Abstract
Endocrine mucin-producing sweat gland carcinoma (EMPSGC) is a rare, low-grade adnexal neoplasm with predilection for the periorbital skin of older women. Histologically and immunophenotypically, EMPSGC is analogous to another neoplasm with neuroendocrine differentiation, solid papillary carcinoma of the breast. Both lesions are spatially associated with neuroendocrine mucinous adenocarcinomas of the skin and breast, respectively. EMPSGC is ostensibly a precursor of neuroendocrine-type mucinous sweat gland adenocarcinoma (MSC), a lesion of uncertain prognosis. Non-neuroendocrine MSC has been deemed locally aggressive with metastatic potential, and previous works speculated that EMPSGC-associated [neuroendocrine-type] MSC had similar recurrence and metastatic potential with implications for patient follow-up. Only 96 cases of EMPSGC have been reported (12 cases in the largest case series). Herein, we present 63 cases diagnosed as ‘EMPSGC’ in comparison with aggregated results from known published EMPSGC cases. We aim to clarify the clinicopathologic features and prognostic significance of the neuroendocrine differentiation of EMPSGC and its associated adenocarcinoma and to determine the nosological relevance of EMPSGC-association in the spectrum of MSC histopathogenesis. Results established an overall female predominance (66.7%) and average presenting age of 64 years. EMPSGC lesions were associated with adjacent MSC in 33.3% of cases. The recurrence rate for neuroendocrine-type MSC was approximately 21%, less than the reported 30% for non-neuroendocrine MSC. There were no cases of metastasis. EMPSGC and neuroendocrine-type MSC are distinct entities with more indolent behavior than previously reported, supporting a favorable prognosis for patients.
INTRODUCTION
Endocrine mucin-producing sweat gland carcinoma (EMPSGC) is a low-grade primary cutaneous adnexal neoplasm with a predilection for the periorbital skin of women in the seventh decade of life.1,2 Primary cutaneous adnexal neoplasms frequently parallel morphological and immunohistochemical features of breast tumors, reflecting the common embryological origins of mammary and sweat glands.3 Histologically, EMPSGC bears striking resemblance to solid papillary carcinoma of the breast.3 The latter displays neuroendocrine morphology, a distinctive immunohistochemistry (IHC) profile, and occasional physical continuity with neuroendocrine invasive mucinous carcinoma of the breast (Type B) of which solid papillary carcinoma is a putative precursor.4,5 Likewise, EMPSGC has garnered recent interest because of its proposed role as an in situ precursor of primary mucinous sweat gland adenocarcinoma with neuroendocrine features.1,6–10
In 1995, Rahilly et al. introduced a neuroendocrine subtype of mucinous sweat gland carcinoma (MSC) [also known as primary cutaneous mucinous carcinoma],11 and as pathologists increasingly recognized the classic neuroendocrine appearance, the diagnosis of EMPSGC emerged.1,3,12 Despite proposing that EMPSGC represents a histological analog of solid papillary carcinoma, a breast carcinoma in situ with malignant potential, Flieder et al. and Zembowicz et al. implied that the term ‘EMPSGC’ encompasses an entire spectrum of neuroendocrine tumors including situ-only lesions, lesions with both in situ and invasive components, and invasive mucinous carcinomas.1,3 Using one name for multiple points on the continuum, from pre-cancerous eccrine duct proliferations to invasive carcinoma, combined with a lack of specific studies on the associated neuroendocrine-type MSC resulted in diagnostic variation and debate. Diagnosticians using the label ‘EMPSGC’ usually pointed out associated in situ and/or invasive components in their microscopic comments. Yet, there were no definitive clinical guidelines regarding whether to treat EMPSGC as an invasive carcinoma, regardless of its position on the continuum, or as a more indolent lesion. In 2018, the World Health Organization (WHO) Classification of Skin Tumours, for the first time, included a chapter on EMPSGC and definitively recommended that hybrid lesions containing in situ and invasive mucinous components should be diagnosed as mucinous adenocarcinoma [with neuroendocrine features].9
To date, there have been no reports specifically describing the characteristics of this EMPSGC-associated MSC. Moreover, while EMPSGC is exceedingly rare, EMPSGC-associated MSC is even less common. Since Flieder et al. first named and described EMPSGC in 1997, we have counted 96 reported cases diagnosed as ‘EMPSGC,’ a third of which were published since 2017.3 Previous reports insinuated identical behavior of EMPSGC-associated MSC to its non-neuroendocrine MSC (Non-NE MSC) counterpart. Due to limited data, authors repeatedly cited the recurrence and metastatic potential of Non-NE MSC as proxies for EMPSGC-associated MSC to guide diagnostic and treatment decisions.1,6,13–16 We provide a retrospective series of 63 cases previously diagnosed as EMPSGC including clinicopathologic features (summarized in Table 1) and deliver a complete summary of the 96 previously reported cases [eTable 1, Supplemental Digital Content, (SDC)].1–3,6–8,10,13,14,16–41 In addition, we present the first case series of EMPSGC-associated MSC and compare it with the series of previously published invasive cases that would now qualify as EMPSGC-associated MSC (Table 2).1–3,6,10,18,20,21,23,25,29,32,36,41 We compare the unique attributes of EMPSGC-associated MSC with those of Non-NE MSC and consider the prognostic significance of the neuroendocrine differentiation of EMPSGC-associated MSC and EMPSGC.
TABLE 1.
Clinical, Histopathologic, and Immunohistochemical Characteristics of Cases Diagnosed as ‘EMPSGC’
| Clinical Characteristics | Neuroendocrine Markers | Other Markers | Histologic Features | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case No. | Age/Sex | Site | Appearance | Clinical Suspicion | Surgical Intervention | Syn | Chr | NSE | ER | PR | SMA or p63 | In Situ/Pushing Invasion | Invasive mucinous component | Recurrence/Follow-up | |
| 1 | 55 | M | Lower | Smooth, erythematous | Recurrent mucinous adenoma | Wedge resect. | + | + | SMA+ | x | Y, 36 mo | ||||
| 2 | 62 | M | Lower | Nodular | Chalazion vs. cyst | Slow Mohs | + | + | + | SMA+ | x | N, 4 mo | |||
| 3 | 56 | F | Lower | Cystic | Eccrine cyst | Mohs | foc+ | (−) | + | + | + | SMA+ | x | N, 3 mo | |
| 4 | 62 | M | Lower | Cystic | Nonmelanoma cancer | Mohs | foc+ | (−) | + | + | x | N, 50 mo | |||
| 5 | 57 | M | Lower | Solid, well-circumscribed, telangiectasia | Mucinous carcinoma | Mohs | + | (−) | + | x | - | ||||
| 6 | 59 | F | Lower | - | - | - | + | + | p63+ | x | N, ≥12 mo | ||||
| 7 | 67 | F | Lower | - | BCC | Mohs | + | + | p63+ | x | N, ≥12 mo | ||||
| 8 | 74 | F | Upper | Cystic | Cyst | Mohs | + | (−) | + | + | SMA+ | x | N, ≥12 mo | ||
| 9 | 71 | F | Upper | Cystic | Cyst | Mohs | + | (−) | + | + | SMA+ | x | N, ≥12 mo | ||
| 10 | 57 | M | Lower | Cystic | Cyst | - | + | (−) | + | + | x | N, ≥12 mo | |||
| 11 | 50 | M | Lower | - | - | - | + | + | + | + | x | N, ≥12 mo | |||
| 12 | 57 | F | Lower | - | - | Mohs | + | + | + | + | x | N, ≥12 mo | |||
| 13 | 66 | F | Lower | Cystic | Inclusion cyst with recurrence | Mohs | + | + | + | + | x | Y, unknown | |||
| 14 | 56 | F | Upper | Cystic | Cyst | - | foc+ | + | + | + | x | N, ≥12 mo | |||
| 15 | 53 | F | Upper | Cystic | Cyst | - | + | + | x | N, ≥12 mo | |||||
| 16 | 57 | F | Lower | - | Recurrent papillary eccrine adenoma | - | + | + | + | + | x | N, ≥12 mo | |||
| 17 | 71 | F | Upper | White, cystic, madarosis, telangiectasia | Chalazion | Mohs | foc+ | foc+ | + | + | x | N, 2 mo | |||
| 18 | 53 | M | Lower | Cystic | Cyst | - | (−) | + | + | + | x | N, ≥12 mo | |||
| 19 | 66 | F | Lower | Cystic | Cyst | - | + | + | + | + | x | N, ≥12 mo | |||
| 20 | 70 | F | Both | Cystic | Canthal cysts | - | + | + | + | + | x | N, ≥12 mo | |||
| 21 | 76 | M | Lower | Cystic | Cyst increasing in size, h/o multiple BCCs of face | Mohs | + | + | + | + | x | N, ≥12 mo | |||
| 22 | 57 | M | Both | Erythematous | Recurrence of EMPSGC | - | + | + | + | + | x | Y, 12 mo | |||
| 23 | 62 | F | Canthus | - | - | - | + | + | + | + | + | x | N, ≥12 mo | ||
| 24 | 52 | F | Lower | Nodular, telangiectasia | - | Mohs | + | + | + | + | x | N, 6 mo | |||
| 25 | 58 | M | Upper | - | - | - | + | + | + | + | x | N, 5 mo | |||
| 26 | 58 | M | Lower | Cystic | Inclusion cyst | - | + | + | + | + | x | N, ≥12 mo | |||
| 27 | 76 | F | Upper | Cystic | - | - | + | - | + | x | N, 2 mo | ||||
| 28 | 73 | F | Upper | Round, subcutaneous nodular, tan pink | Hidrocystoma associated to previous chalazion | Ellipse | foc+ | (−) | + | + | + | p63+ | x | N, 1 mo | |
| 29 | 63 | F | Upper | Slightly raised, centrally located | - | Wedge resect. | foc+ | + | + | SMA+ | x | - | |||
| 30 | 84 | F | Lower | Vascular | Hemangioma | Ellipse | foc+ | + | + | p63+ | x | - | |||
| 31 | 69 | F | Upper + Canthus | Polypoid tan lesion | Tumor | Wedge biopsy | + | + | p63+ | x* | Y, unknown | ||||
| 32 | 62 | F | Lower | Subcutaneous, tan lobulated appearance | - | Wedge biopsy | foc+ | + | + | p63+ | x | - | |||
| 33 | 69 | F | Upper | Skin-colored nodular | - | Biopsy | foc+ | + | + | x | - | ||||
| 34 | 58 | F | Lower | Tan-brown nodular | Low grade EMPSGC | Wedge resect. | + | (−) | SMA+ | x | Y, unknown | ||||
| 35 | 61 | F | Temple | - | Dermal apocrine carcinoma | Ellipse | foc+ | foc+ | + | + | SMA- | x | - | ||
| 36 | 61 | F | Lower | Roughly oval polyp-like lesion lined by tan-gray skin | - | Wedge resect. | foc+ | + | + | p63+ | x | - | |||
| 37 | 69 | F | Lower | - | - | Shave biopsy | foc+ | + | + | p63+ | x | - | |||
| 38 | 71 | M | Canthus | - | - | Ellipse | (−) | foc+ | (−) | (−) | p63+ | x | Y, unknown | ||
| 39 | 72 | M | Lid | - | - | Wedge resect. | (−) | (−) | + | + | + | SMA+ | x | N, 8 mo | |
| 40 | 53 | M | Upper | - | BCC | Slow Mohs | + | + | + | + | + | SMA+ | x | N, 2 mo | |
| 41 | 70 | F | Upper | Cystic | BCC vs. merkel cell carcinoma | Wedge resect. | + | + | + | + | + | SMA+ | x | Y, 10 mo | |
| 42 | 61 | M | Upper | Well-circumscribed, no ulceration | - | Slow Mohs | (−) | (−) | + | + | + | SMA+ | x | N, 18 mo | |
| 43 | 78 | F | Upper | Cystic | BCC | Slow Mohs | + | + | + | + | + | SMA+ | x | Y, 36 mo | |
| 44 | 87 | M | Lower | Well-circumscribed, telangiectasia, nearly white | BCC | Wedge resect. | + | + | + | + | + | SMA+ | x | N, 10 mo | |
| 45 | 66 | F | Upper | Cystic | Cyst/wart | Wedge resect. | (−) | (−) | + | + | + | SMA+ | x | N, 8 mo | |
| 46 | 69 | M | Upper | - | Atypical chalazion | Wedge resect. | + | (−) | + | + | + | SMA+ | x | N, 4 mo | |
| 47 | 57 | F | Lower | Cystic | Hidrocystoma | Shave biopsy | + | + | + | x | - | ||||
| 48 | 81 | F | Canthus | Nodular, telangiectasia | BCC | Wedge resect. | + | + | + | + | x | N, 1 mo | |||
| 49 | 64 | M | Lower | - | - | Ellipse or deep shave | + | + | x | - | |||||
| 50 | 58 | F | Upper | Cystic, telangiectasia | Hidrocystoma | Wedge resect. | foc+ | (−) | + | x | N, 3 mo | ||||
| 51 | 75 | F | Upper | - | - | Wedge resect. | + | + | x | N, 22 mo | |||||
| 52 | 82 | F | Lower | - | - | - | + | (−) | x | - | |||||
| 53 | 52 | M | Lower | Cystic, erythematous, telangiectasia | Hidrocystoma | Wedge w/FS | + | + | x | N, 5 mo | |||||
| 54 | 69 | F | Lower margin | Similar to BCC, erythematous | BCC | Mohs | + | + | + | + | x | N, 11 mo | |||
| 55 | 60 | F | Lower margin | Similar to BCC, erythematous | BCC | Mohs | + | + | + | + | x | N, 22 mo | |||
| 56 | 47 | M | Lower margin | Similar to BCC, erythematous | BCC | Mohs | + | + | + | + | SMA+ | x | N, 60 mo | ||
| 57 | 56 | F | Lower margin | Pearly, like BCC, erythematous | BCC, Mucinous Carcinoma | Mohs | + | + | + | + | SMA+ | x | N, 67 mo | ||
| 58 | 72 | F | Lower | Nodular | BCC | Wedge resect. | + | + | + | (−) | x | N, 12 mo | |||
| 59 | 57 | M | Upper | Tan, nodular | Neoplasm of uncertain behavior | Mohs | (−) | (−) | + | + | + | SMA+ | x | N, 2 mo | |
| 60 | 70 | F | Lower | Cystic | Hidrocystoma vs. other | Wedge w/FS | + | + | + | + | x | N, 12 mo | |||
| 61 | 66 | F | Upper | Cystic, skin-colored, well-circumscribed | Cystic lesion | Wedge resect. | + | + | + | + | x | Y, 34 mo | |||
| 62 | 63 | F | Upper | Skin-colored papule | Retention cyst | Wedge resect. | + | foc+ | + | + | SMA- | x | N, 9 mo | ||
| 63 | 64 | F | Lower | Nodular, pearly, possibly cystic, with distortion of the lid margin, madarosis, telangiectasia | BCC | Biopsy with reconstruction | + | + | + | + | x | N, 1 mo | |||
Lower = lower eyelid, Upper = upper eyelid, Both = upper and lower eyelid; BCC = basal cell carcinoma; Resect. = resection; FS = frozen section; Syn = synaptophysin, Chr = chromogranin, NSE = neuron-specific enolase, ER = estrogen receptor, PR = progesterone receptor; + = positive, foc+ = focally positive, (−) = negative; Light grey background highlights the 10 cases that were previously published by Hoguet et al. and Turnbull et al.7,26;
Dark grey highlights the four cases that were considered neuroendocrine positive based on NSE staining and other features; mo = months
TABLE 2.
Comparative Results for EMPSGC-Associated Mucinous Sweat Gland Adenocarcinoma
| |
Our Series of EMPSGC-Associated
MSC, n=21 |
Previously Published Cases of
EMPSGC-Associated MSC, n=22*Ψ |
||||
|---|---|---|---|---|---|---|
| Women | 61.9% | 66.7% | ||||
| Men | 38.1% | 33.3% | ||||
| Range (years) |
Range (years) |
|||||
| Total Average Age (years) | 66.7 | 52–84 | 64.7 | 36–87 | ||
| Women | 68.9, n=13 | 58–84 | 65.8, n=14 | 51–79 | ||
| Men | 63.3, n=8 | 52–72 | 62.6, n=7 | 36–87 | ||
| Recurrence Rate for EMPSGC-associated MSC | 5/21 (23.8%) | 4/22 (18.2)% | ||||
| Site of Lesion |
Site of Lesion |
|||||
| 10 Lower eyelid | 47.6% | 10 Lower eyelid | 47.6% | |||
| 7 Upper eyelid | 33.3% | 6 Upper eyelid | 28.5% | |||
| 2 Canthus | 9.5% | 4 Cheek | 19.0% | |||
| 1 Temple | 4.8% | 1 Canthus | 4.7% | |||
| 1 Lid, NOS | 4.8% | |||||
| Total | 21 | 100% | 21* | 100% | ||
| Type of Surgical
Intervention |
Type of Surgical
Intervention |
|||||
| 20 Wedge/ellipse excision or excisional biopsy | 90.5% | 10 Excision/”Resection, NOS,” or excisional biopsy or curettage | 47.6% | |||
| 2 Slow Mohs microsurgery | 9.5% | 2 Mohs microsurgery | 9.5% | |||
| 9 Not provided | 42.8% | |||||
| Total | 21 | 100% | 21* | 100% | ||
Calculated based on previously published reports (n=21/22 invasive cases) with definitive information regarding invasive status and patient demographics - see SDC eTable1
NOS = not otherwise specified
MATERIALS AND METHODS
Study Design
Institutional review board approval was obtained for a multi-center retrospective case series with the University of Wisconsin-Madison as the coordinating center. Collaborators represented 13 institutions and their areas of expertise spanned the fields of ophthalmology and oculoplastic surgery, ophthalmic pathology, dermatopathology, neuropathology, and surgical pathology. Collaborators performed retrospective searches for cases diagnosed as ‘EMPSGC’ encountered in their practices from January 1, 1995 to April 30, 2019. Information collected included patient demographics, clinical presentation, initial clinical impression, type of surgical intervention, histologic description, IHC performed, recurrences, and the presence of an invasive mucinous component (Table 1).
A total of 64 cases were collected, with the largest contributions from the departments of ophthalmic pathology at Tufts Medical Center (23), Houston Methodist Hospital (11), New York Eye and Ear Infirmary (8), Johns Hopkins Hospital (7), University of Wisconsin-Madison (5), and Washington University, St. Louis, MO (4). One case each was contributed by the Oregon Health & Science University, University of Texas Southwestern, NorthShore University Health System, Chicago, IL, University of South Florida, University of Calgary, Alberta, Canada, and Kingston Health Sciences Center, Ontario, Canada. Of note, 10 cases had been previously reported.7,26
The collaborators reviewed all cases using hematoxylin and eosin (H&E), occasionally periodic acid-Schiff (PAS), and various IHC stains. Collaborators were required to verify the presence of an invasive component in the EMPSGC cases and to provide information on any radiologic studies (MRI, CT, mammogram, PET scan, etc.) and/or systemic work-up performed within 12 months of the EMPSGC diagnosis. Available clinical information varied from case to case and by institution.
Immunohistochemistry and Exclusion Criteria
All 64 cases were screened for neuroendocrine differentiation by the presence of at least one positively staining neuroendocrine biomarker, synaptophysin, chromogranin, or neuron-specific enolase (NSE).42 We included four cases that were negative for synaptophysin and chromogranin, but positive for NSE because they incorporated other convincing features such as characteristic neuroendocrine morphology and estrogen and progesterone receptor (ER and PR) positivity.1–3,7,8,41 We relied on information provided by collaborators regarding stains performed and their interpretations. Due to the retrospective nature of the study, the same stains were not performed in each case. One case was excluded because it did not have adequate information on morphology or staining.
Data Analysis
The de-identified data was evaluated using Microsoft Excel software including subset analysis by sex and recurrences. The cases were separated into two groups: “EMPSGC [in situ or pushing invasion9]” and “EMPSGC with an invasive mucinous component” (thereafter referred to as ‘EMPSGC-associated MSC’). Two sample t-tests were used to assess for significant differences in the age of presentation between women and men with EMPSGC and amongst the cohort without invasive mucinous component versus the group with EMPSGC-associated MSC. These analyses were repeated for the aggregate series of previously published ‘EMPSGC’ cases and the results were compared (eTable 2, SDC).
RESULTS
Demographics and Clinical Information
A total of 63 cases, originally diagnosed as ‘EMPSGC’, were included in our series and compared to the aggregate of previously published reports (Table 3).1–3,6–8,10,13,14,16–41 Women comprised 66.7% of our cases while 33.3% were men. The overall mean age of clinical presentation was 64 years, with ages ranging from 47 to 87 years. On average, women tended to present at an older age than men (65.9 versus 60.9 years, p=0.03). Twenty-one of our 63 cases (33.3%) contained an associated invasive mucinous component. There was a significant difference between the average age of presentation of the EMPSGC cases [in situ or pushing invasion] from our series and those from the aggregated series of previously published cases (63 versus 67.7 years, p=0.04) [eTable 2, SDC, Comparative Results, Age Analysis).
TABLE 3.
Comparative Results
| |
Zembowicz et al. Cases
Diagnosed as EMPSGC n=12 |
Our Series of Cases Diagnosed
as EMPSGC, n=63 |
Previously Published Cases
Diagnosed as EMPSGC, n=86Ψ |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Women | 66.7% | 66.7% | 64.0% | ||||||
| Men | 33.3% | 33.3% | 36.0% | ||||||
| Range (years) | Range (years) | Range (years) | |||||||
| Total Average Age (years) | 70.0 | 48–84 | 64.2 | 47–87 | 67.2 | 29–88 | |||
| Women | 73.3, n=8 | 60–84 | 65.9, n=42 | 52–84 | 68.4, n=55 | 29–85 | |||
| Men | 64, n=4 | 48–79 | 60.9, n=21 | 47–87 | 65.1, n=33 | 36–88 | |||
| Overall Recurrence Rate |
30%++ |
9/63 (14.3%) |
4/86 (4.7%) |
||||||
| Ratio of EMPSGC Lesions with Invasive
Mucinous Component |
6/12 (50%) |
21/63 (33.3%) |
22/70 (31.4%)* |
||||||
| Recurrence Rate of EMPSGC-Associated MSC | [na]/6 | 5/21 (23.8%) | 4/22 (18.2%) | ||||||
Does not include 10 previously published cases included in our original data collection (Hoguet et al. and Turnbull et al.),7,26 but does include 12 cases published from original series by Zembowicz et al.1
Calculated based on 70/86 previously published cases with definitive information regarding invasive status (see SDC eTable1)
Lesions were frequently skin-colored and cystic appearing (Fig. 1). Initial clinical impression before pathologic evaluation was available for 45 cases (Table 1). Most often, some sort of benign cyst was suspected (46.7%), followed by suspected basal cell carcinoma (26.7%), or chalazion (6.7%). Other less common initial clinical impressions included adenoma, hemangioma, mucinous carcinoma, apocrine carcinoma, neoplasm of uncertain behavior, and non-melanoma carcinoma. Only 2 cases (4.4%) were suspected to be EMPSGC prior to pathologic evaluation. Tumors were predominantly located at the lower eyelid (55.6%), followed by upper eyelid (36.5%), and canthus (3.2%), [eTable 3, Site of Lesion Comparison]. Two cases had lesions on both upper and lower eyelids, and in one case, the lesion was at the temple. Information about follow-up was reported for 52 cases, and follow-up intervals ranged from 1 to 67 months, with an average follow-up interval of 13 months. There was available data regarding surgical intervention for 48 patients, and all had some sort of excision: wedge/ellipse excision or excisional biopsy (58.3%) or Mohs microsurgery (41.7%).
FIGURE 1.
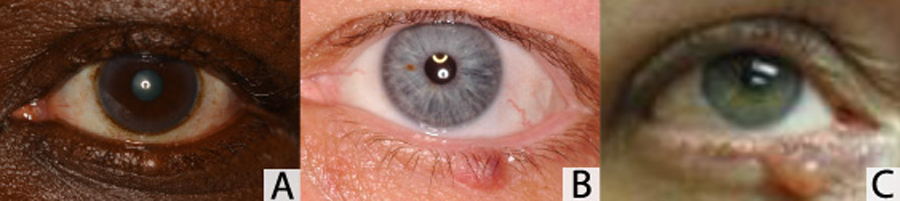
Clinical appearance of EMPSGC and neuroendocrine-type mucinous sweat gland carcinoma. A, Skin-colored, nodular, erythematous, and cystic lesion at the left lower eyelid margin. B, Skin-colored, smooth, nodular, pearlescent, and firm lesion at the left lower eyelid margin. C, Pedunculated, cystic lesion at the right lower eyelid margin.
The overall recurrence rate of our collected cases previously diagnosed as ‘EMPSGC,’ including the 21 that had an invasive mucinous component, was 14.3%. Of the 9 overall recurrences, two thirds were women. The most common site for recurrence was the lower eyelid (44.4%) followed by the upper eyelid (33.3%). More than half (5/9) of the recurrences were associated with a lesion that included an invasive carcinoma component. No metastases were reported.
Microscopic Features
All cases shared elements of characteristic neuroendocrine morphology (Fig. 2). The lesions comprised well-demarcated nodules with partially cystic and partially solid, papillary or cribriform architecture. Commonly cysts were filled with solid proliferations palisading around fibrovascular cores. Tumor cells were usually medium-sized epithelial cells, resembling bland eccrine ductal cells, with bluish cytoplasm and featured round-to-oval nuclei with stippled, “salt and pepper” chromatin (Fig. 3). Foci of both intracellular and extracellular mucin were present (Fig. 3 and Fig. 4A). Rare mitoses were present in about half (16/31) of the cases that provided information about mitoses. Additional findings included rosette-like structures, small clefts of mucin, fibrous stroma, pigment incontinence and reactive changes in the overlying eyelid epidermis. Necrosis was never seen. In some cases, SMA or p63 IHC stains were used to highlight myoepithelial cells. When a nodule composed of neoplastic cells had an intact rim of myoepithelial cells, it was considered in situ, whereas progression to neuroendocrine mucinous adenocarcinoma was signified by pools of extracellular stromal mucin and/or infiltrating tumor glands and nests that lacked an intact myoepithelial rim (Fig. 2 and Fig. 4B).1,8,9 Large expansile nodules that looked in situ but lacked intact myoepithelial rims were characterized as having pushing invasion, concept and terminology borrowed from solid papillary carcinoma of the breast.8,9,43,44
FIGURE 2.
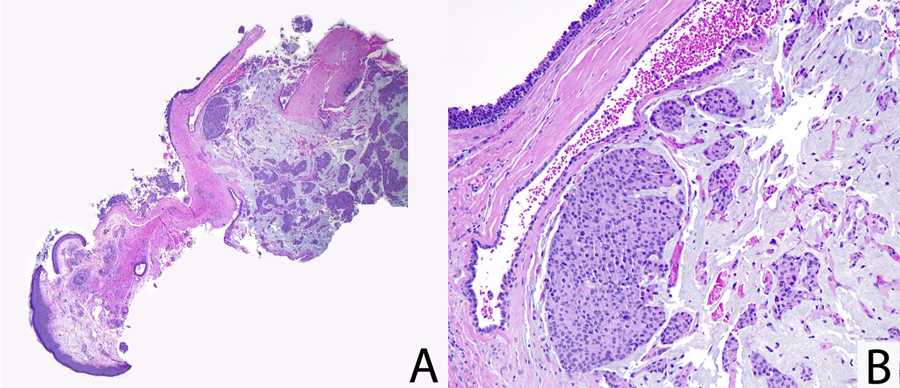
Morphology of neuroendocrine-type mucinous sweat gland carcinoma (Case no. 63). A, Low magnification, Skin with a mucinous tumor comprised of solid nests of amphophilic ductal cells, with oval nuclei and mild nuclear pleomorphism, suspended in stromal pools of mucin. B, High magnification, Solid, bluish tumor nodule adjacent to a cystic space consistent with a benign dilated eccrine gland. Tumor nests and clusters float in surrounding mucin.
FIGURE 3.
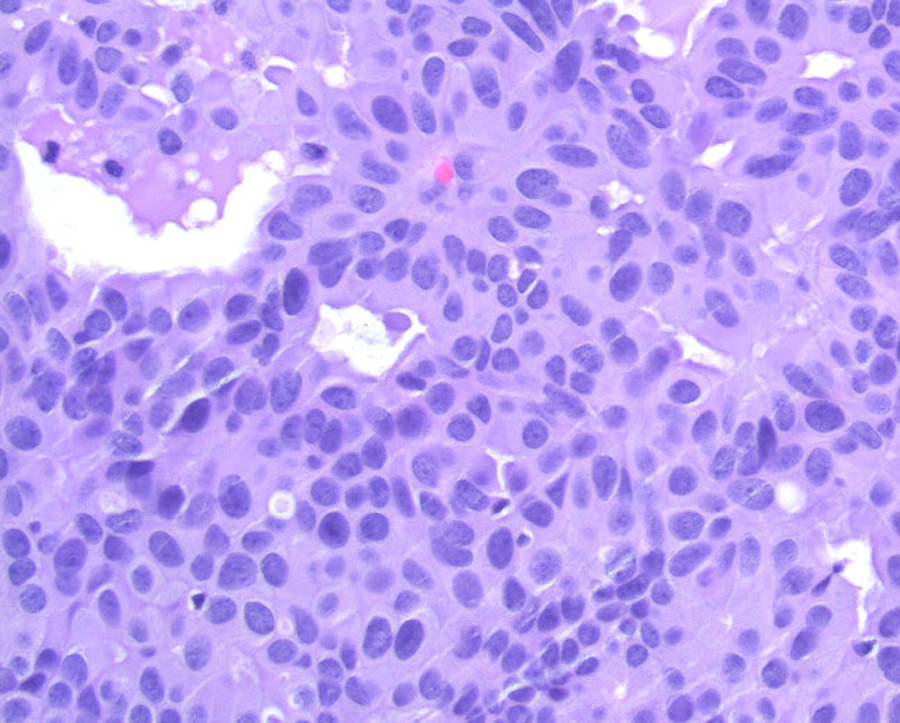
Tumor cells resembling bland eccrine ductal cells, with bluish cytoplasm, round-to-oval nuclei with fine stippled chromatin, and small amounts of intracellular and extracellular mucin.
FIGURE 4.
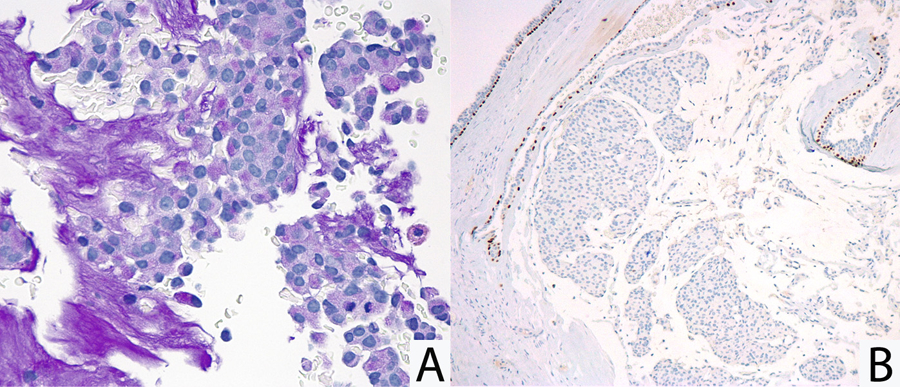
Features of neuroendocrine-type mucinous sweat gland carcinoma (Case no. 63). A, High magnification, Periodic acid–Schiff (PAS) staining highlights intracellular and extracellular mucin. B, Low magnification, p63 staining reveals a loss of myoepithelial rim around invasive nodules, an accepted mark of invasion in carcinomas of the breast. The adjacent normal eccrine glands represent a positive control.
Immunohistochemistry
All 63 cases in our series were tested for synaptophysin and 90.5% stained positively. Fifty-two of the cases had data about chromogranin staining, and of these, 71.2% stained positively. Within our collection, there were 55 cases provided data on ER staining, and 53 on PR staining, with 98.2% and 96.1% staining positively for ER and PR, respectively.
EMPSGC-Associated Mucinous Sweat Gland Adenocarcinoma
EMPSGC-associated MSC (denoted by the presence of an invasive mucinous component)9 was present in 21 cases with a female predominance (61.9% women versus 38.1% men). In this invasive adenocarcinoma subset, the overall mean age of clinical presentation was 66.7 years, ranging from 52 to 84 years (Table 2). The average age of women presenting with EMPSGC-associated MSC was higher than that for men (68.9 versus 63.3 years), but this difference was not significant, p=0.1. This neuroendocrine-type MSC occurred with highest frequency in lower eyelid (47.6%) followed by the upper eyelid (33.3%), canthus (9.5%), and temple (4.8%). While all of these EMPSGC-associated MSC patients underwent some type of excision, wedge/ellipse excisions or excisional biopsies were most frequent (90.5%), and there were two instances of Mohs microsurgery. There were 5/21 recurrences, and three of the five recurrences were seen in female patients. In the aggregate of previously published cases, there were 22 cases containing an invasive mucinous component, with 4/22 recurrences (all female).3,6,18 Combining these recurrence figures yields an approximate EMPSGC-associated MSC recurrence rate of 21% [5/21 and 4/22]. No cases of metastasis were identified in either group.
DISCUSSION
EMPSGC is a reputedly uncommon, low-grade lesion that predominantly affects the eyelid skin of older women and has the potential of being misdiagnosed/underdiagnosed.10 Previous authors have considered EMPSGC’s morphologic and immunophenotypic similarities to another neuroendocrine neoplasm, solid papillary carcinoma of the breast.1,3–5 In at least some cases, both EMPSGC and solid papillary carcinoma represent precursor lesions to spatially adjacent neuroendocrine mucinous sweat gland or invasive mucinous breast carcinomas, respectively.1,3–5 Mucinous carcinomas of the breast are divided into Type A, with no neuroendocrine expression and small cell clusters, and Type B, involving larger nests of neuroendocrine-positive neoplastic cells.4,18 As solid papillary carcinoma shared morphology with Type B mucinous breast carcinoma, it was deemed a likely precursor. Zembowicz et al. adopted a corresponding framework for EMPSGC: they likened cyst-formation within eccrine ducts to atypical ductal hyperplasia in the mammary ducts; atypical cells undermining the eccrine epithelium in EMPSGC akin to pagetoid spread; formation of cystic, solid, and papillary structures without loss of myoepithelial cells in EMPSGC similar to DCIS with intact myoepithelium; and loss of myoepithelial layers around ducts teeming with tumor cells representative of EMPSGC-associated invasive mucinous adenocarcinoma.1,10,18 Like Type B mucinous carcinoma in the breast, EMPSGC-associated MSC represents the neuroendocrine subtype of MSC.1,3,16,18
Included in the analogy was the concept of pushing invasion, which in the context of solid papillary carcinoma, describes a solid pattern of expansile growth rather than frank invasion.1,8,43 While loss of the myoepithelial rim indicates widely accepted evidence of invasion when observed in carcinomas of the breast, pushing invasion, albeit termed ‘invasion’ by definition (due to the loss of myoepithelial rim) is thought of as an in situ entity because of the indolence associated with it.44,45 Pushing invasion or “pushing borders” in solid papillary carcinoma is staged as carcinoma in situ and not like an invasive lesion.45 Similarly, as explained in the 4th edition, WHO Classification of Skin Tumours, an in situ EMPSGC with a focus of pushing invasion should be diagnosed as ‘EMPSGC’ because it lacks a definitive invasive mucinous component.9 As with solid papillary carcinoma, most foci of EMPSGC that appear non-invasive by morphology, in spite of undetectable myoepithelial cells, probably represent examples of carcinoma in situ with compression and obliteration of surrounding myoepithelium, and the degree of compression is likely a function of the size of the duct involved and the rate of growth of the expansile tumor.8,43,44
Notwithstanding these parallels and the distinctions purported, some breast literature authors contested that Type A and Type B mucinous breast carcinomas were too similar to merit a sharp distinction and such labeling had no influence on patient survival.18,46 The significance of neuroendocrine differentiation in the histogenesis of primary cutaneous mucinous carcinoma (MSC) was also debated.1,18 Some questioned the utility of verifying neuroendocrine expression with time-intensive, potentially costly IHC when the neuroendocrine variants might ultimately be treated identically to typical Non-NE MSC lesions.7,17,18 Remarkably, our results illustrate the more favorable prognosis of reduced recurrence and absence of metastasis in neuroendocrine-type MSC, potentially reassuring factors for patients with this diagnosis.
Awareness about how neuroendocrine-type MSC differs in morphology and behavior from the non-neuroendocrine subtype is essential for accurate diagnosis and appropriate clinical management. Neuroendocrine MSC features a female predominance versus the male predominance of the Non-NE MSC. Non-NE MSCs are composed of abundant mucinous areas that comprise more than 90% of the neoplasm; an in situ component may be present but is rarely seen.47 This is in contrast to EMPSGCs and their invasive counterparts, which predominantly feature focal mucin-filled intracytoplasmic vacuoles or smaller pools of extracellular mucin; mucin is never abundant.1,8,18,41 Importantly, Non-NE MSCs lack characteristic neuroendocrine appearance [i.e. bland, uniform tumor cells with medium-sized, round to oval nuclei with diffusely stippled, “salt and pepper” chromatin]1 and often contain atypical mitoses and significant cellular pleomorphism, not seen in neuroendocrine phenotype. As expected, Non-NE MSCs do not express neuroendocrine markers using IHC.
Therefore, the combination of positive neuroendocrine staining, characteristic neuroendocrine morphology, and clinical features are taken together to make the diagnosis of EMPSGC or EMPSGC-associated MSC, and the complete IHC profile including ER/PR positivity is contributory. 1,3,4,48 As with other neuroendocrine neoplasms, some neuroendocrine-type MSCs and/or EMPSGCs are only positive for one neuroendocrine marker. As in the cases we summarize, neuroendocrine staining may be weak, focal, or even absent in cases with characteristic neuroendocrine appearance.1,9,11,26 With limited data and published reports on neuroendocrine-type MSC, previous discussions regarding the clinical behavior of EMPSGC deferred to the Non-NE MSC reports and advocated for identical clinical management.1,13,14,22 The Non-NE MSC literature features a 30% recurrence rate,49–51 and 4.4–11% rate of metastases to regional nodes and distant spread. Consequently, Non-NE MSC is frequently described as a locally aggressive tumor, with limited metastatic potential,52 that should be taken seriously and completely excised to avoid metastases.10,25,49
Primary Non-NE MSC, first described by Lennox et al. in 1952, could itself be considered a rarity based on its low prevalence in the literature.12,49–51,53 Lennox and colleagues proposed that all primary mucin-producing tumors of the skin were of sweat gland origin and, naturally, have commonalities.12,53 Non-NE MSC, EMPSGC, and EMPSGC-associated MSC all have a predilection for the eyelid. A hybrid lesion in which an in situ or pushing borders EMPSGC exists in continuity with an invasive mucinous component should be diagnosed as an ‘invasive adenocarcinoma’ according to the WHO’s clarifying EMPSGC chapter.9 Regarding hybrid Non-NE MSC lesions, Kazakov et al. illustrated how the existence of an in situ component in association with invasive Non-NE MSC helps to characterize that lesion as a primary cutaneous neoplasm rather than a metastatic one.1,48 Cutaneous metastases to the face are exceptionally rare, and breast cancer metastases to the eyelid skin have only rarely been reported (1.2%).54 Even though cutaneous metastatic disease is uncommon, when working up Non-NE MSC, it is imperative to rule out metastasis from a different primary.47,49
By default, even in the case of EMPSGC, authors recommended the preliminary step of ruling out secondary metastases via mammogram and other imaging modalities,14,55 supposing that neuroendocrine mucinous carcinoma of the breast would be the most likely culprit due to similar morphology and a shared positivity for both neuroendocrine and ER/PR markers. This was recommended even in the case of in situ EMPSGC lesions without evidence of an associated invasive carcinoma.14 However, only 9.5% of the excised EMPSGCs (in situ or with pushing invasion) in our series recurred. This reinforces that, while deserving complete excision and subsequent surveillance,1,6,13,14 EMPSGCs are likely to behave more indolently than invasive disease and, thus, might warrant a less rigorous follow-up regimen. Not surprisingly, the excellent outcomes we observed in cases of EMPSGC lacking associated invasive carcinoma mirrors the favorable outcomes seen in the analogous solid papillary carcinoma cases without invasive components.48
Comparison of our own series of EMPSGC-associated MSC (n=21) with the aggregate series of previously published reports (n=22) shows that primary EMPSGC-associated MSC follows a more indolent course than described in the previous MSC literature that predates the recognition of EMPSGC-associated MSC. Hence, without taking neuroendocrine differentiation into consideration, previous recurrence rates described for MSCs are not good proxies for EMPSGC-associated MSC. We provide the first estimated recurrence rate of 21.0% [5/21 and 4/22, Table 2 and Table 3], which is more favorable than the 30% recurrence rate for Non-NE MSC cited by previous authors.49–51 Although two of the studies behind the recurrence rate attributed to Non-NE MSC precede the description of the neuroendocrine subtype, we are convinced that the cases included in the calculation predominantly describe Non-NE MSC based on morphologic and clinical features.50,51
Interestingly, our novel series of EMPSC-associated MSC replicated the female predominance (71.4%, 15/21) reported by Zembowicz et al. and others.1,2 The majority (77.8%) of EMPSGC-associated MSC cases that recurred after excision were also in female patients [7/9], and in our 63 cases diagnosed as ‘EMPSGC,’ women tended to present five years later than men on average, p=0.03. Especially intriguing, however, is the complete lack of any reported metastatic disease in the 96 previously published cases diagnosed as EMPSGC, or our novel 53. It seems that the neuroendocrine differentiation confers the indolence we observe, and likewise, neuroendocrine differentiation has been associated with indolent behavior in the invasive neuroendocrine mucinous counterpart in the breast.40 The counterpart breast literature suggests that low-grade neuroendocrine mucinous breast carcinomas have a low risk of progression and distant dissemination.27
To our knowledge, no cases of metastases pertaining to EMPSGC-associated MSC have been reported. The likelihood of EMPSGC representing a metastatic lesion from another primary is exceedingly low. However, even without significant threat of recurrence or metastasis, these tumors can be locally destructive and cosmetically disfiguring.34 Completely excising the lesion with wedge excision or slow Mohs surgery is an appropriate intervention to diminish the risk of progression to invasive carcinoma if in situ or recurrence.13,14,18 Extensive oncologic work-up along with regular imaging and follow-up for EMPSGC [in situ/pushing invasion] may be excessively cautious given the indolence we encountered. Improved awareness of both EMPSGC and EMPSGC-associated MSC, along with increased understanding of their distinctive characteristics (sex predilection, morphological features, and age of presentation) would facilitate earlier, accurate diagnosis. Correctly diagnosing EMPSGC and EMPSGC-associated MSC carries important prognostic benefits for patients and may avoid undue psychological stress associated with a carcinoma diagnosis.
Since the first neuroendocrine MSC was reported,11 reports and series have consisted of mostly1–3 cases, with the largest of series comprising 9–12 cases.1,2,7,41 We provide a more comprehensive analysis, and we are the first group to review and distinguish Non-NE MSC from the neuroendocrine subtype and address the value of including a neuroendocrine variant in the differential diagnosis of mucinous cutaneous adnexal neoplasms. Our updated incidence for EMPSGC-associated MSC (33.3% and 31.4%, Table 3) is probably more reflective of the true incidence than the previously reported 50% based on 12 cases.1 Here, we review 43 cases of neuroendocrine-type MSC, but we suspect the actual incidence may be higher. Additional research will continue to improve our understanding of these curious lesions. Nonetheless, we offer a timely update and the largest series in comparison with an aggregate of previously published cases diagnosed as ‘EMPSGC.’ Our results corroborate that EMPSGC is a likely precursor of the neuroendocrine-type MSC.1–3,6,9 Furthermore, we emphasize the differences between EMPSGC and EMPSGC-associated MSC, entities which were until recently diagnostically lumped together as ‘EMPSGC.’
Supplementary Material
eTable 1. Summary of Previously Reported Cases, PDF
eTable 2. Comparative Results, Age Analysis, PDF
eTable 3. Site of Lesion Comparison, PDF
FIGURE 5.
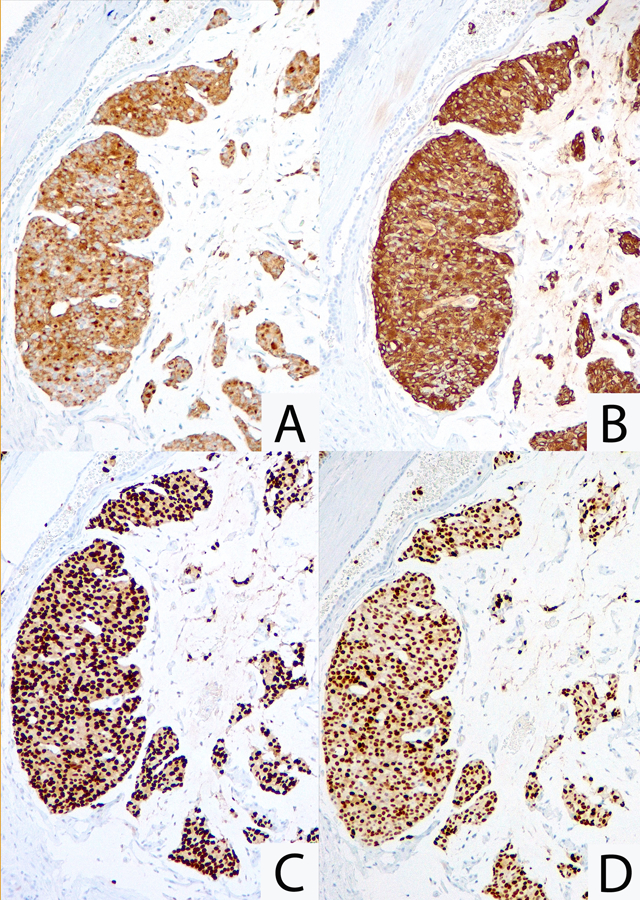
Immunohistochemical staining patterns of the neuroendocrine subtype of mucinous sweat gland carcinoma. Positive cytoplasmic staining for A, Synaptophysin and B, Chromogranin (neuroendocrine staining can be focal). C & D, Strong nuclear staining for estrogen and progesterone receptors, respectively.
Acknowledgments
Disclosures: Funding for this research was provided by NIH Core Grant P30 EY016665 and an Unrestricted Grant from Research to Prevent Blindness, Inc. to the University of Wisconsin Department of Ophthalmology and Visual Sciences.
Acknowledged contributor: Bret Evers (University of Texas Southwestern Medical Center)
Footnotes
Conflicts of Interest and Source of Funding: The authors have disclosed that they have no significant relationships with or financial interest in any commercial companies pertaining to this article.
References
- 1.Zembowicz A, Garcia CF, Tannous ZS, Mihm MC, Koerner F, Pilch BZ. Endocrine mucin-producing sweat gland carcinoma: twelve new cases suggest that it is a precursor of some invasive mucinous carcinomas. Am J Surg Pathol. 2005;29(10):1330–1339. [DOI] [PubMed] [Google Scholar]
- 2.Qin H, Moore RF, Ho CY, Eshleman J, Eberhart CG, Cuda J. Endocrine mucin-producing sweat gland carcinoma: a study of 11 cases with molecular analysis. J Cutan Pathol. 2018;45:691–697. [DOI] [PubMed] [Google Scholar]
- 3.Flieder A, Koerner FC, Pilch BZ, Maluf HM. Endocrine mucin-producing sweat gland carcinoma: a cutaneous neoplasm analogous to solid papillary carcinoma of breast. Am J Surg Pathol. 1997;21(12):1501–1506. [DOI] [PubMed] [Google Scholar]
- 4.Tsang WY, Chan JK. Endocrine ductal carcinoma in situ (E-DCIS) of the breast: a form of low-grade DCIS with distinctive clinicopathologic and biologic characteristics. The American journal of surgical pathology. 1996;20(8):921–943. [DOI] [PubMed] [Google Scholar]
- 5.Maluf HM, Koerner FC. Solid papillary carcinoma of the breast. A form of intraductal carcinoma with endocrine differentiation frequently associated with mucinous carcinoma. Am J Surg Pathol. 1995;19(11):1237–1244. [DOI] [PubMed] [Google Scholar]
- 6.Dhaliwal CA, Torgersen A, Ross JJ, Ironside JW, Biswas A. Endocrine mucin-producing sweat gland carcinoma: report of two cases of an under-recognized malignant neoplasm and review of the literature. Am J Dermatopathol. 2013;35(1):117–124. [DOI] [PubMed] [Google Scholar]
- 7.Hoguet A, Warrow D, Milite J, et al. Mucin-producing sweat gland carcinoma of the eyelid: diagnostic and prognostic considerations. Am J Ophthalmol. 2013;155(3):585–592.e582. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez-Flores A, Cassarino DS. Endocrine mucin-producing sweat gland carcinoma: a study of three cases and CK8, CK18 and CD5/6 immunoexpression. J Cutan Pathol. 2015;42(8):578–586. [DOI] [PubMed] [Google Scholar]
- 9.Zembowicz A, Argenyi ZB, Brenn T et al. , Endocrine mucin-producing sweat gland carcinoma. In: Elder DE, Massi D, Scolyer RA, Willemze R, 4th ed. WHO Classification of Skin Tumours. Lyon, France: IARC Press; 2018:168–169. [Google Scholar]
- 10.Salim AA, Karim RZ, McCarthy SW, Scolyer RA. Endocrine mucin producing sweat gland carcinoma: a clinicopathological analysis of three cases. Pathology. 2012;44(6):568–571. [DOI] [PubMed] [Google Scholar]
- 11.Rahilly MA, Beattie GJ, Lessells AM. Mucinous eccrine carcinoma of the vulva with neuroendocrine differentiation. Histopathology. 1995;27(1):82–86. [DOI] [PubMed] [Google Scholar]
- 12.Lennox B, Pearse AG, Symmers WS. The frequency and significance of mucin in sweat gland tumours. Br J Cancer. 1952;6(4):363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta S, Thiagalingam S, Zembowicz A, Hatton MP. Endocrine mucin-producing sweat gland carcinoma of the eyelid. Ophthalmic Plast Reconstr Surg. 2008;24(2):164–165. [DOI] [PubMed] [Google Scholar]
- 14.Tannous ZS, Avram MM, Zembowicz A, et al. Treatment of synchronous mucinous carcinoma and endocrine mucin-producing sweat gland carcinoma with Mohs’ micrographic surgery. Dermatol Surg. 2005;31(3):364–367. [DOI] [PubMed] [Google Scholar]
- 15.Flux K, Brenn T. Cutaneous Sweat Gland Carcinomas with Basaloid Differentiation An Update with Emphasis on Differential Diagnoses. Clinics in Laboratory Medicine. 2017;37(3):587–601. [DOI] [PubMed] [Google Scholar]
- 16.Bulliard C, Murali R, Maloof A, Adams S. Endocrine mucin-producing sweat gland carcinoma: report of a case and review of the literature. J Cutan Pathol. 2006;33(12):812–816. [DOI] [PubMed] [Google Scholar]
- 17.Bellezza G, Sidoni A, Bucciarelli E. Primary mucinous carcinoma of the skin. Am J Dermatopathol. 2000;22(2):166–170. [DOI] [PubMed] [Google Scholar]
- 18.Emanuel PO, de Vinck D, Waldorf HA, Phelps RG. Recurrent endocrine mucin-producing sweat gland carcinoma. Ann Diagn Pathol. 2007;11(6):448–452. [DOI] [PubMed] [Google Scholar]
- 19.Kim JB, Choi JH, Kim JH, et al. A case of primary cutaneous mucinous carcinoma with neuroendocrine differentiation. Ann Dermatol. 2010;22:472–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang S, Shim SH, Joo M, Kim H, Kim YK. A case of endocrine mucin-producing sweat gland carcinoma co-existing with mucinous carcinoma - a case report. Korean J Pathol. 2010;44(1):97–100. [Google Scholar]
- 21.Inozume T, Kawasaki T, Harada K, et al. A case of endocrine mucin-producing sweat gland carcinoma. Pathol Int. 2012;62(5):344–346. [DOI] [PubMed] [Google Scholar]
- 22.Koike T, Mikami T, Maegawa J, Iwai T, Wada H, Yamanaka S. Recurrent endocrine mucin-producing sweat gland carcinoma in the eyelid. Australas J Dermatol. 2013;54(2):e46–49. [DOI] [PubMed] [Google Scholar]
- 23.Shon W, Salomão DR. WT1 expression in endocrine mucin-producing sweat gland carcinoma: a study of 13 cases. Int J Dermatol. 2014;53(10):1228–1234. [DOI] [PubMed] [Google Scholar]
- 24.Shimizu I, Dufresne R, Robinson-Bostom L. Endocrine mucin-producing sweat gland carcinoma. Cutis. 2014;93(1):47–49. [PubMed] [Google Scholar]
- 25.Collinson AC, Sun MT, James C, Huilgol SC, Selva D. Endocrine mucin-producing sweat gland carcinoma of the eyelid. Int Ophthalmol. 2015;35(6):883–886. [DOI] [PubMed] [Google Scholar]
- 26.Turnbull LI, Puchalsky DR, Xu YG, Bennett DD. A cystic growth on the lower eyelid: a presentation of two cases. Int J Dermatol. 2015;54(7):737–739. [DOI] [PubMed] [Google Scholar]
- 27.Jedrych J, Jones M, Seethala R, Ho J. Primary cutaneous endocrine mucin-producing sweat gland carcinoma co-occurring simultaneously with low-grade ductal mucinous breast cancer: a clinicopathologic conundrum. Am J Dermatopathol. 2015;37(5):425–427. [DOI] [PubMed] [Google Scholar]
- 28.Bamberger M, Medline P, Cullen JB, Gill H. Histopathology of endocrine mucin-producing sweat gland carcinoma of the eyelid. Can J Ophthalmol. 2016;51(2):e72–75. [DOI] [PubMed] [Google Scholar]
- 29.Abdulkader M, Kuhar M, Hattab E, Linos K. GATA3 positivity in endocrine mucin-producing sweat gland carcinoma and invasive mucinous carcinoma of the eyelid: report of 2 cases. Am J Dermatopathol. 2016;38(10):789–791. [DOI] [PubMed] [Google Scholar]
- 30.Cornejo KM, Hutchinson L, Meng X, OʼDonnell P, Deng A. Endocrine mucin-producing sweat gland carcinoma of the eyelid: a report of a case with molecular analysis. Am J Dermatopathol. 2016;38(8):636–638. [DOI] [PubMed] [Google Scholar]
- 31.Lerias S, Rito M, Fonseca R, Rosa J. Endocrine mucin-producing sweat gland carcinoma of the eyelid-case report and review the literature. Virchows Archiv. 2017;471:S115–S115. [Google Scholar]
- 32.Chou YH, Chang YC, Huang YL, Wu CT. Endocrine mucin-producing sweat gland carcinoma with GATA3 expression: report of two cases. Pathology. 2017;49(7):805–808. [DOI] [PubMed] [Google Scholar]
- 33.Westby E, Benson K, Medline P, Hayes R. A case of endocrine mucin-producing sweat gland carcinoma. J Am Acad Dermatol. 2017;76(6):AB4–AB4. [Google Scholar]
- 34.Scott BL, Anyanwu CO, Vandergriff T, Nijhawan RI. Endocrine Mucin-producing sweat gland carcinoma treated with mohs micrographic surgery. Dermatol Surg. 2017;43(12):1498–1500. [DOI] [PubMed] [Google Scholar]
- 35.Ross AG, Chan AA, Mihm MC, Yu JY. Endocrine mucin-producing sweat gland carcinoma: an uncommon presentation. Semin Ophthalmol. 2017;32(4):511–513. [DOI] [PubMed] [Google Scholar]
- 36.Brett MA, Salama S, Gohla G, Alowami S. Endocrine mucin-producing sweat gland carcinoma, a histological challenge. Case Rep Pathol. 2017;2017:6343709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kawasaki T, Kubota T, Ichihara S, Horibe K, Hasebe T. Neuroendocrine cells associated with endocrine mucin-producing sweat gland carcinoma: a potential precursor lesion? Pathology. 2018;50(5):573–575. [DOI] [PubMed] [Google Scholar]
- 38.Charles NC, Proia AD, Lo C. Endocrine mucin-producing sweat gland carcinoma of the eyelid associated with mucinous adenocarcinoma. Ophthalmic Plast Reconstr Surg. 2018;34(2):e37–e38. [DOI] [PubMed] [Google Scholar]
- 39.Navrazhina K, Petukhova T, Wildman HF, Magro CM, Minkis K. Endocrine mucin-producing sweat gland carcinoma of the scalp treated with Mohs micrographic surgery. JAAD Case Rep. 2018;4(9):887–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hasegawa-Murakami Y, Kono M, Yokota K, Inaba H, Fukumoto T, Akiyama M. Dermoscopic features of endocrine mucin-producing sweat gland carcinoma. J Dermatol. 2018;45(3):353–356. [DOI] [PubMed] [Google Scholar]
- 41.Held L, Ruetten A, Kutzner H, Palmedo G, John R, Mentzel T. Endocrine mucin-producing sweat gland carcinoma: Clinicopathologic, immunohistochemical, and molecular analysis of 11 cases with emphasis on MYB immunoexpression. J Cutan Pathol. 2018. [DOI] [PubMed]
- 42.Bhargava R, Dabbs D, ed. Immunohistology of metastatic carcinomas of unknown primary. In: Dabbs D, 3rd ed. Diagnostic Immunohistochemistry. Philadelphia, PA: Elsevier Inc; 2010: 224–225. [Google Scholar]
- 43.Nicolas MM, Wu Y, Middleton LP, Gilcrease MZ. Loss of myoepithelium is variable in solid papillary carcinoma of the breast. Histopathology. 2007;51(5):657–665. [DOI] [PubMed] [Google Scholar]
- 44.Guo S, Wang Y, Rohr J, et al. Solid papillary carcinoma of the breast: A special entity needs to be distinguished from conventional invasive carcinoma avoiding over-treatment. Breast. 2016;26:67–72. [DOI] [PubMed] [Google Scholar]
- 45.Visscher D, Collins L, O’Malley F et al. , Solid papillary carcinoma. In: Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ, 4th ed. WHO Classification of Tumours of the Breast. Lyon, France: IARC Press; 2012:108–109. [Google Scholar]
- 46.Scopsi L, Andreola S, Pilotti S, et al. Mucinous carcinoma of the breast. A clinicopathologic, histochemical, and immunocytochemical study with special reference to neuroendocrine differentiation. Am J Surg Pathol. 1994;18(7):702–711. [PubMed] [Google Scholar]
- 47.Kazakov DV, Suster S, LeBoit PE, et al. Mucinous carcinoma of the skin, primary, and secondary: a clinicopathologic study of 63 cases with emphasis on the morphologic spectrum of primary cutaneous forms: homologies with mucinous lesions in the breast. Am J Surg Pathol. 2005;29(6):764–782. [DOI] [PubMed] [Google Scholar]
- 48.Saremian J, Rosa M. Solid papillary carcinoma of the breast: a pathologically and clinically distinct breast tumor. Arch Pathol Lab Med. 2012;136(10):1308–1311. [DOI] [PubMed] [Google Scholar]
- 49.Segal A, Segal N, Gal A, Tumuluri K. Mucinous sweat gland adenocarcinoma of the eyelid - current knowledge of a rare tumor. Orbit. 2010;29(6):334–340. [DOI] [PubMed] [Google Scholar]
- 50.Snow SN, Reizner GT. Mucinous eccrine carcinoma of the eyelid. Cancer. 1992;70(8):2099–2104. [DOI] [PubMed] [Google Scholar]
- 51.Mendoza S, Helwig EB. Mucinous (adenocystic) carcinoma of the skin. Arch Dermatol. 1971;103(1):68–78. [PubMed] [Google Scholar]
- 52.Wright JD, Font RL. Mucinous sweat gland adenocarcinoma of eyelid: a clinicopathologic study of 21 cases with histochemical and electron microscopic observations. Cancer. 1979;44(5):1757–1768. [DOI] [PubMed] [Google Scholar]
- 53.Santa-Cruz DJ, Meyers JH, Gnepp DR, Perez BM. Primary mucinous carcinoma of the skin. Br J Dermatol. 1978;98(6):645–653. [DOI] [PubMed] [Google Scholar]
- 54.Brownstein MH, Helwig EB. Metastatic tumors of the skin. Cancer. 1972;29(5):1298–1307. [DOI] [PubMed] [Google Scholar]
- 55.Cardoso JC, Calonje E. Malignant sweat gland tumours: an update. Histopathology. 2015;67(5):589–606. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Summary of Previously Reported Cases, PDF
eTable 2. Comparative Results, Age Analysis, PDF
eTable 3. Site of Lesion Comparison, PDF


