To the Editor:
With the introduction of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for the COVID-19 pandemic, the healthcare system was forced to make a significant number of changes in a short period of time. Many of these changes revolved around optimization of safety for professionals who work with patient's upper airways or are directly involved in aerosolizing procedures [[1], [2], [3], [4]]. While the infectivity of the virus and multiple guidelines surrounding the management of patients with the disease have been well established in the literature, the impact these changes have had on the delivery of quality care is not as widely studied. We aimed to determine the impact the pandemic has had on the delivery of quality perioperative medical care, specifically in terms of airway management, at our own institution.
Approval for this study was granted by the West Virginia University Institutional Review Board (IRB #2004966952). Chart review was performed on patients who underwent surgery with general anesthesia requiring intubation with an endotracheal tube at our academic level one trauma center in the first two weeks of April 2019 and April 2020. We assessed multiple variables including lowest oxygen saturation, lowest systolic and diastolic blood pressures, mode of laryngoscopy, number of intubation attempts, case delay in minutes, time from arrival in the operating room (OR) to induction in minutes, time from arrival in the operating room to intubation in minutes, and time from the end of the procedure to extubation in minutes. Patients excluded from this study were pediatric and obstetric patients, as well as those who were intubated prior to arriving in the operating room. Standard deviations (SD) were assessed and t-tests were calculated to compare averages of variables between the two groups with a p-value of 0.05 defining statistical significance in our study.
Within our cohort, 273 patients who underwent surgery in the study period were reviewed with 122 meeting inclusion criteria. 64 patients from April 2019 were included and 58 patients from April 2020 were included.
In 2019, the average number of minutes for case delay was 13.5, compared to 40.9 in 2020 (p < 0.001). OR to induction time in 2019 was 6 min compared to 23 in 2020 (p = 0.025). OR to intubation time in 2019 was 10 min compared to 28 in 2020 (p = 0.031). Lastly, the time between the end of the procedure and extubation in 2019 was 4 min compared to 5 in 2020 (p = 0.062; Fig. 1 ).
Fig. 1.
Perioperative time differences between April 2019 and 2020. Time values are represented in minutes. Standard deviation is represented by error bars. Associated p-values are listed above associated variables.
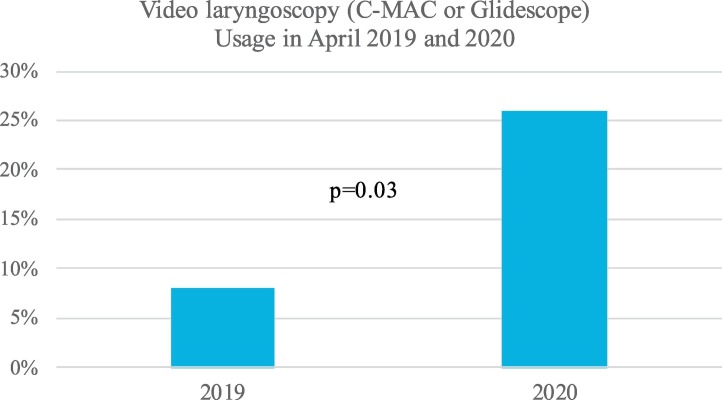
The usage of video laryngoscopy is also shown (Fig. 2 ) as being used in 8% of cases in our cohort in 2019 versus 26% of cases in 2020 (p = 0.03). The average lowest oxygen saturations recorded for the cases within the cohort were 92.7% in 2019 compared to 94.5% in 2020 (p = 0.03).
Fig. 2.
Usage of Video laryngoscopy (C-MAC or Glidescope) differences between April 2019 and 2020. Incidence of usage amongst the cohorts is illustrated. Associated p-value is listed above variables.
An explanation to describe the significant changes in case delay times may surround protective measures introduced during this time, leading to extended length of cases on average in order to minimize potential exposure of providers to COVID-19. Examples of additional precautions include setting up barriers between the anesthesia team and the rest of the operating room prior to inducing anesthesia and intubating, putting on additional protective gear, and adding protective coverings to the C-MACs used for intubation.
The amount of time between patients being brought into the operating room and successful induction and intubation were increased significantly. Given the increased usage of C-MAC in 2020, it is reasonable to surmise that the availability of C-MAC equipment and additional set up time may have contributed to this finding.
One variable that was increased in a positive manner in the 2020 group was the maintenance of higher average oxygen saturations. Although the mechanism behind this is unclear, we postulate that perhaps the more frequent use of CMAC for intubation led to increased maintenance of oxygen saturations. Another possibility which was not examined during this analysis is the attempt made to minimize number of providers in cases in the 2020 time period, particularly when COVID status was still pending and/or highly probably for a positive result. Limiting the number of handoffs and changes of staff during a procedure could contribute to better knowledge of patient history and limit changes in anesthetic management.
The unprecedented and unpredictable nature of the pandemic coupled with the need for quick data collection made a prospective study less feasible. The retrospective nature and small data sets for both time periods are limitations of this study.
While this correspondence illustrates a limited amount of data in a relatively small cohort, we believe it is suggestive of the impacts that institutional adoption of COVID-19 safety protocols in the perioperative period may have. Within this letter, we demonstrate that the safety protocols put in place secondary to the pandemic have led to significant changes in case delay time, OR to induction and intubation times, oxygen saturations, and usage of video laryngoscopy. We, as providers, should be cognizant of changes in practice made at national, institutional, and potentially even personal levels, and should be diligent in looking for ways to maintain our standards of care while adapting to the changes and challenges we face in the light of an ongoing novel viral pandemic.
Acknowledgments
Acknowledgments
We would like to thank and acknowledge the entire operating room staff at West Virginia University Hospitals during this trying time. We would also like to thank Taylor Shackleford, MD, for his help with calculating statistics.
Data availability
Data sets available from the corresponding author upon reasonable request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None.
References
- 1.Ruskin K.J., Ruskin A.C., Musselman B.T., Harvey J.R., Nesthus T.E., O’Connor M. COVID-19, personal protective equipment, and human performance. Anesthesiology. 2021;15 doi: 10.1097/aln.0000000000003684. Published online January. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Balas M., Al-Balas H.I., Al-Balas H. Surgery during the COVID-19 pandemic: a comprehensive overview and perioperative care. Am J Surg. 2020;219(6):903–906. doi: 10.1016/j.amjsurg.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Jabir A., Kerwan A., Nicola M., et al. Impact of the coronavirus (COVID-19) pandemic on surgical practice - part 1. Int J Surg. 2020;79:168–179. doi: 10.1016/j.ijsu.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng H., Hébert H.L., Chatziperi A., et al. Perioperative management of patients with suspected or confirmed COVID-19: review and recommendations for perioperative management from a retrospective cohort study. Br J Anaesth. 2020;125(6):895–911. doi: 10.1016/j.bja.2020.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sets available from the corresponding author upon reasonable request.