Abstract
BACKGROUND
Laparoscopic cholecystectomy (LC) combined with laparoscopic common bile duct (CBD) exploration (LCBDE) is one of the main treatments for choledocholithiasis with CBD diameter of larger than 10 mm. However, for patients with small CBD (CBD diameter ≤ 8 mm), endoscopic sphincterotomy remains the preferred treatment at present, but it also has some drawbacks associated with a series of complications, such as pancreatitis, hemorrhage, cholangitis, and duodenal perforation. To date, few studies have been reported that support the feasibility and safety of LCBDE for choledocholithiasis with small CBD.
AIM
To investigate the feasibility and safety of LCBDE for choledocholithiasis with small CBD.
METHODS
A total of 257 patients without acute cholangitis who underwent LC + LCBDE for cholecystolithiasis from January 2013 to December 2018 in one institution were reviewed. The clinical data were retrospectively collected and analyzed. According to whether the diameter of CBD was larger than 8 mm, 257 patients were divided into large CBD group (n = 146) and small CBD group (n = 111). Propensity score matching (1:1) was performed to adjust for clinical differences. The demographics, intraoperative data, short-term outcomes, and long-term follow-up outcomes for the patients were recorded and compared.
RESULTS
In total, 257 patients who underwent successful LC + LCBDE were enrolled in the study, 146 had large CBD and 111 had small CBD. The median follow-up period was 39 (14-86) mo. For small CBD patients, the median CBD diameter was 0.6 cm (0.2-2.0 cm), the mean operating time was 107.2 ± 28.3 min, and the postoperative bile leak rate, rate of residual CBD stones (CBDS), CBDS recurrence rate, and CBD stenosis rate were 5.41% (6/111), 3.60% (4/111), 1.80% (2/111), and 0% (0/111), respectively; the mean postoperative hospital stay was 7.4 ± 3.6 d. For large CBD patients, the median common bile duct diameter was 1.0 cm (0.3-3.0 cm), the mean operating time was 115.7 ± 32.0 min, and the postoperative bile leak rate, rate of residual CBDS, CBDS recurrence rate, and CBD stenosis rate were 5.41% (9/146), 1.37% (2/146), 6.85% (10/146), and 0% (0/146), respectively; the mean postoperative hospital stay was 7.7 ± 2.7 d. After propensity score matching, 184 patients remained, and all preoperative covariates except diameter of CBD stones were balanced. Postoperative bile leak occurred in 11 patients overall (5.98%), and no difference was found between the small CBD group (4.35%, 4/92) and the large CBD group (7.61%, 7/92). The incidence of CBDS recurrence did not differ significantly between the small CBD group (2.17%, 2/92) and the large CBD group (6.52%, 6/92).
CONCLUSION
LC + LCBDE is safe and feasible for choledocholithiasis patients with small CBD and did not increase the postoperative bile leak rate compared with chole-docholithiasis patients with large CBD.
Keywords: Common bile duct stones, Laparoscopic common bile duct exploration, Endoscopic sphincterotomy, Bile leak, Choledochal stenosis, Recurrence
Core Tip: Previous studies on laparoscopic common bile duct (CBD) exploration (LCBDE) in choledocholithiasis with small diameter have been limited. Although some studies have suggested that small CBD stone may be a significant risk factor for postoperative bile leak after LCBDE, the sample size of small CBD choledocholithiasis in these studies was relatively small. The goal of our study was to emphasize the safety and feasibility of LCBDE for choledocholithiasis with small CBD through large-sample analysis. The results showed that LCBDE for choledocholithiasis with small-diameter without acute cholangitis did not increase the postoperative biliary leak rate and the recurrence rate of CBD stones.
INTRODUCTION
Common bile duct (CBD) stones (CBDS) is a common condition of the biliary tree that can cause serious complications such as cholangitis, pancreatitis, and liver abscess. CBDS always requires surgical intervention, which primarily includes open choledochotomy, perioperative endoscopic sphincterotomy (EST), and laparoscopic CBD exploration (LCBDE)[1,2]. Many studies have shown that conventional open choledochotomy therapy for choledocholithiasis may lead to a wide range of adverse events and a long recovery time[3,4]. With the development of endoscopic technology, EST combined with laparoscopic cholecystectomy (LC) has been widely used as a less invasive treatment for choledocholithiasis. However, the sphincter of Oddi’s destroyed by sphincterotomy may result in refluxing of duodenal juice, which may in turn lead to recurrence of CBDS, recurrent episodes of cholangitis, and even biliary mali-gnancies[5-7]. Ding et al[8] confirmed that compared with LCBDE, EST + LC has a higher recurrence rate of CBDS. In addition, EST is also associated with a series of complications such as pancreatitis, bleeding, perforation, and even death[9,10]. Recently, many studies have confirmed that LCBDE is a safe and cost effective option for CBDS, but these studies mainly focused on the cases whose CBD was larger than 1.0 cm[11-13]. However, whether it is feasible or safe to undergo LCBDE for those with small CBD (CBD diameter ≤ 8 mm) still remains controversial, and few studies have reported to support the feasibility and safety of LCBDE for choledocholithiasis with small CBD[14,15]. In this retrospective study, we investigated the feasibility and safety of LCBDE for choledocholithiasis with small CBD.
MATERIALS AND METHODS
Patients
This was a retrospective study for 257 consecutive patients admitted to the Hepatobiliary and Pancreatic Surgery Department of Fujian Provincial Hospital who underwent LCBDE with primary CBD closure for choledocholithiasis during the 6-year period from January 2013 to December 2018. Preoperative computed tomography (CT) or magnetic resonance cholangiopancreatography (MRCP) examination was performed for all the patients to measure the most dilated part of the supraduodenal common bile duct. Based on whether the diameter of CBD was larger than 8 mm, 257 patients were divided into large CBD group (n = 146) and small CBD group (n = 111). All surgeries were performed by experienced chief physicians. This study was approved by the institutional review board of the Fujian Provincial Hospital. All patients were given written or verbal informed consent prior to study inclusion.
Inclusion criteria included: (1) Patients were diagnosed with cholecystolithiasis complicated with choledocholithiasis by CT or MRCP, and no intrahepatic bile duct stones were found; (2) Patients without obstructive jaundice, and serum bilirubin level was < 2 mg/dL; (3) Child-Pugh A or B; and (4) Cardiopulmonary system and other important organs functioned normally and were able to withstand surgical treatment.
Exclusion criteria included: (1) Previous EST or biliary surgery; (2) Patients with acute cholecystitis, cholangitis, or pancreatitis; (3) Patients with choledochal stenosis or Oddi sphincter dysfunction requiring choledochojejunostomy; and (4) Patients who underwent T-tube drainage during the surgery.
Patient data collection
Medical records were retrospectively reviewed in respect to age, gender, underlying disease, liver function tests, CT or MRCP, operating time, intraoperative blood loss, whether converted to laparotomy, the postoperative hospital stay, postoperative complications, stone clearance rate, stone recurrence, and choledochal stenosis. Postoperative complications were defined as those that occurred within the first 30 d after surgery. Bile leak was defined as bilirubin concentration in the drain fluid at least three times the serum bilirubin concentration on or after postoperative day 3 or as the need for radiologic or operative intervention resulting from biliary collections or bile peritonitis[16].
Surgical procedure
All procedures were performed by highly experienced laparoscopic biliary surgeons. Surgery was performed using a 4-trocars laparoscopic technique under general anesthesia. A 10-mm observation port was placed below the umbilical region, and a 12-mm main operating port was placed below the xiphoid process while two 5-mm operating ports were placed below the costal margin of the right midline clavicle and the costal margin of the right axillary front, respectively. Firstly, the gallbladder triangle was dissected, and the cystic artery and the cystic duct were clipped with Hem-o-lock, respectively, and then dislocated. The gallbladder was then dissociated and removed. A longitudinal incision of approximately 8-10 mm was cut along the anterior wall of the CBD. The flexible choledochoscope (Olympus, Tokyo, Japan) was inserted into CBD to explore the biliary tree including intrahepatic bile ducts and the distal CBD to confirm the number, size, and location of bile duct stones. The CBDS were extracted by a stone extractor (Olympus). For big stones, holmium laser lithotripsy was performed first to crush the stones, which were then extracted by a basket. After removing stones, choledochoscope was performed again to confirm the complete clearance of the stones. Finally, the incision in the anterior wall of the CBD was continuously sutured with 4-0 or 5-0 polydioxanone monofilament absorbable suture.
Follow-up
All patients were routinely assessed for complications after surgery in the outpatient clinic using routine blood tests, liver function tests, and ultrasound, and MRCP was performed if necessary. Follow-up was conducted at 1 wk, 3 mo, 6 mo, and 1 year postoperatively, followed by annual follow-up. The follow-up was performed until April 2019.
Statistical analysis
Propensity score matching (1:1) was designed to limit the influence of confounding factors when estimating treatment outcomes between the two groups. Statistical data were analyzed using the Statistic Package for Social Science 22.0 statistical software (Armonk, NY, United States). The continuous variables were expressed as means ± standard deviation or median (range), and the categorical variables were expressed using frequency distributions. Comparison of variables was carried out by chi-square test or Fisher exact test for categorical variables, and independent Student’s t-test for continuous variables. P < 0.05 was considered statistically significant.
RESULTS
Patient characteristics
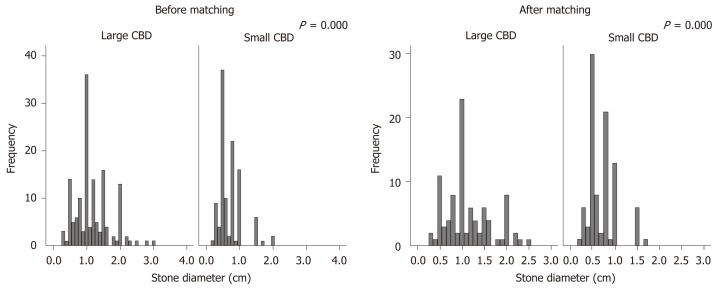
A total of 257 cases were enrolled, and patients’ characteristics, including baseline demographic data, clinical parameters, and underlying diseases, are shown in Table 1. There were 111 patients in the small CBD group (CBD diameter < 8 mm), including 50 males (45.05%) and 61 females (54.95%), with an average age of 57.6 ± 12.4 years. There were 146 patients in the large CBD group (CBD diameter ≥ 8mm), including 57 males (39.04%) and 89 females (60.96%), with an average age of 60.2 ± 14.6. The median common bile duct diameter was 0.6 cm (0.2-2.0 cm) in the small CBD group and 1.0 cm (0.3-3.0 cm) in the large CBD group (Figure 1). Additionally, the diameter of CBD stones, aspartate aminotransferase, and glutamyl transpeptidase varied between the small CBD group and the large CBD group, and this difference was statistically significant (P < 0.05). The two groups were similar in terms of the other evaluated preoperative biochemical parameters and underlying diseases (P > 0.05).
Table 1.
Baseline clinical characteristics of patients with common bile duct stones
|
|
Before matching, n = 257
|
After matching, n = 184
|
|||||
|
|
Large CBD, n = 146
|
Small CBD, n = 111
|
P
value
|
Large CBD, n = 92
|
Small CBD, n = 92
|
P
value
|
|
| Gender | Male | 57 | 50 | 0.333 | 34 | 37 | 0.650 |
| Female | 89 | 61 | 58 | 55 | |||
| Age in yr | 60.2 ± 14.6 | 57.6 ± 12.4 | 0.138 | 59.3 ± 15.3 | 57.7 ± 12.1 | 0.443 | |
| TBil in μmol/L | 13.6 (1.6-34.02) | 15.6 (4.1-33.7) | 0.227 | 12.7 (2.1-34.02) | 13.5 (4.15-33.7) | 0.39 | |
| ALT in U/L | 48.5 (7-609) | 43 (6-626) | 0.364 | 33 (7-609) | 51 (6-626) | 0.152 | |
| AST in U/L | 30 (10-881) | 23 (10-308) | 0.012 | 26 (10-486) | 24 (10-308.8) | 0.729 | |
| GTP in U/L | 265 (11-2135) | 171 (10-1539) | 0.037 | 101 (11-1240) | 186.5 (10-1539) | 0.076 | |
| Number of stone | Single | 52 | 40 | 0.945 | 34 | 32 | 0.759 |
| Multiple | 94 | 71 | 58 | 60 | |||
| Diameter of stones in cm | 1.0 (0.3-3.0) | 0.6 (0.2-2.0) | 0.000 | 1.0 (0.3-2.5) | 0.6 (0.2-1.7) | 0.000 | |
| Hypertension | No | 116 | 77 | 0.064 | 72 | 67 | 0.391 |
| Yes | 30 | 34 | 20 | 25 | |||
| Diabetes | No | 132 | 97 | 0.441 | 83 | 82 | 0.809 |
| Yes | 14 | 14 | 9 | 10 | |||
| Heart disease | No | 134 | 102 | 0.974 | 85 | 83 | 0.601 |
| Yes | 12 | 9 | 7 | 9 | |||
| Pulmonary disease | No | 144 | 107 | 0.449 | 90 | 90 | 1.000 |
| Yes | 2 | 4 | 2 | 2 | |||
| Cerebrovascular disease | No | 142 | 108 | 1.000 | 90 | 90 | 1.000 |
| Yes | 4 | 3 | 2 | 2 | |||
ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; CBD: Common bile duct; GTP: Glutamyl transpeptidase; TBil: Total bilirubin.
Figure 1.
Stone size of patients. CBD: Common bile duct.
Comparison of outcomes between the small and large CBD groups
To adjust for differences in baseline clinical characteristics between the small and large CBD groups, propensity score matching (1:1) was performed as shown in Table 1. All clinical variables that can affect the outcomes were adjusted and compared after propensity score matching.
Short-term outcomes: All surgeries were performed laparoscopically without conversion to laparotomy. The short-term follow-up results after propensity matching are summarized in Table 2. The mean operating time was 106.4 ± 27.7 min for the small CBD group and 114.7 ± 33.7 min for the large CBD group (P = 0.073). The amount of intraoperative blood loss in the small CBD group was 20 (5-200) mL, while that in the large CBD group was 20 (5-200) mL (P = 0.168). Four of 184 patients (2.17%) had residual stones, which were removed by EST after surgery. There was no significant difference in stone clearance rate (97.83% vs 97.83%, P = 1.000), postoperative hospital stay (7.3 ± 3.7 d vs 7.7 ± 2.7 d, P = 0.392), and postoperative bile leak (4.35% vs 7.61%, P = 0.351) between the small CBD and large CBD groups. All patients with postoperative bile leak in both groups recovered through conservative management with drainage.
Table 2.
Safety profile and procedure-related short-term outcomes of the small common bile duct and large common bile duct groups
|
|
|
Before matching, n = 257
|
After matching, n = 184
|
||||
|
|
|
Large CBD, n = 146
|
Small CBD, n = 111
|
P
value
|
Large CBD, n = 92
|
Small CBD, n = 92
|
P
value
|
| Operating time in min | 115.7 ± 32.0 | 107.2 ± 28.3 | 0.379 | 114.7 ± 33.7 | 106.4 ± 27.7 | 0.073 | |
| Intraoperative blood loss in mL | 20 (5-200) | 20 (5-200) | 0.028 | 20 (5-200) | 20 (5-200) | 0.168 | |
| Convert to laparotomy | No | 145 | 111 | 1.000 | 92 | 92 | |
| Yes | 1 | 0 | 0 | 0 | |||
| Successful stone clearance | No | 2 | 4 | 0.449 | 2 | 2 | 1.000 |
| Yes | 144 | 107 | 90 | 90 | |||
| Bile leakage | No | 137 | 105 | 0.797 | 85 | 88 | 0.351 |
| Yes | 9 | 6 | 7 | 4 | |||
| Bleeding | No | 145 | 111 | 1.000 | 91 | 92 | 1.000 |
| Yes | 1 | 0 | 1 | 0 | |||
| Abdominal infection | No | 138 | 106 | 0.724 | 85 | 88 | 0.351 |
| Yes | 8 | 5 | 7 | 4 | |||
| Pneumonia | No | 138 | 110 | 0.102 | 86 | 91 | 0.123 |
| Yes | 8 | 1 | 6 | 1 | |||
| Incision infection | No | 140 | 110 | 0.239 | 88 | 92 | 0.129 |
| Yes | 6 | 1 | 4 | 0 | |||
| Postoperative hospital stay in d | 7.7 ± 2.7 | 7.4 ± 3.6 | 0.406 | 7.7 ± 2.7 | 7.3 ± 3.7 | 0.392 | |
CBD: Common bile duct.
Long-term outcomes: The long-term follow-up results after propensity matching are summarized in Table 3. Recurrent CBDS occurred in a total of eight (4.35%) patients, among which five accepted EST to remove the recurrent CBDS, two underwent surgical treatment, and one refused any further treatment; no symptoms were observed during the follow-up period. There was no significant difference in the recurrence rate between the small CBD group (2.17%, 2/92) and the large group (6.52%, 6/92) (P = 0.278). No postoperative CBD stenosis case was observed in those patients.
Table 3.
Procedure-related long-term outcomes of the small common bile duct and large common bile duct groups
|
Before matching, n = 257
|
After matching, n = 184
|
||||||
|
|
Large CBD, n = 146
|
Small CBD, n = 111
|
P
value
|
Large CBD, n = 92
|
Small CBD, n = 92
|
P
value
|
|
| Choledochal Stenosis | No | 146 | 111 | 92 | 92 | ||
| Yes | 0 | 0 | 0 | 0 | |||
| Stone Recurrence | No | 136 | 109 | 0.057 | 86 | 90 | 0.278 |
| Yes | 10 | 2 | 6 | 2 | |||
CBD: Common bile duct.
DISCUSSION
This study showed that there was no significant difference in surgery outcome or postoperative complications between small and large CBD groups, which confirmed that LCBDE is feasible and safe for choledocholithiasis with small CBD.
Choledocholithiasis is one of the most common diseases in general surgery. With the improvement of living standards and the adjustment of diet structure, the incidence of choledocholithiasis increases year by year[17,18]. Currently, the preferred less invasive treatment is preoperative EST or LCBDE, which is recommended by the British Society of Gastroenterology[19]. However, EST is associated with a series of postoperative complications such as bleeding, pancreatitis, perforation, and even death. The overall postoperative complication rate of EST reached 5%-14%, and the mortality rate was 0.3%-2.3%[20-22]. Some studies[23,24] have shown that compared with two-stage perioperative EST and subsequent LC, single-stage LC + LCBDE can reduce the overall hospital stay and cost. Ding et al[8] indicated that the single-stage LC + LCBDE and two-stage preoperative EST followed by LC are equally effective in achieving initial CBDS clearance, but recurrent CBDS is more likely to occur in patients who had undergone two-stage treatment (9.47% vs 2.06%). This result may be due to the fact that EST disrupts the integrity of the Oddi sphincter, which will make it easier for the duodenal contents to reflux into the biliary system, leading to bacterial colonization and the subsequent CBDS formation. Although no high-level evidence indicated that EST will cause atypia or malignancy, EST has been demonstrated to cause reactive and proliferative changes in the CBD biliary epithelium[25].
T-tube drainage has been widely used in laparoscopic choledochotomy in order to decompress the biliary tree, reduce the complications such as bile leak and CBD stenosis, and provide an access for postoperative trans-T–tube tract choledochoscopy to detect any residual stones and removal them. However, T-tube drainage is associated with a postoperative complication rate of around 10.5%-20%, including fluid and electrolyte imbalance, accidental T-tube displacements, bile leak and wound cellulites around the T-tube, and bile peritonitis after T-tube removal[26,27]. An updated meta-analysis has shown that compared with primary CBD closure, planned T-tube insertion prolongs overall hospital stay and operating time without any evidence of benefit[28]. Thus, among patients undergoing laparoscopic choledochotomy for CBDS, T-tube drainage may not be necessary.
LCBDE can be carried out via the transductal approach or the transcystic approach, the latter is known as laparoscopic transcystic common bile duct exploration (LTCBDE). This approach protects the integrity of the CBD and avoids suture repair after choledochotomy, which is thought to be associated with lower morbidity compared to the transductal approach. A study from Tokumura et al[29] found only one bile leak in 91 patients (1%) with successful stone clearance using the transcystic approach. Another study from Waage et al[30] found one bile leak in 110 patients (0.9%) using the transcystic approach. However, it should be pointed out that their study did not indicate the diameter of the CBD. In fact, it is very difficult to perform LTCBDE in choledocholithiasis with small CBD. For those patients, cystic duct is always smaller than 3 mm, making it difficult for the 5 mm cholangioscope to pass through the cystic duct. Fang et al[31] successfully performed LTCBDE in 205 cases, but none of them was with small CBD. Thus, we believe that LTCBDE is safe and efficacious for the management of choledocholithiasis with large CBD but that it might not be appropriate for those with small CBD.
Although more and more studies have confirmed that LCBDE is a safe and cost effective option for choledocholithiasis, these studies mainly focused on cases whose CBD was larger than 1.0 cm[11-13]. Whether it is feasible or safe to undergo LCBDE for those with small CBD still remains controversial. The controversy mainly focuses on the difficulty of CBD suture and its complications. It was believed that LCBDE for small CBD is more likely to lead to postoperative bile leak and CBD stenosis.
Hua et al[32] showed that choledocholithiasis with a non-dilated CBD (CBD diameter < 8 mm) was more likely to suffer postoperative bile leak than those with dilated CBD (CBD diameter ≥ 8 mm) (22.2% vs 3.0%). However, it should be noted that in their studies, the sample size of small CBD choledocholithiasis was small (only nine cases). It was speculated that the reason for this result may be the lack of experience in LCBDE for choledocholithiasis with small CBD. Khaled et al[33] reported that there was a learning curve with the procedure of LCBDE, and the risk of bile leak was reduced with growing experience of the surgeon as the rate of bile leak was decreased from 3.5% (2/57) in the first 5 years to 1.5% (1/68) in the subsequent 5 years (the average CBD diameter was 9.4 mm). In our opinion, appropriate patient selection is essential to avoid postoperative bile leak for choledocholithiasis with small CBD. In patients with small CBD, inflammatory edema of the CBD wall is more likely to cause difficulty in suture if complicated with acute cholangitis, and it will cause relaxation of the suture when the inflammatory edema subsides after surgery. All of these causes would increase the risk of postoperative bile leak. In this study, all surgeries were performed by highly experienced general surgeons with a wealth of laparoscopic suture techniques, and those patients with acute cholangitis were excluded to reduce the effect of CBD wall edema. The overall postoperative bile leak rate was 5.8% in this study, which was comparable to that of 3.8%-11.3% reported by others[34-37]. Besides, the bile leak rate was found to be 5.4% in patients with small CBD, which was not significantly different from those with large CBD (6.2%), and this is comparable to the bile leak rates of 5.8%-8.1% in patients with CBD ≥ 10 mm as reported previously[35,38]. Thus, it was believed that it is safe and feasible for small CBD patients to perform LCBDE and that it will not increase the risk of postoperative bile leak as long as appropriate cases are selected.
Hua et al[32] found that CBDS clearance is a significant risk factor for bile leak. With residual stones, intraluminal pressure in the bile duct will increase, and bile fluid will leak from the suturing site. Lauter et al[39] reported that 11 of 71 patients (15.5%) had residual stones after LCBDE. However, in our series, the rate of residual stones was 2.3%, which is lower than that in previously published series. This may be due to the development of choledochoscopy technology with optical magnification, direct visualization, and clearer vision. Besides, repeated confirmation before closing the CBD also increased the clearance rate of CBDS.
As for postoperative choledochal stenosis, no evidence has shown that LCBDE with primary closure would increase the risk of choledochal stenosis, even in small CBD patients. Cai et al[40] showed that no postoperative choledochal stenosis was found in 223 patients with a median follow-up of 26 mo, including 137 patients of primary closure and 102 patients of T-tube drainage. Khaled et al[33] reported postoperative choledochal stenosis was found in one of 120 patients (0.8%), with primary closure following LCBDE with a median follow-up of 39.2 mo (mean CBD diameter was 9.4 mm). In this study, no postoperative choledochal stenosis was found in either the small CBD group or the large CBD group with a mean follow-up period of 39 mo. Postoperative choledochal stenosis after LCBDE seems to occur rarely regardless of the CBD diameter. These results revealed that the primary closure after LCBDE can be performed without increasing the risk of postoperative choledochal stenosis in patients with small CBD.
This study also has its limitations. Although the effects of confounding factors were adjusted by performing propensity score matching, due to its retrospective nature, there may be selection bias between the two groups. Additional randomized controlled trials are needed to validate further these findings.
CONCLUSION
In summary, primary CBD closure following LCBDE + LC is a safe and effective approach for the management of choledocholithiasis with small CBD, as long as appropriate cases are selected, and does not increase the short-term or long-term complications compared with choledocholithiasis with large CBD.
ARTICLE HIGHLIGHTS
Research background
Laparoscopic common bile duct (CBD) exploration (LCBDE) combined with cholecystectomy (LC) is a common therapeutic modality for the management of CBD stones (CBDS). Over time, LCBDE + LC is mainly performed for choledocholithiasis with CBD diameter of larger than 10 mm. However, it remains unclear whether LCBDE is feasible or safe for those with small CBD (CBD diameter ≤ 8 mm).
Research motivation
Some clinical practitioners have argued that LCBDE for small CBD may be more likely to lead to postoperative bile leak and CBD stenosis. We wanted to investigate these issues to help guide clinicians in efforts to improve management of CBDS, especially for those with small CBD.
Research objectives
The retrospective study is aimed to compare the clinical outcomes of large CBD group vs small CBD group to investigate the feasibility and safety of LCBDE for choledocholithiasis with small CBD.
Research methods
This study includes 257 patients with cholecystolithiasis who met the criteria. The short-term and long-term clinical outcomes were compared between the large CBD group and the small CBD group. Propensity score matching (1:1) was performed to adjust for the effects of confounding factors.
Research results
There was no significant difference in operating time, intraoperative blood loss, conversion to laparotomy, and rate of residual CBDS between large CBD group and small CBD group. LCBDE for small CBD would not increase the risk of postoperative bile leak and CBD stenosis compared with large CBD.
Research conclusions
Primary CBD closure following LCBDE + LC is a safe and effective approach to the management of choledocholithiasis with small CBD, as long as appropriate cases are selected, and does not increase the short-term or long-term complications compared with choledocholithiasis with large CBD.
Research perspectives
LCBDE + LC can be performed safely for choledocholithiasis with small CBD without increasing the risk of postoperative bile leak and CBD stenosis. Additional randomized controlled trials are needed to validate further these findings.
ACKNOWLEDGEMENTS
We are grateful to all the participants and colleagues for their contributions.
Footnotes
Institutional review board statement: This study was approved by the institutional review board of the Fujian Provincial Hospital
Informed consent statement: All involved persons provided written or verbal informed consent prior to study inclusion.
Conflict-of-interest statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Manuscript source: Unsolicited manuscript
Peer-review started: December 5, 2020
First decision: December 21, 2020
Article in press: January 26, 2021
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aktekin A, Ruiz-Jasbon F S-Editor: Zhang L L-Editor: Filipodia P-Editor: Zhang YL
Contributor Information
Xiao-Xiao Huang, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Jia-Yi Wu, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Yan-Nan Bai, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Jun-Yi Wu, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Jia-Hui Lv, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Wei-Zhao Chen, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Li-Ming Huang, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Rong-Fa Huang, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China.
Mao-Lin Yan, Department of Hepatobiliary and Pancreatic Surgery, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou 350001, Fujian Province, China. yanmaolin74@163.com.
Data sharing statement
Technical appendix, statistical code, and dataset available from the corresponding author at yanmaolin74@163.com.
References
- 1.Pitt HA. Role of open choledochotomy in the treatment of choledocholithiasis. Am J Surg. 1993;165:483–486. doi: 10.1016/s0002-9610(05)80946-8. [DOI] [PubMed] [Google Scholar]
- 2.Hanif F, Ahmed Z, Samie MA, Nassar AH. Laparoscopic transcystic bile duct exploration: the treatment of first choice for common bile duct stones. Surg Endosc. 2010;24:1552–1556. doi: 10.1007/s00464-009-0809-4. [DOI] [PubMed] [Google Scholar]
- 3.Zhu QD, Tao CL, Zhou MT, Yu ZP, Shi HQ, Zhang QY. Primary closure vs T-tube drainage after common bile duct exploration for choledocholithiasis. Langenbecks Arch Surg. 2011;396:53–62. doi: 10.1007/s00423-010-0660-z. [DOI] [PubMed] [Google Scholar]
- 4.Tham TC, Carr-Locke DL, Collins JS. Endoscopic sphincterotomy in the young patient: is there cause for concern? Gut. 1997;40:697–700. doi: 10.1136/gut.40.6.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Natsui M, Saito Y, Abe S, Iwanaga A, Ikarashi S, Nozawa Y, Nakadaira H. Long-term outcomes of endoscopic papillary balloon dilation and endoscopic sphincterotomy for bile duct stones. Dig Endosc. 2013;25:313–321. doi: 10.1111/j.1443-1661.2012.01393.x. [DOI] [PubMed] [Google Scholar]
- 6.Li T, Wen J, Bie L, Gong B. Comparison of the Long-Term Outcomes of Endoscopic Papillary Large Balloon Dilation Alone vs Endoscopic Sphincterotomy for Removal of Bile Duct Stones. Gastroenterol Res Pract. 2018;2018:6430701. doi: 10.1155/2018/6430701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, Saisho H. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52:116–121. doi: 10.1136/gut.52.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ding G, Cai W, Qin M. Single-stage vs. two-stage management for concomitant gallstones and common bile duct stones: a prospective randomized trial with long-term follow-up. J Gastrointest Surg. 2014;18:947–951. doi: 10.1007/s11605-014-2467-7. [DOI] [PubMed] [Google Scholar]
- 9.Zhao ZH, Hu LH, Ren HB, Zhao AJ, Qian YY, Sun XT, Su S, Zhu SG, Yu J, Zou WB, Guo XR, Wang L, Li ZS, Liao Z. Incidence and risk factors for post-ERCP pancreatitis in chronic pancreatitis. Gastrointest Endosc 2017; 86: 519-524. :e1. doi: 10.1016/j.gie.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 10.Lyu Y, Cheng Y, Wang B, Xu Y, Du W. What is impact of nonsteroidal anti-inflammatory drugs in the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2018;18:106. doi: 10.1186/s12876-018-0837-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu X, Huang ZJ, Zhong JY, Ran YH, Ma ML, Zhang HW. Laparoscopic common bile duct exploration with primary closure is safe for management of choledocholithiasis in elderly patients. Hepatobiliary Pancreat Dis Int. 2019;18:557–561. doi: 10.1016/j.hbpd.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Salama AF, Abd Ellatif ME, Abd Elaziz H, Magdy A, Rizk H, Basheer M, Jamal W, Dawoud I, El Nakeeb A. Preliminary experience with laparoscopic common bile duct exploration. BMC Surg. 2017;17:32. doi: 10.1186/s12893-017-0225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu WS, Zou Y, Yang B, Jiang Y, Sun DL. Laparoscopic Exploration Can Salvage Recurrent Common Bile Duct Stone after Cholecystectomy. Am Surg. 2017;83:1343–1346. [PubMed] [Google Scholar]
- 14.Chen AP, Zhao C, Chen DF, Wang SM, Xiao H, Wen YQ. Laparoscopic choledocholithotomy for thin choledochus. Zhongguo Shiyong Waike Zazhi . 2005;25:673–674. [Google Scholar]
- 15.Peng J, Ma JL, Hao JH, Lan H. Laparoscopic common bile duct exploration with primary closure for the treatment of small-diameter choledocholithiasis. Gandanyi Waike Zazhi . 2015;27:519–520. [Google Scholar]
- 16.Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–688. doi: 10.1016/j.surg.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Tazuma S, Unno M, Igarashi Y, Inui K, Uchiyama K, Kai M, Tsuyuguchi T, Maguchi H, Mori T, Yamaguchi K, Ryozawa S, Nimura Y, Fujita N, Kubota K, Shoda J, Tabata M, Mine T, Sugano K, Watanabe M, Shimosegawa T. Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol. 2017;52:276–300. doi: 10.1007/s00535-016-1289-7. [DOI] [PubMed] [Google Scholar]
- 18.Helton WS, Ayloo S. Technical Aspects of Bile Duct Evaluation and Exploration: An Update. Surg Clin North Am. 2019;99:259–282. doi: 10.1016/j.suc.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 19.Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T. Updated guideline on the management of common bile duct stones (CBDS) Gut. 2017;66:765–782. doi: 10.1136/gutjnl-2016-312317. [DOI] [PubMed] [Google Scholar]
- 20.Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, Diamond T, Taylor MA. Surgical vs endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2013:CD003327. doi: 10.1002/14651858.CD003327.pub3. [DOI] [PubMed] [Google Scholar]
- 21.Costi R, Gnocchi A, Di Mario F, Sarli L. Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol. 2014;20:13382–13401. doi: 10.3748/wjg.v20.i37.13382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feng Y, Zhu H, Chen X, Xu S, Cheng W, Ni J, Shi R. Comparison of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for retrieval of choledocholithiasis: a meta-analysis of randomized controlled trials. J Gastroenterol. 2012;47:655–663. doi: 10.1007/s00535-012-0528-9. [DOI] [PubMed] [Google Scholar]
- 23.Zhu HY, Xu M, Shen HJ, Yang C, Li F, Li KW, Shi WJ, Ji F. A meta-analysis of single-stage vs two-stage management for concomitant gallstones and common bile duct stones. Clin Res Hepatol Gastroenterol. 2015;39:584–593. doi: 10.1016/j.clinre.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 24.Mattila A, Mrena J, Kellokumpu I. Cost-analysis and effectiveness of one-stage laparoscopic vs two-stage endolaparoscopic management of cholecystocholedocholithiasis: a retrospective cohort study. BMC Surg. 2017;17:79. doi: 10.1186/s12893-017-0274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalaitzis J, Vezakis A, Fragulidis G, Anagnostopoulou I, Rizos S, Papalambros E, Polydorou A. Effects of endoscopic sphincterotomy on biliary epithelium: a case-control study. World J Gastroenterol. 2012;18:794–799. doi: 10.3748/wjg.v18.i8.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cuschieri A, Croce E, Faggioni A, Jakimowicz J, Lacy A, Lezoche E, Morino M, Ribeiro VM, Toouli J, Visa J, Wayand W. EAES ductal stone study. Preliminary findings of multi-center prospective randomized trial comparing two-stage vs single-stage management. Surg Endosc. 1996;10:1130–1135. doi: 10.1007/s004649900264. [DOI] [PubMed] [Google Scholar]
- 27.Martin IJ, Bailey IS, Rhodes M, O'Rourke N, Nathanson L, Fielding G. Towards T-tube free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg. 1998;228:29–34. doi: 10.1097/00000658-199807000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gurusamy KS, Koti R, Davidson BR. T-tube drainage vs primary closure after laparoscopic common bile duct exploration. Cochrane Database Syst Rev. :2013: CD005641. doi: 10.1002/14651858.CD005640.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tokumura H, Umezawa A, Cao H, Sakamoto N, Imaoka Y, Ouchi A, Yamamoto K. Laparoscopic management of common bile duct stones: transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg. 2002;9:206–212. doi: 10.1007/s005340200020. [DOI] [PubMed] [Google Scholar]
- 30.Waage A, Strömberg C, Leijonmarck CE, Arvidsson D. Long-term results from laparoscopic common bile duct exploration. Surg Endosc. 2003;17:1181–1185. doi: 10.1007/s00464-002-8937-0. [DOI] [PubMed] [Google Scholar]
- 31.Fang L, Wang J, Dai WC, Liang B, Chen HM, Fu XW, Zheng BB, Lei J, Huang CW, Zou SB. Laparoscopic transcystic common bile duct exploration: surgical indications and procedure strategies. Surg Endosc. 2018;32:4742–4748. doi: 10.1007/s00464-018-6195-z. [DOI] [PubMed] [Google Scholar]
- 32.Hua J, Meng H, Yao L, Gong J, Xu B, Yang T, Sun W, Wang Y, Mao Y, Zhang T, Zhou B, Song Z. Five hundred consecutive laparoscopic common bile duct explorations: 5-year experience at a single institution. Surg Endosc. 2017;31:3581–3589. doi: 10.1007/s00464-016-5388-6. [DOI] [PubMed] [Google Scholar]
- 33.Khaled YS, Malde DJ, de Souza C, Kalia A, Ammori BJ. Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis. Surg Endosc. 2013;27:4164–4170. doi: 10.1007/s00464-013-3015-3. [DOI] [PubMed] [Google Scholar]
- 34.Hua J, Lin S, Qian D, He Z, Zhang T, Song Z. Primary closure and rate of bile leak following laparoscopic common bile duct exploration via choledochotomy. Dig Surg. 2015;32:1–8. doi: 10.1159/000368326. [DOI] [PubMed] [Google Scholar]
- 35.Liu D, Cao F, Liu J, Xu D, Wang Y, Li F. Risk factors for bile leakage after primary closure following laparoscopic common bile duct exploration: a retrospective cohort study. BMC Surg. 2017;17:1. doi: 10.1186/s12893-016-0201-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.He MY, Zhou XD, Chen H, Zheng P, Zhang FZ, Ren WW. Various approaches of laparoscopic common bile duct exploration plus primary duct closure for choledocholithiasis: A systematic review and meta-analysis. Hepatobiliary Pancreat Dis Int. 2018;17:183–191. doi: 10.1016/j.hbpd.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 37.Yin Z, Xu K, Sun J, Zhang J, Xiao Z, Wang J, Niu H, Zhao Q, Lin S, Li Y. Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? Ann Surg. 2013;257:54–66. doi: 10.1097/SLA.0b013e318268314b. [DOI] [PubMed] [Google Scholar]
- 38.Wen SQ, Hu QH, Wan M, Tai S, Xie XY, Wu Q, Yang SL, Liao GQ. Appropriate Patient Selection Is Essential for the Success of Primary Closure After Laparoscopic Common Bile Duct Exploration. Dig Dis Sci. 2017;62:1321–1326. doi: 10.1007/s10620-017-4507-0. [DOI] [PubMed] [Google Scholar]
- 39.Lauter DM, Froines EJ. Laparoscopic common duct exploration in the management of choledocholithiasis. Am J Surg. 2000;179:372–374. doi: 10.1016/s0002-9610(00)00368-8. [DOI] [PubMed] [Google Scholar]
- 40.Cai H, Sun D, Sun Y, Bai J, Zhao H, Miao Y. Primary closure following laparoscopic common bile duct exploration combined with intraoperative cholangiography and choledochoscopy. World J Surg. 2012;36:164–170. doi: 10.1007/s00268-011-1346-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Technical appendix, statistical code, and dataset available from the corresponding author at yanmaolin74@163.com.