Abstract
Background
Inguinal hernia repair is the most common general surgery procedure and can be performed under local or general anesthesia. We hypothesized that using local rather than general anesthesia would improve outcomes, especially for older adults.
Methods
This is a retrospective review of 97,437 patients in the Veterans Affairs Surgical Quality Improvement Program who had open inguinal hernia surgery under local or general anesthesia. Outcomes included 30-day postoperative complications, operative time, and recovery time.
Results
Our cohort included 22,333 (23%) Veterans who received local and 75,104 (77%) who received general anesthesia. Mean age was 62 years. Local anesthesia was associated with a 37% decrease in the odds of postoperative complications (95% CI 0.54–0.73), a 13% decrease in operative time (95% CI 17.5–7.5), and a 27% shorter recovery room stay (95% CI 27.5–25.5), regardless of age.
Conclusions
Using local rather than general anesthesia is associated with a profound decrease in complications (equivalent to “de-aging” patients by 30 years) and could significantly reduce costs for this common procedure.
Keywords: Elderly, Inguinal hernia, Veterans, Local anesthesia, General anesthesia
ARTICLE SUMMARY
We found that using local rather than general anesthesia for inguinal hernia surgery was associated with significantly fewer complications and less time in the operating room and post-anesthesia care units, regardless of patient age. The importance of this finding is the potential reduction in postoperative morbidity, mortality, and costs for the most common general surgery procedure performed in the US.
INTRODUCTION
Exposing older adults to general anesthesia may increase their risk of developing short- and long-term cognitive and physical decline.1–3 Although the evidence linking general anesthesia to poor outcomes is not conclusive, the American College of Surgeons and the American Geriatrics Society recently recommended that surgeons explore alternatives to general anesthesia for common operations in older adults.4
Inguinal hernia repair is the most common general surgery procedure performed in the US, with over 800,000 operations annually.5 Individuals aged 65 years and older are 40–90% more likely to develop hernias than their younger counterparts, and older adults are expected to comprise ~20% of the US population in the near future.6, 7 Although inguinal hernia surgery can be performed under either local or general anesthesia, ~80% of inguinal hernias in the US are repaired using general anesthesia.8, 9 It is unclear whether the existing evidence supports a benefit for general over local anesthesia, especially in older adults.
Randomized studies performed in Europe comparing recovery after inguinal hernia surgery under local versus general anesthesia have yielded conflicting results. Nordin et al. demonstrated that using local anesthesia reduced morbidity by 29%, unplanned admissions by 19%, and operative time and costs by 15%.10, 11 By contrast, O’Dwyer et al. did not find any significant differences in morbidity and only a small improvement in costs.12 However, both studies primarily recruited younger and healthier patients and did not specifically compare outcomes in older adults, which is the population most likely to benefit from having surgery under local anesthesia. Additionally, no observational studies have adequately evaluated the benefits of local over general anesthesia in older adults. The largest US study was limited to a small subset of hospitals, did not examine results for older adults, involved only four years of data, and was unable to adjust for hospital effects that significantly inflate the risk of Type 1 error.8 Consequently, there is a substantial gap in literature on selection of anesthesia modality for inguinal hernia repair in the US, especially for older adults.
The purpose of this study was to assess whether the potential benefits of local versus general anesthesia differ in older versus younger adults. We hypothesized that patients ≥65 years old would derive the most benefit from having surgery under local anesthesia, but that all age groups would have superior peri- and postoperative outcomes with local compared to general anesthesia.
MATERIALS & METHODS
Setting
We analyzed patients in the Veterans Affairs Surgical Quality Improvement Program (VASQIP) who had inguinal hernia surgery from 1998–2018 after obtaining approval from the VA North Texas Health System IRB. VASQIP is a prospectively maintained database of a representative sample of all operations performed in the Veterans Affairs health system. The database captures preoperative co-morbidity, time in the operating room and postoperative anesthesia care unit, and postoperative complications. Methods for data collection and quality control in VASQIP have been previously published.13
Inclusion criteria
We included all Veterans aged 18 years and older who had elective, unilateral, open inguinal hernia repair under local or general anesthesia during the study period, based on the primary operation Common Procedure Terminology code of 49505. We included both inpatient and ambulatory cases.
Exclusion criteria
We excluded Veterans who had concurrent procedures, other procedures not consistent with inguinal hernia repair, bilateral hernias (by procedure or diagnosis codes), primary diagnosis other than unilateral inguinal hernia, preoperative ventilator dependence, or if the primary surgeon specialty was not general surgery. We also excluded patients who received spinal, epidural, or other anesthesia modalities.
Outcomes
Primary outcome
Our primary outcome was the rate of postoperative complications within 30 days of surgery. Complications captured by VASQIP include wound infection, dehiscence, pneumonia, re-intubation, pulmonary embolus, failure to wean from the ventilator, renal insufficiency/failure, urinary tract infection, stroke, cardiac arrest, myocardial infarction, postoperative bleeding that requires transfusion, deep vein thrombosis, sepsis/septic shock, and reoperation. All complications were defined according to VASQIP guidelines, which can be viewed at the following website: (http://vaww.vhadataportal.med.va.gov/Portals/0/VASQIP_Non-Cardiac_Variable_Definitions.pdf).
Secondary outcomes
Secondary outcomes included total operating room time (difference between the time patients exit and enter the operating room) and time spent in the post-anesthesia care unit (PACU).
Independent variable
The primary exposure of interest was the use of local or general anesthesia for inguinal hernia surgery. We also explored potential interactions between anesthesia modality and patient age.
Statistical analysis
For univariable analysis, we used the likelihood ratio chi-square to compare proportions and the Mann-Whitney U test for continuous variables. To control for known confounding and account for clustering within hospitals, we used generalized estimating equations with an exchangeable correlation matrix for binary outcomes and hierarchical linear regression for continuous outcomes, with hospitals allowed to have random intercepts. Variables included as potential confounders for anesthesia type and age are shown in Table 1. For each model, we tested functional forms for continuous variables and ran standard residual diagnostics to assess model fit and influence. We also tested interactions between anesthesia modality and comorbidities (COPD/Dyspnea, congestive heart failure, diabetes, and stroke, etc.) to determine whether the benefits of local anesthesia varied within particular subgroups of older patients. Since none of these effects were significant, the findings presented below represent outcomes for the entire cohort. Continuous dependent variables were transformed to natural logarithms to normalize their distribution and satisfy the assumptions of the hierarchical linear models. Consequently, results are expressed as semi-elasticities (percent change in the dependent variable with a unit change in the independent variable).
Table 1.
Characteristics of patients having inguinal hernia repair under local or general anesthesia.
| General anesthesia | Local anesthesia | p-value | |
|---|---|---|---|
| N = 75,104 | N = 22,333 | ||
| Age, median (IQR) | 62 (16) | 66 (17) | <0.0001 |
| Male gender | 74,711 (99.5%) | 22,240 (99.6%) | 0.04 |
| Race & ethnicity | <0.0001 | ||
| White | 46,835 (62.4%) | 15,009 (67.2%) | |
| Black | 11,791 (15.7%) | 2,353 (10.5%) | |
| Hispanic | 2,248 (3.0%) | 530 (2.4%) | |
| Other | 548 (0.7%) | 152 (0.7%) | |
| Unknown | 13,682 (18.2%) | 4,289 (19.2%) | |
| American Society of Anesthesiologists class | <0.0001 | ||
| 1 | 3,832 (5.1%) | 1,059 (4.7%) | |
| 2 | 33,592 (44.7%) | 9,303 (41.7%) | |
| 3+ | 37,677 (50.2%) | 11,968 (53.6) | |
| Post graduate year (PGY) of surgeon | <0.0001 | ||
| Attending | 32,284 (43.0%) | 12,273 (55.0%) | |
| Intern | 9,658 (12.9%) | 3,674 (16.5%) | |
| Second year | 9,859 (13.1%) | 1,893 (8.5%) | |
| Third year | 7,926 (10.6%) | 1,759 (7.9%) | |
| Fourth year | 4,379 (5.8%) | 729 (3.3%) | |
| Chief resident | 9,883 (13.2%) | 1,793 (8.0%) | |
| Post graduate year>5 | 1,115 (1.5%) | 212 (1.0%) | |
| Wound class | 0.002 | ||
| Clean | 72,743 (97.0%) | 21,720 (97.0%) | |
| Clean/contaminated, contaminated, or infected | 2,361 (3.0%) | 613 (3.0%) | |
| Diabetes | <0.0001 | ||
| None/diet controlled | 67,621 (90.0%) | 20,143 (90.2%) | |
| Oral medications | 5,357 (7.1%) | 1,465 (6.6%) | |
| Insulin | 1,819 (2.4%) | 557 (2.5%) | |
| Dyspnea | <0.0001 | ||
| None | 69,825 (93.0%) | 19,941 (89.3%) | |
| Minimal exertion | 4,843 (6.5%) | 2,121 (9.5%) | |
| At rest | 203 (0.3%) | 138 (0.6%) | |
| Alcohol use | 6,617 (8.8%) | 1,794 (8.0%) | <0.0001 |
| Functional status | <0.0001 | ||
| Independent | 73,881 (98.4%) | 21,713 (97.2%) | |
| Partially/totally dependent | 1,168 (1.6%) | 610 (2.7%) | |
| Active smoker | 25,833 (34.4%) | 6,686 (29.9%) | <0.0001 |
| History of congestive heart failure | 1,799 (2.4%) | 587 (2.6%) | <0.0001 |
| History of stroke with deficit | 1,408 (1.9%) | 590 (2.6%) | <0.0001 |
| History of stroke without deficit | 1,491 (2.0%) | 558 (2.5%) | <0.0001 |
| History of hemiplegia | 695 (0.9%) | 275 (1.2%) | <0.0001 |
| History of temporary ischemic attack | 1,410 (1.9%) | 534 (2.4%) | <0.0001 |
| History of bleeding disorder | 1,882 (2.5%) | 538 (2.4%) | <0.0001 |
| History of disseminated cancer | 188 (0.3%) | 109 (0.5%) | <0.0001 |
| History of steroid use | 704 (0.9%) | 356 (1.6%) | <0.0001 |
| History of 10% weight loss | 569 (0.8%) | 243 (1.1%) | <0.0001 |
| History of chronic obstructive pulmonary disease | 6,497 (8.7%) | 2,674 (12.0%) | <0.0001 |
| History of dialysis | 352 (0.5%) | 108 (0.5%) | <0.0001 |
| Outcomes | |||
| Operating room time (minutes), median (IQR) | 105 (46) | 89 (40) | <0.0001 |
| Post-anesthesia care unit time (minutes), median (IQR) | 75 (45) | 60 (42) | <0.0001 |
| Any postoperative complication | 971 (1.3%) | 224 (1.0%) | <0.0001 |
|
17 (0.02%) | 1 (0.0%) | 0.08 |
|
35 (0.05%) | 11 (0.05%) | 0.9 |
|
19 (0.03%) | 10 (0.04%) | 0.1 |
|
48 (0.06%) | 17 (0.08%) | 0.5 |
|
18 (0.02%) | 1 (0.0%) | 0.07 |
|
6 (0.01%) | 1 (0.0%) | 0.6 |
|
15 (0.02%) | 1 (0.0%) | 0.1 |
|
5 (0.01%) | 2 (0.01%) | 0.7 |
|
41 (0.05%) | 13 (0.06%) | 0.8 |
|
2 (0.0%) | 1 (0.0%) | 0.7 |
|
55 (0.07%) | 11 (0.05%) | 0.2 |
|
86 (0.1%) | 27 (0.1%) | 0.8 |
|
62 (0.08%) | 5 (0.02%) | 0.003 |
|
40 (0.05%) | 10 (0.04%) | 0.6 |
|
796 (1.1%) | 257 (1.2%) | 0.2 |
|
293 (0.4%) | 73 (0.3%) | 0.2 |
|
284 (0.4%) | 43 (0.2%) | <0.0001 |
|
49 (0.07%) | 19 (0.09%) | 0.3 |
To address bias from endogeneity in hierarchical models, we additionally employed an instrumental variable approach for continuous outcomes and a related two-stage residual inclusion model with bootstrapped standard errors for categorical outcomes.14 Based on previous work, our instrument for predicting use of local anesthesia was the proportion of cases performed at each hospital that were done under local.15 To verify that the instrument was sufficiently strong for prediction we examined correlation between the instrument and our independent variable, and we applied the tests of Stock and Yogo that compare the F statistic from each model to different levels of relative bias.16 For our models, the F statistic was sufficient to tolerate a range of 5%-30% relative bias, indicating that we had chosen a strong instrument. As an additional check on instrument performance, we also compared balance of patient characteristics above and below the median level of our instrument (data not shown).
Differences were considered significant if p<0.05, and all analysis was done using Stata version 15.1 (StataCorp. 2017. Stata Statistical Software: Release 15.1 College Station, TX: StataCorp LLC.).
RESULTS
Patient characteristics
We evaluated 97,437 Veterans who had open inguinal hernia repair from 1998–2018, and 22,333 (23%) of the surgeries were performed under local anesthesia. Table 1 shows that Veterans having hernia surgery under local rather than general anesthesia were older (median age 66 vs 62) and more likely to be Caucasian than African American or Hispanic. As expected for a VA population, the number of women having inguinal hernia repair was low (<1%) for each anesthesia modality.
Local anesthesia is associated with fewer postoperative complications for all ages
As shown in Table 1, Veterans who received local anesthesia were less likely to have a postoperative complication compared to those that received general anesthesia (1.0% vs 1.3%, p<0.0001). Table 1 also shows differences according to individual complications captured by VASQIP.
After adjusting for age, functional status, comorbidity, and the other factors in Table 1, using local rather than general anesthesia for inguinal hernia repair was associated with a 37% decrease in the odds of having postoperative complications (OR 0.63, 95% CI 0.54–0.73). By contrast, each year increase in age was associated with a small but significant increase in the odds of complications (OR 1.02, 95% CI 1.01–1.02). There was no significant interaction between age and use of local anesthesia, indicating that the benefits of local are consistent across age groups. Indeed, as shown in Figure 1A, the complication rate for a patient having surgery under local anesthesia was equivalent to a similar general anesthesia patient who was 30 years younger. In other words, the complication rate for a 90-year-old local anesthesia patient was the same as a 60-year-old general anesthesia patient.
Figure 1.
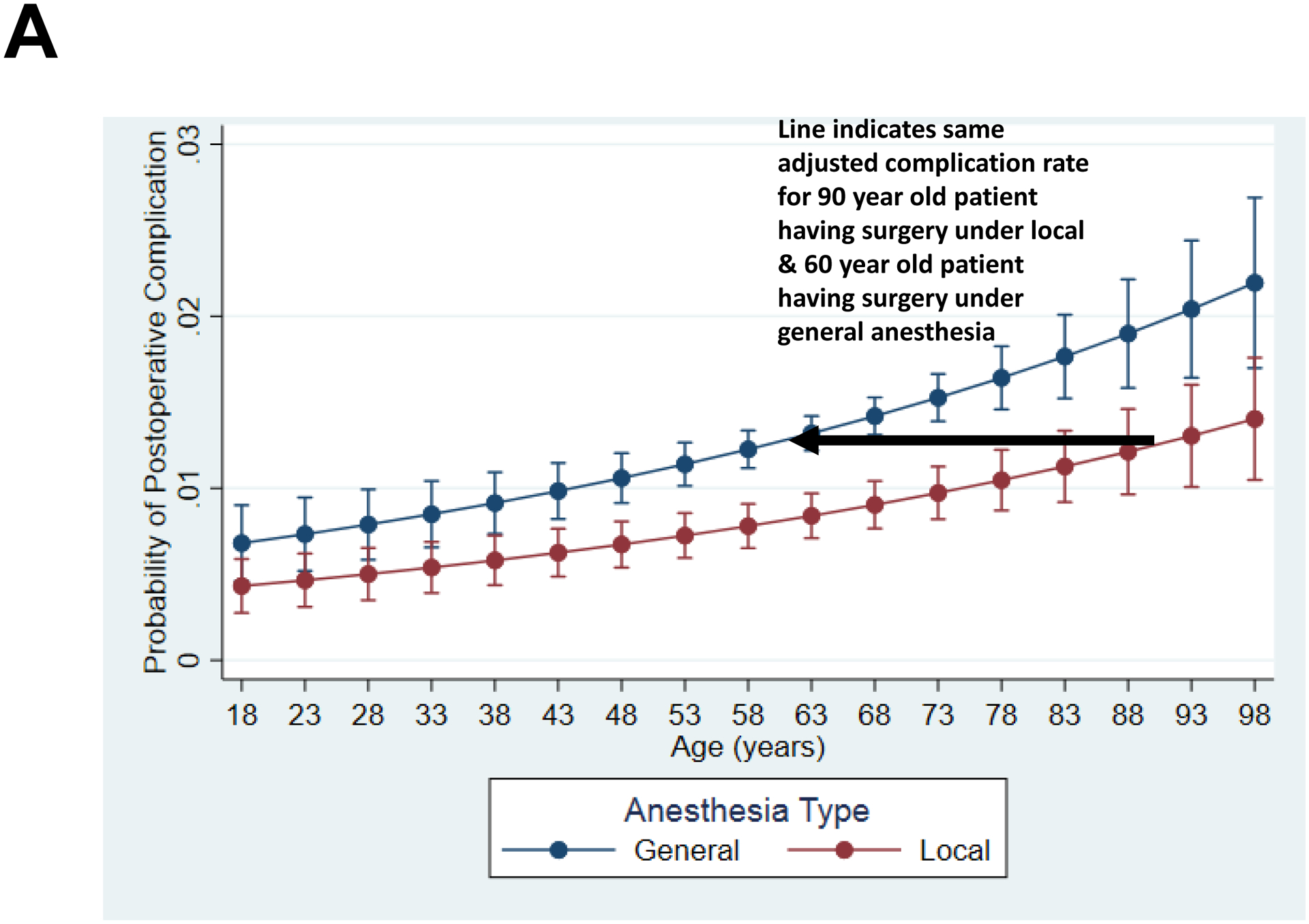
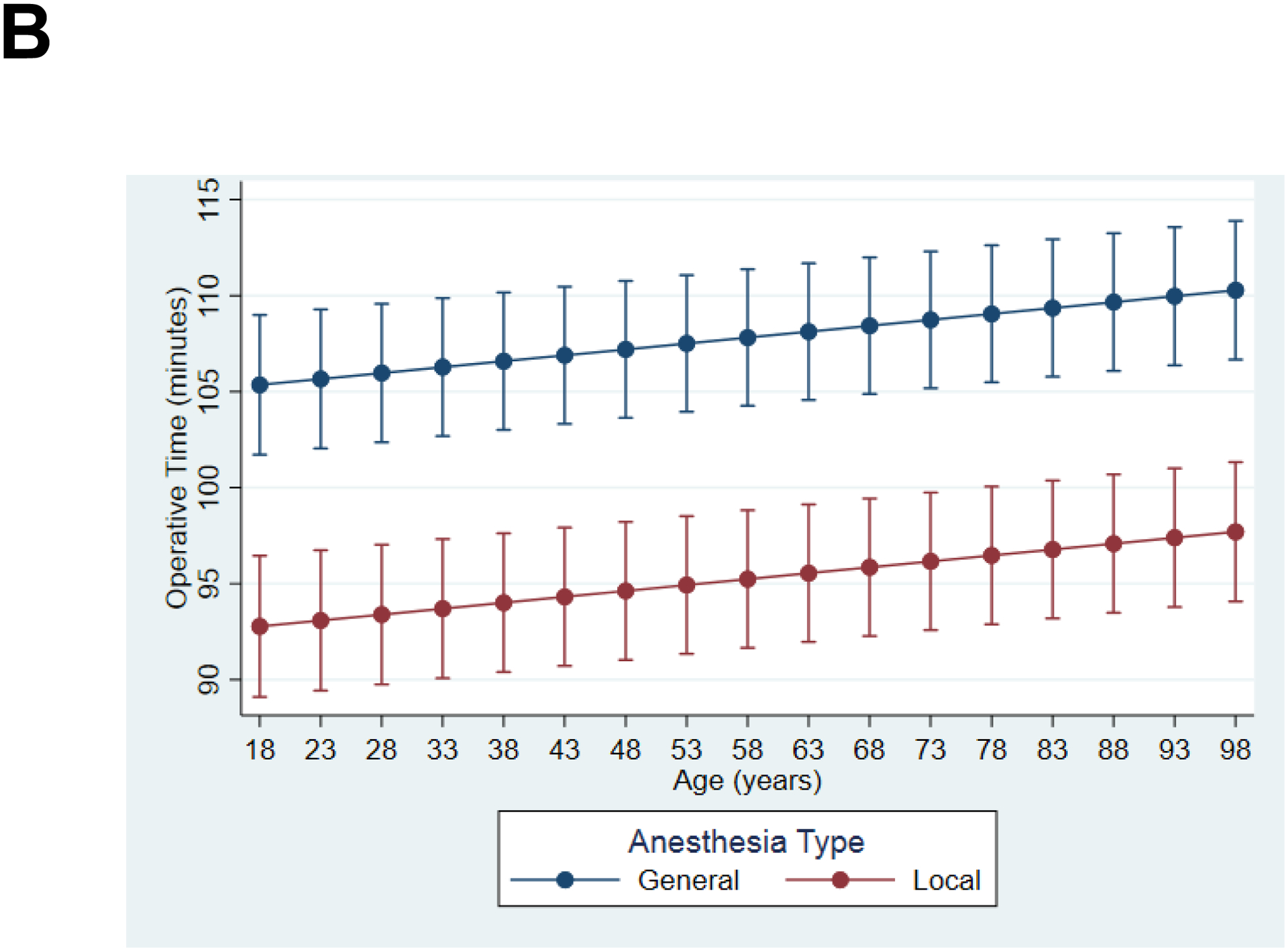
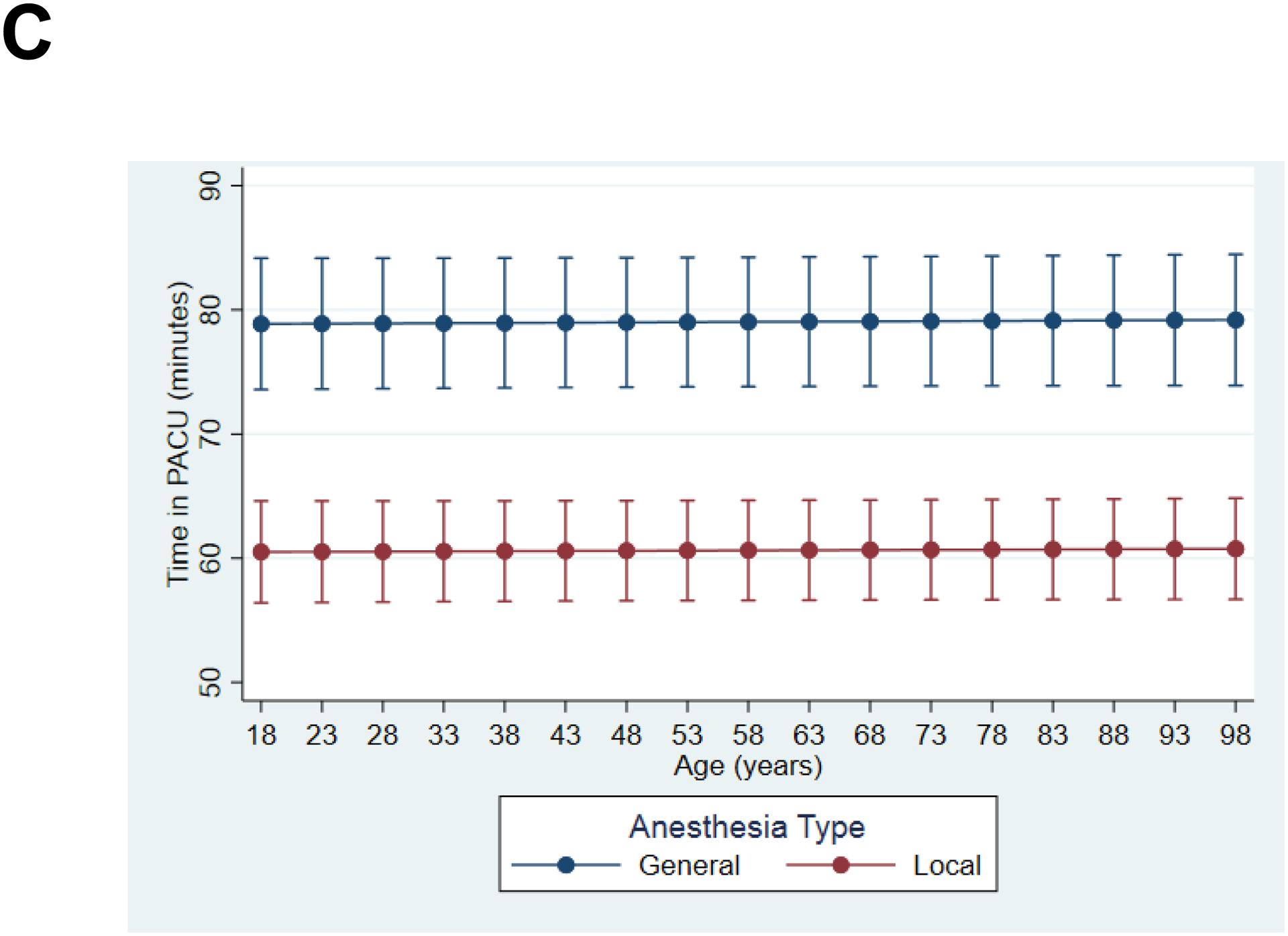
Risk-adjusted comparison of outcomes for local versus general anesthesia across the age spectrum of this cohort show a consistent and age-independent benefit of local over general anesthesia for (A) Postoperative complications, (B) Operative time, and (C) post-anesthesia recovery unit (PACU) time.
Our two-stage residual inclusion model also showed a strong association between use of local anesthesia and fewer complications compared to general anesthesia (OR 0.63, 95% CI 0.47–0.85).
Local anesthesia is associated with shorter operative time for all age groups
After adjusting for known confounding factors, local anesthesia was associated with a 12.5% reduction (~12 minutes) in total operative time (95% CI 17.5% - 7.5%) compared to general anesthesia. Increasing age was associated with a 0.1% increase in operative time (95% CI 0.05% - 0.13%), and there was no significant interaction between age and anesthesia modality. Figure 1B shows the adjusted operative time for patients having surgery under local compared to general anesthesia and demonstrates the consistent effect across all age groups. Our instrumental variable model was consistent with the above findings and use of local anesthesia was associated with a 12% decrease in operative time (95% CI 13.3%-11.1%) compared to general anesthesia.
Local anesthesia is associated with more rapid postoperative recovery for all ages
In addition to evaluating postoperative complications and operative time, we also compared time in the PACU following surgery. This represents a proxy for speed of postoperative recovery since most inguinal hernia surgery in the US is performed as an outpatient operation. Additionally, monitored post-anesthesia care is high intensity and high cost care, so shorter PACU stays could translate to significant cost savings for health systems. We found that using local anesthesia was associated with a 26.5% shorter PACU stay (95% CI 27.5% - 25.5%), while age was not a significant predictor. As shown in Figure 1C, this translated to an ~20-minute decrease in PACU time that was consistent for all age groups. The instrumental variable model was again consistent with our hierarchical regression and showed that local anesthesia was associated with a 37% shorter PACU stay (95% CI 39.3%-34.1%) compared to general anesthesia.
DISCUSSION
Our study represents the largest analysis of US patients having inguinal hernia surgery under local or general anesthesia, and is the first study to explicitly explore whether the benefits of local anesthesia varied with age. Although we had hypothesized that using local rather than general anesthesia for inguinal hernia repair would be more beneficial in older compared to younger adults, our analysis showed a strong association between use of local anesthesia and improved outcomes for patients of all ages. Our most striking finding was that choosing local over general anesthesia for hernia surgery appeared to “de-age” patients by 30 years. In essence, we found that a 65-year old patient who has a hernia repair under local anesthesia will have the same risk of postoperative complications as a 35-year old who has the same operation under general anesthesia. This benefit was consistent across all age groups, so a similar benefit exists for patients who are 80 or even 90 years old at the time of surgery. Individuals having hernia surgery under local anesthesia also spend 20 minutes less in the PACU and 12 minutes less in the operating room. From a health systems standpoint, operating room and PACU time represent some of the most expensive care arenas in a hospital. Spending a combined time of >30 minutes less in these high-cost settings could have profound implications for US health care costs, given that general surgeons perform this operation 800,000 times each year. Additionally, a significant reduction in operating and PACU time per case would facilitate higher operative volume at busy facilities. From a patient perspective, shorter PACU stay is also consistent with a more rapid recovery after surgery and shorter operative time could potentially reduce the cognitive and physical stress of the operation.
The main impetus for considering alternatives to general anesthesia for surgery, particularly among older adults, is concern that exposure to general anesthesia leads to accelerated postoperative cognitive and physical dysfunction. The American College of Surgeons and the American Geriatrics Society issued guidelines for perioperative care of older adults that recommended surgeons strongly consider alternatives to general anesthesia.4 Chen et al. studied 1 million surgical patients and found that administration of general anesthesia increased the risk of dementia in patients ≥50 years old by 34% while surgery under local anesthesia was not associated with a difference in risk.2 Other research has questioned whether it is anesthesia, surgery, or a combination of those and other factors that drive postoperative changes in older adults.17,18
Randomized trials specifically comparing outcomes of inguinal hernia surgery under local or general anesthesia have yielded mixed results. Nordin et al. randomized 616 inguinal hernia patients in Switzerland to local, regional, and general anesthesia. They found that operative times were 5 minutes faster for local compared to general anesthesia patients, complications were decreased by 29%, and unplanned admissions were decreased by 19%.10 Additionally, they conducted a cost-effectiveness analysis that showed more rapid recovery and shorter hospital/operative times in the local group led to cost savings of >$400 per case.11 By contrast, O’Dwyer et al. randomized 140 Scottish patients to local and 139 to general anesthesia.12 They did not see any difference in complications (though the definitions were different from Nordin et al.), operative time, or immediate cognitive recovery. They did find a small cost savings of $40 per case. A key limitation of both trials was the study populations mostly consisted of younger and healthier participants. Since general anesthesia is expected to affect older adults more than their younger counterparts, both studies are likely to have underestimated the potential benefits of local anesthesia by focusing on a less at-risk population. Although our results show a consistent, age-independent benefit of local anesthesia, the VASQIP database does not capture cognitive changes from anesthesia or the incidence of urinary retention (which increases with age). Consequently, we expect that a randomized trial focusing on older adults is still more likely to demonstrate the full range of benefits from avoiding general anesthesia. Our study also differs from the above randomized trial and most observational studies in other important ways. Both major randomized trials and most large observational studies comparing local versus general anesthesia for inguinal hernias were conducted on European patients. In Europe, inguinal hernia repair has typically been an inpatient procedure with an expected hospitalization of up to 3 days or more. Consequently, any cost savings from faster operative or recovery time with local anesthesia tended to be offset by the greater costs of inpatient hospitalization. Before making decisions that operative and anesthesia approach in US patients, is important to understand the implications of those decisions by studying outcomes in our population. Our study addresses this critical need.
Limitations
Although our study shows the potential for substantial benefit if surgeons perform hernia surgery under local rather than general anesthesia, there are several limitations that must be acknowledged. First, some of the benefit associated with local anesthesia may be due to unknown confounding or bias that we cannot adjust for in our models given the observational nature of this study. However, our instrumental variable and two-stage residual inclusion models yielded results that were consistent with our mixed model approach. Additionally, it should be noted that one benefit of the observational design is the large sample size which enables us to identify differences in complications even for surgeries with low morbidity. It would be very difficult to adequately power a randomized trial to detect the differences observed in our study that are nonetheless important for patients. As mentioned above, VASQIP does not capture cognitive outcomes or functional status after surgery. Consequently, our estimates of the potential benefits for local anesthesia are likely to be conservative. We also do not have access to data regarding the size and duration of the hernia prior to repair or operative details such as the use of mesh or the number of patients who began surgery under local anesthesia but required conversion to general anesthesia. It is possible that surgeons are reluctant to repair more complex and large hernias under local anesthesia, translating to bias in our results. Our instrumental variable analysis should, to some extent, address this weakness. Additionally, patients having surgery under local anesthesia tended to be older and sicker (Table 1), so we would expect this group to have more complications and longer recovery times. The fact that patients in the current study having surgery under local anesthesia actually experienced significantly fewer complications in spite of this bias tends to support the validity of our findings. Finally, one might argue that it may be difficult to generalize our findings to a non-Veteran population. However, since the vast majority of inguinal hernia patients are men, we see little reason to assume that our findings would not apply to a broader population.
In summary, our findings suggest that surgeons should consider using local rather than general anesthesia for open inguinal hernia surgery in both old and young patients. Although our results need to be verified in a randomized trial that includes a similar population of older adults with multiple comorbidities, we found a remarkable decrease in complication rate and resource utilization associated with using local anesthesia for hernia repair.
ACKNOWLEDGEMENTS
People
The authors would like to thank Dave Primm for help in editing this manuscript.
Funding/Financial Support
This work was supported by a GEMSSTAR grant from the National Institute of Aging (1R03AG056330; for C.J.B.). Dr. Brown was supported, in part, by a VA Rehabilitation R&D Merit Award (1 I01 RX001995). Dr. Berger acknowledges support from K76 AG057022.
Footnotes
COI/Disclosures
The authors have no related personal or financial conflicts of interest to disclose.
REFERENCES
- 1.Chen P-L, Yang C-W, Tseng Y-K, et al. Risk of dementia after anaesthesia and surgery. The British Journal of Psychiatry 2014; 204(3):188–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen C-W, Lin C-C, Chen K-B, et al. Increased risk of dementia in people with previous exposure to general anesthesia: A nationwide population-based case–control study. Alzheimer’s & Dementia 2014; 10(2):196–204. [DOI] [PubMed] [Google Scholar]
- 3.Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. The Lancet 1998; 351(9106):857–861. [DOI] [PubMed] [Google Scholar]
- 4.Optimal Perioperative Management of the Geriatric Patient: Best Practices Guidelines from ACS NSQIP/American Geriatrics Society. Available at: https://www.facs.org/~/media/files/qualityprograms/geriatric/acs. Accessed 12/18/2017. [DOI] [PubMed]
- 5.U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Digestive diseases statistics for the United States 2010. Available at: https://www.aafp.org/afp/2013/0615/p844.html#afp20130615p844-b2. Accessed 12/20/2017.
- 6.Cheema FN, Abraham NS, Berger DH, et al. Novel approaches to perioperative assessment and intervention may improve long-term outcomes after colorectal cancer resection in older adults. Ann Surg 2011; 253(5):867–874. [DOI] [PubMed] [Google Scholar]
- 7.Mull HJ, Rosen AK, Pizer SD, et al. Association between postoperative admission and location of hernia surgery: A matched case-control study in the veterans administration. JAMA Surgery 2016; 151(12):1187–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhattacharya SD, Vaslef SN, Pappas TN, et al. Locoregional versus general anesthesia for open inguinal herniorrhaphy: a National Surgical Quality Improvement Program analysis. Am Surg 2012; 78(7):798–802. [PubMed] [Google Scholar]
- 9.Neumayer L, Giobbie-Hurder A, Jonasson O, et al. Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 2004; 350(18):1819–1827. [DOI] [PubMed] [Google Scholar]
- 10.Nordin P, Zetterström H, Gunnarsson U, et al. Local, regional, or general anaesthesia in groin hernia repair: multicentre randomised trial. The Lancet 2003; 362(9387):853–858. [DOI] [PubMed] [Google Scholar]
- 11.Nordin P, Zetterström H, Carlsson P, et al. Cost–effectiveness analysis of local, regional and general anaesthesia for inguinal hernia repair using data from a randomized clinical trial. British Journal of Surgery 2007; 94(4):500–505. [DOI] [PubMed] [Google Scholar]
- 12.O’Dwyer PJ, Serpell MG, Millar K, et al. Local or General Anesthesia for Open Hernia Repair: A Randomized Trial. Annals of Surgery 2003; 237(4):574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 1998; 228(4):491–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Terza JV. Two-Stage Residual Inclusion Estimation in Health Services Research and Health Economics. Health Services Research 2018; 53(3):1890–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sheffield KM, Riall TS, Han Y, et al. Association between cholecystectomy with vs without intraoperative cholangiography and risk of common duct injury. JAMA 2013; 310(8):812–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stock JH, Yogo M. Testing for weak instruments in linear IV regression. Cambridge: Cambridge University Press, 2005. [Google Scholar]
- 17.Davis N, Lee M, Lin AY, et al. Post-operative cognitive function following general versus regional anesthesia, a systematic review. Journal of neurosurgical anesthesiology 2014; 26(4):369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evered L, Scott DA, Silbert B, et al. Postoperative cognitive dysfunction is independent of type of surgery and anesthetic. Anesth Analg 2011; 112(5):1179–1185. [DOI] [PubMed] [Google Scholar]


