Abstract
Tears of the rotator cuff tendons can occur that do not allow anatomic footprint restoration yet may not be large enough to require a superior capsular reconstruction technique. Typically, these intermediate-sized tears are addressed with a medialized repair or partial repair technique. A partially repaired rotator cuff tendon, however, can lead to a high retear rate, as the repaired tendon is required to serve as both a dynamic tendon and a static ligamentous stabilizer. One potential static support, as a nearby autologous graft donor, is the proximal long head biceps tendon. The purpose of this Technical Note is to describe a surgical technique for an anterior cable reconstruction using the proximal biceps tendon for large rotator cuff defects.
Technique Video
Coronal T2 magnetic resonance imaging of the shoulder shows a full-thickness tear involving the supraspinatus and infraspinatus tendons (12-19 seconds). Shoulder arthroscopy is performed in the lateral decubitus position; viewing from a posterior portal, diagnostic arthroscopy is performed. Evaluation of the biceps tendon demonstrates an intact biceps anchor without significant pathology involving the proximal aspect of the biceps tendon (13-32 seconds). A full-thickness tear involving the supraspinatus and infraspinatus tendon is confirmed and a single-row repair of the infraspinatus is performed using a single tripled-loaded suture 5.5-mm Corkscrew anchor (33-45 seconds). After repair of the infraspinatus tendon, residual dysfunction of the superior capsule is seen. To provide further ligamentous support to the repaired tendon, a reconstruction of the anterior cable is performed using the nearby biceps tendon (46-57 seconds). Reconstruction begins with creation of a trough adjacent to the repaired tendon using a 5.0-mm diameter burr. Within the trough, adjacent to the articular cartilage, a double loaded 5.5-mm diameter Corkscrew anchor is placed (58 seconds to 1 minute, 12 seconds). Loop-around fixation is performed by passing the sutures around the biceps tendon, as opposed to through the tendon, to not disrupt the integrity of the graft (1 minute, 15 seconds to 1 minute, 20 seconds). Next, 2 separate #2 FiberWires are passed separately through the repaired tendon edge and the other limb is again passed around the biceps tendon and not through the tendon (1 minute, 21 seconds to 1 minute, 30 seconds). Before securing the graft in position, the arm is rotated to 30° of external rotation to obtain optimal length of the biceps tendon so as not to overconstrain the glenohumeral joint. With the arm in position, starting at the suture anchor, the suture limbs are tied to stabilize the biceps tendon in the trough (1 minute, 31 seconds to 1 minute, 55 seconds). The biceps tendon graft is then linked to the repaired rotator cuff tendon with separate side to side ties of the suture limbs. Again, importance is emphasized in maintaining the arm positioned in 30° of external rotation while the reconstructed anterior cable is coupled to the repaired tendon. Once the biceps tendon and rotator cuff are joined, rotation of the arm is checked to ensure no constrains in motion are observed (1 minute, 56 seconds to 2 minutes, 50 seconds). At the edge of the greater tuberosity, the graft is released from the remaining biceps with use of arthroscopic scissors and ablation probe. A #2 FiberWire is passed through the transected lateral edge of the biceps graft and then secured over the lateral edge of the greater tuberosity with a 4.75-mm SwiveLock anchor. This lateral anchor fixation provides graft end stability (2 minutes, 52 seconds to 3 minutes, 22 seconds). The coupled construct of a static ligamentous support and a dynamic tendon allows unrestricted rotational motion while at the same time providing superior constraint (3 minutes, 24 seconds to 3 minutes, 45 seconds). The anterior cable reconstruction provides a static ligamentous support to help off-load the dynamic stress of the repaired rotator cuff tendon while at the same time reactivating the underlying capsule (3 minutes, 46 seconds to 3 minutes, 58 seconds).
The anterior cable of the rotator cuff is the primary ligamentous load-bearing structure deep to the supraspinatus tendon.1 With this in mind, the most anterior portion of the supraspinatus, involving 8 to 12 mm of the tendon immediately posterior to the bicipital groove, contains the rotator cable. Notably, the rotator cable is a ligamentous structure, to be distinguished from the anterior cord of the supraspinatus tendon; of the cable and cord structures, the cable attachment is more medial on the supraspinatus footprint. Tears involving this anterior cable portion of the supraspinatus have been demonstrated to lead to propagation of rotator cuff tendon tears through tendon strain of the infraspinatus.2 Equally important, tears involving the anterior cable of the supraspinatus have been shown to lead to greater translation of the humeral head in both a superior and posterior directions.1 That is to say, the dynamic tendinous portion of the supraspinatus is supported by the static ligamentous structure of the anterior cable.
Tears of the rotator cuff tendons can lead to both pain and dysfunction of the shoulder. Tears, with minimal retraction and tendon loss, can be repaired using transosseous-equivalent repair techniques to restore the anatomic footprint of the rotator cuff tendons.3, 4, 5, 6 In contrast, massive irreparable tears of the rotator cuff tendons, with significant retraction and fatty atrophy, can be addressed with superior capsular reconstruction.7,8 Also, tears of the rotator cuff tendons can occur that do not allow for anatomic footprint restoration yet are not large enough to require an superior capsular reconstruction technique; typically, these intermediate tears are addressed with a medialized repair or partial repair technique. In this setting, the partial repair of the rotator cuff tendon is required to serve as both a dynamic tendon and a static ligamentous support. As a result, partially repaired rotator cuff tendons can lead to a high retear rate.9
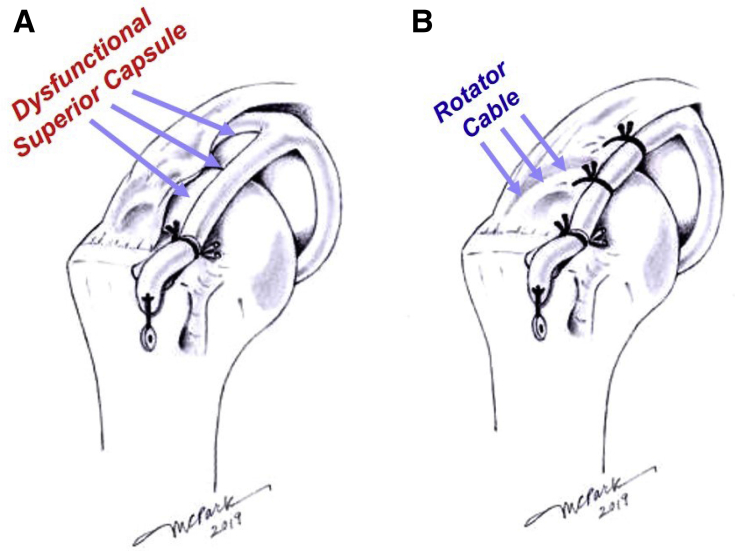
Support of a medialized repair or partial repair of the rotator cuff with a static ligamentous support may help reduce retear rates. Such a static ligamentous support would need to maintain a congruent glenohumeral joint while at the same time not restrict range of motion. One potential static support, as a nearby autologous graft donor, is the long head proximal biceps tendon. Often, the biceps tendon is tenotomized, as some belief the tendon to be a pain generator in the shoulder. Rather than disregarding this intra-articular structure, the biceps can be used as a graft for reconstruction of the anterior cable. As such, the tendon would be conserved at the anchor site of the superior labrum while using a free distal end, which is transected at the level of the bicipital groove transverse ligament; this autologous graft would span over the humeral head to be fixated of the footprint of the native superior capsule. The reconstructed anterior cable, using local proximal biceps tendon, can then be used via side-to-side sutures to purchase the partially repaired rotator cuff tendon and thereby reactivate its underlying capsule that was rendered dysfunctional before repair (Fig 1). This Technical Note describes an arthroscopic anterior cable reconstruction (ACR) using autologous proximal long head biceps tendon to restore posterosuperior capsule functionality.
Fig 1.
ACR schematic depicting capsular tissue (rotator cuff tendon and muscle subtracted). (A) Dysfunctional superior capsule depicting capsular redundancy (arrows). (B) Restoration of underlying capsule (arrows highlighting the rotator cable) using side-to-side sutures to repair the underlying posterosuperior capsule to the autologous biceps tendon ACR. (ACR, anterior cable reconstruction.)
Surgical Technique (With Video Illustration)
The key points of the technique are summarized in Table 1, and the technique is demonstrated in Video 1.
Table 1.
Surgical Steps, Pearls, and Pitfalls
| Surgical Step | Pearls | Pitfalls |
|---|---|---|
| Diagnostic arthroscopy | Biceps present with intact anchor | Biceps not present, or with pathology, consider use of allograft |
| Infraspinatus tendon repair | Partial or medialized repair performed with single-row triple-loaded anchor | Some type of repair is needed to be able to relink to the anterior cable |
| Greater tuberosity preparation | A trough is created, using a burr, on the greater tuberosity next to the repaired infraspinatus tendon. Within the trough, next to the articular cartilage, a double-loaded Corkscrew anchor is placed | Prevent creating too deep of a trough in the bone that compromises receiving an anchor |
| Graft securing to capsular footprint | Loop around fixation with sutures passed around biceps tendon, and not through the tendon itself. Arm positioned in 30° abduction and 30° external rotation when tensioning the graft. | Sutures passed through the biceps tendon graft have been found to cut through the graft. Not rotating the arm to 30° external rotation when tensioning the graft can lead to shortened length of the biceps and overconstraint of the glenohumeral joint |
| Native posteriorsuperior capsule repaired to biceps tendon | Loop around fixation links the biceps tendon to the repaired rotator cuff. #2 FiberWire is passed through the repaired tendon and wrapped around the biceps with arm in 30° abduction and 30° external rotation | Side-to-side repairs should be performed with the loop passed around the biceps and not through the biceps to avoid disrupting the integrity of the graft |
| Lateral anchor fixation of transferred biceps tendon | Lateral end of biceps at edge of greater tuberosity is released from remaining biceps. #2 FiberWire is passed through end of transected biceps and passed through 4.75-mm SwiveLock Anchor to be fixated into lateral edge of greater tuberosity | Securing the graft at the lateral edge helps prevent the graft from subluxation out of the trough and prevents the end of the graft from flipping over |
Patient Positioning, Setup, and Diagnostic Arthroscopy
General endotracheal anesthesia is used along with regional anesthesia. The patient is positioned in the lateral decubitus position. The extremity is prepped, draped, and then suspended in 30° abduction and 30° forward flexion with typically 10 pounds lateral traction applied to the arm. A standard posterior viewing portal is established into the glenohumeral joint. Diagnostic arthroscopy is typically performed using a 30° arthroscope. A standard anterior portal is established in the rotator interval for careful evaluation of the long head of the biceps. It is important to realize that this procedure can only be performed with an intact biceps anchor and sufficient integrity of the proximal biceps tendon. Attention is shifted to the subacromial space, through the posterior portal, where the repairability of the rotator cuff is assessed based on retraction, mobility, and tissue quality. Using needle localization, for optimal placement, an anterolateral working portal is established. Equally important, the infraspinatus must be repairable, and at minimum the posterior half, to link the underlying posterosuperior capsule to the reconstructed anterior cable, thus completing the ACR construct.
Repair of the Infraspinatus Tendon
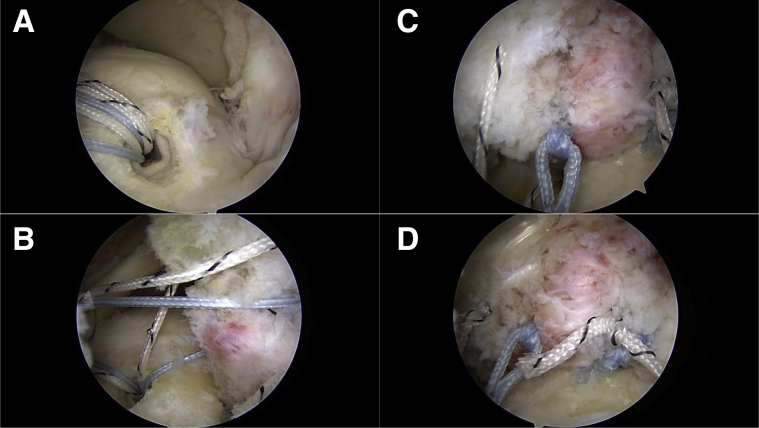
Based on the mobility and quality of the tendon, a partial repair or medialized repair can be performed on the infraspinatus tendon. Trial reduction, using tissue graspers, is assessed to determine placement of anchors and type of repair. The footprint of the greater tuberosity is prepared with use of electrocautery and a shaver or burr (Arthrex, Naples, FL). After preparation, a punch is used to create a pilot hole for placement of a single triple-loaded 5.5-mm Corkscrew anchor (Arthrex). A single row repair, using simple suture passes and knot tying, reduces the tendon of the infraspinatus down to the greater tuberosity footprint (Fig 2). Ultimately, the tear pattern dictates the type of repair construct of choice; the minimum requirement for the ACR is that the tendon repair restore a superior portion of the rotator cuff tendon.
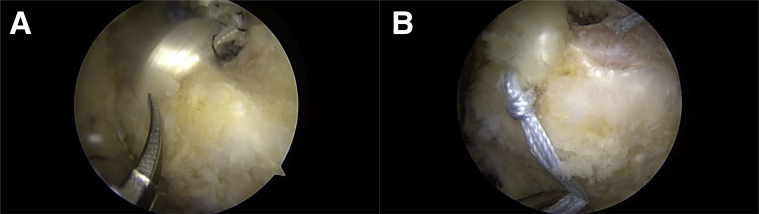
Fig 2.
Infraspinatus repair. Lateral decubitus position, posterior viewing portal. (A) Anchor placement, triple loaded. (B) Simple suture passage through the intraspinatus tendon. (C) Single-row repair with simple suture passes and knot tying. (D) Repaired infraspinatus tendon, dual-anchor single-row construct.
Greater Tuberosity Preparation for the Biceps Tendon
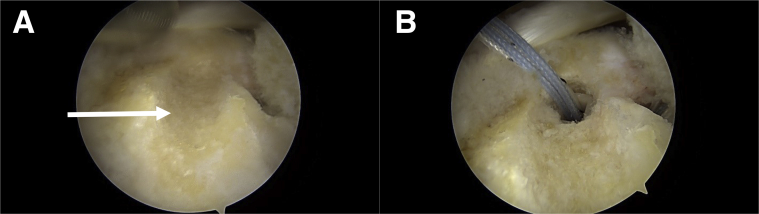
Next to the repaired infraspinatus tendon, a burr is used to create a trough on the greater tuberosity, approximating the width of the biceps tendon. At the same time, the trough increases surface area for healing and stability of the transferred biceps tendon. Adjacent to the articular cartilage, within the trough, a punch is used to create a pilot hole for receiving a single double-loaded 5.5-mm Corkscrew anchor (Arthrex; Fig 3).
Fig 3.
Greater tuberosity preparation. Lateral decubitus position, posterior viewing portal. (A) Trough created next to repaired infraspinatus tendon using a burr. (B) Double-loaded anchor placed adjacent to the articular margin.
Securing the Graft to the Capsular Footprint Site
Suture limbs from the anchor are placed on either side of the biceps tendon before knot-tying (and not through the tendon) to allow for sutures that loop-around the graft—therefore called “loop-around” fixation. We have found sutures passed through the tendon graft cut through the graft relatively easily with external rotation or adduction. Critical to note, before tying the “loop-around” sutures, the arm must be positioned at 30° abduction and 30° external rotation. This position of the arm allows optimal length of the biceps tendon graft so as to not overconstrain the glenohumeral joint (Fig 4).
Fig 4.
Optimal length of biceps tendon graft. On this axial view of a left shoulder, the external rotation (ER) arc of the humerus requires biceps length. Fixation of the biceps tendon graft with the arm positioned in relative external rotation allows the optimal length of the biceps tendon graft so as to not overconstrain the glenohumeral joint.
Repairing Native Posterosuperior Capsule (Deep to the Repair) to the Biceps Tendon
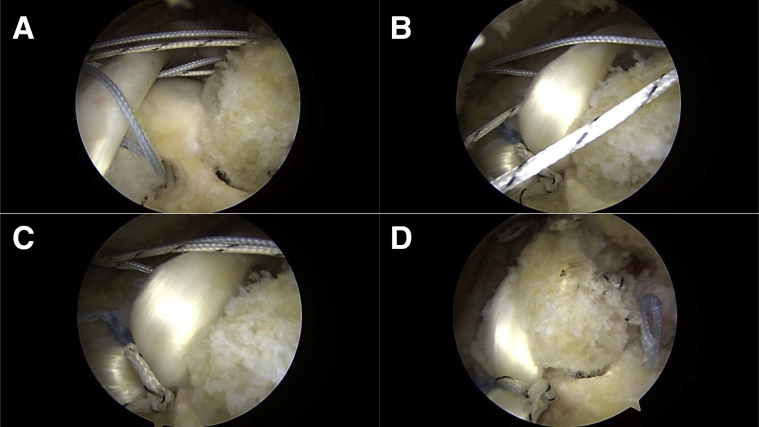
Loop-around fixation is again used to link the biceps tendon to the repaired rotator cuff (particularly, the posterosuperior capsule that is deep to the repaired tendon), by passing one limb of the paired sutures around the biceps tendon and the other matching limb through the repaired rotator cuff with its underlying superior capsule, in a side-to-side manner. This process is repeated by passing an additional independent #2 FiberWire (Arthrex) with emphasis placed on not piercing the biceps tendon with the suture. Once the arm is properly positioned (at 30° abduction and 30° external rotation), the suture limbs are sequentially tied to re-link the repaired underlying superior capsule to the static anterior cable support provided by the transferred and reconstructed biceps tendon. The native capsule, when restored to the cable graft, can now function against superiorly and posteriorly directed forces against the humeral head (compared with before tendon repair, with both the tendon and underlying capsule unable to provide superior stability against a high-riding humeral head) (Fig 5).
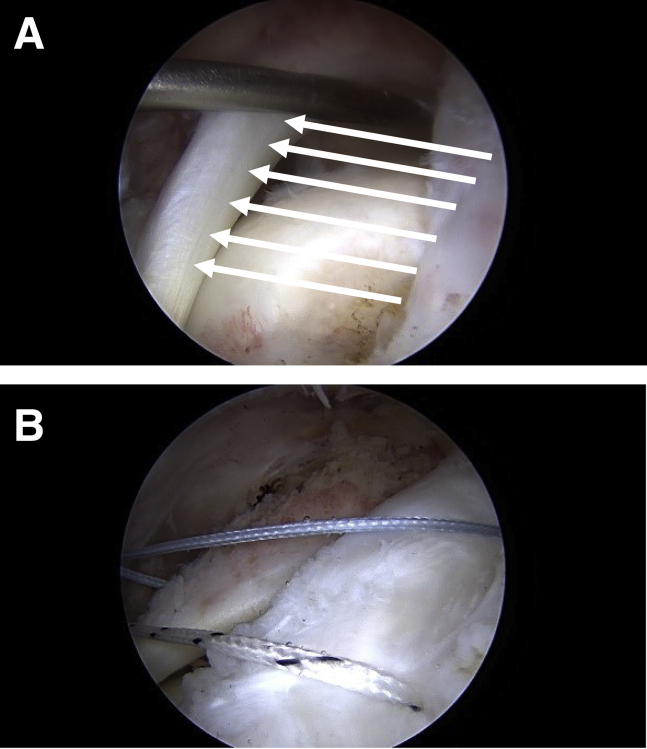
Fig 5.
Repairing the native posterosuperior capsule to biceps tendon. Lateral decubitus position, posterior viewing portal. (A) Loop-around fixation. Sutures are passed around the biceps tendon and not through the tendon. (B) Arm is rotated to 30° external rotation prior to knot-tying. (C) Sutures are tied down to re-link the tendon graft to the anchor. (D) Reactivation of repaired underlying superior capsule to the static anterior cable support.
Lateral Anchor Fixation of the Transferred Biceps Tendon for Graft-End Stability
Once the transferred biceps tendon is secured, the lateral end of the biceps, at the edge of the greater tuberosity footprint is released from the remaining biceps, after transverse ligament dissection, with use of arthroscopic scissors. A #2 FiberWire is passed through the end of the transferred biceps tendon with a luggage-tag locking type stitch and then passed through a knotless 4.75-mm SwiveLock Anchor (Arthrex). A pilot hole approximately placed 10 mm distal-lateral to the greater tuberosity footprint is created with a designated anchor punch. The anchor, with suture passed through the end of the transferred biceps tendon, is then seated to provide graft-end stability, primarily to secure the graft into its groove and preventing the end from uncontrolled displacement (Fig 6).
Fig 6.
Lateral anchor fixation. Lateral decubitus position, posterior viewing portal. (A) Lateral end of the biceps tendon, at the level of the bicipital transverse ligament, is transected with use of an arthroscopic scissor. (B) A #2 FiberWire is passed through the end of the biceps tendon using a luggage-tag configuration, then passed through a 4.75-mm SwiveLock anchor 10 mm distal-lateral to the greater tuberosity.
Postoperative Recovery and Rehabilitation
Postoperatively, the patient is placed in a sling and abduction brace to limit passive range of motion of the shoulder for the first 6 weeks. At 4 weeks, progressive passive- and active-assisted range of motion is initiated, in a graded manner. At 12 weeks, progressive strengthening of the rotator cuff and scapular stabilizers is started with the guidance of a physical therapist. Goals are to achieve functional active shoulder motion and strength with balanced biomechanics of the glenohumeral and scapulothoracic joints.
Discussion
In this technique, we demonstrate an arthroscopic anterior cable reconstruction, with use of autologous long head of the proximal biceps tendon, to provide static support to a repaired infraspinatus rotator cuff tendon (Fig 7). For these repairs of the infraspinatus without ACR, whether medialized or partially restored, the tendon is obligated to function as both a tendon and a ligament. Under those circumstances, ACR of the superior capsule can offer ligamentous support to enhance the functionality of the infraspinatus tendon repair. Together, the ACR and partially repaired infraspinatus tendon can provide improved function, by maintaining congruency of the glenohumeral joint, and can provide improved longevity, by the coupled construct of a static ligamentous support and a dynamic tendon.
Fig 7.
ACR acts as a suspension cable. (A) Defect in the anterior cable with capsule fallen away and dysfunctional (B) Restoration of posterosuperior capsule tension by relinking the repaired infraspinatus with the ACR biceps tendon graft. (ACR, anterior cable reconstruction.)
A few Technical Note have described use of the proximal biceps tendon to recapitulate a superior capsule reconstruction.10,11 In contradistinction, our technique is described as an anterior cable reconstruction by use of a cord-like graft to recreate an anterior cable, instead of use of the cord-like biceps tendon to recreate a superior capsule. Furthermore, our technique focuses on restoration of an anterior primary load-bearing structure, rather than spanning the humeral head, to provide a superior constraint. Superior constraint is provided by the individual native posterosuperior capsule, as it is reconstituted by way of side-to-side sutures secured around the graft.
Fundamental components of the ACR technique include graft linkage adjacent to a repaired cuff tendon, footprint preparation, arm positioning, and loop-around fixation. The technique begins with a repair performed on the infraspinatus tendon. As opposed to primary fixation of the biceps tendon before repairing the rotator cuff tendon, as described in other techniques using autologous biceps tendon graft,10,11 the current technique focuses first on repair of the rotator cuff tendon, then advancing the biceps tendon to the restored cuff tendon. By doing so, the ACR is performed at the anterior margin of the repaired rotator cuff, to restore the ligamentous support, without requiring the repaired cuff tendon to be over tensioned or brought into a forced position based on arbitrary graft placement. At the same time, the biceps tendon is brought adjacent to, and not underneath, the repaired rotator cuff tendon. In contrast to other techniques where the graft is placed below a repaired rotator cuff tendon to afford augmentation,12 our technique places the graft adjacent to the individual repaired tendon to create a functional anterior cable structure for linking, and thereby reactivating, inherent native underlying posterosuperior capsule that was dysfunctional without proper tension before repair (Fig 1). Based on biomechanical analyses, this reactivation helps to explain restoration of superior capsule function and kinematic normalization in superior, and anteroposterior directions.
Following repair of the rotator cuff tendon, footprint preparation for anterior cable reconstruction focuses on creation of a bone trough on the greater tuberosity. The trough approximates the width of the biceps tendon, increasing contact area of the transferred tendon graft to facilitate healing biology. Further, the recipient trough for the biceps tendon improves graft stability during rotational motions of the shoulder. This emphasis on footprint preparation is in contrast to other techniques, which perform a simple decortication of the greater tuberosity.10
The intra-articular portion of the long head of the biceps tendon has different lengths based on the position of the humeral head. Important to realize, the intra-articular length of the proximal biceps is shortest with the arm in abduction and internal rotation. When the arm, for example, is brought into adduction, the biceps is lengthened with further lengthening created by external rotation of the arm. To not over constrain the glenohumeral joint, the position of the arm must be considered when fixating the transferred biceps tendon. The optimal position of the arm, when securing the biceps tendon, was elucidated in a biomechanical study by Park et al.13 As demonstrated by Park et al.,13 with the arm in adduction the biceps graft was too lax to prevent superior migration, and with the arm in internal rotation the biceps graft was too restricted leading to graft failure. Given these points, the optimal position of the arm, when tensioning the transferred biceps tendon, is 30° abduction and 30° external rotation with respect to the body.13
Emphasis is placed on fixation of the biceps tendon so as to not disrupt the tubular structure of the graft. Whereas other techniques describe piercing through the biceps to fixate the tendon,10,11 our technique stresses loop-around fixation with sutures tied over, and not through, the biceps tendon. This form of fixation was formulated through the study by Park et al.,13 where the stiffness of the tubular graft was found to be disrupted by passing sutures through the tendon leading to early graft failure. Equally important, the transferred biceps tendon is secured to the repaired rotator cuff capsule, with loop-around fixation, to allow restoration of individual posterosuperior capsule functionality. Loop-around fixation allows adaptability of the biceps graft to find an equilibrium length and tension in relation to individual posterosuperior capsule.
Our described ACR technique using long head of the biceps tendon has several advantages. The technique uses an intra-articular autologous graft source, with less morbidity than an autologous tensor fascia lata graft,7 and with more histological consistency than a dermal allograft.14 At the same time, the autologous biceps tendon is still able to prevent superior migration of the humeral head as the aforementioned grafts without limiting range of motion.13 Additional therapeutic effects, by using the proximal biceps tendon, may be seen for those patients with symptoms due to biceps tendonitis or biceps subluxation. Use of a cord-like tendon graft like the biceps, in comparison with the use of a dermal allograft, can lend to a simplified technique that does not require handling a larger folded-over sheet-like graft, and shuttling from outside the shoulder with challenging suture management.
Further, using an autologous proximal biceps tendon that is already secured to the glenoid through the native anchor site obviates the need for anchor fixation and another interface for potential failure. Use of less implants along with not using an allograft may lend to a more cost-effective procedure. Although these advantages may be true, this technique is limited by the need of a proximal biceps tendon to be both present and functional. Another limitation of this technique is the need to have an infraspinatus or supraspinatus tendon that can be repaired in some fashion to provide a linkable structure to the biceps scaffold. Risks of this technique include potential pain from use of the long head of the biceps tendon or potential cosmetic deformity from tenotomy of the long head of the biceps tendon. Given these considerations, preoperative imaging with magnetic resonance imaging to evaluate for the presence of the proximal biceps tendon, along with the reparability of the rotator cuff tendons, is paramount to determine feasibility of the ACR technique.
We describe a surgical technique for anterior cable reconstruction using an autologous proximal biceps tendon for large rotator cuff defects that has been biomechanically validated.13 This ACR technique is aimed to address intermediate-to-large sized tears, where only a partial repair or medialized repair can be performed, and to restore the repaired dynamic tendon and reactivate the underlying capsule with a ligamentous static structure. Further clinical studies are warranted to investigate the functional and patient-reported outcomes of the ACR technique.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Coronal T2 magnetic resonance imaging of the shoulder shows a full-thickness tear involving the supraspinatus and infraspinatus tendons (12-19 seconds). Shoulder arthroscopy is performed in the lateral decubitus position; viewing from a posterior portal, diagnostic arthroscopy is performed. Evaluation of the biceps tendon demonstrates an intact biceps anchor without significant pathology involving the proximal aspect of the biceps tendon (13-32 seconds). A full-thickness tear involving the supraspinatus and infraspinatus tendon is confirmed and a single-row repair of the infraspinatus is performed using a single tripled-loaded suture 5.5-mm Corkscrew anchor (33-45 seconds). After repair of the infraspinatus tendon, residual dysfunction of the superior capsule is seen. To provide further ligamentous support to the repaired tendon, a reconstruction of the anterior cable is performed using the nearby biceps tendon (46-57 seconds). Reconstruction begins with creation of a trough adjacent to the repaired tendon using a 5.0-mm diameter burr. Within the trough, adjacent to the articular cartilage, a double loaded 5.5-mm diameter Corkscrew anchor is placed (58 seconds to 1 minute, 12 seconds). Loop-around fixation is performed by passing the sutures around the biceps tendon, as opposed to through the tendon, to not disrupt the integrity of the graft (1 minute, 15 seconds to 1 minute, 20 seconds). Next, 2 separate #2 FiberWires are passed separately through the repaired tendon edge and the other limb is again passed around the biceps tendon and not through the tendon (1 minute, 21 seconds to 1 minute, 30 seconds). Before securing the graft in position, the arm is rotated to 30° of external rotation to obtain optimal length of the biceps tendon so as not to overconstrain the glenohumeral joint. With the arm in position, starting at the suture anchor, the suture limbs are tied to stabilize the biceps tendon in the trough (1 minute, 31 seconds to 1 minute, 55 seconds). The biceps tendon graft is then linked to the repaired rotator cuff tendon with separate side to side ties of the suture limbs. Again, importance is emphasized in maintaining the arm positioned in 30° of external rotation while the reconstructed anterior cable is coupled to the repaired tendon. Once the biceps tendon and rotator cuff are joined, rotation of the arm is checked to ensure no constrains in motion are observed (1 minute, 56 seconds to 2 minutes, 50 seconds). At the edge of the greater tuberosity, the graft is released from the remaining biceps with use of arthroscopic scissors and ablation probe. A #2 FiberWire is passed through the transected lateral edge of the biceps graft and then secured over the lateral edge of the greater tuberosity with a 4.75-mm SwiveLock anchor. This lateral anchor fixation provides graft end stability (2 minutes, 52 seconds to 3 minutes, 22 seconds). The coupled construct of a static ligamentous support and a dynamic tendon allows unrestricted rotational motion while at the same time providing superior constraint (3 minutes, 24 seconds to 3 minutes, 45 seconds). The anterior cable reconstruction provides a static ligamentous support to help off-load the dynamic stress of the repaired rotator cuff tendon while at the same time reactivating the underlying capsule (3 minutes, 46 seconds to 3 minutes, 58 seconds).
References
- 1.Mesiha M.M., Derwin K.A., Sibole S.C., Erdemire A., McCarron J.A. The biomechanical relevance of anterior rotator cuff cable tears in a cadaveric shoulder model. J Bone Joint Surg Am. 2013;95:1817–1824. doi: 10.2106/JBJS.L.00784. [DOI] [PubMed] [Google Scholar]
- 2.Andarawis-Puri N., Ricchetti E.T., Soslowsky L.J. Interaction between the supraspinatus and infraspinatus tendons: Effect of anterior supraspinatus tendon full-thickness tears on infraspinatus tendon strain. Am J Sports Med. 2009;37:1831–1839. doi: 10.1177/0363546509334222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park M.C., ElAtrrache N.S., Ahmad C.S., Tibone J.E. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy. 2006;22:1360.e1–1360.e5. doi: 10.1016/j.arthro.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 4.Park M.C., Tibone J.E., ElAttrache N.S., Ahmad C.S., Jun B.J., Lee T.Q. Part II. Biomechanical assessment for a footprint restoring arthroscopic transosseous-equivalent rotator cuff repair technique compared to a double-row technique. J Shoulder Elbow Surg. 2007;16:469–476. doi: 10.1016/j.jse.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Park M.C., ElAttrache N.S., Tibone J.E., Ahmad C.S., Jun B.J., Lee T.Q. Part I. Footprint contact characteristics for an arthroscopic transosseous-equivalent rotator cuff repair technique. J Shoulder Elbow Surg. 2007;16:461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Park M.C., Pirolo J.M., Park C.J., McGarry M.H., Tibone J.E., Lee T.Q. The effect of abduction and rotation on footprint contact for single-row, double-row, and transosseous-equivalent rotator cuff repair techniques. Am J Sports Med. 2009;37:1599–1608. doi: 10.1177/0363546509332506. [DOI] [PubMed] [Google Scholar]
- 7.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 8.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 9.Yoo J.C., Ahn J.H., Koh K.H., Lim K.S. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy. 2009;25:1093–1100. doi: 10.1016/j.arthro.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Kim Y.S., Lee H.J., Park I., Sung G.Y., Kim D.J., Kim J.H. Arthroscopic in situ modified superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boutsiadis A., Chen S., Jiang C., Lenoir H., Delsol P., Barth J. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: “The Chinese way. Arthrosc Tech. 2017;6:e1559–e1566. doi: 10.1016/j.eats.2017.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cabarcas B.C., Garcia G.H., Gowd A.K., Liu Jn, Romeo A.A. Arthroscopic superior capsular reconstruction and over-the-top rotator cuff repair incorporation for treatment of massive rotator cuff tears. Arthrosc Tech. 2018;7:e829–e837. doi: 10.1016/j.eats.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park M.C., Itami Y., Lin C.C. Anterior cable reconstruction using the proximal biceps tendon for large rotator cuff defects limits superior migration and subacromial contact without inhibiting range of motion: A biomechanical analysis. Arthroscopy. 2018;34:2590–2600. doi: 10.1016/j.arthro.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 14.Burkhart S.S., Denard P.J., Adams C.R., Brady P.C., Hartzler R.U. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. doi: 10.1016/j.eats.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronal T2 magnetic resonance imaging of the shoulder shows a full-thickness tear involving the supraspinatus and infraspinatus tendons (12-19 seconds). Shoulder arthroscopy is performed in the lateral decubitus position; viewing from a posterior portal, diagnostic arthroscopy is performed. Evaluation of the biceps tendon demonstrates an intact biceps anchor without significant pathology involving the proximal aspect of the biceps tendon (13-32 seconds). A full-thickness tear involving the supraspinatus and infraspinatus tendon is confirmed and a single-row repair of the infraspinatus is performed using a single tripled-loaded suture 5.5-mm Corkscrew anchor (33-45 seconds). After repair of the infraspinatus tendon, residual dysfunction of the superior capsule is seen. To provide further ligamentous support to the repaired tendon, a reconstruction of the anterior cable is performed using the nearby biceps tendon (46-57 seconds). Reconstruction begins with creation of a trough adjacent to the repaired tendon using a 5.0-mm diameter burr. Within the trough, adjacent to the articular cartilage, a double loaded 5.5-mm diameter Corkscrew anchor is placed (58 seconds to 1 minute, 12 seconds). Loop-around fixation is performed by passing the sutures around the biceps tendon, as opposed to through the tendon, to not disrupt the integrity of the graft (1 minute, 15 seconds to 1 minute, 20 seconds). Next, 2 separate #2 FiberWires are passed separately through the repaired tendon edge and the other limb is again passed around the biceps tendon and not through the tendon (1 minute, 21 seconds to 1 minute, 30 seconds). Before securing the graft in position, the arm is rotated to 30° of external rotation to obtain optimal length of the biceps tendon so as not to overconstrain the glenohumeral joint. With the arm in position, starting at the suture anchor, the suture limbs are tied to stabilize the biceps tendon in the trough (1 minute, 31 seconds to 1 minute, 55 seconds). The biceps tendon graft is then linked to the repaired rotator cuff tendon with separate side to side ties of the suture limbs. Again, importance is emphasized in maintaining the arm positioned in 30° of external rotation while the reconstructed anterior cable is coupled to the repaired tendon. Once the biceps tendon and rotator cuff are joined, rotation of the arm is checked to ensure no constrains in motion are observed (1 minute, 56 seconds to 2 minutes, 50 seconds). At the edge of the greater tuberosity, the graft is released from the remaining biceps with use of arthroscopic scissors and ablation probe. A #2 FiberWire is passed through the transected lateral edge of the biceps graft and then secured over the lateral edge of the greater tuberosity with a 4.75-mm SwiveLock anchor. This lateral anchor fixation provides graft end stability (2 minutes, 52 seconds to 3 minutes, 22 seconds). The coupled construct of a static ligamentous support and a dynamic tendon allows unrestricted rotational motion while at the same time providing superior constraint (3 minutes, 24 seconds to 3 minutes, 45 seconds). The anterior cable reconstruction provides a static ligamentous support to help off-load the dynamic stress of the repaired rotator cuff tendon while at the same time reactivating the underlying capsule (3 minutes, 46 seconds to 3 minutes, 58 seconds).
Coronal T2 magnetic resonance imaging of the shoulder shows a full-thickness tear involving the supraspinatus and infraspinatus tendons (12-19 seconds). Shoulder arthroscopy is performed in the lateral decubitus position; viewing from a posterior portal, diagnostic arthroscopy is performed. Evaluation of the biceps tendon demonstrates an intact biceps anchor without significant pathology involving the proximal aspect of the biceps tendon (13-32 seconds). A full-thickness tear involving the supraspinatus and infraspinatus tendon is confirmed and a single-row repair of the infraspinatus is performed using a single tripled-loaded suture 5.5-mm Corkscrew anchor (33-45 seconds). After repair of the infraspinatus tendon, residual dysfunction of the superior capsule is seen. To provide further ligamentous support to the repaired tendon, a reconstruction of the anterior cable is performed using the nearby biceps tendon (46-57 seconds). Reconstruction begins with creation of a trough adjacent to the repaired tendon using a 5.0-mm diameter burr. Within the trough, adjacent to the articular cartilage, a double loaded 5.5-mm diameter Corkscrew anchor is placed (58 seconds to 1 minute, 12 seconds). Loop-around fixation is performed by passing the sutures around the biceps tendon, as opposed to through the tendon, to not disrupt the integrity of the graft (1 minute, 15 seconds to 1 minute, 20 seconds). Next, 2 separate #2 FiberWires are passed separately through the repaired tendon edge and the other limb is again passed around the biceps tendon and not through the tendon (1 minute, 21 seconds to 1 minute, 30 seconds). Before securing the graft in position, the arm is rotated to 30° of external rotation to obtain optimal length of the biceps tendon so as not to overconstrain the glenohumeral joint. With the arm in position, starting at the suture anchor, the suture limbs are tied to stabilize the biceps tendon in the trough (1 minute, 31 seconds to 1 minute, 55 seconds). The biceps tendon graft is then linked to the repaired rotator cuff tendon with separate side to side ties of the suture limbs. Again, importance is emphasized in maintaining the arm positioned in 30° of external rotation while the reconstructed anterior cable is coupled to the repaired tendon. Once the biceps tendon and rotator cuff are joined, rotation of the arm is checked to ensure no constrains in motion are observed (1 minute, 56 seconds to 2 minutes, 50 seconds). At the edge of the greater tuberosity, the graft is released from the remaining biceps with use of arthroscopic scissors and ablation probe. A #2 FiberWire is passed through the transected lateral edge of the biceps graft and then secured over the lateral edge of the greater tuberosity with a 4.75-mm SwiveLock anchor. This lateral anchor fixation provides graft end stability (2 minutes, 52 seconds to 3 minutes, 22 seconds). The coupled construct of a static ligamentous support and a dynamic tendon allows unrestricted rotational motion while at the same time providing superior constraint (3 minutes, 24 seconds to 3 minutes, 45 seconds). The anterior cable reconstruction provides a static ligamentous support to help off-load the dynamic stress of the repaired rotator cuff tendon while at the same time reactivating the underlying capsule (3 minutes, 46 seconds to 3 minutes, 58 seconds).