Key Points
Question
What is the effect of clear and covered masks on communication in the surgeon-patient relationship?
Findings
In this randomized clinical trial of 200 patients, when surgeons wore clear masks rather than standard covered masks, patients rated their surgeon significantly higher in providing understandable explanations, demonstrating empathy, and eliciting trust.
Meaning
Patients reported improved communication when surgeons donned a clear mask, suggesting that not seeing the surgeon’s face may have negative consequences for the surgeon-patient relationship.
This randomized clinical trial evaluates the effects of clear vs standard covered masks on patient perceptions of communication with surgeons during outpatient surgical clinic encounters.
Abstract
Importance
During the COVID-19 pandemic, wearing masks has become necessary, especially within health care. However, to our knowledge, the consequences of mask wearing on communication between surgeons and patients have not been studied.
Objective
To evaluate the effects of clear vs standard covered masks on communication during surgical clinic encounters.
Design
This randomized clinical trial examined communication between surgeons and their patients when surgeons wore clear vs covered masks in surgical outpatient clinics at a single academic medical center. New patients were recruited from participating surgeons’ clinic schedules.
Interventions
Surgeons wore either clear masks or covered masks for each clinic visit with a new patient, based on a per-visit randomization plan.
Main Outcomes and Measures
The primary outcome measures included patient perceptions of (1) surgeon communication and (2) trust in surgeons, as well as (3) quantitative assessments and (4) qualitative assessments regarding patient impressions of the surgeon’s mask. After the clinic encounter, patients completed a verbal survey including validated Clinician and Group Consumer Assessment of Healthcare Providers and Systems questions. Additional questions involved surgeon empathy, trust, and the patient’s impression of the surgeon’s mask. Data were analyzed by comparing patient data in the clear vs covered groups using Cochran-Mantel-Haenszel tests, and comments were analyzed for themes.
Results
Two hundred patients were enrolled from 15 surgeons’ clinics spanning 7 subspecialties. When surgeons wore a clear mask, patients rated their surgeons higher for providing understandable explanations (clear, 95 of 100 [95%] vs covered, 78 of 100 [78%]; P < .001), demonstrating empathy (clear, 99 [99%] vs covered, 85 [85%]; P < .001), and building trust (clear, 94 [94%] vs covered, 72 [72%]; P < .001). Patients preferred clear masks (clear, 100 [100%] vs covered, 72 [72%]; P < .001), citing improved surgeon communication and appreciation for visualization of the face. Conversely, 8 of 15 surgeons (53%) were unlikely to choose the clear mask over their standard covered mask.
Conclusions and Relevance
This randomized clinical trial demonstrates that patients prefer to see their surgeon’s face. Surgeons who wore clear masks were perceived by patients to be better communicators, have more empathy, and elicit greater trust. Because masks will remain part of the health care landscape for some time, deliberate attention to preserving communication within the surgeon-patient relationship is warranted.
Trial Registration
ClinicalTrials.gov Identifier: NCT04595695
Introduction
Effective communication between physicians and patients has many known benefits, including improved patient understanding and adherence to treatment recommendations, superior clinical outcomes, and higher patient and clinician satisfaction.1,2,3,4,5 Communication is at the heart of the surgeon-patient relationship and crucial for developing trust, explaining complex concepts, and engaging patients in shared decision-making while accounting for their expectations and concerns.2,6,7
Nonverbal communication is a particularly important aspect of effective communication.8 Facial expressions are a key component of nonverbal communication, and during the COVID-19 pandemic, masks have become ubiquitous in the health care setting, inadvertently causing a potential barrier to effective communication.9 While the extent of long-term mask use in the health care setting remains unknown, for the time being, there is a demonstrated protective benefit to wearing masks10,11 and a general consensus that masks should continue to be worn, especially in the health care setting.12,13
Unfortunately, there are few data specifically studying the effect that masks have on communication with patients; however, there is evidence that they may serve as a hindrance to the patient-physician relationship.14 See-through or clear masks have demonstrated improved understanding for patients with hearing impairment,15 yet the benefit beyond this patient population appears to be unknown. Our hypothesis was that masks create communication barriers within the surgeon-patient relationship and clear masks would improve patient perceptions of surgeon communication. By randomizing surgeons to wearing either standard covered masks vs clear masks that allowed patients to see their surgeon’s entire face, this study aimed to evaluate patient perceptions of masks and how they may affect communication in the surgical clinic setting.
Methods
Surgeons at a single academic institution were recruited via email. Surgeons’ schedules were reviewed for new, in-person, outpatient clinic visits for patients with whom the surgeon had no prior relationship. Before each clinic day, using a group generator,16 the 15 participating surgeons were randomized to wearing either a clear vs covered mask type for each of their new patients. To be included, patients had to be older than 18 years, speak English fluently, and have capacity to make medical decisions independently. This study was approved by the institutional review board at the University of North Carolina at Chapel Hill and follows CONSORT reporting guidelines. The trial was registered with ClinicalTrials.gov (identifier: NCT04595695) after 80 participants had enrolled because of an administrative oversight. However, the protocol remained consistent for all enrolled patients and was not changed at any time throughout the clinical trial (Trial Protocol in Supplement 2). At the completion of the clinic visit, 1 researcher (I.M.K., wearing the same mask as the surgeon for consistency) met with the patient to seek verbal informed consent for study participation based on the institutional review board–approved consent language.
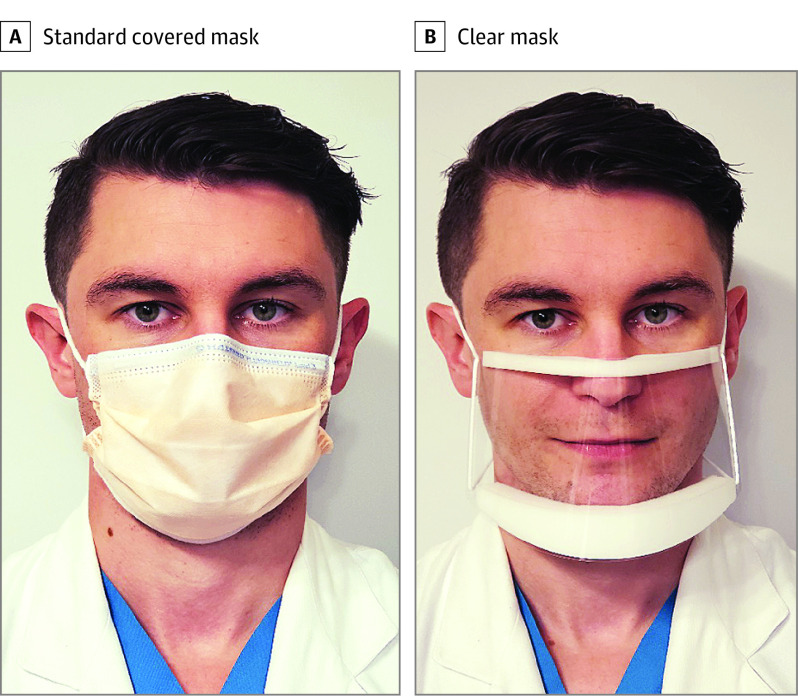
The surgeon was provided either a clear mask (ClearMask LLC)17 or instructed to wear their standard covered clinic mask for each encounter with a patient (Figure 1), based on the randomization. The clear masks are ASTM level 3, equivalent to the standard surgical masks. If the patient was deemed high risk and an N95 respirator was recommended based on hospital policy (eg, recent fever, cough, sore throat),18 the person was excluded from the study. If the surgeon declined to wear the clear mask or no longer wished to participate, they were removed from the study. Surgeons were instructed to conduct their clinic visit as they typically would, only mentioning that they were participating in a study if the patient asked about the mask. All patients wore a covered mask of their choosing during the clinic visits, per hospital policy.
Figure 1. Images of Masks.
A surgeon wearing a covered mask (A) and a clear mask (B).
Patient demographics were collected via the electronic health record. Patients were asked to confirm that this was their first time meeting the surgeon. Patient participation included a scripted 10-question verbal survey with 4-point Likert scale responses (eTable 1 in Supplement 1). The survey was adapted from the Clinician and Group Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) survey questions that measure communication (from 1, indicating not at all, to 4, indicating completely).19 Additional questions were added to assess surgeon empathy and trust, as well as a question rating the surgeon’s mask with an invitation to provide additional comments. Comments were immediately transcribed. Following completion of the survey, patients were provided debriefing information about the study design to avoid biasing their responses.
After the surgeons’ involvement in the study was complete, they were asked a single 4-point Likert-scale question regarding their likelihood of choosing the clear mask in the future (where 1 indicated a low likelihood and 4 a high likelihood). Additionally, surgeons were asked to provide feedback regarding their experience with wearing the mask.
Primary Outcomes and Measures
Because there appeared to be no previous existing data examining the effect of mask type on surgeon-patient communication, exploratory data analysis was conducted.20 As such, a single primary study end point was not selected at the outset of the trial. The 4 primary outcome measures included patient perceptions of (1) surgeon communication (measured by CG-CAHPS and empathy responses) and (2) patient trust in the surgeon, as well as (3) quantitative assessments and (4) qualitative assessments regarding patient impressions of the surgeon’s mask. An interval analysis was conducted to aid in calculating study end points.
Analysis
Likert responses were analyzed by question for clear vs covered masks. Given the tendency of patients to more frequently rate experiences as positive, answer choices were converted from Likert-scale data to dichotomous data. Consequently, answers were categorized as positive vs negative, which is also termed the top box method, a standard for evaluating CG-CAHPS data.21,22 As such, the top choice of 4 on the Likert scale was considered positive, whereas ratings of 1 to 3 were considered negative. Analysis was done using JMP version 14.3.0 (SAS Institute).
Based on trends noted in the data from the first 50 patients, sample sizes were calculated per question and variables were assumed to be dichotomous. An α level of .05 and power of 90% were used in the calculations. A minimum sample size of 180 patients was calculated, with 90 patients per group. Because of the exploratory nature of this study, the decision was made to terminate the trial at 200 patients. Following complete data collection, each question was analyzed using Cochran-Mantel-Haenszel tests, stratified by surgeon to remove potential individual surgeon bias to the results. All P values were calculated using χ2 tests and deemed significant at less than .05.
Patient and surgeon open-ended responses were qualitatively analyzed by multiple investigators (I.M.K., M.E.R., C.C., and M.R.K.) through open coding to create a codebook. Using a process of thematic analysis,23 codes were collapsed and expanded in an iterative fashion to ensure accurate data representation. Comments within each theme were grouped by tone and analyzed as a percentage of the total. Investigators (I.M.K., M.E.R., and M.R.K.) met regularly to review the data and arbitrate any differences in interpretations of emerging themes.
Results
Surgeon and Patient Demographics
Fifteen surgeons agreed to participate, with specialties including gastrointestinal surgery (n = 2), general surgery (n = 2), plastic surgery (n = 1), surgical oncology (n = 3), thoracic surgery (n = 3), transplant surgery (n = 2), and vascular surgery (n = 2). Six surgeons (40%) were women, and 9 were men. Surgeon race/ethnicities included Black/African American (n = 2), Asian (n = 2), White (n = 9), and Hispanic (n = 2). Surgeons accrued a mean (SD) of 13 (6) patients each, with surgeons donning each mask type approximately 50% of the time. One surgeon withdrew from the study early because of mask discomfort.
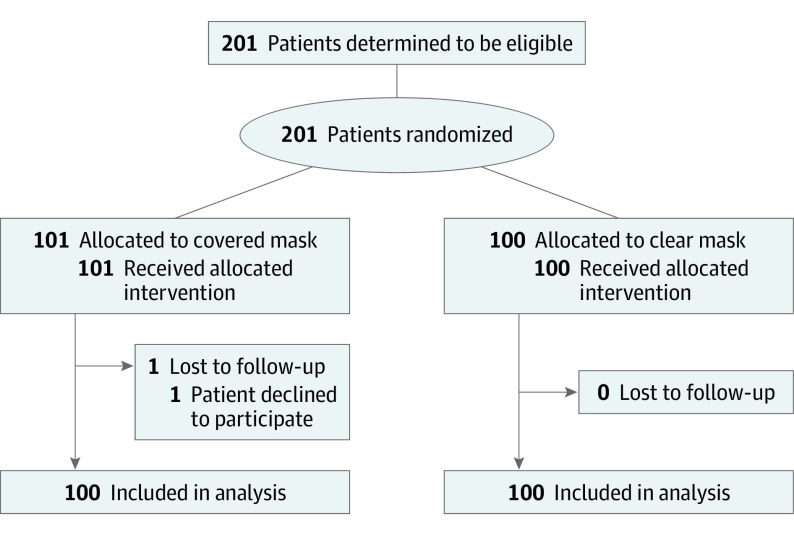
Two hundred patients were enrolled in this study from September 3 to November 12, 2020, 100 in each arm (Figure 2). Only 1 patient did not agree to participate after being approached by the research team. Of the patients, 114 (57%) were women, with 127 White participants and 66 Black/African American participants (Table 1). No demographic differences were found between patients in the clear vs covered mask groups.
Figure 2. CONSORT Diagram of Enrollment and Follow-up.
Table 1. Patient Demographics.
| Characteristic | Patients, No. | |
|---|---|---|
| Group with surgeons with covered masks (n = 100) | Group with surgeons with clear masks (n = 100) | |
| Female | 57 | 57 |
| Male | 43 | 43 |
| Age, mean (SD), y | 54 (18) | 55 (15) |
| Race/ethnicity | ||
| Black/African American | 34 | 32 |
| White | 63 | 64 |
| Other | 3 | 4 |
| Surgical visit type | ||
| General | 20 | 19 |
| Gastrointestinal | 9 | 8 |
| Oncology | 15 | 18 |
| Plastics | 8 | 8 |
| Thoracic | 10 | 13 |
| Transplant | 16 | 13 |
| Vascular | 22 | 21 |
Primary Study Outcomes
Surgeon Communication and Trust
Patients in general provided mostly positive answers to the survey questions. Within the clear mask group, all questions were answered positively by at least 93% of patients (explaining, 95 patients; listening, 99 patients; answering questions, 99 patients; knowing history, 100 patients; showing respect, 97 patients; spending time, 97 patients; demonstrating empathy, 99 patients; trust in surgeon decisions, 94 patients; comfort with surgeon operating, 94 patients; mask impression, 100 patients). However, within the covered mask group, several questions were answered positively only between 70% to 80% of the time (explaining, 78 patients; knowing history, 78 patients; trust in surgeon decisions, 72 patients; and mask impression, 72 patients), with the remainder having results closer to those of the clear mask group (listening, 97 patients; answering questions, 95 patients; showing respect, 96 patients; spending time, 97 patients; demonstrating empathy, 85 patients; comfort with surgeon operating, 88 patients). For all questions, the clear mask group answered positively at the same or greater frequency than the covered mask group.
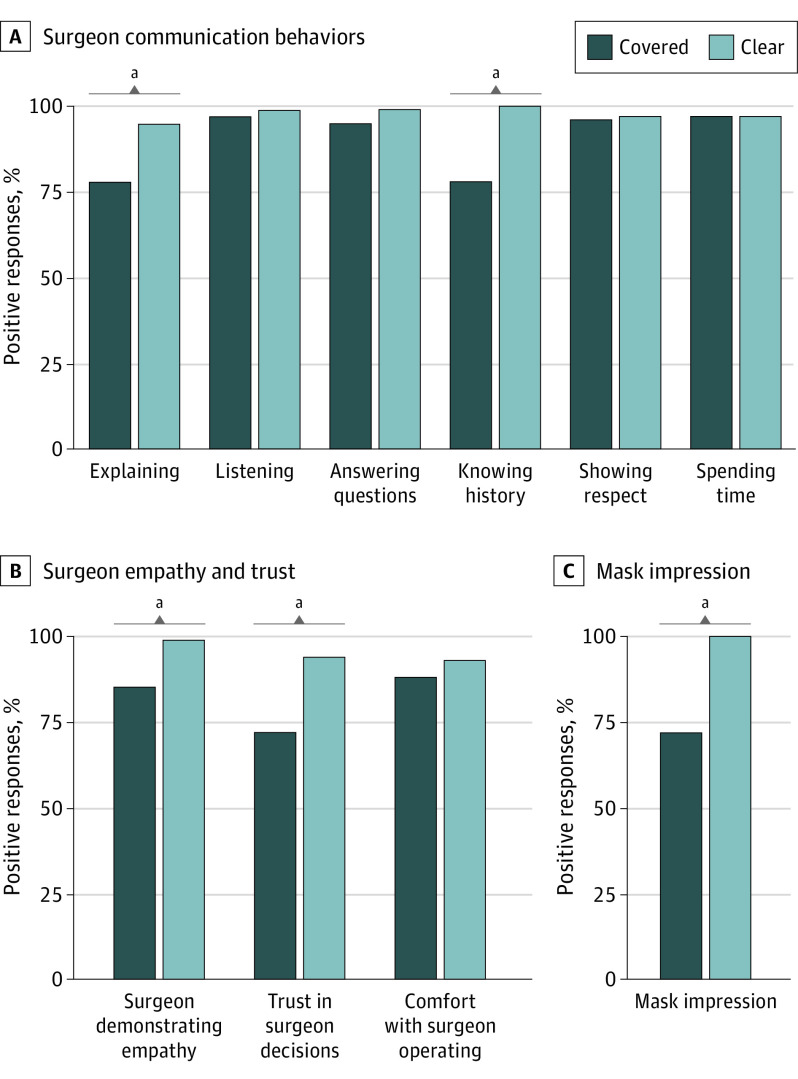
Regarding the CG-CAHPS questions (Figure 3A), patients in the clear mask group had significantly more positive responses compared with the covered mask group when answering 2 questions: “Did this provider explain things in a way that was easy to understand?” (clear masks, 95 patients [95%] vs covered masks, 78 patients [78%]; P < .001) and “Did this provider seem to know the important information about your medical history?” (100 patients [100%] vs 78 patients [78%]; P < .001). These differences were not seen in the other CG-CAHPS questions.
Figure 3. Positive Patient Responses by Mask Type.
A, Clinician and Group Consumer Assessment of Healthcare Providers and Systems questions pertaining to surgeon communication behaviors. B, Surgeon empathy and trust questions. C, Patient impression of mask. aP < .001.
Concerning surgeon empathy (Figure 3B), patients in the clear mask group had significantly more positive responses (99 patients [99%]) compared with the covered mask group (85 patients [85%]; P < .001). Similarly, patients in the clear mask group more frequently reported trusting their surgeon’s decisions (94 patients [94%] vs 72 patients [72%]; P < .001; Figure 3B). Even with the differences in levels of reported trust between groups, there was no statistical difference in patient comfort for allowing surgeons to operate.
Patient Impressions of Mask Type: Quantitative and Qualitative Analyses
When asked about their impressions of the surgeon mask, patients whose surgeon wore a clear mask had unanimously positive ratings (100 patients [100%]). This was significantly different than the positive ratings patients gave to the covered masks (72 patients [72%]; P < .001; Figure 3C).
Patient comments regarding masks mirrored their ratings (Table 2 and eTables 2 and 3 in Supplement 1), with comments about the clear masks being overwhelmingly positive (91 of 97 comments [94%] positive) whereas comments regarding the covered masks more frequently ranged from neutral to negative (24 of 86 comments [28%] positive). Four major themes were identified: opinions, communication factors, visualization of the face, and utility. Of the comments voiced by the patients that were labeled as opinions (129 opinion comments of 183 total comments [70.5%]), for the clear masks, 93% were positive (68 of 74 opinion comments on clear masks); for the covered masks, only 5% were positive (3 of 55 opinion comments on covered masks; P < .001). Communication factors included comments involving hearing and understanding the surgeon, whereas comments on visualization of the face concerned patients’ ability to see the surgeons face, lips, or mouth. Patients felt that the clear masks provided a view of the surgeon’s face (42 comments on facial visualization of 97 comments on clear masks [43%]) and improved understanding of the surgeon’s words (35 comments on understanding of 97 comments on clear masks [36%]). Mask utility involved comments about perceived comfort or protection. Some patients (13 comments on utility of 97 comments on clear masks [13%]) felt that clear masks appeared more comfortable and/or were perceived as providing better protection against viral transmission. Overall, patient comments demonstrated an excitement for the clear mask, whereas covered masks were more often met with complaints.
Table 2. Themes and Representative Quotations of Patient Impressions of Their Surgeon’s Mask.
| Themes | Patient group | |
|---|---|---|
| Surgeon with covered mask | Surgeon with clear mask | |
| Opinion | ||
| Positive/ negative |
|
|
| Communication factors | ||
| Understanding/ hearing |
|
|
| Visualization of the face | ||
| Face/mouth |
|
|
| Expressions |
|
|
| Utility | ||
| Comfort |
|
|
| Protection |
|
|
Surgeon Responses
When surgeons were asked how likely they are to choose the clear mask for future encounters, only 47% responded favorably (with a score of 3 or 4) on a 4-point Likert scale (in which 1 was a low likelihood and 4 a high likelihood; 1: n = 6 surgeons; 2: n = 2; 3: n = 5; 4: n = 2). (The top box method was not used for this finding because surgeon responses were thought to not adhere to the same response pattern as patient responses, since these data were more normally distributed.) Four surgeons (27%) mentioned that their likelihood of choosing the clear mask would be higher if patients demonstrated a preference for it. Surgeons commented both positively and negatively about the comfort of wearing clear masks, which included mask fit and mask fogging. Importantly, several surgeons voiced concerns regarding the perceived level of protection from the clear mask.
Discussion
The unprecedented COVID-19 pandemic has brought changes across health care, one of which is the widespread use of masks. While critical to health and safety, the interpersonal consequences of routinely wearing masks are not clearly understood. This randomized clinical trial is, to our knowledge, the first study to examine the effect of the surgeon’s mask on communication with patients in the clinic setting. Surgeons were randomized by individual patient clinic encounters to wearing either a clear or covered mask; at the conclusion of the visit, patients were asked to evaluate their communication experience with their surgeon using standardized CG-CAHPS questions, as well as additional questions pertaining to surgeon empathy and trust. For all questions, nearly all patients rated surgeons wearing the clear masks favorably. Surgeons wearing clear masks vs covered masks were rated significantly higher for 3 communication behaviors: explaining in an understandable way, knowing medical history, and demonstrating empathy. Perhaps most interestingly, patients in the clear mask group reported higher trust in the surgeon’s decisions than patients in the covered mask group, although mask type did not affect patient comfort level with the surgeon operating. While patients showed an overwhelming preference for their surgeon wearing a clear mask, more than half of the surgeons would not choose to wear the clear mask in the future.
Examining the CG-CAHPS questions, more patients interacting with surgeons wearing a clear mask felt that the surgeons knew their medical history and explained things in an understandable way compared with surgeons wearing a covered mask. While the words and communication techniques the surgeons used to explain concepts likely did not change based on the mask they wore, the patients’ perceptions were nonetheless altered. This may be for multiple reasons, including both verbal and nonverbal barriers caused by the covered masks. Multiple patients expressed difficulty with hearing their surgeon while they wore a covered mask. Although both masks likely muffle sounds, many patients felt it was easier to hear when surgeons wore clear masks. By covering the surgeon’s face below the eyes, patients lose many of the nonverbal cues expressed by the surgeon to aid in explanation. The clear mask allows for the patient to read the surgeon’s lips, while also visualizing nonverbal facial expressions. This may explain the higher ratings expressed by patients in these 2 domains.
A key finding in our study is that patients perceived higher surgeon empathy in the clear mask group compared with the covered mask group. The effect of masks on physician-patient interactions was examined in a large 2013 study14 performed in Hong Kong in patients in primary care who were randomized to their physician wearing a mask vs no mask. Patients rated physician empathy lower in the mask group, although there was no difference in overall patient satisfaction. Although this study focused on a different population within a different culture, their findings mirror ours in that the patients perceived lower empathy when the physician’s face was not visible. Demonstrating empathy is a critical skill for a successful physician-patient relationship,24,25 because it improves patient satisfaction and leads to better outcomes.26,27 A significant portion of empathy is nonverbal, with facial expressions playing a key role in effective communication.28,29,30 Therefore, deliberate emphasis on verbal empathic responses is needed, especially in the COVID-19 era.
A vital component of the physician-patient relationship is trust, which has been linked to higher patient satisfaction, beneficial patient behaviors, fewer symptoms, and a higher quality of life.31 In our study, 22% fewer patients reported complete trust in their surgeon’s decisions when the surgeon wore a covered mask vs a clear mask. Surgical procedures are associated with risks, which are often quite significant. With diminished trust between patient and surgeon, any deviation from the expected result of an operation may lead to considerable frustration, accusations, and even litigation.32 While patients in the covered mask group reported decreased trust in their surgeon’s decisions, mask type did not affect their comfort with allowing the surgeon to operate to the same extent. This disconnection could have significant implications for both the patient experience and surgeon practice. However, as with empathy, the negative effect of the covered mask on trust was mitigated by the clear mask.
While patients preferred their surgeon wearing a clear mask, surgeons did not rate the mask as highly. More than half of the participating surgeons were unlikely to choose the clear mask in the future. Most concerning, surgeons voiced questions about appropriate protection. While the clear masks’ protection rating is equivalent to standard covered masks, lack of confidence in their ability to provide protection would likely be a barrier in their use. Importantly, some surgeons expressed a willingness to wear the clear mask if there was a demonstrated patient benefit. This study does show that benefit, in that the negative consequences of surgeons wearing covered masks were significantly mitigated by the clear mask.
Strengths
Our study has strengths. This was the first study, to our knowledge, to examine the effect of concealing the surgeon’s face on surgeon-patient communication in the clinic setting, and it was done so in a randomized fashion to minimize bias. The findings are strengthened by the large number of patient encounters and the fact that patients had no prior relationship with the surgeon. Additionally, both our patient population and surgeon specialty type were diverse, contributing to the generalizability of the results.
Limitations
Although there are many strengths of this study, the results should be viewed within its limitations. While surgeons were not aware of the patient questions or responses, they were unable to be blinded to their mask type, which may have introduced bias in their patient interactions. Similarly, the researcher surveying the patients was not blinded to mask type, which may have inadvertently influenced patient responses, although a verbal script was followed. Additionally, because patients were asked to immediately answer questions following the clinic visit, their responses may have been more positive than if they completed responses later, in an anonymously written form. However, the effect of question format should be mitigated by the randomization. Lastly, we studied only 1 type of clear mask and acknowledge that many styles of face coverings are increasingly available. Further investigation is needed.
Conclusions
The COVID-19 pandemic has abruptly changed health care in ways never before seen. Masks are an important and necessary part of preventing the spread of COVID-19; however, there have been consequences on the surgeon-patient relationship. This randomized clinical trial comparing patient ratings of surgeons wearing clear vs covered masks suggests that not seeing the surgeon’s face negatively affects patient understanding, perceived empathy, and trust. These findings should alert surgeons, because patient perceptions may not be detectable without purposeful attention to communication. We must make every effort to protect the sacred physician-patient relationship during these unprecedented times. Additional investigation is needed to better understand the differences in communication with clear and covered masks and whether there are other communication behaviors or technologies that may mitigate the effects of covered masks. In the meantime, health care workers must be aware of the barrier created by covering their face and find ways to overcome it.9,33
eTable 1. Patient Questions Following Clinic Visit with Surgeon
eTable 2. Individual Patient Comments Regarding Surgeons’ Covered Masks
eTable 3. Individual Patient Comments Regarding Surgeons’ Clear Masks
Trial Protocol
Data Sharing Statement
References
- 1.Burney DW III. Surgeon-patient communication: the key to patient satisfaction, patient-centered care, and shared decision making. Instr Course Lect. 2017;66:659-665. [PubMed] [Google Scholar]
- 2.Tongue JR, Epps HR, Forese LL. Communication skills. Instr Course Lect. 2005;54:3-9. [PubMed] [Google Scholar]
- 3.Stewart M, Brown JB, Boon H, Galajda J, Meredith L, Sangster M. Evidence on patient-doctor communication. Cancer Prev Control. 1999;3(1):25-30. [PubMed] [Google Scholar]
- 4.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826-834. doi: 10.1097/MLR.0b013e31819a5acc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kapadia MR, Kieran K. Being affable, available, and able is not enough: prioritizing surgeon-patient communication. JAMA Surg. 2020;155(4):277-278. doi: 10.1001/jamasurg.2019.5884 [DOI] [PubMed] [Google Scholar]
- 6.Levinson W, Hudak P, Tricco AC. A systematic review of surgeon-patient communication: strengths and opportunities for improvement. Patient Educ Couns. 2013;93(1):3-17. doi: 10.1016/j.pec.2013.03.023 [DOI] [PubMed] [Google Scholar]
- 7.Han JL, Pappas TN. A review of empathy, its importance, and its teaching in surgical training. J Surg Educ. 2018;75(1):88-94. doi: 10.1016/j.jsurg.2017.06.035 [DOI] [PubMed] [Google Scholar]
- 8.Little P, White P, Kelly J, Everitt H, Mercer S. Randomised controlled trial of a brief intervention targeting predominantly non-verbal communication in general practice consultations. Br J Gen Pract. 2015;65(635):e351-e356. doi: 10.3399/bjgp15X685237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schlögl M, A Jones C. Maintaining our humanity through the mask: mindful communication during COVID-19. J Am Geriatr Soc. 2020;68(5):E12-E13. doi: 10.1111/jgs.16488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020;92(9):1567-1571. doi: 10.1002/jmv.25805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8(5):434-436. doi: 10.1016/S2213-2600(20)30134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization . What is WHO’s view on masks? Updated June 7, 2020. Accessed October 8, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-masks
- 13.US Centers for Disease Control and Prevention . Guidance for wearing masks: help slow the spread of COVID-19. Updated August 2020. Accessed October 8, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html
- 14.Wong CK, Yip BH, Mercer S, et al. Effect of facemasks on empathy and relational continuity: a randomised controlled trial in primary care. BMC Fam Pract. 2013;14:200. doi: 10.1186/1471-2296-14-200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Atcherson SR, Mendel LL, Baltimore WJ, et al. The effect of conventional and transparent surgical masks on speech understanding in individuals with and without hearing loss. J Am Acad Audiol. 2017;28(1):58-67. doi: 10.3766/jaaa.15151 [DOI] [PubMed] [Google Scholar]
- 16.RandomLists . Random team generator:. Accessed October 12, 2020. https://www.randomlists.com/team-generator
- 17.ClearMask, LLC . See the person, not the mask. Published 2021. Accessed February 24, 2021. https://www.theclearmask.com/
- 18.UNC Health Care . Physician resources. Updated April 14, 2020. Accessed October 12, 2020. https://www.unchealthcare.org/coronavirus/physician-resources/
- 19.Agency for Healthcare Research and Quality . CAHPS clinician & group survey. Updated June 2020. Accessed October 8, 2020. https://www.ahrq.gov/cahps/surveys-guidance/cg/index.html
- 20.Tukey JW. We need both exploratory and confirmatory. The American Statistician. 1980;34(1):23-25. doi: 10.2307/2682991 [DOI] [Google Scholar]
- 21.MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychol Methods. 2002;7(1):19-40. doi: 10.1037/1082-989X.7.1.19 [DOI] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research and Quality . The CAHPS Clinician & Group Survey Database: how results are calculated. Updated July 2016. Accessed February 24, 2021. https://cahpsdatabase.ahrq.gov/cahpsidb/Public/Files/Doc4_How_Results_are_Calculated_CG_2015.pdf
- 23.Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1). doi: 10.1177/1609406917733847 [DOI] [Google Scholar]
- 24.Halpern J. What is clinical empathy? J Gen Intern Med. 2003;18(8):670-674. doi: 10.1046/j.1525-1497.2003.21017.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berman AC, Chutka DS. Assessing effective physician-patient communication skills: “Are you listening to me, doc?”. Korean J Med Educ. 2016;28(2):243-249. doi: 10.3946/kjme.2016.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-e84. doi: 10.3399/bjgp13X660814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sinclair S, Beamer K, Hack TF, et al. Sympathy, empathy, and compassion: a grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliat Med. 2017;31(5):437-447. doi: 10.1177/0269216316663499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frith C. Role of facial expressions in social interactions. Philos Trans R Soc Lond B Biol Sci. 2009;364(1535):3453-3458. doi: 10.1098/rstb.2009.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zenger J, Folkman J. What great listeners actually do. Published July 14, 2016. Accessed February 15, 2021. https://hbr.org/2016/07/what-great-listeners-actually-do
- 30.Benbenishty JS, Hannink JR. Non-verbal communication to restore patient-provider trust. Intensive Care Med. 2015;41(7):1359-1360. doi: 10.1007/s00134-015-3710-8 [DOI] [PubMed] [Google Scholar]
- 31.Birkhäuer J, Gaab J, Kossowsky J, et al. Trust in the health care professional and health outcome: a meta-analysis. PLoS One. 2017;12(2):e0170988. doi: 10.1371/journal.pone.0170988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murff HJ, France DJ, Blackford J, et al. Relationship between patient complaints and surgical complications. Qual Saf Health Care. 2006;15(1):13-16. doi: 10.1136/qshc.2005.013847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duckett K. Behind the mask: new challenges to gaining patient trust. Home Healthc Now. 2020;38(6):327-330. doi: 10.1097/NHH.0000000000000940 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Patient Questions Following Clinic Visit with Surgeon
eTable 2. Individual Patient Comments Regarding Surgeons’ Covered Masks
eTable 3. Individual Patient Comments Regarding Surgeons’ Clear Masks
Trial Protocol
Data Sharing Statement