacromial view of right shoulder through the posterior-lateral portal). (A) Setting the tunnel-aiming device. (B) Drilling the tunnel. (C) Placing the guide suture. HH, humeral head; RC, rotator cuff.
Fig 7.
Fabricating tunnel IV (arthroscopic subacromial view of right shoulder through the posterior-lateral portal). (A) Drilling the K-wire through the humeral head. (B) Placing the guide suture through the canulated drill. HH, humeral head; RC, rotator cuff.
Placing the Supraspinatus Graft
A superior fossa portal is created. A suture retriever is placed in this portal and passed through the supraspinatus at its muscle-tendon conjunction to its underside. The guide suture in tunnel IV is retrieved through the supraspinatus (Fig 8). One graft tendon is placed through the supraspinatus, from the superior to the inferior side, into tunnel IV for a length of 3 cm. The superior part of the graft is pulled into the subacromial space to fold the graft and then pulled into tunnel III (Fig 9). In this way, the graft tendon is suspended on the supraspinatus tendon (Fig 10). Both ends of the graft are pulled to tension the supraspinatus.
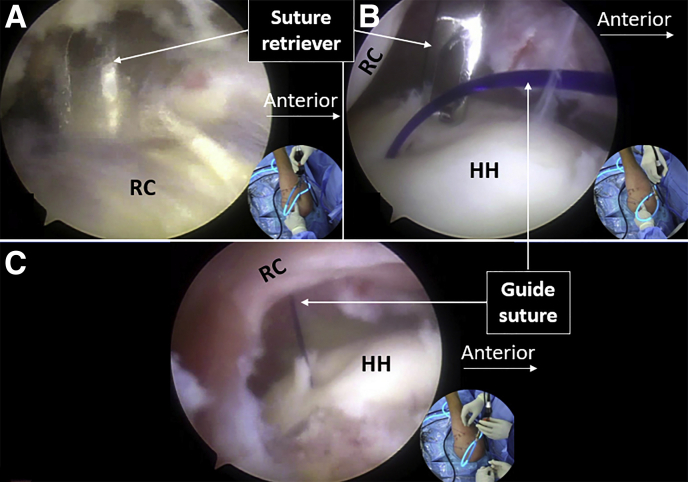
Fig 8.
Passing the guide suture for the graft through the supraspinatus (arthroscopic subacromial view of right shoulder through the posterior-lateral portal). (A) Pushing a suture retriever into the supraspinatus at the tendon-muscle conjunction. (B) Passing the suture retriever to the underside of the supraspinatus. (C) Retrieving the guide suture from tunnel IV through the supraspinatus. HH, humeral head; RC, rotator cuff.
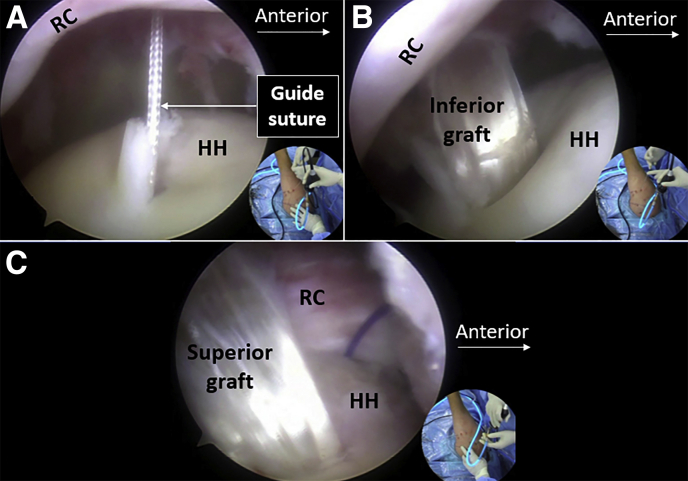
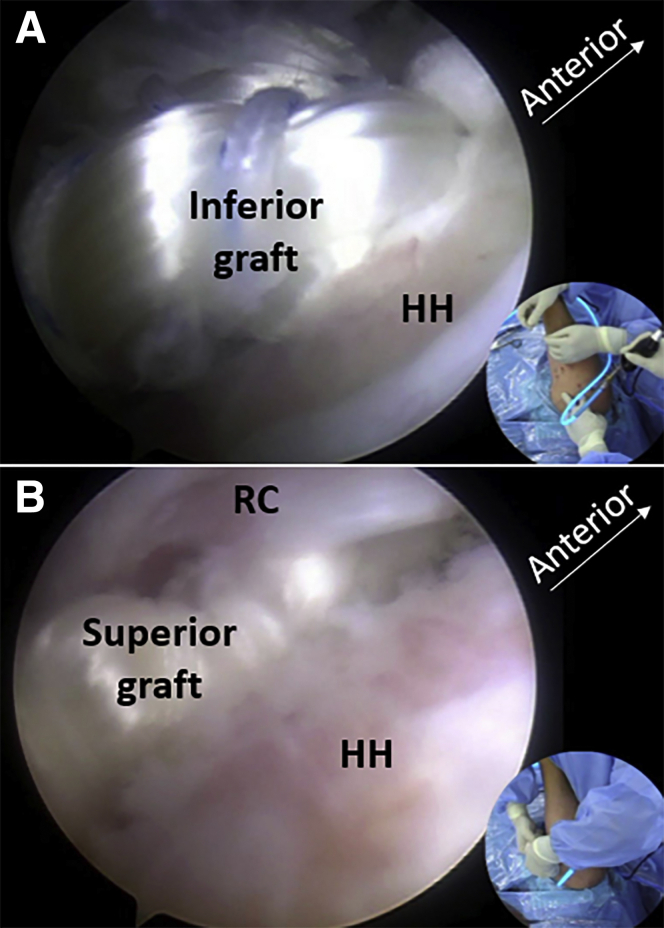
Fig 9.
Placement of the tendon graft for the supraspinatus (arthroscopic subacromial view of right shoulder through the posterior-lateral portal). (A) Replacing the original PDS II guide suture with a No. 2 ultra-high molecular weight polyethylene suture (Smith & Nephew) suture. (B) Placing the tendon graft through the supraspinatus into tunnel IV. (C) Placing the superior part of the tendon graft into tunnel III. HH, humeral head; RC, rotator cuff.
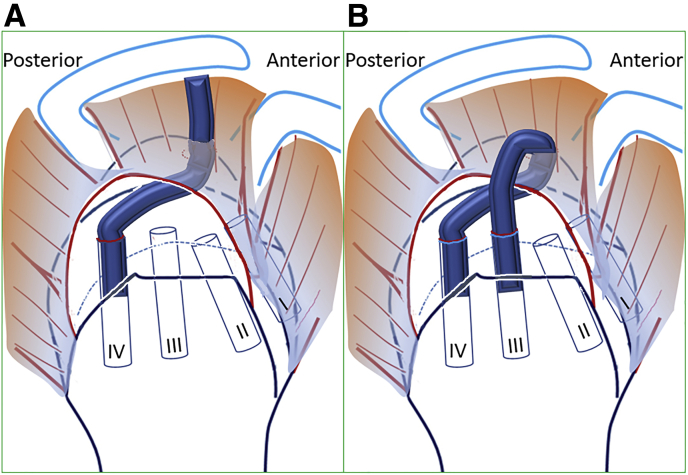
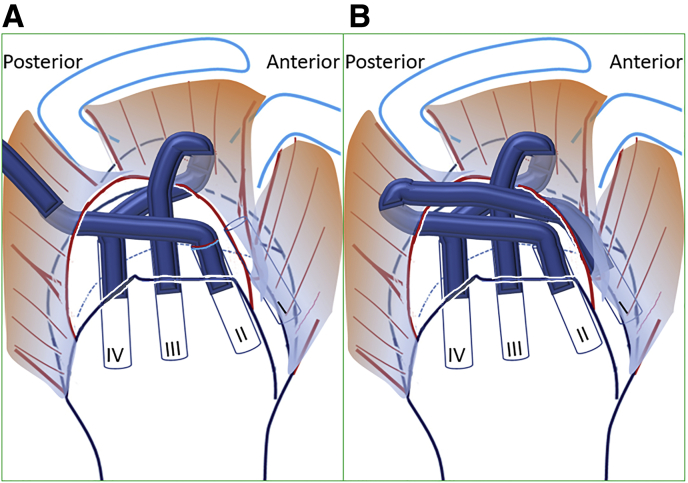
Fig 10.
Illustration of graft placement for the supraspinatus (lateral view of right shoulder). (A) Placing the tendon graft through the supraspinatus into tunnel IV. (B) Placing the superior part of the tendon graft into tunnel III and suspending the graft on the supraspinatus tendon.
Placing the Infraspinatus Graft
A suture retriever is placed in the posterior portal and passed through the tendon-muscle conjunction of the infraspinatus. The guide suture in tunnel II is pulled through the infraspinatus. The tendon graft for the infraspinatus is passed through the infraspinatus from the posterior superior to the anterior inferior side and into tunnel II for a length of 3 cm (Fig 11). The posterior part of the graft is pulled into the subacromial space to suspend the graft on the infraspinatus tendon and pulled into tunnel I (Fig 12). Both ends of the graft are tightened to tension the infraspinatus (Fig 13).
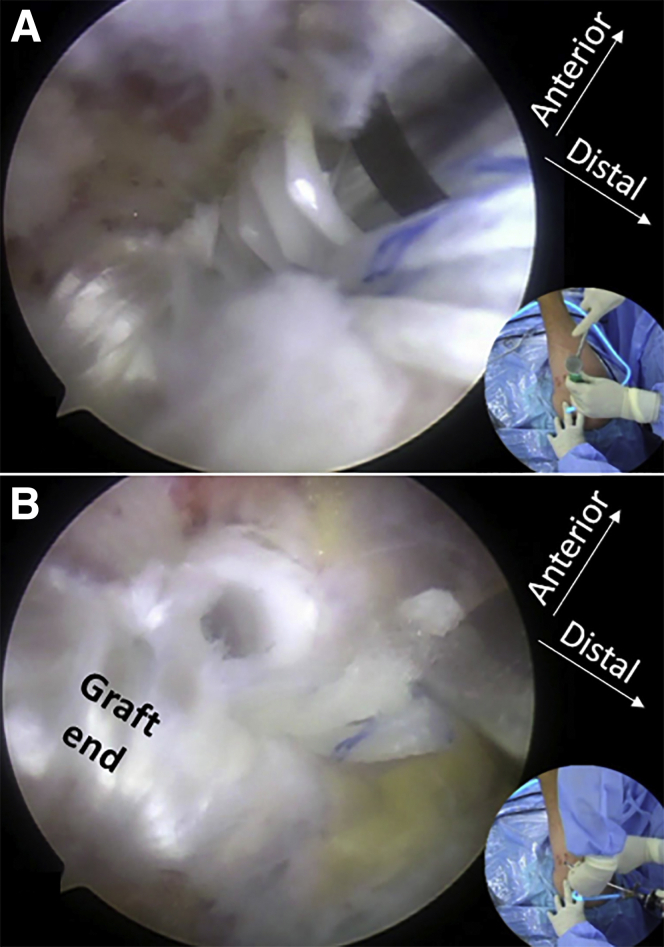
Fig 11.
Placement of the tendon graft for the infraspinatus (arthroscopic subacromial view of right shoulder through the posterior-lateral portal). (A) Placing the tendon graft through the infraspinatus into tunnel II. (B) Placing the superior part of the tendon graft into tunnel I. HH, humeral head; RC, rotator cuff.
Fig 12.
Illustration of graft placement for the infraspinatus (lateral view of right shoulder). (A) Placing the tendon graft through the infraspinatus into tunnel II. (B) Placing the superior part of the tendon graft into tunnel I and suspending the graft on the infraspinatus tendon.
Fig 13.
Final view of the grafts for the supraspinatus (A) and infraspinatus (B) near the tuberosities (arthroscopic subacromial view of right shoulder through the midlateral portal).
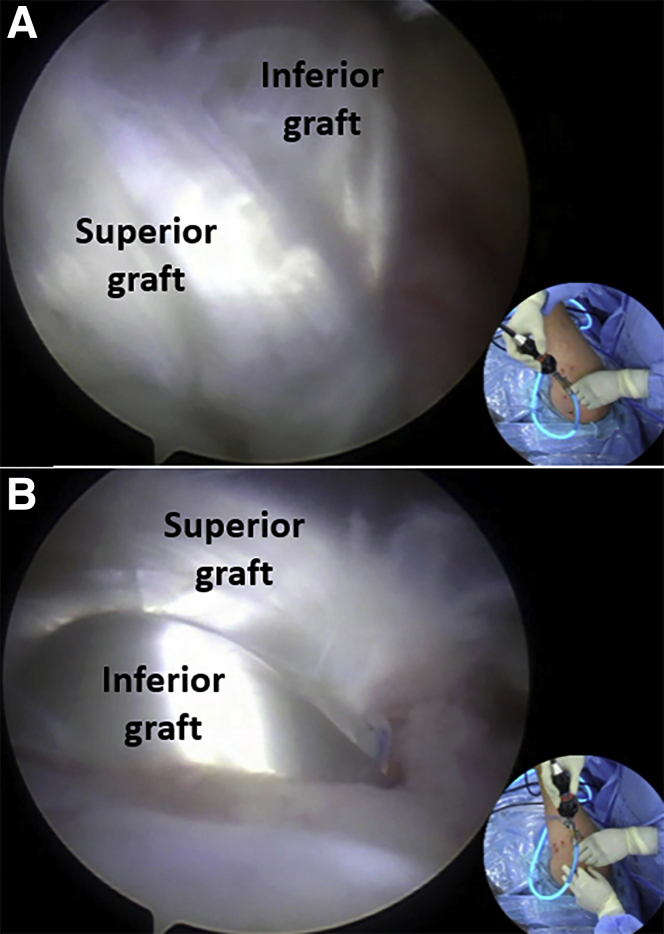
Distal Fixation of the Grafts
For each graft, when none of the graft ends protrudes the distal orifice of the humeral tunnel, the braiding sutures from the graft ends are tied over the bone bridge between the 2 distal orifices (Fig 14). When any ends of the graft protrude the distal orifice, 1 knotless suture anchor is used to fix both ends of the graft at a site distally (Fig 15).
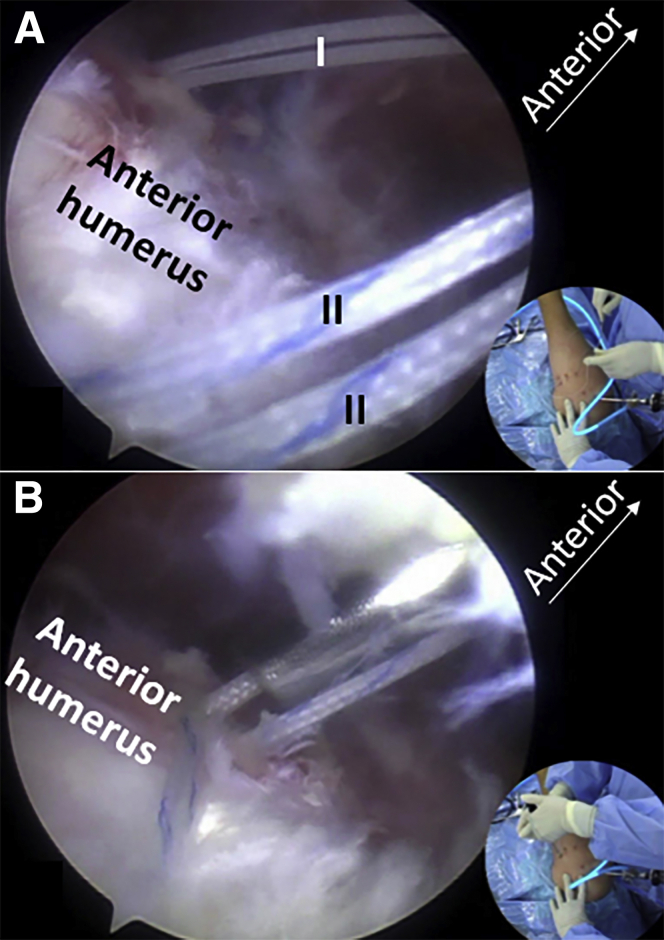
Fig 14.
Finding the braiding suture from the ends of infraspinatus graft (A) and tying the suture over the bone bridge between the orifices for graft fixation (B) (arthroscopic subanterior deltoid view of right shoulder through the midlateral portal). I, sutures from tunnel I. II, sutures from tunnel II.
Fig 15.
Fixing the ends of the supraspinatus graft with a knotless lateral row suture anchor (Arthrex, Naples, FL, U.S.A.) due to graft tend protrusion (arthroscopic sublateral deltoid view of right shoulder through the posterior-lateral portal). (A) View during fixation. (B) View after fixation.
Discussion
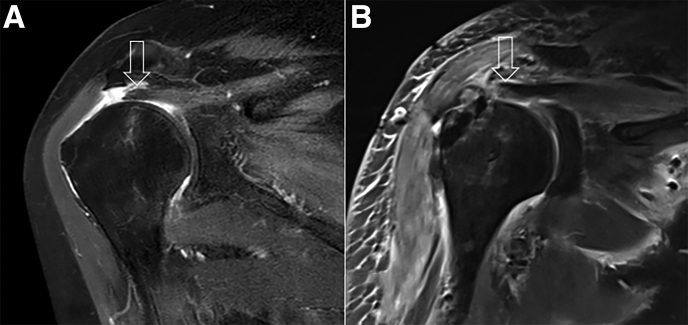
The purpose of rotator cuff reconstruction is to restore the force chain of the native rotator cuff and make the disconnected but usable rotator cuff functional (Fig 16). Compared with superior capsule reconstruction in which structural restoration of the rotator cuff is given up,7,8 rotator cuff reconstruction is more reasonable when the medial rotator cuff structure is usable.9,10
Fig 16.
Preoperative (A) and postoperative (B) coronal view magnetic resonance images of left shoulder. (A) The lateral edge of the rotator cuff (arrow). (B) The restored force chain (arrow).
A successful rotator cuff reconstruction relies on not only a strong time-zero bridging of the rotator cuff and the greater tuberosity but also a reliable terminal stage connection. Thus, the first prerequisite of ideal rotator cuff reconstruction is that eventually, the bridging structure can simultaneously hold the medial rotator cuff tendon and stick to the greater tuberosity satisfactorily, either through biological healing or mechanical holding. The second prerequisite is that the bridging structure has enough strength not only immediately after the operation but also during or after its remodeling.
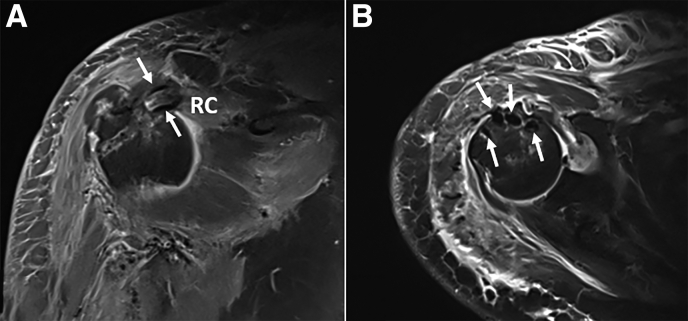
In previous reports of rotator cuff reconstruction, the bridging structure is sutured to the medial rotor cuff. The results depend on the healing between the graft and the rotator cuff, which is unpredictable due to its healing nature between soft tissues.11 In the current technique, the graft tendons are suspended on the rotator cuff tendons. A strong connection is mechanically established between the graft and the rotator cuff regardless of the final healing status, so long as the grafting tendon and the rotator cuff tendon are strong (Fig 17). In most previous reports, the bridging material was laterally pressed to the surface of the native footprint, which resulted in unreliable healing.12 In the current technique, we place the grafting structure into the humeral tunnels for a better tendon-bone healing (Fig 17).13
Fig 17.
Postoperative magnetic resonance images of left shoulder. (A) Coronal view image indicating the graft tendon (arrows) suspending the rotator cuff tendon. (B) Transverse view image indicating the graft ends in the humeral tunnels (arrows).
The pearls and pitfalls of this technique are listed in Table 3, and the advantages and disadvantages of this technique are listed in Table 4. The main risk of this technique is greater tuberosity fracture caused by severe regional osteoporosis and the large bone tunnels. Creating smaller tunnels is helpful. The other risk is axillary nerve injury. Passing the drill through the deltoid with manual reverse rotation may minimize this risk.
Table 3.
Pearls and Pitfalls of Rotator Cuff Reconstruction for Irreparable Posterior-Superior Rotator Cuff Tear
|
|
|
|
|
|
|
Table 4.
Advantages and Disadvantages of Rotator Cuff Reconstruction for Irreparable Posterior-Superior Rotator Cuff Tear
| Advantages |
|
|
| Disadvantages |
|
|
Footnotes
The authors report the following potential conflict of interest or source of funding: Funded by National Natural Science Foundation of China (grants 31972923 and 81772341).
Supplementary Data
Rotator Cuff Reconstruction for Irreparable Posterior-Superior Rotator Cuff Tear. 1. This procedure is performed on the right shoulder. The arthroscope is placed through the midlateral portal. One bone tunnel–aiming device is placed through an accessory anterolateral portal. 2. Tunnel I is created through the lesser tuberosity, at the anterior edge of the bicipital groove. Tunnel II is created through the greater tuberosity, at the posterior edge of the bicipital groove. Guide sutures are placed through the tunnels. 3. The arthroscope is placed through the posterior-lateral portal. The bone tunnel–aiming device is placed through an accessory lateral portal. 4. Tunnel III is created through the middle part of the greater tuberosity. Tunnel IV is created through the posterior part of the greater tuberosity. Guide sutures are placed in the tunnels. 5. The superior fossa portal is created. A suture retriever is placed through the supraspinatus. The guide suture in tunnel IV is retrieved through the supraspinatus. 6. The supraspinatus graft is passed through the supraspinatus into tunnel IV. The superior part of the graft is pulled into tunnel III. 7. A suture retriever is placed through the infraspinatus. The guide suture in tunnel II is retrieved through the infraspinatus. 8. The infraspinatus graft is passed through the infraspinatus into tunnel II. The superior part of the graft is pulled into tunnel I. 9. The scope is placed into the anterior subdeltoid space. The 2 ends of the infraspinatus graft are fixed by tying the sutures over the bone bridge. 10. The scope is placed into the lateral subdeltoid space. The 2 ends of the supraspinatus grafts are fixed with a knotless suture anchor.
References
- 1.Oh J.H., Park M.S., Rhee S.M. Treatment strategy for irreparable rotator cuff tears. Clin Orthop Surg. 2018;10:119–134. doi: 10.4055/cios.2018.10.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Novi M., Kumar A., Paladini P., Porcellini G., Merolla G. Irreparable rotator cuff tears: Challenges and solutions. Orthop Res Rev. 2018;10:93–103. doi: 10.2147/ORR.S151259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carver T.J., Kraeutler M.J., Smith J.R., Bravman J.T., McCarty E.C. Nonarthroplasty surgical treatment options for massive, irreparable rotator cuff tears. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118805385. :2325967118805385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kooistra B., Gurnani N., Weening A., van den Bekerom M., van Deurzen D. Low level of evidence for all treatment modalities for irreparable posterosuperior rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2019;27:4038–4048. doi: 10.1007/s00167-019-05710-0. [DOI] [PubMed] [Google Scholar]
- 5.Lewington M.R., Ferguson D.P., Smith T.D., Burks R., Coady C., Wong I.H. Graft utilization in the bridging reconstruction of irreparable rotator cuff tears: A systematic review. Am J Sports Med. 2017;45:3149–3157. doi: 10.1177/0363546517694355. [DOI] [PubMed] [Google Scholar]
- 6.Jones C.R., Snyder S.J. Massive irreparable rotator cuff tears: A solution that bridges the gap. Sports Med Arthrosc Rev. 2015;23:130–138. doi: 10.1097/JSA.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 7.Zastrow R.K., London D.A., Parsons B.O., Cagle P.J. Superior capsule reconstruction for irreparable rotator cuff tears: A systematic review. Arthroscopy. 2019;35:2525–2534.e1. doi: 10.1016/j.arthro.2019.02.053. [DOI] [PubMed] [Google Scholar]
- 8.Dimock R.A.C., Malik S., Consigliere P., Imam M.A., Narvani A.A. Superior capsule reconstruction: What do we know? Arch Bone Jt Surg. 2019;7:3–11. [PMC free article] [PubMed] [Google Scholar]
- 9.Lewington M.R., Ferguson D.P., Smith T.D., Burks R., Coady C., Wong I.H. Graft utilization in the bridging reconstruction of irreparable rotator cuff tears: A systematic review. Am J Sports Med. 2017;45:3149–3157. doi: 10.1177/0363546517694355. [DOI] [PubMed] [Google Scholar]
- 10.Karuppaiah K., Sinha J. Scaffolds in the management of massive rotator cuff tears: Current concepts and literature review. EFORT Open Rev. 2019;4:557–566. doi: 10.1302/2058-5241.4.180040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mori D., Funakoshi N., Yamashita F., Wakabayashi T. Effect of fatty degeneration of the infraspinatus on the efficacy of arthroscopic patch autograft procedure for large to massive rotator cuff tears. Am J Sports Med. 2015;43:1108–1117. doi: 10.1177/0363546515569680. [DOI] [PubMed] [Google Scholar]
- 12.Jones C.R., Snyder S.J. Massive irreparable rotator cuff tears: A solution that bridges the gap. Sports Med Arthrosc. 2015;23:130–138. doi: 10.1097/JSA.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 13.Li X., Shen P., Su W., Zhao S., Zhao J. Into-tunnel repair versus onto-surface repair for rotator cuff tears in a rabbit model. Am J Sports Med. 2018;46:1711–1719. doi: 10.1177/0363546518764685. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Rotator Cuff Reconstruction for Irreparable Posterior-Superior Rotator Cuff Tear. 1. This procedure is performed on the right shoulder. The arthroscope is placed through the midlateral portal. One bone tunnel–aiming device is placed through an accessory anterolateral portal. 2. Tunnel I is created through the lesser tuberosity, at the anterior edge of the bicipital groove. Tunnel II is created through the greater tuberosity, at the posterior edge of the bicipital groove. Guide sutures are placed through the tunnels. 3. The arthroscope is placed through the posterior-lateral portal. The bone tunnel–aiming device is placed through an accessory lateral portal. 4. Tunnel III is created through the middle part of the greater tuberosity. Tunnel IV is created through the posterior part of the greater tuberosity. Guide sutures are placed in the tunnels. 5. The superior fossa portal is created. A suture retriever is placed through the supraspinatus. The guide suture in tunnel IV is retrieved through the supraspinatus. 6. The supraspinatus graft is passed through the supraspinatus into tunnel IV. The superior part of the graft is pulled into tunnel III. 7. A suture retriever is placed through the infraspinatus. The guide suture in tunnel II is retrieved through the infraspinatus. 8. The infraspinatus graft is passed through the infraspinatus into tunnel II. The superior part of the graft is pulled into tunnel I. 9. The scope is placed into the anterior subdeltoid space. The 2 ends of the infraspinatus graft are fixed by tying the sutures over the bone bridge. 10. The scope is placed into the lateral subdeltoid space. The 2 ends of the supraspinatus grafts are fixed with a knotless suture anchor.
Rotator Cuff Reconstruction for Irreparable Posterior-Superior Rotator Cuff Tear. 1. This procedure is performed on the right shoulder. The arthroscope is placed through the midlateral portal. One bone tunnel–aiming device is placed through an accessory anterolateral portal. 2. Tunnel I is created through the lesser tuberosity, at the anterior edge of the bicipital groove. Tunnel II is created through the greater tuberosity, at the posterior edge of the bicipital groove. Guide sutures are placed through the tunnels. 3. The arthroscope is placed through the posterior-lateral portal. The bone tunnel–aiming device is placed through an accessory lateral portal. 4. Tunnel III is created through the middle part of the greater tuberosity. Tunnel IV is created through the posterior part of the greater tuberosity. Guide sutures are placed in the tunnels. 5. The superior fossa portal is created. A suture retriever is placed through the supraspinatus. The guide suture in tunnel IV is retrieved through the supraspinatus. 6. The supraspinatus graft is passed through the supraspinatus into tunnel IV. The superior part of the graft is pulled into tunnel III. 7. A suture retriever is placed through the infraspinatus. The guide suture in tunnel II is retrieved through the infraspinatus. 8. The infraspinatus graft is passed through the infraspinatus into tunnel II. The superior part of the graft is pulled into tunnel I. 9. The scope is placed into the anterior subdeltoid space. The 2 ends of the infraspinatus graft are fixed by tying the sutures over the bone bridge. 10. The scope is placed into the lateral subdeltoid space. The 2 ends of the supraspinatus grafts are fixed with a knotless suture anchor.