Abstract
Background.
Slipped rib syndrome (SRS) is a painful disorder caused when 1 or more of the 8th-10th false ribs become abnormally mobile. Established treatment modalities include analgesia, intercostal nerve injection, and costal cartilage excision. No definitive surgical correction of SRS without cartilage excision has been previously described. We aimed to determine whether a nonexcisional repair technique in affected adults could demonstrate significant relief from SRS using standardized outcome measures.
Methods.
We performed a retrospective review of cases of SRS treated at our institution in 2019. We obtained data by survey before and after sutured 10th rib fixation, using a self-reported rating scale from 0–10 at defined intervals. Surveyed outcome measures were compared pre- and postoperatively using the Wilcoxon signed rank sum test. The use of neural modulating, narcotic, and nonsteroidal antiinflammatory drug medications was also compared pre- and postoperatively using McNemar’s test where applicable.
Results.
SRS was diagnosed using clinical examination alone in 42 adults and repaired in 29 patients. Median postoperative improvement in pain at 1 and 6 months was 75% (P < .001) and 80% (P < .001), respectively. Improvements in other outcome measures were similar. In patients who took pain medications preoperatively, narcotics were discontinued at 1 month by 100%, neural modulators by 86%, and nonsteroidal antiinflammatory drugs by 92% (all P values < .001). Pain medication use remained minimal at 6 months in 23 (79%) of patients completing follow-up.
Conclusions.
Minimally invasive slipped rib repair in adults provides significant relief of SRS, offering a useful alternative to costal cartilage excision. It is well tolerated and effective.
Slipped rib syndrome (SRS) is a painful disorder1–3 caused by 1 or more abnormally mobile false 8th-10th ribs.3 It most commonly occurs in the 10th rib. The normally nonfloating 8th-10th cartilaginous rib tips coalesce into a common arch to join the sternum.4,5 Through various etiological processes including trauma3,4 and degenerative changes, 1 or more of the anterior rib tips may slip away and separate from the arch.
A slipped rib is anchored to the axial skeleton only posteriorly at the costovertebral joint. Intercostal nerves are known to be highly sensitive and prone to producing chronic pain when injured. With minimal, repetitive movement of the slipped rib compressing the intercostal nerve against the stable rib above it,4–6 the nerve may become irritated. It may generate severe pain in a dermatomal distribution in the affected intercostal space, originating anteriorly and radiating back to the spine. Such intercostal neuralgia is the predominant symptom observed in SRS. SRS is common2 and, in some reports,1,7 accounts for 1% of all new general medical referrals and 5% of new gastroenterology referrals. It often remains undiagnosed for a prolonged time,2,8,9 however, and many patients undergo nondiagnostic testing4 and nontherapeutic procedures1,2,7,8,10 as a result.11
In the pediatric population, SRS may be congenital and more complex due to deformed bone or cartilage.8 Little is known about SRS in adults, as there are only scant case reports in the literature.9,11 Previously described therapies have included: (1) reassurance, rest,1,6 and analgesic prescription; (2) intercostal nerve block; and (3) costal cartilage excision. Nonsurgical therapies are largely ineffective.4,5 The utility of costal cartilage excision has been reported in small numbers over the past century.2,5,8,10
We hypothesized that simple restoration of normal rib anatomy would alleviate the pain from SRS without sacrificing the normal function and protective structure of the rib cage. The primary aim of this study was to determine, using standardized outcome measures, if stabilization of the 10th costal insertion would effectively terminate the repetitive minor trauma to the 9th intercostal nerve that leads to intercostal neuralgia and SRS. A secondary objective was to describe an operative technique that is simple and easily reproducible by a range of surgical specialists.
Patients and Methods
Institutional review board approval was obtained for retrospective review of our 1-year case series conducted in 2019 at a university thoracic surgical practice; informed consent was waived. We clinically diagnosed SRS when (1) a palpable separation of at least 1 cm was noted at the anterior insertion of the 10th rib into the costal arch, (2) the 10th rib was unusually mobile on palpation, and (3) palpation at the separation point reproduced the patient’s pain.
Children were excluded from the study. No other exclusion criteria were applied. All adult patients confirmed with SRS completed the Örebro Musculoskeletal Pain Survey Questionnaire Short Form12 to establish a preoperative baseline perception of their own suffering caused by the syndrome. We offered all patients definitive repair, costal cartilage excision, or observation. No patients chose excision. Patients desiring repair underwent an operation devised and standardized by the first author, as follows (Video).
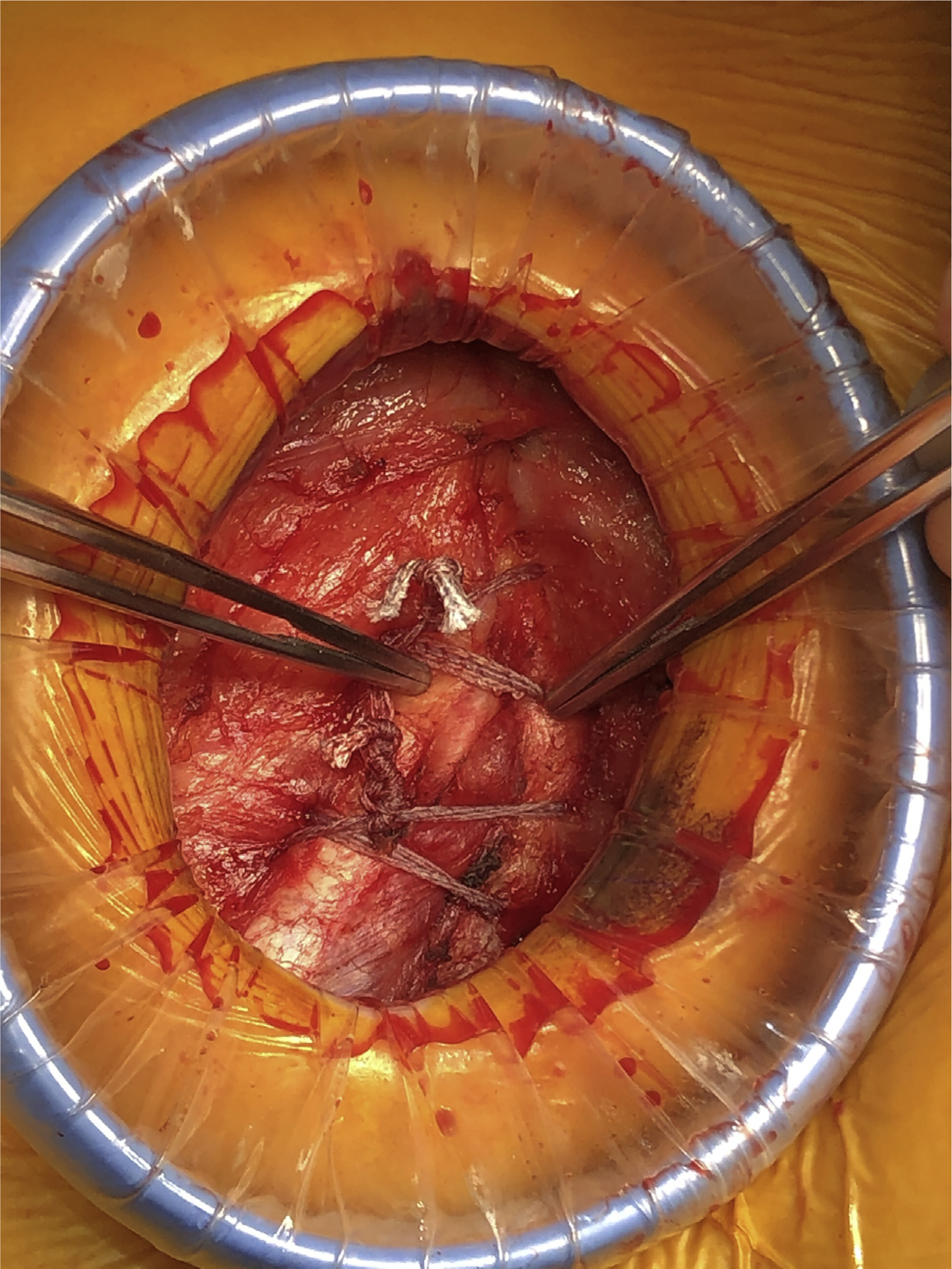
General anesthesia with single lumen endotracheal intubation is established. The patient is placed in a semilateral decubitus position with the operating table in the flat position, so as to maintain minimal space between ribs. Posterolateral intercostal blocks are injected in levels 7–11 using 5 mL of a 50/50 mixture of 0.5% plain bupivacaine and 1.3% liposomal bupivacaine (Exparel, Pacira Biosciences, Inc., Parsippany, NJ) at each level. A diagonal 3-cm incision is centered over the palpable separation point of the slipped rib from the common costal cartilage (Figure 1). External oblique muscle fibers are separated, not divided. The 10th rib tip is exposed by gently lifting the muscle and loose fascia away from the common cartilage for a few centimeters radially outward. A small wound protector (SurgiSleeve, Covidien, Dublin, Ireland) helps to lift and radially retract the soft tissues and expose the operative site through the small incision. Anatomy of the false ribs is inspected to confirm the diagnosis and determine whether there are multiple slipped ribs. Mild to moderate deformity of the slipped rib can be corrected because the cartilage is quite malleable (Figure 2). Orthopedic tape suture (TigerTape 2 mm x 76.2 cm; Arthrex, Naples, FL) is preferred, so as to widen the surface area of force applied to the fragile 10th rib and prevent suture pull-through. The suture is placed superior to, and skived around, the 9th rib to avoid penetration of the pleural space. The suture is drawn through the intercostal muscle just above the superior border of the 10th rib (Figure 3). The suture is then placed deep to the 10th rib and driven through its cartilaginous shaft. It is specifically not placed circumferentially around the rib, so as to avoid entrapment of the 10th intercostal nerve (Figure 4). Two separate figure-of-eight sutures are placed in like manner. Both sutures are tied simultaneously in order to distribute tension evenly along the length of the 10th rib (Figure 5). The external oblique muscle edges are closed, followed by closure of the subcutaneous fascia and skin. No thoracostomy tube is necessary. The patient is discharged the same day with scheduled oral nonsteroidal antiinflammatory drugs (NSAIDs) and a short course of oral narcotics. Our chosen analgesic regimen includes: (1) ketorolac 10 mg orally scheduled every 8 hours for 5 days, and (2) oxycodone 5 mg/acetaminophen 325 mg orally every 6 hours as needed, 30 tablets total.
Figure 1.
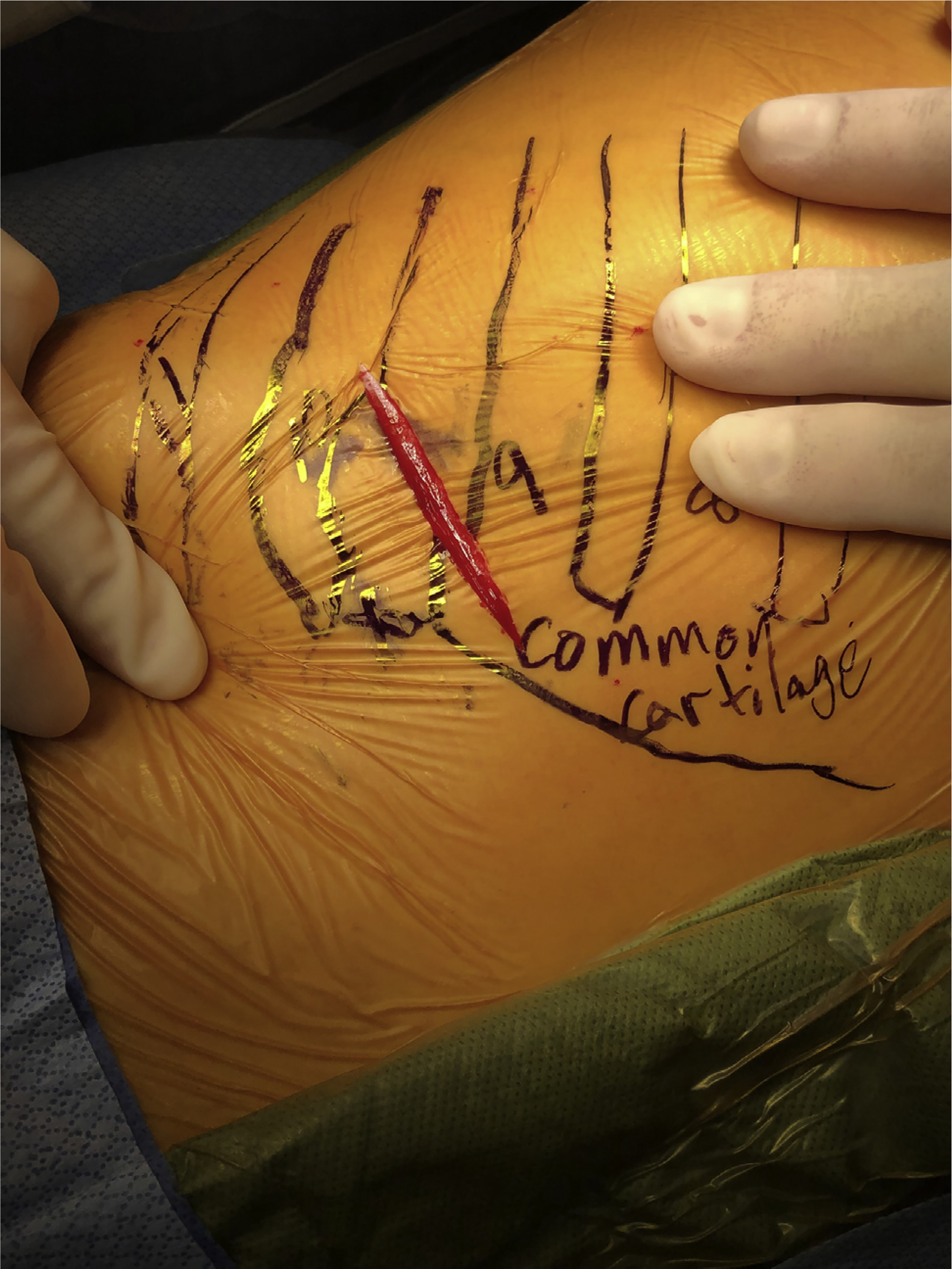
Surgical incision centered over slipped rib point of separation.
Figure 2.
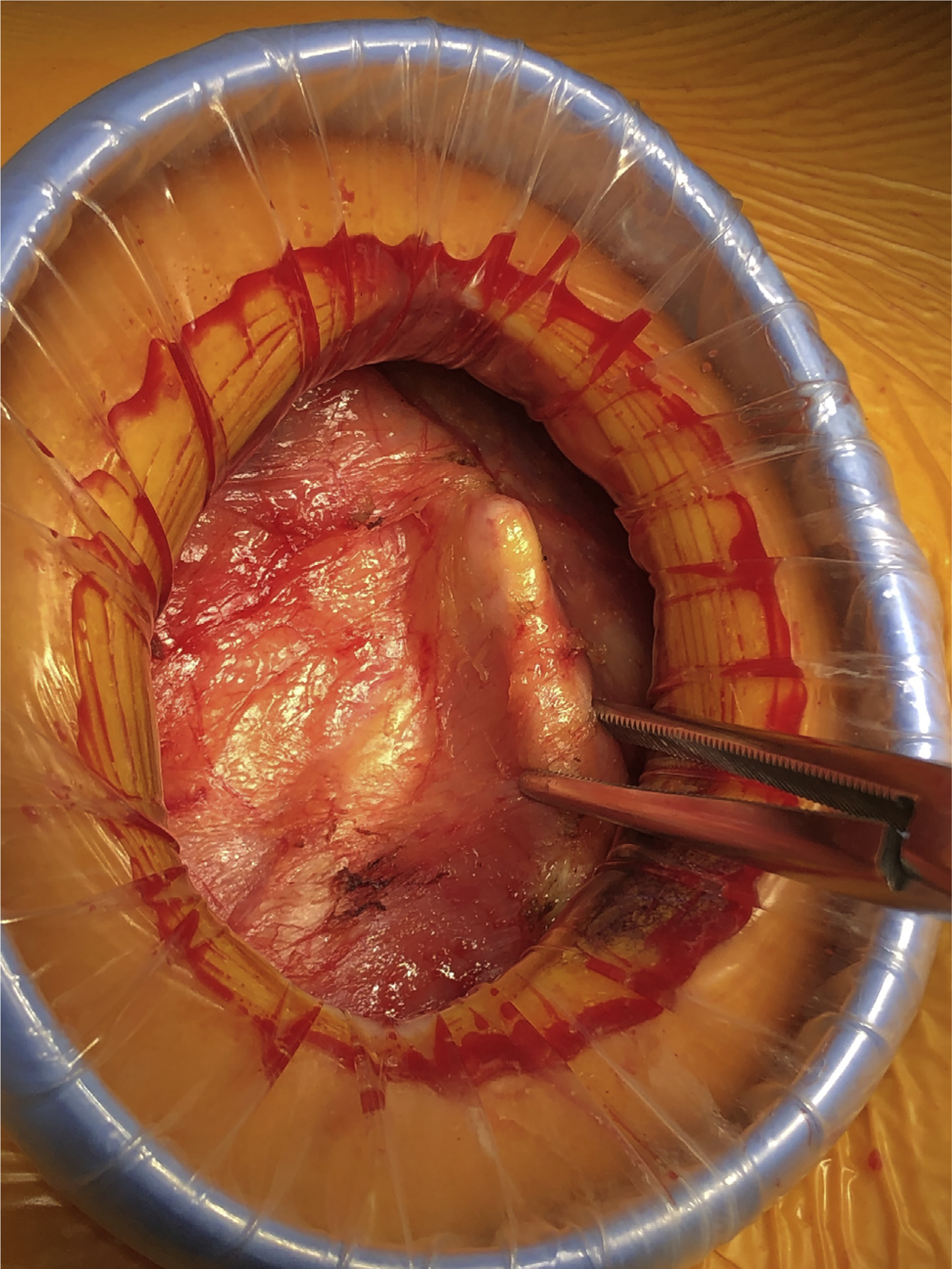
Slipped rib operative exposure.
Figure 3.
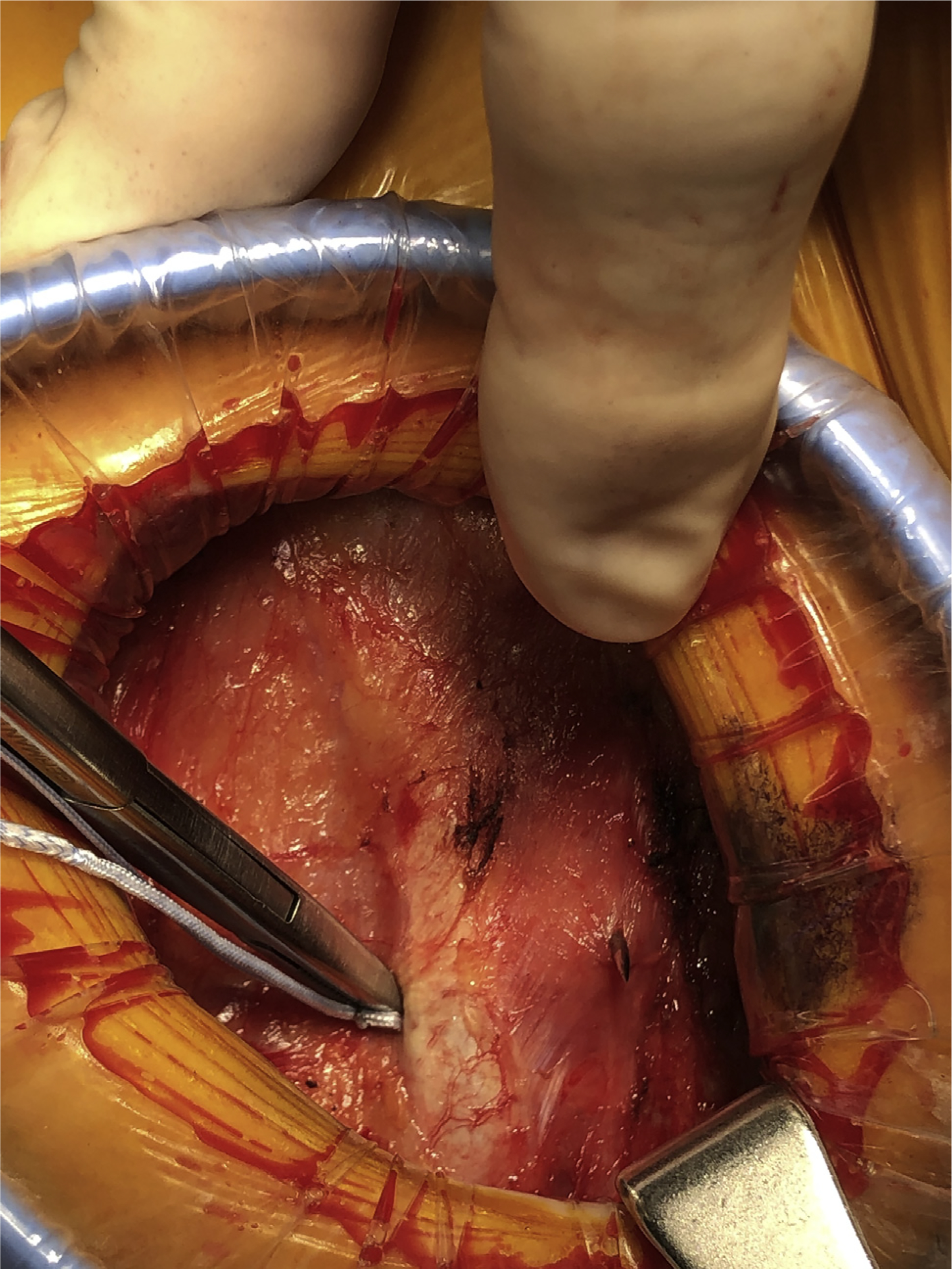
Suture placement around stable rib above slipped rib.
Figure 4.
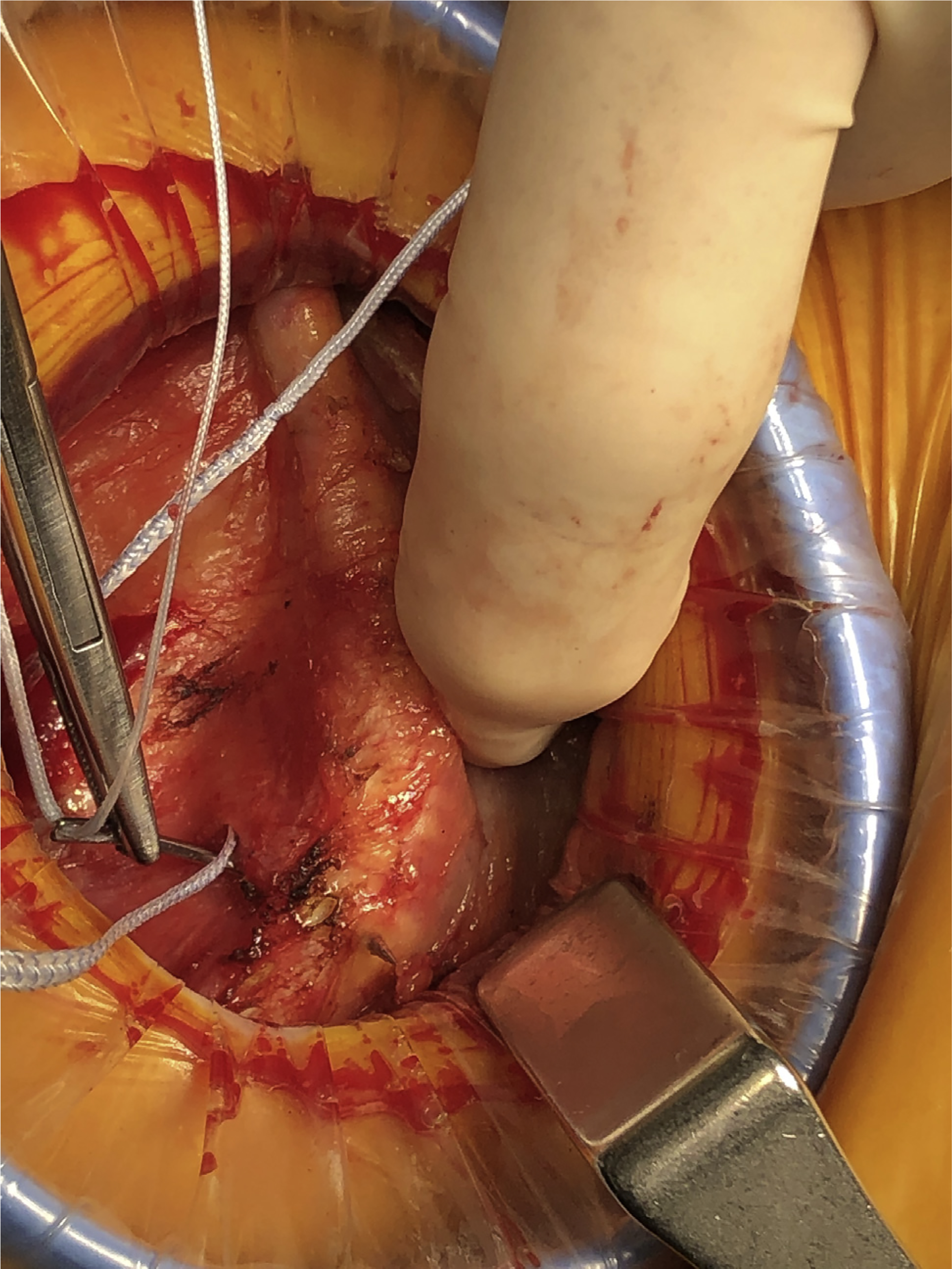
Suture placement directly through slipped rib.
Figure 5.
Completed slipped rib repair.
All patients who underwent repair were followed clinically at 1-week and 1-month intervals. Six-month interval was completed in 23 patients (79%). They completed the Örebro Musculoskeletal Pain Survey Questionnaire Short Form at each visit to evaluate the perceived effect of the procedure on the outcome measures listed in Table 1. Wilcoxon signed rank sum testing was used to compare postoperative results of each outcome measure with preoperative levels and determine statistically significant treatment effects. Use of neural modulating, narcotic, and NSAID medications was also compared pre- and postoperatively using McNemar’s test where applicable. We examined the operative site at each visit to confirm the durability of the repair.
Table 1.
Outcome Measures
| 0–10 Scale | Yes/No |
|---|---|
| Pain level in the past week | Current use of neural modulating medication(s) for pain |
| Current tension and anxiety levels | Current use of NSAID medication(s) |
| Current level of depression | Current use of narcotic pain medication(s) |
| Ability to do light work for 1 hour | |
| Ability to sleep | |
| Likelihood of return to usual duties in 3 months | |
| Worry that current pain will become permanent |
NSAID, nonsteroidal antiinflammatory drug.
Results
The diagnosis of SRS was made clinically in 42 patients. Median age was 50 years and SRS was disproportionately more common in women (86%). It was more common on the right side (62%). About one third (31%) recalled trauma to the area. Most had experienced a prolonged course (median, 18 months; range, 1–144 months) with multiple referrals to various specialists (median, 2 physicians) and non-diagnostic testing (median, 2 studies). Over one third (40%) had been subjected to at least 1 invasive testing modality or nontherapeutic surgical procedure. Eight (19%) had undergone laparoscopic cholecystectomy for the pain and experienced persistent or worsened pain afterwards. Three patients (7%) without SRS symptoms developed them immediately after laparoscopic cholecystectomy for acute cholecystitis. Symptoms began immediately after other laparoscopic surgery in 3 patients (7%). Most patients were taking either a neural modulating medication, NSAID analgesic, or narcotic pain medication at the time of diagnosis and many were on a combination of medications to treat the pain (Table 2). All of the observations were higher in the operative group, compared with the group that did not undergo repair. All patients were noted subjectively to be highly frustrated with their situations. Suicidal ideations because of the unrelenting pain were documented in one third (12 patients) and 3 had actually attempted suicide.
Table 2.
Pain Medication Use at Initial Consultation
| Pain Medication | Operative Group (n = 29) | Nonoperative Group (n = 13) |
|---|---|---|
| NSAIDs | 24 (83) | 7 (54) |
| Neural modulators | 14 (48) | 3 (23) |
| Narcotics | 8 (28) | 1 (8) |
Values are presented as n (%).
NSAID, nonsteroidal antiinflammatory drug.
Thirteen patients (31%) did not undergo repair. Unrelated lung cancer was diagnosed and treated in 2 patients, interfering with rib repair. Two patients declined repair when their medical insurance would not provide coverage for surgery. Nine patients opted to continue observation alone because they did not feel their symptoms were severe enough to warrant surgical repair or resection.
We performed the repair in 29 patients (69%). Clinical examination findings correlated with operative anatomical findings in 100% of patients, supporting our premise that the correct diagnosis can be made with history and physical examination alone. Immediate postoperative pain was variable and was not measured until 1 week postoperatively. No patients required additional prescription pain medication beyond the standard regimen. All patients reported feeling generally improved at 1 week, compared to preoperatively, with regard to their overall comfort and well being. One patient required hospital admission for 24 hours for pain control. No patients discharged the day of surgery required readmission. Three patients required a short hospital admission for reasons unrelated to their slipped rib repairs. All specific outcome measures steadily improved over time. Figures 6 and 7 demonstrate the median level of improvement in each specific outcome measured. At 1 and 6 month,s respectively, median pain decreased 75% and 80% (P < .001), ability to do light work increased 60% and 70% (P < .001), ability to sleep increased 60% and 75% (P < .001), tension and anxiety decreased 50% and 100% P < .001), depression decreased 80% and 100% (P < .001), worry about pain becoming permanent decreased 88% and 100% (P < .001), and outlook for return to normal duties within 3 months increased 75% and 89% (P < .001). Table 3 demonstrates the dramatic reduction of pain medication use after repair. The only complications observed were 2 minor skin reactions to topical skin adhesive (Exofin, Chemence Medical, Inc., Alpharetta, GA), and these resolved expectantly. No mortality was observed. All repairs maintained durable stability over the follow-up period and no revisions were required.
Figure 6.
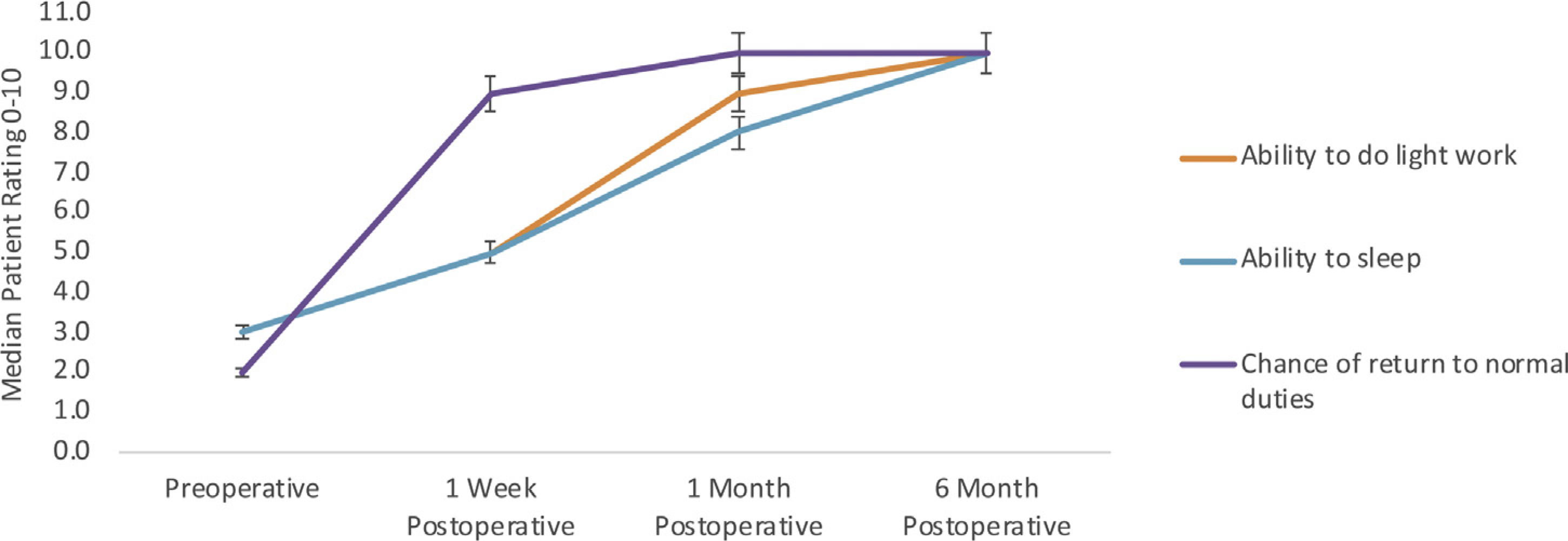
Increase in function after slipped rib repair (n = 29 at 1 week and 1 month. n = 23 at 6 months, P < .001 all outcome measures).
Figure 7.
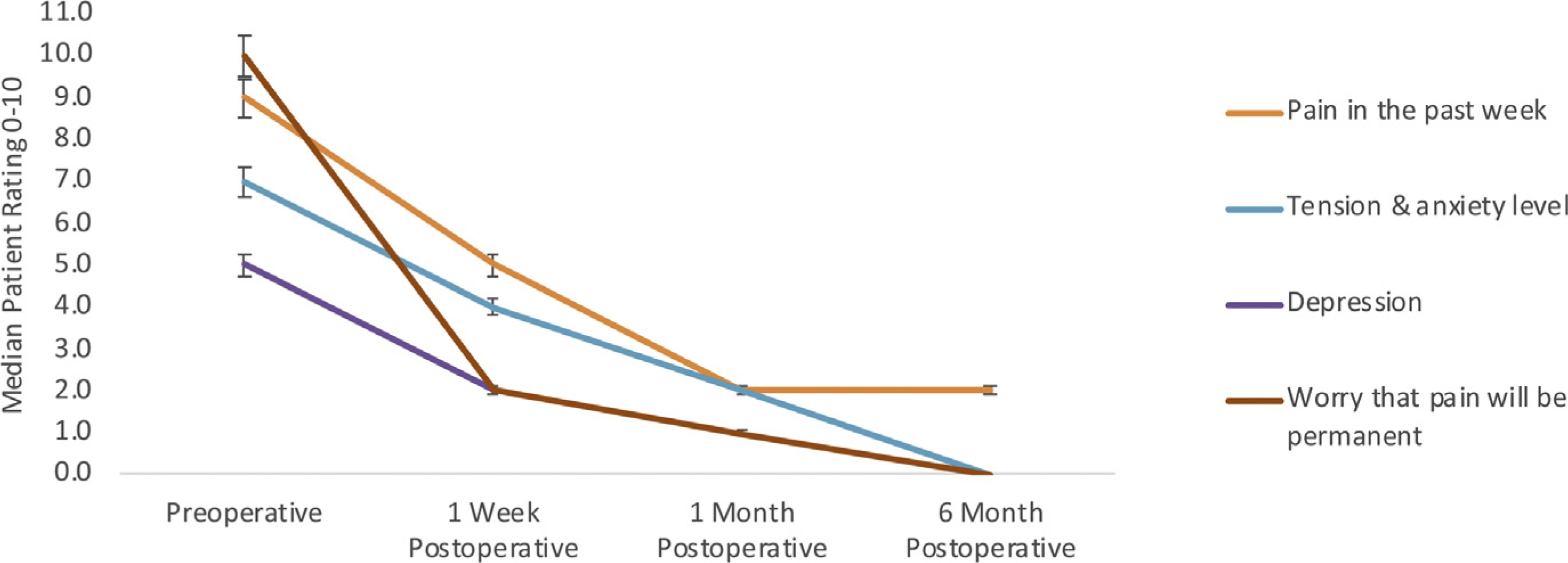
Decrease in disability after slipped rib repair (n = 29 at 1 week and 1 month. n = 23 at 6 months, P < .001 all outcome measures).
Table 3.
Number of Patients Using Pain Medications
| Pain Medication | Before repair (n = 29) | 1 month after repair (follow-up n = 29) | 6 months after repair (follow-up n = 23) |
|---|---|---|---|
| NSAIDs | 24 (83) | 2 (7) | 2 (9) |
| Neural modulators | 14 (48) | 2 (7) | 3 (13) |
| Narcotics | 8 (28) | 0 | 0 |
Values are presented as n (%).
NSAID, nonsteroidal antiinflammatory drug.
Comment
SRS is poorly understood by many medical providers.6,13 Few pediatric and surgical texts describe it in detail,4,7,8 and the medical literature is sparse. The collective experience of the patients in this series demonstrates the difficult and prolonged process of arriving at a correct diagnosis. Many patients sought care from multiple specialists and underwent multiple radiologic studies and invasive procedures unsuccessfully, without any significant pain relief. The diagnosis often took years to become apparent. Frequently, patients were given vague diagnoses such as chostochondritis and offered no treatment or referral to a surgeon with experience in the disorder.
Intercostal neuralgia caused by SRS can be severely painful and debilitating. Most patients in this series reported a significant reduction in their productivity and limitation in activities of daily living. One fourth of the patients in the series reported such severe pain and depression over failure to find relief that they had considered or attempted suicide. A significant number of patients were eventually prescribed neural modulating medications or muscle relaxants and narcotics, in addition to NSAIDs. In the current era of prescription drug abuse and overprescription, a simple, permanent solution to eliminate a common source of severe, chronic pain is highly desirable.
Timely recognition of SRS is likely the most important aspect of treatment.4 Diagnosis is simple and requires no imaging studies2,7 or invasive testing,5 although immediate pain relief and confirmation of a questionable diagnosis may be obtained with intercostal nerve injection.8,13 Most (76%) of the patients we diagnosed with SRS presented with prior imaging studies. We reviewed all available studies and found none that confirmed SRS. Previous authors14 have promoted use of the “hooking maneuver” to clinically diagnose SRS. We found it difficult to elicit the finding in all but very thin patients with extremely hypermobile slipped ribs. As previously reported,8 we discovered it to be exceedingly painful. We therefore abandoned the maneuver early on in our series. Alternatively, we propose the following clinical examination criteria be met for proper diagnosis: (1) a palpable separation of at least 1 cm at the anterior insertion of the 10th rib into the costal arch, (2) the 10th rib is unusually mobile on palpation,2 and (3) palpation at the separation point reproduces the patient’s pain.7
The standard surgical procedure reported in the literature, costal cartilage excision2,10 of up to 3 ribs,4,5,8 has disadvantages. First, it is a technically difficult procedure when performed correctly.5,8 Second, it is invasive and may be associated with painful recovery.5 Third, it usually involves resection of 2 to 3 rib cartilages. This removes normal protective and functional structures, rather than restoring anatomy to normal. Last, recurrence of pain and rib instability is reported to occur in about one fourth of patients.5 The entire premise of costal cartilage excision is debatable because, at least in the case of adults, the cartilage is typically normal. The separation of the cartilage tip is the actual problem. The cartilage is an “innocent bystander” that is sacrificed in order to stop constant aggravation and trauma to the intercostal nerve. Simple restoration of normal structure accomplishes the same ultimate goal with the benefit of retaining normal anatomy.
There are limitations to this study. Notably, children were excluded. Further study in a pediatric population may thus be necessary to draw conclusions about the utility of costal cartilage repair in children. Additionally, only relatively short-term follow-up data were analyzed. It is possible that recurrences or other complications may occur over a longer period of time. Third, this was a retrospective study. Patients were not randomized to repair vs excision or observation. Adequate follow-up of the nonoperative patients was not achieved, so no meaningful comparison between the 2 groups could be completed.
Our report demonstrates that, in adult patients, restoration of normal rib anatomy may eliminate the repetitive minor trauma to the affected intercostal nerve that leads to intercostal neuralgia and SRS. The data presented in our patient-reported subjective outcome measures in this study demonstrate a significant improvement in overall well being, return to function, and reduction of pain medication usage. The operation is simple, easily reproducible, and requires no costly hardware or prostheses. It does not cause any significant disfigurement to the patient. We conclude that, in appropriate adult patients, it is a useful alternative to costal cartilage excision that is well-tolerated and effective.
Supplementary Material
References
- 1.Wright J Slipping rib syndrome. Lancet. 1980;2:632–634. [DOI] [PubMed] [Google Scholar]
- 2.Copeland G, Machin D, Shennan J. Surgical treatment of the ‘slipping rib syndrome’. Br J Surg. 1984;71:522–523. [DOI] [PubMed] [Google Scholar]
- 3.Holmes J A study of the slipping-rib-cartilage syndrome. N Engl J Med. 1941;224:928–932. [Google Scholar]
- 4.Porter G Slipping rib syndrome: an infrequently recognized entity in children. A report of three cases and review of the literature. Pediatrics. 1985;76:810–813. [PubMed] [Google Scholar]
- 5.Gould J, Rentea R, Poola A, Aguayo P, St Peter S. The effectiveness of costal cartilage excision in children for slipping rib syndrome. J Pediatr Surg. 2016;51:2030–2032. [DOI] [PubMed] [Google Scholar]
- 6.Frada G The painful floating-rib syndrome. Minerva Med. 1975;66:2679–2689. [PubMed] [Google Scholar]
- 7.Scott E, Scott B. Painful rib syndrome: a review of 76 cases. Gut. 1993;34:1006–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fu R, Iqbal C, Jaroszewski D, St Peter S. Costal cartilage excision for the treatment of pediatric slipping rib syndrome. J Pediatr Surg. 2012;47:1825–1827. [DOI] [PubMed] [Google Scholar]
- 9.Loffeld R Painful rib syndrome: a cause of pain complaints that often goes unnoticed. Ned Tijdschr Geneeskd. 2002;146: 1813–1815. [PubMed] [Google Scholar]
- 10.Davies-Colley R Slipping rib. Br Med J. 1922;1:432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lum-Hee N, Abdulla AJ. Slipping rib syndrome: an over-looked cause of chest and abdominal pain. Int J Clin Pract. 1997;51:252–253. [PubMed] [Google Scholar]
- 12.Linton SJ, Nicholas M, MacDonald S. Development of a short form of the Örebro Musculoskeletal Pain Screening Questionnaire. Spine (Phila Pa 1976). 2011;36:1891–1895. [DOI] [PubMed] [Google Scholar]
- 13.Khan N, Waseem S, Ullah S, Mehmood H. Slipping rib syndrome in a female adult with longstanding intractable upper abdominal pain. Case Rep Med. 2018;2018:7484560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.GJ HI, DC Z. Slipping rib syndrome: diagnosis using the “hooking maneuver”. JAMA. 1977;237:794–795. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


