Abstract
Massive, irreparable rotator cuff tears in patients without severe signs of osteoarthritis remains a major challenge for orthopaedic surgeons. These can be a source of significant pain and functional loss occurring most commonly in a relatively frail, elderly patient population. A plethora of surgical techniques covering minimally invasive, arthroscopic techniques and open, salvage procedures have been described for this challenging patient cohort. Continuous evolvement of arthroscopic techniques has led to all-arthroscopic superior capsular reconstruction techniques using allografts, thereby reducing donor side morbidity along with decreased soft tissue dissection. However, conventional superior capsular reconstruction is noted to be a technically complex, time-consuming, and high-cost surgery, which may put this technique beyond the confidence of many shoulder surgeons. The subacromial balloon spacer has emerged as a potential solution in these patients, providing interposition between the humeral head and acromion. However, the subacromial balloon biodegrades rapidly and its effect is only temporary. Thus this technique article presents using an acellular human dermal allograft to reconstruct the bursal layer, which is normally interposed between the humeral head and the acromion. The proposed technique provides a permanent interposition graft preventing humeral acromial contact, which does not undergo rapid biodegradation. The surgical technique is technically feasible, both minimizing surgical time and therefore operative risk to the patient.
Technique Video
Complete demonstration of the surgical bursal acromial reconstruction technique.
Massive, irreparable rotator cuff tears (RCT) in patients without severe signs of osteoarthritis remains a major challenge for orthopaedic surgeons. These can be a source of significant pain and functional loss occurring most commonly in a relatively frail, elderly patient population. A plethora of surgical techniques covering minimally invasive, arthroscopic techniques and open, salvage procedures have been described for this challenging patient cohort.1, 2, 3, 4, 5, 6
Recently, several biomechanical studies underlined the importance of the superior capsule and the (postero)superior rotator cuff as an important static stabilizer of the shoulder joint preventing superior migration of the humeral head.7, 8, 9, 10, 11 Consequently, superior capsular reconstruction (SCR), originally described by Mihata et al.9 in 2012, has since then evaded the field of orthopaedic surgery.6,8,12,13 Continuous evolvement of arthroscopic techniques has led to all-arthroscopic SCR techniques using allografts,14 thereby reducing donor side morbidity along with decreased soft tissue dissection.8,13 However, conventional SCR is noted to be a technically complex, time-consuming, and high-cost surgery, which may put this technique beyond the confidence of many shoulder surgeons. Additionally, a considerable number of anchors are needed to securely fix the graft between the greater tuberosity and superior glenoid rim. Subsequently, graft rupture and clinical failures may occur.15, 16, 17, 18, 19 This is more prevalent in the elderly population, with potentially poor glenoid and humeral head bone quality enhancing bone-anchor interface failure. To this, SCR requires an intact infraspinatus tendon for side-to-side attachment to the graft. As such, the subacromial balloon spacer has emerged as a potential solution in these patients, providing interposition between the humeral head and the acromion, preventing superior humeral translation, and potentially addressing recentering of the humerus in the glenoid.3,6,7 However, the subacromial balloon biodegrades rapidly and its effect on the humeral-acromial joint is only temporary.3,7
Thus this arthroscopic technique article presents an alternative technique to conventional SCR and the subacromial balloon spacer by reconstructing the normal bursal layer in-between the humeral head and acromion. An acellular human dermal allograft is fixed to the undersurface of the acromion, providing a permanent interposition graft, which does not biodegrade. The surgical technique is straightforward, minimizing surgical time and providing a permanent arthroscopic solution for this challenging patient group.
Surgical Technique (With Video Illustration)
Video 1 shows a complete demonstration of the surgical technique detailed in the following steps.
Step 1: Arthroscopic Preparation
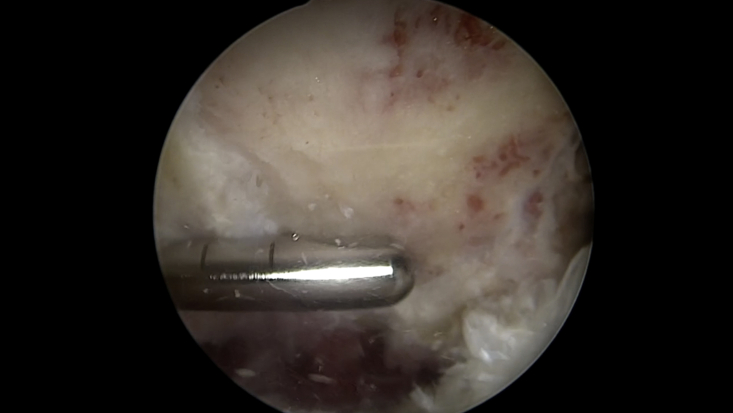
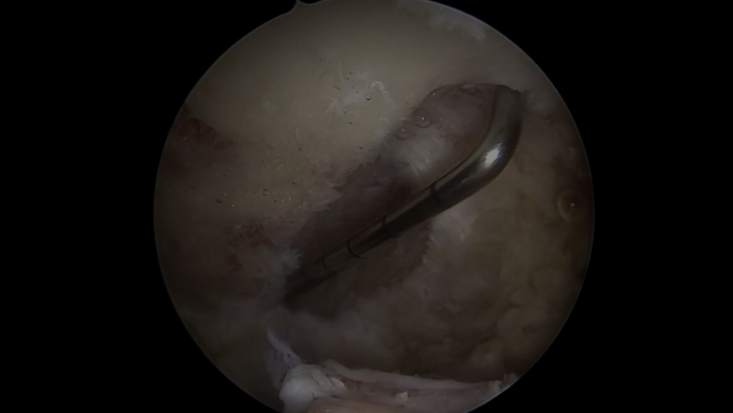
The patient is positioned in either the beach chair position (authors’ preference), or lateral decubitus position and prepared for standard shoulder arthroscopy, ensuring the acromioclavicular joint (ACJ) is within the surgical field. Arthroscopic viewing/working portal are shown in Fig 1 and further detailed later in this text. A bursectomy, minimal acromioplasty (Fig 2), and lateral clavicle excision are performed. This provides space for graft insertion, providing a flat, bleeding bed for graft application and access to tie the graft around the acromion.
Fig 1.
Left shoulder. Arthroscopic portal placement for the bursal acromial reconstruction procedure. (ACJ, acromioclavicular joint.)
Fig 2.
Left shoulder. A bursectomy, minimal acromioplasty, and lateral clavicle excision are performed. This provides space for graft insertion, providing a flat, bleeding bed for graft application and access to tie the graft around the acromion.
Step 2: Graft Preparation
The surface area of the acromion is measured (Fig 3), and the graft is trimmed to the appropriate size for sufficient coverage. In our experience, a 35- x 25-mm acellular human dermal allograft (ArthroFLEX, LifeNet Health, Virginia Beach, VA) is appropriate for most patients. A crossed suture tape configuration with “lasso-loop” knots at each corner is created by passing a SutureTape (Arthrex, Naples, FL) from corner to corner sequentially. These suture tapes provide a broad-based support for the graft.
Fig 3.
Left shoulder. The surface area of the acromion is measured to trim the graft to appropriate size for sufficient coverage. In our experience, a 35 x 25-mm acellular human dermal allograft (ArthroFLEX, LifeNet Health) is appropriate for most patients.
A suture loop is passed through the corner of the graft (Fig 4), and the tail of the suture is fed back through the loop and tightened to remove the slack. This technique has been termed the “lasso loop” (Fig 5).20 The lasso loop (Arthrex) is used on each corner, locking the sutures to the graft and holding the graft spread wide open when held under tension. The SutureTapes (Arthrex) are prepassed through the graft outside the body in anticipation of “shuttling” the graft into the subacromial space. Although multiple suture configurations could be used, the technique shown is useful because it locks the sutures to the graft, prevents them from sliding during delivery and fixation, and also helps keep the graft spread open. A FiberLink (Arthrex) and a TigerLink (Arthrex) are passed through the long medial and lateral sides of the graft, as shown in Fig 6.
Fig 4.
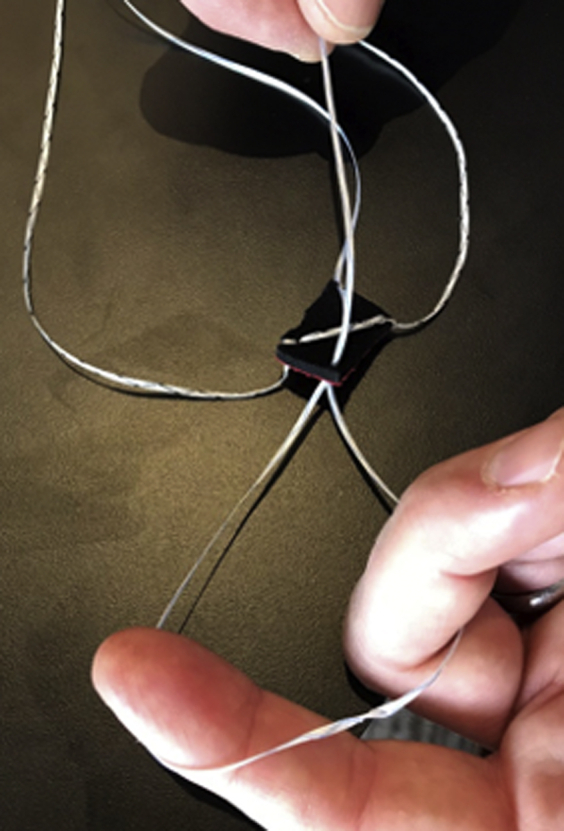
Initial pass creating “loop.”
Fig 5.
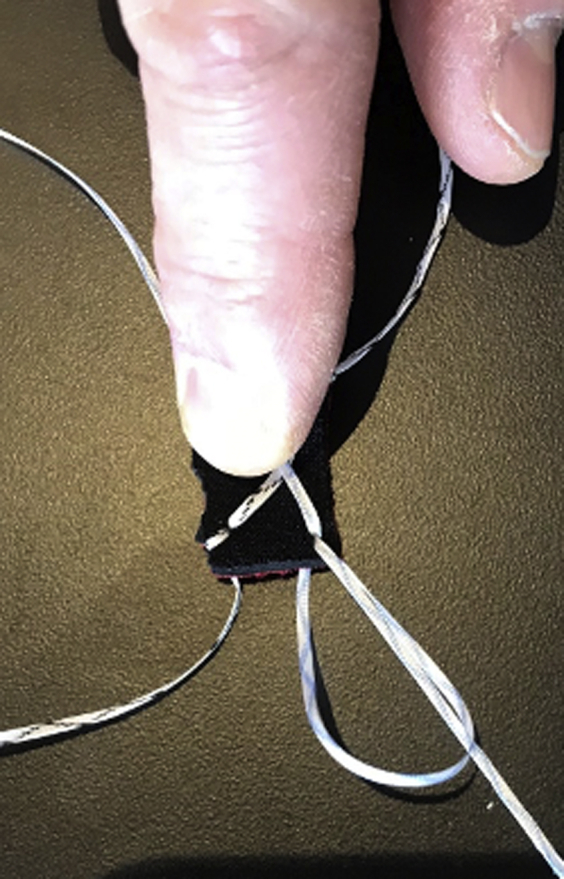
Free limb of suture passed through loop created.
Fig 6.
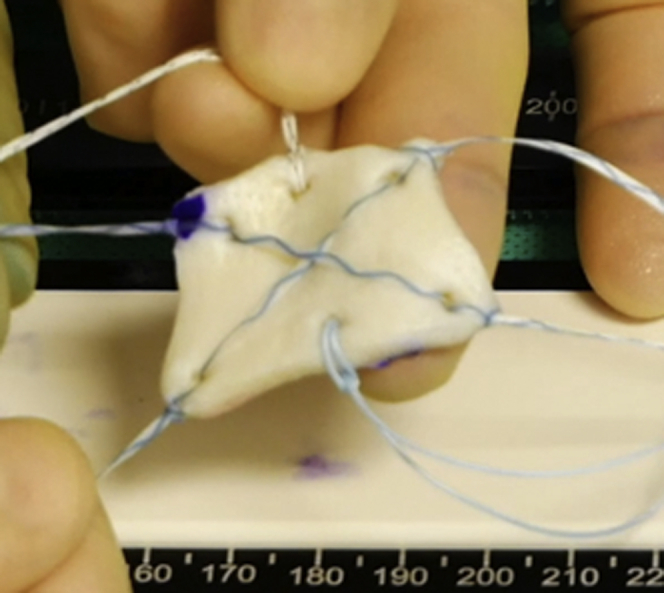
Final construct.
Step 3: Graft Insertion
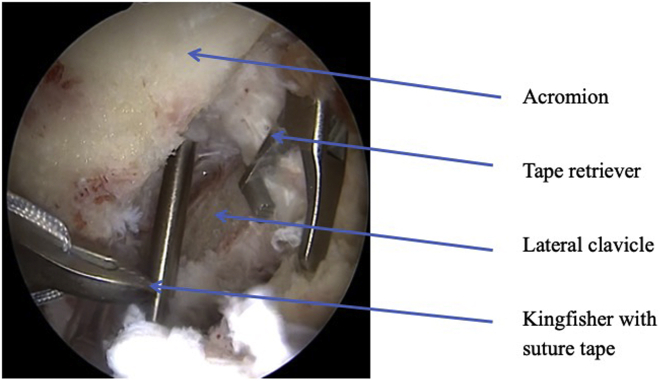
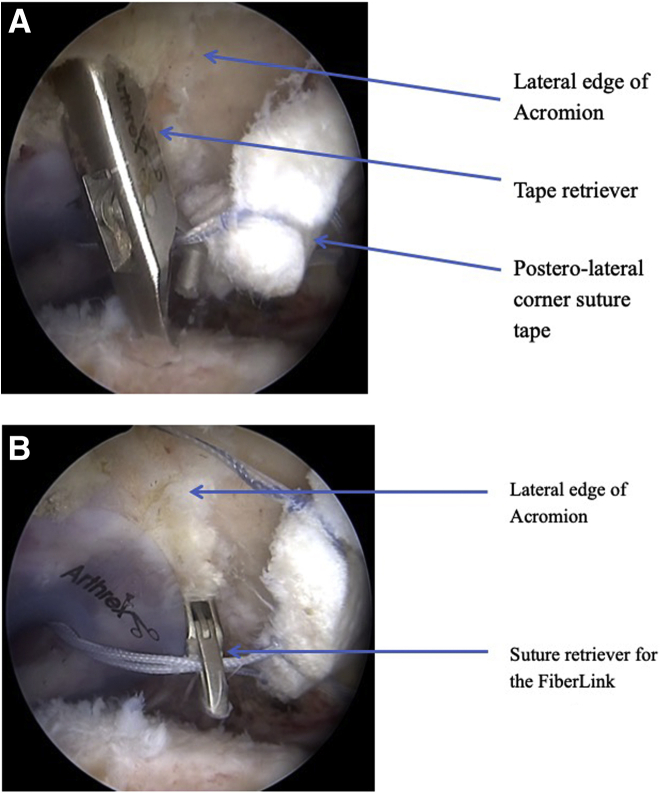
Place a suture tape retriever through the Neviaser portal and a suture manipulator thought the mid ACJ port, as shown in the arthroscopic image (Fig 7). Introduce the tape from the posteromedial corner of the graft through a 10- x 4-mm PassPort canula (Arthrex) using a grasper (Arthrex), and pass it off to the tape retriever positioned through the Neviaser portal. Retrieve the tape out through the Neviaser portal. Repeat this step, passing the FiberLink (Arthrex) from the long medial side to the waiting suture manipulator in the mid ACJ portal and retrieve. Finally, place the tape retriever in the anterior ACJ portal. Using a grasper (Arthrex), introduce the suture tape from the anteromedial corner of the graft into the subacromial space and pass it to the waiting tape retriever in the anterior ACJ portal. All 3 sutures from the medial side of the graft are now passed. The graft can be inserted into the subacromial space by a number of techniques. Either fold the graft lengthways in half then using a grasper to introduce the graft or use a back grasper (Arthrex). Once the graft is pulled into place under the acromion, the lateral 3 sutures need to be passed. Using a needle in outside-in-technique, locate the posterior lateral suture retrieval port. It should be opposite the medial Neviaser portal on the acromion. Introduce a tape retriever through this portal and retrieve the suture tape from the posterior lateral corner of the graft, as shown in Fig 8A. Sequentially repeat the earlier described step retrieving the FiberLink (Arthrex) from the long lateral edge of the graft (Fig 8B), and then finally the suture tape from the anterolateral corner.
Fig 7.
Left shoulder arthroscopic image showing suture tape retriever in the Neviaser portal. Lateral clavicle has been excised.
Fig 8.
(A, B) Arthroscopic image of left shoulder showing lateral suture retrieval of the suture tape.
All 6 sutures are now passed up through the bursa and retrieved out through the skin. The corresponding tails of each suture are then retrieved for tying. From the posterolateral acromial portal, introduce a KingFisher (Arthrex)/grasper, slide it along the superior surface of the acromion, and out through the anteromedial/ACJ portal. Retrieve the suture from the ACJ portal back out through the posterolateral acromial port, as shown in Fig 9.
Fig 9.

Posterior view of left shoulder showing retrieval of the suture tape from the acromioclavicular joint portal to the posterolateral portal ready for tying.
The FiberLinks (Arthrex) are then retireved out through the lateral mid acromial portal, and finally the remaining SutureTapes. The SutureTapes (Arthrex) are tyed initially, then the FiberLinks (Arthrex) are tied together, securing the graft on the undersurface of the acromium with the tapes wrapped and tied around the superior surface of the acromium (Fig 10 A and B).
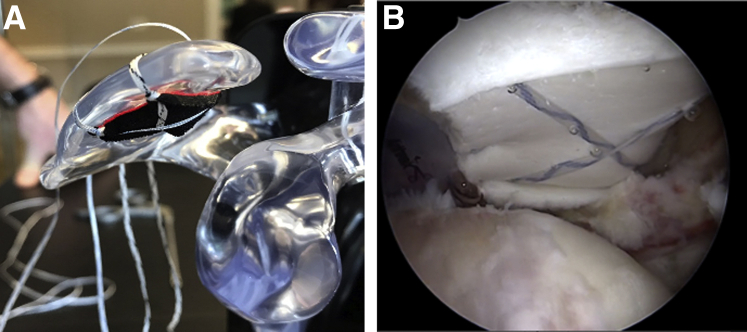
Fig 10.
(A) Acrylic model showing the graft on the undersurface of the acromium with sutures tied over the superior surface. (B) Arthroscopic image of a left shoulder showing the graft secured to the undersurface of the acromium articulating with the humeral head beneath.
Rehabilitation
The rehabilitation after bursal acromial reconstruction (BAR) focuses on maintaining shoulder movement and promoting deltoid strengthening, while maintaining graft integrity and avoiding excessive shearing forces and gently compressing the graft to promote bone-to-graft healing.
In the first 3 weeks postoperatively, the patient is treated with a shoulder sling, with passive supported lateral rotation from day 1, supported active lateral rotation from week 2, and passive- and active-assisted elevation up to 60°. From weeks 3 to 6, resistance is added to supported active lateral rotation, active unsupported open chain exercises without resistance are started (performed in uncompensated and comfortable ranges), and loading is initiated with the arm in neutral (e.g., Farmers walks, Suitcase walks, etc.). From week 6 onward, specific capsular/posterior joint stretching are started as able, resistance to open chain exercises all planes added (only for uncompensated ranges), and structured deltoid program is commenced.
Given that no longitudinal studies exist for this procedure, the rehabilitation has been informed using carefully applied clinical reasoning, knowledge of the procedure performed, and observations of postoperative outcomes in this early patient cohort.
Discussion
Irreparable rotator cuff tears can lead to significant limitation in active shoulder function, thus leading to pain and muscle weakness.7,21, 22, 23 Biomechanically, this is mainly owing to increased superior humeral head translation, which may enhance painful contact between the humeral head and the acromion.24, 25, 26, 27 Consequently, reconstruction of the superior capsule was demonstrated to improve shoulder function by reversing superior humeral head migration,9,10,28, 29, 30 and by acting as a “pillow” or a “spacer” underneath the acromion. Additionally, patients may benefit from SCR owing to pain relief of an interposition arthroplasty, thus preventing painful direct bone-to-bone contact. However, potential donor-site morbidity, high-learning curves, complex techniques, high-costs and high clinical failure rates, and early graft tears on the glenoidal side and concomitant graft failures still raises concern among shoulder surgeons when indicating patients for SCR.15, 16, 17, 18, 19 Thus the surgical procedure and the prolonged postoperative rehabilitation course of SCR is highly challenging, putting it beyond the confidence of many arthroscopists and patients. Several authors highlighted the need for careful patient choice and that SCR is not suitable for all cases of massive irreparable RCT.6,8,12,13
Along with SCR, the subacromial balloon spacer yielded initial promising outcomes,3 however, is limited to its availability and reduced longevity. In our experience, the subacromial balloon spacer held great early promise. A comparatively minimally invasive, surgically straightforward procedure with a logical mechanism of action; namely recentering the glenohumeral articulation and “cushioning” the acromiohumeral articulation. However, an internal audit of 32 patient procedures revealed a significant proportion of initial improvement, but sudden subsequent deterioration in pain and functional scores. The mean age for the cohort of patients undergoing this procedure was 72 years (range, 50-86 years). The mean Oxford Shoulder Score improved from 21 preoperatively to only 22.7 at 3 months, 24.5 at 6 months, and 28.3 at 12 months. In total, 11 out of 32 patients (34%) required further procedures (3 SCRs and 8 reverse arthroplasties). In patients younger than age 70 years (11 patients) the mean Oxford Shoulder Score improved from 19 preoperatively to 24 postoperatively. Six out of the 11 patients younger than age 70 years had further procedures compared with 5 out of 21 patients who were age 70 years or older. A common theme postoperatively in half the patients was a sudden onset deterioration in symptoms around the 6-week mark. We postulated that this was owing to the balloon’s inherent degradation and subsequent “popping,” with complete loss of beneficial effects.
However, biomechanical investigations underlined the importance of a subacromial spacer to properly retain the humeral head.7,9, 10, 11,30 The BAR technique, however, provides a permanent interposition graft, which does not biodegrade. In contrast to conventional SCR, the surgical technique is technically feasible, and minimizes surgical time without the use of bone anchors, thus opening an arthroscopic solution for this challenging patient group. Additionally, the BAR technique potentially offers greater longevity within a similar biomechanical mechanism of action. By providing a nonresorbable implant that creates a “cushion” between the humeral head and the acromion, the BAR prevents superior migration of the humeral head. The interposition effect of the graft in the setting of an SCR was examined by Mirzayan et al.31 who coined the term “biological tuberosity effect.” In their article, procedures in which the graft remained attached to the tuberosity had a significantly better outcome than those in which the tuberosity was uncovered.31
We therefore sought to devise a technique that combined the technical simplicity of the balloon interposition with the longevity of the allograft implant used in SCR. It incorporates the benefits of each of the previously described techniques but minimizes the potential negatives of these. Its longevity should prevent the early failures seen with the balloon interposition, while remaining a relatively simple procedure to perform. An additional factor to consider as a potential limitation to the SCR is its significant cost; the SCR technique requires 6 to 7 anchors, numerous sutures, and the allograft.
Of importance, the BAR procedure should not be considered as a panacea for all or all cuff tears in the elderly, but rather be considered that it has an important place within the armamentarium of the treating surgeon to manage a specific patient group. The indication for the BAR procedure includes an elderly patient with a compensated, irreparable RCT with minimal glenohumeral articulation degenerative joint disease. The presence of significant arthritis is a contraindication to the BAR procedure. Reverse total shoulder replacement remains our gold standard for management of these patients, but this is outside of the scope of this article. The main complaint to address in this patient population is pain from humeral acromial contact, termed “HAC pain,” with good passive and active range of motion. Overall, the inclusion criteria for SCR are similar, with the main difference being age of the patient. We reserve SCR for the younger cohort of patients, and BAR for the elderly group of patients (age ≥75 years). So far, the authors of this article have not used the BAR technique routinely in the pseudoparalytic shoulder in isolation. In the younger aged patient with pseudoparalysis and a preserved joint, we perform an SCR with a BAR. This gives the added benefit over a standard SCR in this patient group of a potential head depressor effect owing to the double thickness of graft material. Our framework for arthroscopic management of rotator cuff pathology is summarized in Table 1.
Table 1.
Decision-Making Algorithm
| Age <60 Years | Age 60-75 Years | Age >75 Years | Infraspinatus | Osteoarthritis | Compensated | Treatment Option |
|---|---|---|---|---|---|---|
| ✓ | X | X | If absent supraspinatus rotation graft | None | X | SCR + BAR |
| ✓ | ✓ | ?/X | Present | Mild | ✓ | SCR |
| X | X | ✓ | + / – | Mild | ✓ | BAR |
| X | X | ✓ | N/A | Mild | X | Reverse total shoulder arthroplasty |
| X | ? | ✓ | N/A | Severe | + / – | Reverse total shoulder arthroplasty |
BAR, bursal acromial reconstruction; N/A, not applicable; SCR, superior capsular reconstruction.
As with all operative procedures, there are potential risks and limitations (Tables 2 and 3). In particular, the human dermal allograft is a potential source of infection or immunologic response. It should be noted that the ArthroFLEX (LifeNet Health) dermal allograft used for this technique is an acellular dermal extracellular matrix processed which retains its growth factors, native collagen scaffold, and elastin, but with donor DNA removed from the dermal matrix, to create a biocompatible scaffold. Additionally, this technique does not directly address the function of the shoulder, in that there is no attempt to reconstruct the active function of the rotator cuff. However, the intended indication for the BAR is the shoulder with an irreparable cuff tear, as such, the graft acts to interpose between the humeral head and the acromion to prevent abnormal acromiohumeral articulation. To this, it potentially restores glenohumeral articular congruence, returning a mechanical advantage to the deltoid. This may allow a secondary functional improvement.
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
|
|
AP, anterior to posterior; CA, coracoacromical; ML, medial to lateral.
Table 3.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
SCR, superior capsular reconstruction.
Conclusions
This technique article presents the technique of BAR using an acellular dermal allograft in the treatment of irreparable RCTs in the elderly population.
Footnotes
The authors report the following potential conflict of interest or source of funding: The University of Connecticut Health Center/UConn Musculoskeletal Institute has received direct funding and material support from Arthrex Inc. (Naples, FL). The company and the society had no influence on the final manuscript. A.D.M. is a consultant for Orthofix and Arthrex and receives research grants from Arthrex. M.R. is a consultant for Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Complete demonstration of the surgical bursal acromial reconstruction technique.
References
- 1.Zastrow R.K., London D.A., Parsons B.O., Cagle P.J. Superior capsule reconstruction for irreparable rotator cuff tears: A systematic review. Arthroscopy. 2019;35:2525–2534.e1. doi: 10.1016/j.arthro.2019.02.053. [DOI] [PubMed] [Google Scholar]
- 2.Strauss E.J., Salata M.J., Kercher J. The arthroscopic management of partial-thickness rotator cuff tears: A systematic review of the literature. Arthroscopy. 2011;27:568–580. doi: 10.1016/j.arthro.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 3.Stewart R.K., Kaplin L., Parada S.A., Graves B.R., Verma N.N., Waterman B.R. Outcomes of subacromial balloon spacer implantation for massive and irreparable rotator cuff tears: A systematic review. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119875717. 2325967119875717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Namdari S., Voleti P., Baldwin K., Glaser D., Huffman G.R. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: A systematic review. J Bone Joint Surg Am. 2012;94:891–898. doi: 10.2106/JBJS.K.00841. [DOI] [PubMed] [Google Scholar]
- 5.Ladermann A., Collin P., Athwal G.S., Scheibel M., Zumstein M.A., Nourissat G. Current concepts in the primary management of irreparable posterosuperior rotator cuff tears without arthritis. EFORT Open Rev. 2018;3:200–209. doi: 10.1302/2058-5241.3.180002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kooistra B., Gurnani N., Weening A., van den Bekerom M., van Deurzen D. Low level of evidence for all treatment modalities for irreparable posterosuperior rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2019;27:4038–4048. doi: 10.1007/s00167-019-05710-0. [DOI] [PubMed] [Google Scholar]
- 7.Singh S., Reeves J., Langohr G.D.G., Johnson J.A., Athwal G.S. The subacromial balloon spacer versus superior capsular reconstruction in the treatment of irreparable rotator cuff tears: A biomechanical assessment. Arthroscopy. 2019;35:382–389. doi: 10.1016/j.arthro.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 8.Makovicka J.L., Chung A.S., Patel K.A., Deckey D.G., Hassebrock J.D., Tokish J.M. Superior capsule reconstruction for irreparable rotator cuff tears: A systematic review of biomechanical and clinical outcomes by graft type. J Shoulder Elbow Surg. 2020;29:392–401. doi: 10.1016/j.jse.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 10.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical effect of thickness and tension of fascia lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy. 2016;32:418–426. doi: 10.1016/j.arthro.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 11.Mihata T., Bui C.N., Akeda M. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elbow Surg. 2017;26:2158–2166. doi: 10.1016/j.jse.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 12.Ekhtiari S., Adili A.F., Memon M. Sources, quality, and reported outcomes of superior capsular reconstruction: A systematic review. Curr Rev Musculoskelet Med. 2019;12:173–180. doi: 10.1007/s12178-019-09551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catapano M., de Sa D., Ekhtiari S., Lin A., Bedi A., Lesniak B.P. Arthroscopic superior capsular reconstruction for massive, irreparable rotator cuff tears: A systematic review of modern literature. Arthroscopy. 2019;35:1243–1253. doi: 10.1016/j.arthro.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 14.Tokish J.M., Beicker C. Superior capsule reconstruction technique using an acellular dermal allograft. Arthrosc Techn. 2015;4:e833–e839. doi: 10.1016/j.eats.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lim S., AlRamadhan H., Kwak J.M., Hong H., Jeon I.H. Graft tears after arthroscopic superior capsule reconstruction (ASCR): Pattern of failure and its correlation with clinical outcome. Arch Orthop Trauma Surg. 2019;139:231–239. doi: 10.1007/s00402-018-3025-7. [DOI] [PubMed] [Google Scholar]
- 16.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 17.Hirahara A.M., Adams C.R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Techn. 2015;4:e637–e641. doi: 10.1016/j.eats.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferguson D.P., Lewington M.R., Smith T.D., Wong I.H. Graft utilization in the augmentation of large-to-massive rotator cuff repairs: A systematic review. Am J Sports Med. 2016;44:2984–2992. doi: 10.1177/0363546515624463. [DOI] [PubMed] [Google Scholar]
- 19.Castagna A., Garofalo R., Maman E., Gray A.C., Brooks E.A. Comparative cost-effectiveness analysis of the subacromial spacer for irreparable and massive rotator cuff tears. Int Orthop. 2019;43:395–403. doi: 10.1007/s00264-018-4065-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lafosse L., Van Raebroeckx A., Brzoska R. A new technique to improve tissue grip: “the lasso-loop stitch”. Arthroscopy. 2006;22:1246.e1–1246.e3. doi: 10.1016/j.arthro.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 21.Mihata T., Lee T.Q., Hasegawa A. Arthroscopic superior capsule reconstruction can eliminate pseudoparalysis in patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:2707–2716. doi: 10.1177/0363546518786489. [DOI] [PubMed] [Google Scholar]
- 22.Chung S.W., Kim J.Y., Kim M.H., Kim S.H., Oh J.H. Arthroscopic repair of massive rotator cuff tears: Outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41:1674–1683. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 23.Burkhart S.S., Hartzler R.U. Superior capsular reconstruction reverses profound pseudoparalysis in patients with irreparable rotator cuff tears and minimal or no glenohumeral arthritis. Arthroscopy. 2019;35:22–28. doi: 10.1016/j.arthro.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 24.Burkhart S.S., Esch J.C., Jolson R.S. The rotator crescent and rotator cable: An anatomic description of the shoulder's “suspension bridge”. Arthroscopy. 1993;9:611–616. doi: 10.1016/s0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 25.Thompson W.O., Debski R.E., Boardman N.D., 3rd A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24:286–292. doi: 10.1177/036354659602400307. [DOI] [PubMed] [Google Scholar]
- 26.Paletta G.A., Jr., Warner J.J., Warren R.F., Deutsch A., Altchek D.W. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elb Surg. 1997;6:516–527. doi: 10.1016/s1058-2746(97)90084-7. [DOI] [PubMed] [Google Scholar]
- 27.Nové-Josserand L., Edwards T.B., O'Connor D.P., Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Rel Res. 2005:90–96. doi: 10.1097/01.blo.0000151441.05180.0e. [DOI] [PubMed] [Google Scholar]
- 28.Mihata T., Lee T.Q., Hasegawa A. Superior capsule reconstruction for reinforcement of arthroscopic rotator cuff repair improves cuff integrity. Am J Sports Med. 2019;47:379–388. doi: 10.1177/0363546518816689. [DOI] [PubMed] [Google Scholar]
- 29.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44:1423–1430. doi: 10.1177/0363546516631751. [DOI] [PubMed] [Google Scholar]
- 30.Scheiderer B., Kia C., Obopilwe E. Biomechanical effect of superior capsule reconstruction using a 3-mm and 6-mm thick acellular dermal allograft in a dynamic shoulder model. Arthroscopy. 2020;36:355–364. doi: 10.1016/j.arthro.2019.08.026. [DOI] [PubMed] [Google Scholar]
- 31.Mirzayan R., Stone M.A., Batech M., Acevedo D.C., Singh A. Failed dermal allograft procedures for irreparable rotator cuff tears can still improve pain and function: The "Biologic Tuberoplasty Effect. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119863432. 2325967119863432. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Complete demonstration of the surgical bursal acromial reconstruction technique.
Complete demonstration of the surgical bursal acromial reconstruction technique.