Abstract
Anterior cruciate ligament reconstruction (ACLR) with additional procedures could be necessary for patients with increased preoperative pivot shift. Double-bundle (DB) ACLR provides more footprint coverage and recreates the 2 functional anteromedial (AM) and posterolateral (PL) bundles, which are believed to give better joint function and stability than single-bundle (SB) ACLR. Internal brace augmentation with suture tape is proposed along with tendon graft in ACLR to protect the newly reconstructed ligament during rehabilitation. Additional reconstruction with anterolateral ligament (ALL) during ACLR has shown significant reduction in the level of persistent pivot shift. In Technical Note we present a modified surgical technique of combined anatomic DB ACLR and ALLR with hamstring autograft and internal brace, using button suspensory fixation device and aperture screws. The objective of this technique is to decrease residual anterior and rotational instability after ACLR and ALLR.
Technique Video
The whole procedure of the surgery is as follows. A male professional kickboxer injured his right knee during competition. MRI revealed complete torn ACL. One month after the accident, he had very unstable knee and can't go back his game due to giving way sensation. High grade pivot was observed after anesthesia. We put him in supine position with a leg holder and then made all the bony landmarks, including lateral femoral epicondyle, Gerdy's tubercle, which led us to find out the origin and insertion of anterior lateral ligament, ALL. Normally, it is located 2 centimeters below the joint line. We used autogolus hamstring tendon graft, a closed looped endobutton and a Swivelock anchor to fix the graft. The semitendinosus tendon was looped three times, with one side linked with endobutton and the other side fixed with multiple Krakow sutures. The average length of the triple semitendinosus tendon was around 8.5 to 9cm and the diameter was around 7-8 mm in the femoral side, and 8-9 mm in the tibial side. The gracilis tendon was sutured at both ends, and the Fibertape from the Swivelock anchor was used as an internal brace to go along with gracilis tendon, which worked intra-articularlly as the PL bundle of ACL, and extra-articularlly as the ALL reconstruction. The average length of the gracilis tendon and Fibertape was always more than 15cm, which is long enough to make a loop starting from medial knee, intra-articularlly, out from lateral knee and then fixed at the medial knee again. The average diameter was less than 5mm, which allowed us to drill a femoral PL tunnel and an ALL-tibial tunnel with a 5mm rigid reamer. We debrided the torn ACL until clear visualization of the whole anatomy. A flexible pin was inserted in the center of the footprint of the AM bundle. Then a flexible reamer was then used to create the femoral AM tunnel according to the diameter of prepared tendon graft. We must make sure the posterior wall was preserved. One No.5 Ethibond suture would be passed within femoral AM tunnel for further tendon shuttling. Then the scope would be shifted into anteromedial portal. The ACL guide now was inserted through anterolateral portal, with its tip aiming at the center of the PL bundle footprint intra-articullarly, and the sheath outside the knee, aiming at the ALL-femoral origin. One rigid guide pin was then inserted with an outside-in manor, exiting intra-articularly at the center of PL bundle. A 5mm rigid reamer would be used to create femoral PL tunnel. Then, the tibial ACL tunnel would be made 1mm larger than the diameter of the tibial side of the prepared semitendinosus tendon. For example, if the tibial side of prepared semitendinosus tendon is 8mm, we used a 9mm reamer to create the tibial ACL tunnel. Another No. 5 Ethibond suture will then be passed through tibial ACL tunnel intra-articularly and pulled out extra-articularly by the grasper put in the femoral PL tunnel in advanced. We used this suture to tie the gracilis tendon and Fibertape, shuttling intraarticularly through the tibial ACL tunnel, and pulled out from femoral PL tunnel until they exited the skin of lateral thigh. The length outside the lateral femoral cortex should be long enough to create extraarticular ALL, which could be determined by the length of the gracilis incorporated inside the tibial ACL tunnel. In general, the single gracilis is long enough to occupy the full length of the tibial ACL tunnel and at least 25mm long, inside the tibia ALL tunnel. Thereafter, the AM bundle suture was tied with both limbs of endobutton, shuttling semitendinosus tendon proximally, until the button was flipped and fixed on the femoral cortical surface. A 6 x 25 mm interference screws would be used to fix the PLB by an outside-in manner. The tibial drill guide was set at 55°, with its tip aimed about 2 cm below ACL tibial tunnel, avoiding undesirable tunnel connection. The cannulated sleeve of the guide was placed posteriorly and proximally to the Gerdy's tubercle, where a stamp incision was made. Then, a pin is drilled from lateral to the medial side of the tibia and a consecutive 5 mm tunnel was created by a rigid reamer. A No.5 Ethibond suture was then shuttled from lateral to the medial tibia, facilitating further graft passage. Then another interference screw one millimeter larger than the size of the drilled tibial ACL tunnel, was used to fix the tibial end in the tibial ACL tunnel for both grafts and FiberTape at 60° of knee flexion. At last, the single gracilis and FiberTape were shuttled from the lateral end of the femoral PL tunnel, underneath the iliotibial band, to the lateral end of the tibial ALL tunnel as the ALLR. They were then shuttled through the tibial ALL tunnel from lateral to medial side of the tibia, making sure both gracilis and FiberTape were inside ALL tibial tunnel. The both limbs of No.2 Ethibond sutures of the gracillis and FiberTape were tied together at 20° of knee flexion and neutral knee rotation. Augmentation fixation was done by fixing as many sutures intraosseous by a 4.75 mm Swivelock anchor. The final construct is shown like the cartoon picture. Finally, we will check if there were any impingement during ROM. Luckily, no pivot was observed after the surgery in all our patients.
Double-bundle (DB) anterior cruciate ligament reconstruction (ACLR) gives better joint function and stability than single-bundle (SB) ACLR biomechanically.1 Suture tape augmentation has been proposed to protect the newly reconstructed ligament during rehabilitation.2 The anterolateral ligament (ALL) has been reported to have a synergistic function with ACL toward the stability of knee rotation.3, 4, 5
In this Technical Note we present a modified surgical technique of combined anatomic DB ACLR and ALLR with hamstring autograft and internal brace, using button suspensory fixation device and aperture screws. The objective of this technique is to decrease the residual anterior and rotational instability after ACLR and ALLR.
Technique
Surgical Indications
The indications for anatomic DB ACLR and ALLR with hamstring autograft and internal brace are shown in Table 1.
Table 1.
Indications
|
|
|
|
|
Patient Preparation and Bony Landmarks
The patient is positioned supine with a leg holder. Bony landmarks are marked as follows: lateral and medial joint lines, lateral femoral epicondyle, tibial tuberosity, fibular head, Gerdy's tubercle, and anterolateral ligament footprint (Fig 1).
Fig 1.
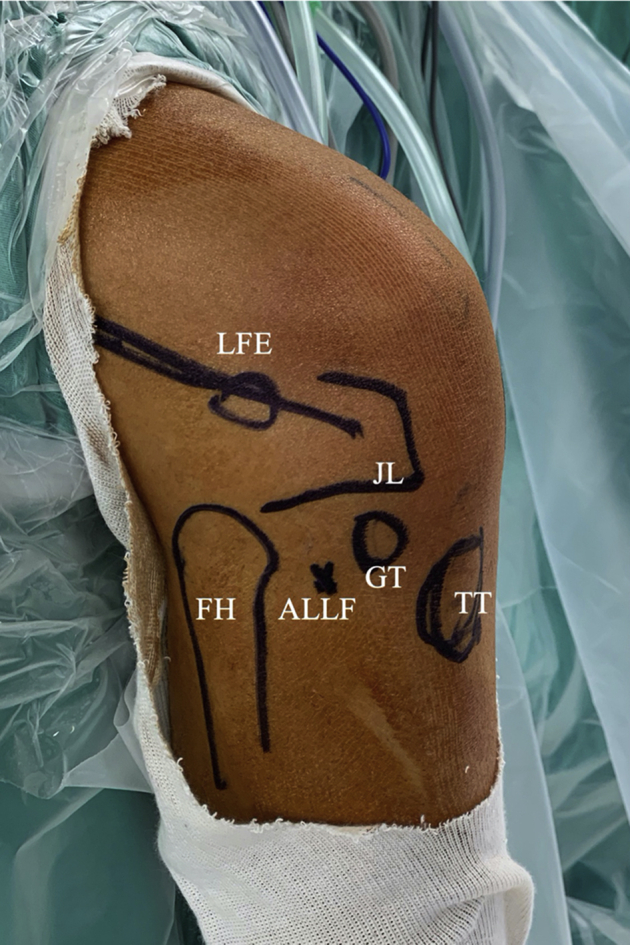
Bony landmarks of DB ACLR and ALLR for right knee in a leg holder. ACLR, anterior cruciate ligament reconstruction; ALLF, anterolateral ligament footprint; ALLR, anterolateral ligament reconstruction; DB, double-bundle; FH, fibular head; GT, Gerdy’s tubercle; JL, joint line; LFE, lateral femoral epicondyle; TT, tibial tuberosity.
Surgical Technique
Graft Harvesting
The semitendinosus and gracilis autografts are harvested with full length from the insertion site with a tendon stripper.
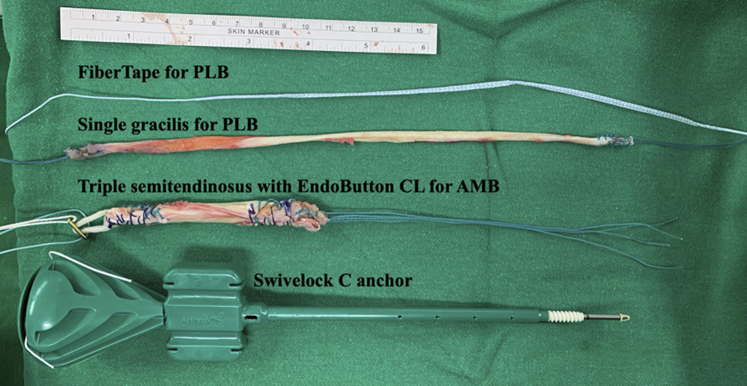
Graft Preparation: AM Bundle
The semitendinosus is prepared in a triple-folded fashion, with tibial ends sutured with no. 2 Ethibond (Ethicon, Somerville, NJ). A 15-mm EndoButton CL (Smith & Nephew Endoscopy, Andover, MA) is attached at the femoral side for AMB fixation. The diameter of the graft is 7 to 9 mm, and the length of the graft is ∼850 to 900 mm according to the tendon quality harvested (Fig 2).
Fig 2.
Graft preparation and instruments needed for fixation. The semitendinosus is prepared in a triple-folded fashion, with tibial end sutured with no. 2 Ethibond. A 15-mm EndoButton CL is attached at the femoral side for AMB fixation. The gracilis is whipstitched with no. 2 Ethibond at both ends without folding. The FiberTape is taken from one 4.75 × 19.1-mm Biocomposite Swivelock C anchor. AMB, anteromedial bundle; PLB, posterolateral bundle.
Graft Preparation: PL Bundle and ALL Graft
The gracilis is whipstitched with no. 2 Ethibond sutures at both ends without folding. The FiberTape (Arthrex, Naples, FL) is taken from one 4.75 × 19.1-mm Biocomposite Swivelock C anchor (Swivelock C; Arthrex). It is shuttled together with gracilis tendon as an internal brace for PLB and ALL (Fig 2).
Femoral and Tibial Tunnel Preparation: Femoral AM Tunnel
The ACL remnant is kept, and the centers of AMB and PLB are marked with a microfracture awl inserted from the anteromedial portal (AMP) under direct vision using a 30° arthroscope from the anterolateral portal (ALP). A Clancy curved drill guide (Smith & Nephew) is introduced through the AMP, ensuring its tip rests in the middle of the AMB femoral footprint (Fig 3A). A flexible passing pin is then inserted through the curved drill guide and advanced through the femoral condyle until it exits the distal thigh. Sounding of the lateral femoral outer cortex is performed to obtain the total osseous length. The curved drill guide is then removed, and a Clancy flexible reamer is inserted over the passing pin (Fig 3B) and advanced to the determined depth. A no. 5 Ethibond suture is placed through the slot of the flexible guide pin and pulled into the knee through the AMP and then pulled out from the proximal femoral cortex (AMB suture) (Fig 3C). The other side of the suture is retrieved retrogradely through the tibial tunnel once it is made.
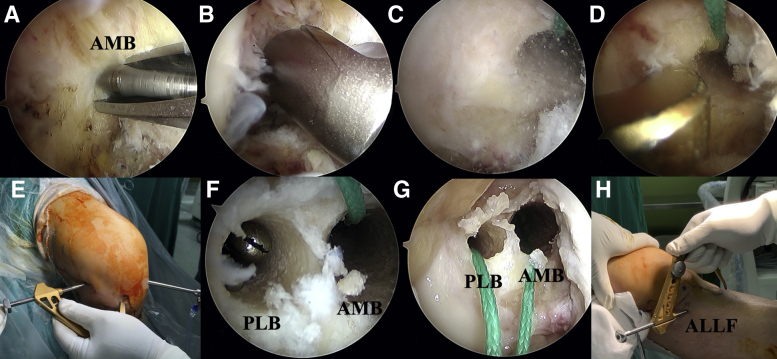
Fig 3.
Femoral and tibial tunnel preparation. (A) Viewing from anterolateral portal (ALP) of right knee, a Clancy curved drill guide is introduced through the anteromedial portal (AMP). A flexible passing pin is aimed at the middle of the AMB femoral footprint and advanced through the femoral condyle until it exits the distal thigh. (B) A Clancy flexible reamer is inserted over the passing pin and advanced to the determined depth. (C) A no. 5 Ethibond suture is shuttled through the AMP and pulled out from proximal femoral cortex. (D and E) Viewing from AMP, a outside-in ACL drill guide is introduced from the ALP with the tip placed at the center of the PLB femoral footprint. The drill sleeve is placed just proximally and posteriorly to the lateral femoral epicondyle. (F) A 5-mm-wide femoral tunnel is created by a rigid reamer in an outside-in manner. A suture grasper is put in the femoral PL tunnel for further suture passing. (G) After tibial ACL tunnel is made, one no. 5 Ethibond suture is shuttled through tibial ACL tunnel and taken out from femoral PL tunnel by the grasper that was placed in advanced. This suture is used to shuttle the PLB graft (single gracilis) and FiberTape as an internal brace. (H) The tibial drill guide is set at 55°, and its tip is aimed ∼2 cm below ACL tibial tunnel, avoiding undesirable tunnel connection. The cannulated sleeve of the guide is placed posteriorly and proximally to the Gerdy’s tubercle (ALL tibial footprint, ALLF). A 5-mm tunnel is created from lateral to medial and forms the ALL tibial tunnel. AMB, anteromedial bundle; PLB, posterolateral bundle.
Femoral and Tibial Tunnel Preparation: Femoral PL Tunnel
After the femoral AM tunnel is made by the flexible reamer, the scope is then shifted into the AM portal. The outside-in ACL drill guide (Smith & Nephew) is introduced from the AL portal with the tip placed at the site of the PLB femoral footprint (Fig 3D, E). Outside the joint, the accompanying drill sleeve is placed just proximally and posteriorly to the lateral femoral epicondyle. After guide pin placement, a 5-mm-wide femoral tunnel is created by a rigid reamer in an outside-in manner. This technique guarantees the femoral AM and PL tunnels to be positioned divergent to each other and prevents tunnel connection. A suture grasper is put in the femoral PL tunnel for further suture passing (Fig 3F).
Femoral and Tibial Tunnel Preparation: Tibia ACL Tunnel
The ACL tibial drill guide is placed in AMP (viewed from ALP) and positioned in the center of the ACL tibial insertion. A tibial tunnel 1 mm larger than the diameter of AMB graft (triple semitendinosus) is made. Then, one no. 5 Ethibond suture is passed from the tibial ACL tunnel into the joint and taken out from the femoral PL tunnel. This suture is used to shuttle the PLB graft (single gracilis) and FiberTape as an internal brace (Fig 3G).
Femoral and Tibial Tunnel Preparation: Tibial ALL Tunnel
The tibial drill guide is set at 55°, and its tip is aimed ∼2 cm below ACL tibial tunnel, avoiding undesirable tunnel connection. The cannulated sleeve of the guide is placed posteriorly and proximally to the Gerdy's tubercle, where a stamp incision is made (Fig 3H). Then, a pin is drilled from lateral to the medial side of the tibia and a consecutive 5-mm tunnel is created by a rigid reamer. A no. 5 Ethibond suture is then shuttled from lateral to the medial tibia, facilitating further graft passage (tibial ALL tunnel).
Graft Shuttling and Fixation
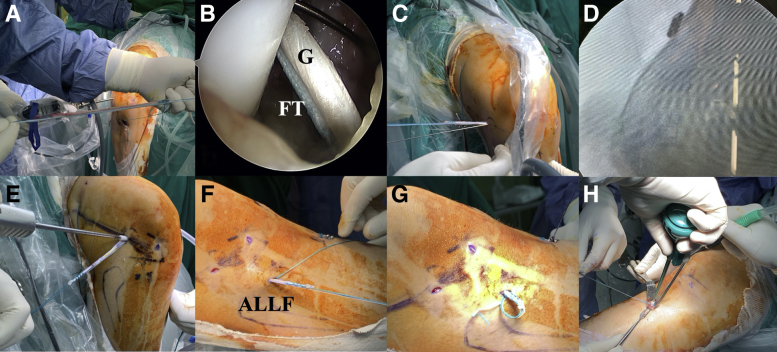
After all tunnels were prepared, there is one no. 5 Ethibond suture from tibial ACL tunnel to femoral AM tunnel (AMB suture) and another suture passed from the tibial ACL tunnel to the femoral PL tunnel (PLB suture) (Fig 3G). The third no. 5 Ethibond suture is placed from lateral tibia ALL footprint to the medial side of the tibia (tibial ALL suture). First, the single gracilis and FiberTape are tied together with the PLB suture (Fig 4A), shuttled intraarticularly through the tibial ACL tunnel, and pulled out from femoral PL tunnel until they exit the skin of lateral thigh (Fig 4B, C). The length outside the lateral femoral cortex should be enough to create extraarticular ALL, which is determined by the length of gracilis incorporated inside the tibial ACL tunnel. In general, the single gracilis is long enough to occupy the full length of the tibial ACL tunnel and ≥25 mm long inside the tibia ALL tunnel.
Fig 4.
Graft shuttling and fixation of right knee. (A, B, and C) The single gracilis (G) and FiberTape (FT) are tied together with the PLB suture and shuttled intraarticularly through tibial ACL tunnel. They are pulled out from femoral PL tunnel until they exit the skin of lateral thigh. The length outside the lateral femoral cortex should be enough to create extraarticular ALL. (D) The AM bundle graft is an EndoButton on the femoral cortex. (E) A 6 × 25-mm hydroxyapatite interference screw is used to fix the PLB in an outside-in manner. (F) The single G and FT are shuttled from the lateral end of the femoral PL tunnel, underneath the iliotibial band, to the lateral end of the tibial ALL tunnel (ALLF). (G) G and FT are shuttled through the tibial ALL tunnel from lateral to medial side of the tibia, making sure both G and FT are inside ALL tibial tunnel. (H) Augmentation fixation is done by fixing as many sutures as possible intraosseously by a 4.75-mm Swivelock anchor. ALLF, anterolateral ligament footprint.
Thereafter, the AM bundle suture is tied with both limbs of EndoButton (Smith & Nephew Endoscopy) and shuttled proximally until the button is flipped and fixed on the femoral cortical surface (Fig 4D). A 6 × 25-mm hydroxyapatite interference screw (BioRCI-HA screws; Smith & Nephew) is used to fix the PLB in an outside-in manner (Fig 4E). Then another hydroxyapatite interference screw 1 mm larger than the drilled tibial ACL tunnel is used to fix the tibial end in the tibial ACL tunnel of both grafts and FiberTape at 60° knee flexion.
Last, the single gracilis and FiberTape are shuttled from the lateral end of the femoral PL tunnel, underneath the iliotibial band, to the lateral end of the tibial ALL tunnel as the ALLR (Fig 4F). They are then shuttled through the tibial ALL tunnel from lateral to medial side of the tibia, making sure both gracilis and FiberTape are inside ALL tibial tunnel (Fig 4G). Then both limbs of no. 2 Ethibond sutures of the gracilis and FiberTape are tied together at 20° knee flexion and neutral knee rotation. Augmentation fixation is done by fixing as many sutures as possible intraosseously by a 4.75-mm Swivelock anchor (Fig 4H).
The final construct is shown in Fig 5. The whole procedure of the surgery is shown in the Video 1. The pearls and pitfalls of the surgical steps are shown in Table 2. The advantages, risks, and limitations of this technique are shown in Table 3.
Fig 5.
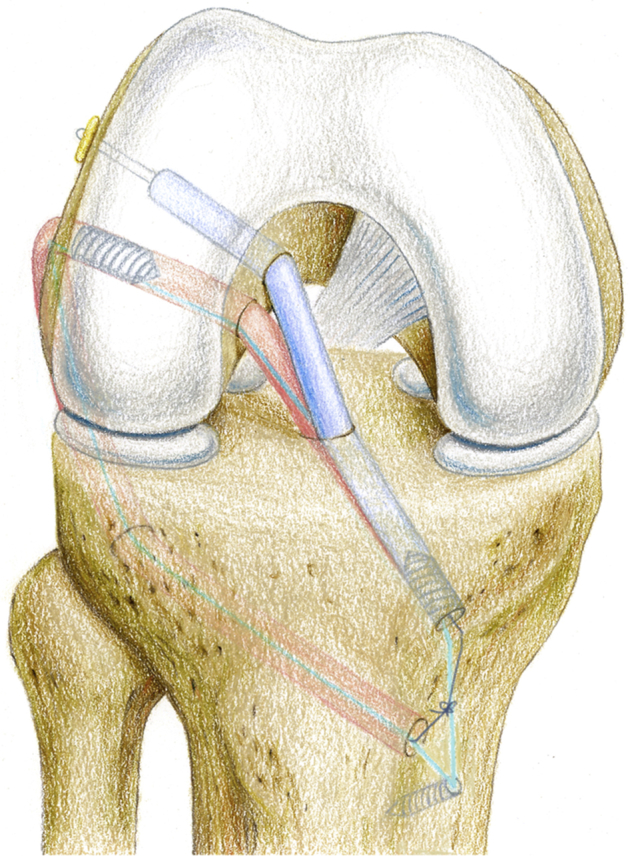
The final anatomic double-bundle ACL reconstruction with extra-articular anterolateral ligament reconstruction and internal brace of right knee. Blue, anteromedial bundle of ACL; red, posterolateral bundle of ACL; light blue, FiberTape.
Table 2.
Surgical Steps, Tips, Pearls, and Pitfalls
| Surgical Step | Tips and Pearls | Pitfalls |
|---|---|---|
| Bony landmarks | Mark lateral and medial joint lines, lateral femoral epicondyle, tibial tuberosity, fibular head, and Gerdy's tubercle. | There may be difficulty in recognizing these landmarks in larger patients. |
| Graft harvesting | Semitendinosus and gracilis autograft are harvested with full length from the insertion site. |
|
|
||
| Graft preparation |
|
|
|
|
|
|
|
|
| Femoral AM tunnel preparation |
|
|
|
|
|
|
||
|
||
|
||
| Femoral PL tunnel preparation |
|
|
|
|
|
|
||
|
||
|
||
| Tibial ACL tunnel preparation |
|
Be sure not to damage the suture passed through the femoral AM tunnel, which will be used to shuttle the AMB graft into the femoral AM tunnel later, during tibial ACL tunnel drilling. |
|
||
|
||
|
||
| Tibial ALL tunnel preparation |
|
|
|
|
|
|
||
|
||
|
||
| Graft shuttling and fixation |
|
|
|
|
|
|
|
|
|
||
|
||
|
||
|
||
|
ACL, anterior cruciate ligament; ALL, anterolateral ligament; ALLR, anterolateral ligament reconstruction; AM, anteromedial; AMB, anteromedial bundle; IT, iliotibial; PL, posterolateral; PLB, posterolateral bundle.
Table 3.
Advantages, Risks, and Limitations
| Advantages |
|
|
|
|
|
| Risks |
|
|
|
|
| Limitations |
|
|
|
|
Postoperative Management
The postoperative rehabilitation protocols are summarized in Table 4.
Table 4.
Postoperative Management
| Activity | Timing Postoperatively |
|---|---|
| Jogging | 3 months |
| Sprinting and competitive exercises | 6 months |
| Return to full sports activities | 9 months |
| Patients without meniscus repair | |
| No brace needed | |
| Continuous passive motion | Immediately after surgery |
| Walking with crutches | First 2 weeks |
| Full weightbearing | After 2 weeks |
| Patients with meniscus repair | |
| ROM brace | First 6 weeks |
| 0° to 60° | First 4 weeks |
| Full range of motion | After 4 weeks |
| Partial weightbearing with crutches | First 4 weeks |
Discussion
There are 11% to 30% recurrent and persistent instabilities reported after ACLR.6,7 Anatomic ACLR with additional procedures is probably necessary for patients with increased preoperative rotational instability.8,9
DB ACLR has been proven to provide improved knee rotational stability.10 Suture tape augmentation has been proposed to be used along with allograft or autograft ACLR11,12 with lower failure rates than the conventional ones.13,14 The objective of suture tape augmentation is to protect the newly reconstructed ligament during rehabilitation.2
Inderhaug et al.15 showed that intra-articular ACLR alone would not reestablish normal kinematics after combined ACL and anterolateral injury. A 2018 survey found that 38% of respondents used some type of adjunctive anterolateral reconstruction for selected cases.16 ALL was reported to have a synergistic function with ACL toward the stability of knee rotation3, 4, 5 without increasing long-term risk of osteoarthritis.17,18 It was also associated with a 2-fold reduction in the failure rate of medial meniscus repair and a 3-fold reduction in ACL graft rupture rates.9,19
Graft fixation also impacts the stability and healing of ACLR. Cortical suspensory fixation is characterized by circumferential graft-to-tunnel healing. Different fixation methods have been reported in the literature when ACLR and ALLR are considered.19 Sonnery-Cottet et al.19 fixed their autologous hamstring tendon with aperture screws, and Boutsiadis et al.20 used adjustable-loop suspensory fixation device with aperture screws. Both groups recreated SB ACLR and ALLR successfully. In the current study, we develop this technique to provide DB ACLR with ALLR at the same time. Further clinical results should be followed to discover the clinical significance in reducing residual rotational instability in comparison to conventional techniques.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The whole procedure of the surgery is as follows. A male professional kickboxer injured his right knee during competition. MRI revealed complete torn ACL. One month after the accident, he had very unstable knee and can't go back his game due to giving way sensation. High grade pivot was observed after anesthesia. We put him in supine position with a leg holder and then made all the bony landmarks, including lateral femoral epicondyle, Gerdy's tubercle, which led us to find out the origin and insertion of anterior lateral ligament, ALL. Normally, it is located 2 centimeters below the joint line. We used autogolus hamstring tendon graft, a closed looped endobutton and a Swivelock anchor to fix the graft. The semitendinosus tendon was looped three times, with one side linked with endobutton and the other side fixed with multiple Krakow sutures. The average length of the triple semitendinosus tendon was around 8.5 to 9cm and the diameter was around 7-8 mm in the femoral side, and 8-9 mm in the tibial side. The gracilis tendon was sutured at both ends, and the Fibertape from the Swivelock anchor was used as an internal brace to go along with gracilis tendon, which worked intra-articularlly as the PL bundle of ACL, and extra-articularlly as the ALL reconstruction. The average length of the gracilis tendon and Fibertape was always more than 15cm, which is long enough to make a loop starting from medial knee, intra-articularlly, out from lateral knee and then fixed at the medial knee again. The average diameter was less than 5mm, which allowed us to drill a femoral PL tunnel and an ALL-tibial tunnel with a 5mm rigid reamer. We debrided the torn ACL until clear visualization of the whole anatomy. A flexible pin was inserted in the center of the footprint of the AM bundle. Then a flexible reamer was then used to create the femoral AM tunnel according to the diameter of prepared tendon graft. We must make sure the posterior wall was preserved. One No.5 Ethibond suture would be passed within femoral AM tunnel for further tendon shuttling. Then the scope would be shifted into anteromedial portal. The ACL guide now was inserted through anterolateral portal, with its tip aiming at the center of the PL bundle footprint intra-articullarly, and the sheath outside the knee, aiming at the ALL-femoral origin. One rigid guide pin was then inserted with an outside-in manor, exiting intra-articularly at the center of PL bundle. A 5mm rigid reamer would be used to create femoral PL tunnel. Then, the tibial ACL tunnel would be made 1mm larger than the diameter of the tibial side of the prepared semitendinosus tendon. For example, if the tibial side of prepared semitendinosus tendon is 8mm, we used a 9mm reamer to create the tibial ACL tunnel. Another No. 5 Ethibond suture will then be passed through tibial ACL tunnel intra-articularly and pulled out extra-articularly by the grasper put in the femoral PL tunnel in advanced. We used this suture to tie the gracilis tendon and Fibertape, shuttling intraarticularly through the tibial ACL tunnel, and pulled out from femoral PL tunnel until they exited the skin of lateral thigh. The length outside the lateral femoral cortex should be long enough to create extraarticular ALL, which could be determined by the length of the gracilis incorporated inside the tibial ACL tunnel. In general, the single gracilis is long enough to occupy the full length of the tibial ACL tunnel and at least 25mm long, inside the tibia ALL tunnel. Thereafter, the AM bundle suture was tied with both limbs of endobutton, shuttling semitendinosus tendon proximally, until the button was flipped and fixed on the femoral cortical surface. A 6 x 25 mm interference screws would be used to fix the PLB by an outside-in manner. The tibial drill guide was set at 55°, with its tip aimed about 2 cm below ACL tibial tunnel, avoiding undesirable tunnel connection. The cannulated sleeve of the guide was placed posteriorly and proximally to the Gerdy's tubercle, where a stamp incision was made. Then, a pin is drilled from lateral to the medial side of the tibia and a consecutive 5 mm tunnel was created by a rigid reamer. A No.5 Ethibond suture was then shuttled from lateral to the medial tibia, facilitating further graft passage. Then another interference screw one millimeter larger than the size of the drilled tibial ACL tunnel, was used to fix the tibial end in the tibial ACL tunnel for both grafts and FiberTape at 60° of knee flexion. At last, the single gracilis and FiberTape were shuttled from the lateral end of the femoral PL tunnel, underneath the iliotibial band, to the lateral end of the tibial ALL tunnel as the ALLR. They were then shuttled through the tibial ALL tunnel from lateral to medial side of the tibia, making sure both gracilis and FiberTape were inside ALL tibial tunnel. The both limbs of No.2 Ethibond sutures of the gracillis and FiberTape were tied together at 20° of knee flexion and neutral knee rotation. Augmentation fixation was done by fixing as many sutures intraosseous by a 4.75 mm Swivelock anchor. The final construct is shown like the cartoon picture. Finally, we will check if there were any impingement during ROM. Luckily, no pivot was observed after the surgery in all our patients.
References
- 1.Zhang H., Qiu M., Zhou A., Zhang J., Jiang D. Anatomic anterolateral ligament reconstruction improves postoperative clinical outcomes combined with anatomic anterior cruciate ligament reconstruction. J Sports Sci Med. 2016;15:688–696. [PMC free article] [PubMed] [Google Scholar]
- 2.Heusdens C.H., Hopper G.P., Dossche L., Roelant E., Mackay G.M. Anterior cruciate ligament repair with independent suture tape reinforcement: A case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2019;27:60–67. doi: 10.1007/s00167-018-5239-1. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy M.I., Claes S., Fuso F.A. The anterolateral ligament: An anatomic, radiographic, and biomechanical analysis. Am J Sports Med. 2015;43:1606–1615. doi: 10.1177/0363546515578253. [DOI] [PubMed] [Google Scholar]
- 4.Slette E.L., Mikula J.D., Schon J.M. Biomechanical results of lateral extra-articular tenodesis procedures of the knee: A systematic review. Arthroscopy. 2016;32:2592–2611. doi: 10.1016/j.arthro.2016.04.028. [DOI] [PubMed] [Google Scholar]
- 5.Sonnery-Cottet B., Lutz C., Daggett M. The involvement of the anterolateral ligament in rotational control of the knee. Am J Sports Med. 2016;44:1209–1214. doi: 10.1177/0363546515625282. [DOI] [PubMed] [Google Scholar]
- 6.Anderson A.F., Snyder R.B., Lipscomb A.B., Jr. Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med. 2001;29:272–279. doi: 10.1177/03635465010290030201. [DOI] [PubMed] [Google Scholar]
- 7.Kocher M.S., Steadman J.R., Briggs K., Zurakowski D., Sterett W.I., Hawkins R.J. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84:1560–1572. doi: 10.2106/00004623-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H., Murphy C.G., Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43:1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 9.Sonnery-Cottet B., Saithna A., Cavalier M. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: A prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med. 2017;45:1547–1557. doi: 10.1177/0363546516686057. [DOI] [PubMed] [Google Scholar]
- 10.Markolf K.L., Park S., Jackson S.R., McAllister D.R. Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am. 2009;91:107–118. doi: 10.2106/JBJS.G.01215. [DOI] [PubMed] [Google Scholar]
- 11.Smith P.A., Bley J.A. Allograft anterior cruciate ligament reconstruction utilizing internal brace augmentation. Arthrosc Tech. 2016;5:e1143–e1147. doi: 10.1016/j.eats.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson S.R., Youssefzadeh K.A., Limpisvasti O. Anterior cruciate ligament reconstruction with suture tape augmentation: A surgical technique. Arthrosc Tech. 2019;8:e1579–e1582. doi: 10.1016/j.eats.2019.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaeding C.C., Aros B., Pedroza A. Allograft versus autograft anterior cruciate ligament reconstruction: Predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Desai N., Andernord D., Sundemo D. Revision surgery in anterior cruciate ligament reconstruction: A cohort study of 17,682 patients from the Swedish National knee ligament Register. Knee Surg Sports Traumatol Arthrosc. 2017;25:1542–1554. doi: 10.1007/s00167-016-4399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inderhaug E., Stephen J.M., Williams A., Amis A.A. Anterolateral tenodesis or anterolateral ligament complex reconstruction: Effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med. 2017;45:3089–3097. doi: 10.1177/0363546517724422. [DOI] [PubMed] [Google Scholar]
- 16.Tramer J.S., Fidai M.S., Kadri O. Anterolateral ligament reconstruction practice patterns across the United States. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118811063. 2325967118811063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duthon V.B., Magnussen R.A., Servien E., Neyret P. ACL reconstruction and extra-articular tenodesis. Clin Sports Med. 2013;32:141–153. doi: 10.1016/j.csm.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 18.Mouarbes D., Menetrey J., Marot V., Courtot L., Berard E., Cavaignac E. Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am J Sports Med. 2019;47:3531–3540. doi: 10.1177/0363546518825340. [DOI] [PubMed] [Google Scholar]
- 19.Sonnery-Cottet B., Vieira T.D., Ouanezar H. Anterolateral ligament of the knee: Diagnosis, indications, technique, outcomes. Arthroscopy. 2019;35:302–303. doi: 10.1016/j.arthro.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 20.Boutsiadis A., Brossard P., Panisset J.-C., Graveleau N., Barth J. Minimally invasive combined anterior and anterolateral stabilization of the knee using hamstring tendons and adjustable-loop suspensory fixation device: Surgical technique. Arthrosc Tech. 2017;6:e419–e425. doi: 10.1016/j.eats.2016.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The whole procedure of the surgery is as follows. A male professional kickboxer injured his right knee during competition. MRI revealed complete torn ACL. One month after the accident, he had very unstable knee and can't go back his game due to giving way sensation. High grade pivot was observed after anesthesia. We put him in supine position with a leg holder and then made all the bony landmarks, including lateral femoral epicondyle, Gerdy's tubercle, which led us to find out the origin and insertion of anterior lateral ligament, ALL. Normally, it is located 2 centimeters below the joint line. We used autogolus hamstring tendon graft, a closed looped endobutton and a Swivelock anchor to fix the graft. The semitendinosus tendon was looped three times, with one side linked with endobutton and the other side fixed with multiple Krakow sutures. The average length of the triple semitendinosus tendon was around 8.5 to 9cm and the diameter was around 7-8 mm in the femoral side, and 8-9 mm in the tibial side. The gracilis tendon was sutured at both ends, and the Fibertape from the Swivelock anchor was used as an internal brace to go along with gracilis tendon, which worked intra-articularlly as the PL bundle of ACL, and extra-articularlly as the ALL reconstruction. The average length of the gracilis tendon and Fibertape was always more than 15cm, which is long enough to make a loop starting from medial knee, intra-articularlly, out from lateral knee and then fixed at the medial knee again. The average diameter was less than 5mm, which allowed us to drill a femoral PL tunnel and an ALL-tibial tunnel with a 5mm rigid reamer. We debrided the torn ACL until clear visualization of the whole anatomy. A flexible pin was inserted in the center of the footprint of the AM bundle. Then a flexible reamer was then used to create the femoral AM tunnel according to the diameter of prepared tendon graft. We must make sure the posterior wall was preserved. One No.5 Ethibond suture would be passed within femoral AM tunnel for further tendon shuttling. Then the scope would be shifted into anteromedial portal. The ACL guide now was inserted through anterolateral portal, with its tip aiming at the center of the PL bundle footprint intra-articullarly, and the sheath outside the knee, aiming at the ALL-femoral origin. One rigid guide pin was then inserted with an outside-in manor, exiting intra-articularly at the center of PL bundle. A 5mm rigid reamer would be used to create femoral PL tunnel. Then, the tibial ACL tunnel would be made 1mm larger than the diameter of the tibial side of the prepared semitendinosus tendon. For example, if the tibial side of prepared semitendinosus tendon is 8mm, we used a 9mm reamer to create the tibial ACL tunnel. Another No. 5 Ethibond suture will then be passed through tibial ACL tunnel intra-articularly and pulled out extra-articularly by the grasper put in the femoral PL tunnel in advanced. We used this suture to tie the gracilis tendon and Fibertape, shuttling intraarticularly through the tibial ACL tunnel, and pulled out from femoral PL tunnel until they exited the skin of lateral thigh. The length outside the lateral femoral cortex should be long enough to create extraarticular ALL, which could be determined by the length of the gracilis incorporated inside the tibial ACL tunnel. In general, the single gracilis is long enough to occupy the full length of the tibial ACL tunnel and at least 25mm long, inside the tibia ALL tunnel. Thereafter, the AM bundle suture was tied with both limbs of endobutton, shuttling semitendinosus tendon proximally, until the button was flipped and fixed on the femoral cortical surface. A 6 x 25 mm interference screws would be used to fix the PLB by an outside-in manner. The tibial drill guide was set at 55°, with its tip aimed about 2 cm below ACL tibial tunnel, avoiding undesirable tunnel connection. The cannulated sleeve of the guide was placed posteriorly and proximally to the Gerdy's tubercle, where a stamp incision was made. Then, a pin is drilled from lateral to the medial side of the tibia and a consecutive 5 mm tunnel was created by a rigid reamer. A No.5 Ethibond suture was then shuttled from lateral to the medial tibia, facilitating further graft passage. Then another interference screw one millimeter larger than the size of the drilled tibial ACL tunnel, was used to fix the tibial end in the tibial ACL tunnel for both grafts and FiberTape at 60° of knee flexion. At last, the single gracilis and FiberTape were shuttled from the lateral end of the femoral PL tunnel, underneath the iliotibial band, to the lateral end of the tibial ALL tunnel as the ALLR. They were then shuttled through the tibial ALL tunnel from lateral to medial side of the tibia, making sure both gracilis and FiberTape were inside ALL tibial tunnel. The both limbs of No.2 Ethibond sutures of the gracillis and FiberTape were tied together at 20° of knee flexion and neutral knee rotation. Augmentation fixation was done by fixing as many sutures intraosseous by a 4.75 mm Swivelock anchor. The final construct is shown like the cartoon picture. Finally, we will check if there were any impingement during ROM. Luckily, no pivot was observed after the surgery in all our patients.
The whole procedure of the surgery is as follows. A male professional kickboxer injured his right knee during competition. MRI revealed complete torn ACL. One month after the accident, he had very unstable knee and can't go back his game due to giving way sensation. High grade pivot was observed after anesthesia. We put him in supine position with a leg holder and then made all the bony landmarks, including lateral femoral epicondyle, Gerdy's tubercle, which led us to find out the origin and insertion of anterior lateral ligament, ALL. Normally, it is located 2 centimeters below the joint line. We used autogolus hamstring tendon graft, a closed looped endobutton and a Swivelock anchor to fix the graft. The semitendinosus tendon was looped three times, with one side linked with endobutton and the other side fixed with multiple Krakow sutures. The average length of the triple semitendinosus tendon was around 8.5 to 9cm and the diameter was around 7-8 mm in the femoral side, and 8-9 mm in the tibial side. The gracilis tendon was sutured at both ends, and the Fibertape from the Swivelock anchor was used as an internal brace to go along with gracilis tendon, which worked intra-articularlly as the PL bundle of ACL, and extra-articularlly as the ALL reconstruction. The average length of the gracilis tendon and Fibertape was always more than 15cm, which is long enough to make a loop starting from medial knee, intra-articularlly, out from lateral knee and then fixed at the medial knee again. The average diameter was less than 5mm, which allowed us to drill a femoral PL tunnel and an ALL-tibial tunnel with a 5mm rigid reamer. We debrided the torn ACL until clear visualization of the whole anatomy. A flexible pin was inserted in the center of the footprint of the AM bundle. Then a flexible reamer was then used to create the femoral AM tunnel according to the diameter of prepared tendon graft. We must make sure the posterior wall was preserved. One No.5 Ethibond suture would be passed within femoral AM tunnel for further tendon shuttling. Then the scope would be shifted into anteromedial portal. The ACL guide now was inserted through anterolateral portal, with its tip aiming at the center of the PL bundle footprint intra-articullarly, and the sheath outside the knee, aiming at the ALL-femoral origin. One rigid guide pin was then inserted with an outside-in manor, exiting intra-articularly at the center of PL bundle. A 5mm rigid reamer would be used to create femoral PL tunnel. Then, the tibial ACL tunnel would be made 1mm larger than the diameter of the tibial side of the prepared semitendinosus tendon. For example, if the tibial side of prepared semitendinosus tendon is 8mm, we used a 9mm reamer to create the tibial ACL tunnel. Another No. 5 Ethibond suture will then be passed through tibial ACL tunnel intra-articularly and pulled out extra-articularly by the grasper put in the femoral PL tunnel in advanced. We used this suture to tie the gracilis tendon and Fibertape, shuttling intraarticularly through the tibial ACL tunnel, and pulled out from femoral PL tunnel until they exited the skin of lateral thigh. The length outside the lateral femoral cortex should be long enough to create extraarticular ALL, which could be determined by the length of the gracilis incorporated inside the tibial ACL tunnel. In general, the single gracilis is long enough to occupy the full length of the tibial ACL tunnel and at least 25mm long, inside the tibia ALL tunnel. Thereafter, the AM bundle suture was tied with both limbs of endobutton, shuttling semitendinosus tendon proximally, until the button was flipped and fixed on the femoral cortical surface. A 6 x 25 mm interference screws would be used to fix the PLB by an outside-in manner. The tibial drill guide was set at 55°, with its tip aimed about 2 cm below ACL tibial tunnel, avoiding undesirable tunnel connection. The cannulated sleeve of the guide was placed posteriorly and proximally to the Gerdy's tubercle, where a stamp incision was made. Then, a pin is drilled from lateral to the medial side of the tibia and a consecutive 5 mm tunnel was created by a rigid reamer. A No.5 Ethibond suture was then shuttled from lateral to the medial tibia, facilitating further graft passage. Then another interference screw one millimeter larger than the size of the drilled tibial ACL tunnel, was used to fix the tibial end in the tibial ACL tunnel for both grafts and FiberTape at 60° of knee flexion. At last, the single gracilis and FiberTape were shuttled from the lateral end of the femoral PL tunnel, underneath the iliotibial band, to the lateral end of the tibial ALL tunnel as the ALLR. They were then shuttled through the tibial ALL tunnel from lateral to medial side of the tibia, making sure both gracilis and FiberTape were inside ALL tibial tunnel. The both limbs of No.2 Ethibond sutures of the gracillis and FiberTape were tied together at 20° of knee flexion and neutral knee rotation. Augmentation fixation was done by fixing as many sutures intraosseous by a 4.75 mm Swivelock anchor. The final construct is shown like the cartoon picture. Finally, we will check if there were any impingement during ROM. Luckily, no pivot was observed after the surgery in all our patients.