Abstract
Posttraumatic Stress Disorder (PTSD) is associated with difficulties in intimate relationships, with most prior research examining associations with continuous, single-dimension, and often-unstandardized measures of general relationship quality or aggression. Standardized, well-normed assessments that include multiple couple problem areas could provide more precise information about the presence and specific nature of clinically significant concerns in patient care settings. This investigation aimed to replicate findings regarding increased difficulties in relationship functioning among Operations Enduring and Iraqi Freedom Veterans with PTSD and their romantic partners, specifically using a standardized assessment that permits identification of cases of clinically significant general couple distress and difficulties across multiple problem areas. We compared 32 male Veterans with PTSD and 33 without PTSD, and their romantic partners on reports of several problem areas using the revised Marital Satisfaction Inventory (MSI-R). All participants underwent structured diagnostic interviewing. PTSD couples reported clinically significant levels of relationship distress several times more frequently than comparison couples, both for general distress and across all specific problem areas (e.g., aggressive behavior, quality of leisure time together, sexual functioning, conflicts about finances and child rearing). The most notable problem areas for PTSD couples were affective and problem-solving communication. These results replicate associations of PTSD with general couple discord and multiple specific areas of couple difficulties and extend them by documenting the clinical severity of these problems. Mental health providers may consider incorporating standardized couple assessments into their evaluations of Veterans’ functioning. Couples therapies may consider using such measures to prioritize targets for treatment.
Keywords: PTSD, couples, relationship quality, Marital Satisfaction Inventory
Of the more than two million troops from the United States deployed in the Iraq and Afghanistan Wars since 2001, up to 25% return with signs of posttraumatic stress disorder (PTSD) (Seal et al., 2009). PTSD is associated with strained intimate relationships, as reported by Veterans of multiple eras and their partners (Lambert, Engh, Hasburn, & Holzer, 2012; Taft, Watkins, Stafford, Street, & Monson, 2011). These couple problems are usually studied in terms of continuous scores on measures of general relationship quality (i.e., marital satisfaction or adjustment) or aggression and intimate partner violence (IPV), revealing greater difficulty for Veterans with PTSD and their partners (Lambert et al., 2012; Taft et al., 2011).
Although prior reviews have established robust associations of PTSD with general relationship quality and aggression (see review by Campbell & Renshaw, 2018; meta-analyses by Lambert et al., 2012; Taft et al., 2011), the prevalence of clinically-meaningful levels of relationship difficulties is less well established. Treating relationship quality as a continuous variable has advantages in maximizing sensitivity of statistical tests and in estimating effect sizes. However, it does not provide direct information about clinically meaningful levels of relationship distress. This is also true when studies use relationship measures with well-established norms, though only examine associations with continuous relationship quality scores. Information about clinically significant levels of couple distress could clarify the implications of prior research for practice and policy. For example, identification of clinically significant relationship distress has clear implications for individual and couples-based treatment plans. Further, information about the prevalence of clinically significant relationship distress can guide the refinement of clinical services for veterans with PTSD and can inform policy decisions about support for related screening, assessment, and intervention services.
Prior research in this area typically uses well-validated, self-report measures of relationship satisfaction and functioning (e.g., Relationship Assessment Scale [Hendrick, Dicke, & Hendrick, 1988]; Marital Problems Index [Jordan et al., 1992], Conflict Tactics Scale [Straus, 1979]; Dyadic Adjustment Scale [Spanier 1976]). Although such measures are well-established, the majority of them lack substantial normative information especially regarding specific areas of couple difficulty beyond aggression and IPV. Use of such measures, like the examination of only continuous scores from well-validated relationship measures, creates potentially important interpretive ambiguities, in both research and clinical applications. Specifically, it is possible that associations of PTSD symptom severity or diagnoses with continuous measures of marital quality could reflect variations within the essentially normal range of relationship quality, as opposed to clinically significant relationship difficulties more typical of couples experiencing high strain, who are seeking couple therapy, or who are at high risk of relationship disruption (i.e., separation, divorce).
Research using taxometric analyses to distinguish the categorical versus continuous structure of relationship quality illustrates this concern. In such studies, marital discord is most accurately seen as a qualitatively distinct category, occurring in 20 – 30% of couples (Beach, Fincham, Amir, & Leonard, 2005; Whisman, Snyder, & Beach, 2008), rather than the upper portions of an otherwise continuous dimension. However, there is considerable variability in levels of relationship quality within both the discordant and non-discordant categories (Beach et al., 2005; Whisman et al., 2008). Hence, it is difficult to determine if associations of PTSD with continuous measures of relationship quality reflect associations with a) clearly problematic levels of couple distress; b) subclinical couple concerns that might not warrant a full course of treatment; or with c) some combination of these levels of couple functioning. The use of standardized measures with adequate normative information and an examination of scores falling within established, clinical cutoffs would help to determine the extent to which such associations include clinically severe couple problems.
Given the value of couple-based therapy for PTSD (Monson et al., 2012), assessment and intervention could be bolstered by utilizing measures that identify clinically meaningful levels of couple discord and that extend beyond the traditional single, global dimension of relationship quality to include various dimensions and aspects of relationship functioning. There are theoretical and empirical reasons to anticipate that individuals with PTSD may have difficulties in multiple areas of relationship functioning. For example, prior research on PTSD symptom severity in Veterans and other populations predicts difficulties in emotional and sexual intimacy, support from partner, shared relationship activities, and parenting satisfaction, as well as elevated levels of aggression and IPV (e.g., Berz, Taft, Watkins, & Monson, 2008; LaMotte, Taft, Reardon, & Miller, 2015; Taft et al., 2011). PTSD symptoms of avoidance, emotional numbing, and hyperarousal are often associated with the lowest relationship satisfaction generally and are also associated with deteriorations in communication, intimacy, and parenting satisfaction, and increased conflict, for example (e.g., Berz et al., 2008; Solomon, Dekel, & Zerach, 2008). These investigations typically rely on continuous measures and non-normative data, and research that examines clinically significant levels of difficulty in these areas would be informative for describing the population and prioritizing targets for intervention.
The Marital Satisfaction Inventory – Revised (MSI-R; Snyder, 1997) and the Dyadic Adjustment Scale (DAS; Spanier 1976) are two validated and normed measures of multiple aspects of relationship functioning that have been used previously with individuals who have PTSD. However, most investigations have used shortened versions, have only reported on general relationship quality, or have not reported comparisons to norms (e.g., Balderrama-Durbin et al., 2015; Meis, Barry, Kehle, and Erbes, 2010). There are two exceptions. In Bosnian war refugees (Spasojevic et al., 2000), more severe PTSD symptoms were associated with general couple distress and difficulties in several specific relationship domains of the MSI-R, including affective and problem-solving communication, the quality of leisure time together, sexual functioning, and discussions of finances. In another study, wives of Israeli combat Veterans with PTSD endorsed less consensus (i.e., level of agreement and time spent together), affection, and less overall marital adjustment on the DAS than controls (Levin et al., 2016). However, the findings in both investigations are limited by the assessment of PTSD via self-report, rather than more definitive clinical diagnostic interviews. The use of self-report measures to assess PTSD is common among most investigations of PTSD and relationship satisfaction in this population (see meta-analysis by Lambert et al., 2012), whereas the present study utilizes both clinical interview and self-report measures to rule in and out the presence of PTSD.
As a preliminary step to examine the potential value of using a well-normed, comprehensive, and standardized measure of relationship functioning in U.S. Veterans, this investigation compared Operations Enduring and Iraqi Freedom (OEF/OIF) Veterans with and without diagnosed PTSD, and their romantic partners, on global couple functioning and seven problem area subscales using the clinical cut points for the MSI-R. In a prior report from this study using continuous marital adjustment scores, Veterans with PTSD and their partners reported elevated global distress on the MSI-R, greater problems in general positive relationship functioning (i.e., higher disaffection, or low warmth and intimacy), and higher overall negative functioning (i.e., higher disharmony, or hostility and conflict) (Herrington et al., 2008) compared to couples without PTSD (Caska et al., 2014). In the present paper, we go beyond these initial findings to pursue three additional aims. First, we use normative information (Snyder, 1997) and cut-offs established in prior taxometric research (Whisman et al., 2008) to examine the frequency of clinically-significant levels of couple discord. Second, we test associations of PTSD with specific couple problems, using the MSI-R scales of Affective Communication, Problem-Solving Communication, Time Together, Aggression, Disagreement about Finances, Conflict over Child Rearing, and Sexual Dissatisfaction. Third, given that couples’ agreement on relationship problems can influence couple therapy engagement and outcome (Biesen & Doss, 2013), we examined associations between Veterans’ and partners’ scores on these measures and whether the level of agreement differed between PTSD and comparison group couples.
For the first aim, we predicted that a higher proportion of PTSD couples would score in the distressed range for MSI-R norms (Snyder, 1997), and that a greater proportion would meet the cutoff for discordant taxon membership (Whisman et al., 2008). For the second aim, we predicted that Veterans with PTSD and their partners would report greater difficulties than the comparison group across specific problems, with the greatest difficulties in the communication domains (LaMotte et al., 2015; Spasojevic et al., 2000), and that PTSD couples would report a greater frequency of clinically significant problems across areas. For the third aim, we predicted Veterans’ and partners’ relationship quality scores would be significantly associated. In sum, the overarching goal is to extend the research on relationship discord in OEF/OIF Veterans by utilizing a well-normed, standardized assessment measure of relationship functioning to allow for identification of clinically significant levels of general and specific relationship distress.
Methods
Participants
As described in greater detail elsewhere (Caska et al., 2014), the 65 United States Veterans had deployed 1.5 times on average (SD = 0.64), mostly with the Army (77.7%), in Iraq (64%), Afghanistan (18.8%), or both (17.2%). Of these, 32 met criteria for PTSD. Ages of the Veterans with PTSD ranged from 24 to 53 (M = 32.7; SD = 7.6), and 94% were Caucasian. Their partners’ ages ranged from 19 to 49 (M = 31.1; SD = 8.2), and 84% were Caucasian. Of these couples, 84% were married and living together (M = 6.6 years); the rest were unmarried and living together (M = 2.3 years). These Veterans and partners had typically completed high school (28.2%) or some college (50%). The 33 Veterans in the comparison group ranged in age from 23 to 49 (M = 34.7; SD = 7.3), and their partners ranged in age from 21 to 47 (M = 32.1; SD = 8.1). Almost all were Caucasian (97% Veterans; 94% partners). All comparison group couples were married and living together (M = 9.0 years; SD = 7.3) and had typically completed college (31.8%) or some college (59.1%). Statistical control of education, household income, length of time living together, and number or location of deployments did not alter any results.
Given the focus of the overall study, potential participants were excluded if they had a history of cardiovascular disease or were taking related medications. Other exclusion criteria included active suicidality, homicidality, mania, psychosis, and/or alcohol/drug dependence within the last 3 months. For the PTSD group, Veterans were not excluded for other psychiatric diagnoses, given the typical comorbidity found in PTSD (Pietrzak, Goldstein, Southwick, & Grant, 2011). Of the 32 PTSD group Veterans, 28 reached diagnostic threshold for clinical PTSD, and four endorsed significant but slightly sub-threshold levels, as described below. Significant distress and impairment, aggression, and partner distress are found in Veterans with sub-threshold PTSD, similar to those meeting full criteria (e.g., Jakupcak et al., 2007).
For Veterans considered for the comparison group, those with any current Axis I disorder were excluded. For couples initially considered for either group, those in which partners met criteria for current PTSD from their own trauma history were excluded. Partners reporting PTSD symptoms related to the Veterans’ trauma or PTSD symptoms were not excluded. Please see the manuscript by Caska and colleagues (2014) for additional details regarding recruitment, screening, and selection.
Measures
Clinician Administered PTSD Scale
(CAPS; Blake et al., 1995). PTSD was assessed using this well-validated structured interview (Weathers, Ruscio, & Keane, 1999). The scoring rule of symptom frequency of at least 1 and intensity of at least 2 was used as a cutoff, combined with DSM-IV-TR (American Psychiatric Association, 1994) criteria specifying an index trauma, one Cluster B, three cluster C, and four cluster D symptoms, in addition to requirements for general distress/impairment. The four Veterans in the PTSD group with sub-threshold PTSD were either one point below the required intensity for one symptom or missing one required symptom in a cluster. Three, trained, graduate students independently re-rated a random subset (20%) of audiotaped interviews to determine the inter-rater reliability of PTSD diagnoses, according to DSM-IV-TR criteria. The inter-rater reliability for PTSD diagnosis (i.e., presence vs. absence) was Kappa = .83 (p < .01).
Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID)
(Research Version; First & Gibbon, 2004). The Patient and Non-Patient Editions of the SCID were used to evaluate inclusion and exclusion criteria. PTSD group Veterans completed the patient version; all other participants completed the non-patient version, focused on current Axis I disorders. For Veterans, the SCID assessment of PTSD focused on non-military traumas, as military-related traumas were assessed in the CAPS. A random sample of audio recorded SCID interviews was re-rated by another trained interviewer and Kappa estimates ranged from .74 – 1.00 (all ps < .05).
PTSD Checklist
(PCL; Weathers et al., 1993). This well-validated (Keane, Street, & Stafford, 2004) self-report scale of PTSD symptoms asks participants to respond in terms of the prior month. Veterans completed the military version, to assess symptom severity. A cutoff score of ≥ 35 was required for the PTSD group and ≤ 29 for the comparison group (Bliese et al., 2008).
Marital Satisfaction Inventory - Revised
(MSI-R; Snyder, 1997). This 150-item, true-false, self-report measure provides normed scores for global distress (GDS) and specific problem areas. The 13-item Affective Communication scale (AFC) assesses dissatisfaction with affection and understanding expressed by one’s partner. The 19-item Problem-Solving Communication scale (PSC) assesses difficulties resolving differences. The 10-item Aggression (AGG) scale assesses intimidation and physical aggression from one’s partner. The 10-item Time Together (TTO) scale assesses difficulties with companionship and shared activities. The 11-item Disagreement about Finances scale (FIN) assesses conflict about finances. The 13-item Sexual Dissatisfaction (SEX) scale assesses complaints about the frequency and quality of sexual activities. The 44 couples with children also completed the 10-item Conflict over Child Rearing scale (CCR), assessing disagreements about parenting. Raw scores were transformed to T-Scores using the published norms (Snyder, 1997), with scores of 50 – 60 reflecting a possible problem area, and scores above 60 reflecting a clear problem area. In the cutoff for membership in the discordant couple taxon, Whisman et al (2008) averaged the GDS, AFC, PSC, TTO, and SEX T-scores for both partners. Scores of 54T or greater are strongly related with taxon membership, with sensitivity, specificity, positive predictive power, and negative predictive power all exceeding .95 in ROC analyses. Internal consistencies for this sample are presented in Table 1.
Table 1.
Descriptive Information for Veterans and Partner MSI-R Scales
| Veterans | Partners | |||||
|---|---|---|---|---|---|---|
| Scale | Mean | SD | α | Mean | SD | α |
| Affective Communication (AFC) | 51.6 | 10.6 | .89 | 52.1 | 10.5 | .91 |
| Problem-Solving Communication (PSC) | 52.5 | 11.1 | .92 | 52.9 | 10.3 | .93 |
| Aggression (AGG) | 52.3 | 9.3 | .82 | 50.4 | 9.08 | .83 |
| Time Together (TTO) | 50.2 | 10.5 | .84 | 49.1 | 10.3 | .87 |
| Disagreement about Finances (FIN) | 51.7 | 10.6 | .81 | 51.5 | 9.9 | .83 |
| Sexual Dissatisfaction (SEX) | 47.5 | 10.2 | .89 | 48.4 | 9.7 | .84 |
| Conflict over Child Rearing (CCR) | 51.8 | 9.0 | .76 | 49.9 | 9.0 | .81 |
Procedure
The Institutional Review Boards of the University of Utah and the Salt Lake City Veterans Affairs Medical Center approved the protocol; Veterans and partners completed informed consent. PTSD group couples were recruited through the Salt Lake City VAMC, fliers, direct referral from mental health providers, and post-deployment workshops. Comparison couples were recruited through programs for Veterans and their families, and post-deployment workshops. Veterans recruited through the VAMC completed telephone screenings, and a medical record review of their initial PTSD evaluation was conducted. All other participants completed questionnaires to determine eligibility. Prior to a laboratory session, all participants completed a background questionnaire, the MSI-R, and PCL. Instructions stressed independent completion. Following a psychophysiological session (Caska et al., 2014), Veterans and partners participated in separate SCID interviews; Veterans also completed the CAPS. Participants were debriefed separately to address any sensitive concerns, including safety assessments. Referrals for individual or couples-based mental health services were provided to those interested.
Overview of Analyses
The first aim used Χ2 tests to examine differences between PTSD and comparison couples in the proportions reporting good, intermediate, and problematic relationship functioning on the GDS, as defined by the MSI-R norms (Snyder, 1997). The association of couple-based MSI-R taxon cut-off scores with PTSD was tested similarly to classify marital discord. For the second aim, we replicated prior research using continuous relationship quality scores, testing the hypotheses regarding levels of distress across specific problem areas using a (2) (Couple Type: PTSD vs. Comparison) x (2) (Role: Veteran vs. Partner) x (6) (Scale: AFC, PSC, AGG, TTO, FIN, SEX) mixed ANOVA. Treating Veterans and Partners as two levels of the repeated factor “Role” fully accommodates dyadic data and permits direct tests of differences between Veterans and partners (Kenny, Kashy, & Cook, 2006). Treating the six subscales as the repeated factor “Scale” accommodates correlations among problem area scores, as well as their nesting within members of the dyad, and permits direct tests of the pattern of the relative elevation (i.e., severity) across these domains, as well as differences in those profile configurations as a function of Couple Type (i.e., PTSD vs. Comparison) and Role in the dyad (i.e., Veteran vs. Partner).
In this analysis, the main effect for Couple Type indicates a difference between PTSD couples and comparisons in overall problem severity, averaging across problem areas (i.e., overall profile elevation or severity) and across Veterans and their partners. A significant Couple Type by Scale interaction indicates that the magnitude of the difference between PTSD couples and comparisons, averaging scores across Veterans and their partners, varies across the six problem domains. Significant interactions with the Role factor indicate varying patterns of difficulties for Veterans versus partners. In effects for the Scale factor, Mauchly’s test of sphericity was significant, Χ2(14) = 49.3, p < .001. Therefore, MANOVA tests were utilized. Following interactions involving the Scale factor, univariate Couple Type by Role ANOVAs of individual scales were conducted. Individual mean differences were tested using the appropriate error mean square (Bernhardson, 1975). Effect sizes are reported as partial eta-squared (η2p).
The second aim also utilized Χ2 tests to identify associations of PTSD with Veterans’ and partners’ scores on specific problems that reflect good, intermediate, and clearly problematic ranges in MSI-R norms (Snyder, 1997). For the third aim, Pearson correlations tested Veterans’ and partners’ agreement on continuous scores and ordinal correlations tested agreement on problem area categories of good, intermediate, and problematic functioning. Differences in agreement levels between PTSD and comparison group couples were tested by examining contrasts between independent correlations. The CCR scale was examined separately in the 44 couples with children, using similar analyses.
Results
As reported elsewhere (Caska et al., 2014), PTSD group Veterans reported higher PTSD symptoms than comparisons, reflecting moderate to severe severity on the PCL and CAPS. As reported previously, large Couple Type differences on continuous GDS scores indicated moderate couple distress in the PTSD group and normal levels in comparison couples.
Categories of Overall Couple Distress
In new analyses to identify the frequency of meaningful levels of overall couple distress, GDS scores were categorized in the good, intermediate, and problematic ranges using published norms (Snyder, 1997). Veterans with PTSD reported a greater frequency of elevated scores (Good: 15.6%; Intermediate: 34.4%; Problematic: 50%) than did comparison group Veterans (Good: 60.6%; Intermediate: 34.4%; Problematic: 6.1%), Χ2 (2) = 19.88, p < .001, as did partners in the PTSD (Good: 18.8%; Intermediate: 40.6%; Problematic: 40.6%) versus comparison groups (Good: 48.5%; Intermediate: 48.5%; Problematic: 3.0%), Χ2 (2) = 15.13, p = .001.
Using the established taxometric cutoff (Whisman et al., 2008), 69% of PTSD couples were in the discordant group (vs. 31% non-discordant), compared to 9% of the comparison group couples (vs. 91% non-discordant), Χ2(1) = 24.4, p < .0001. The higher prevalence of discordant taxon membership as compared to MSI-R norms reflects the fact that the mean T-score required for taxon membership (i.e., 54T) falls within the MRI-R intermediate problem range.
Problem Area Differences between PTSD and Comparison Group Couples
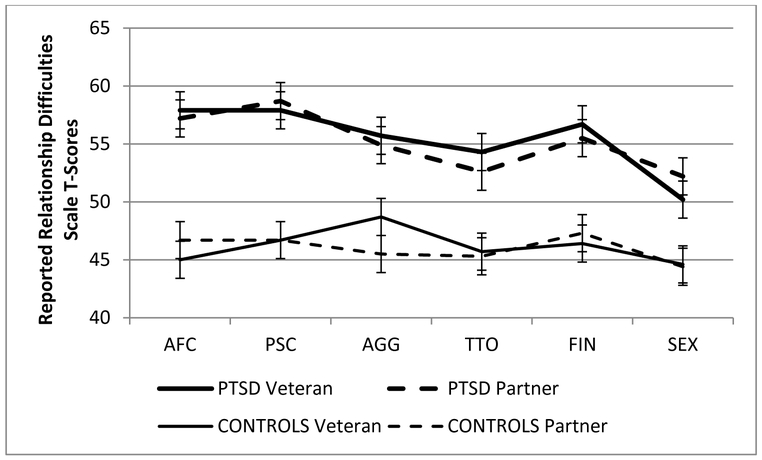
In the Couple Type x Role x Scale mixed ANOVA, a significant main effect for Couple Type, F(1, 58) = 35.98, p < .001, η2p = .38, indicated that, averaging across the six subscales and across Veterans and partners, PTSD couples reported greater relationship distress than comparison group couples (means = 55.3 vs. 46.1, SEs = 1.07 vs. 1.11). That is, the overall profile of scores across problem areas was elevated in PTSD couples. In a significant Couple Type x Scale interaction, Wilk’s λ = .80, F(5, 54) = 2.69, p = .03, η2p = .20, (see Table 2), the differences between PTSD and comparison group couples varied across scales. Couple Type x Role mixed ANOVAs for each scale are reported in Table 2. The largest Couple Type effects in terms of effect size and scale elevations were AFC and PSC, with smaller effects for FIN, AGG, TTO, and SEX. The Couple Type and Couple Type x Scale effects were not qualified by interactions with Role, both p > .18, both η2p < .11. Hence, as depicted in Figure 1, group differences were virtually identical for Veterans and their partners. In an analysis of the CCR scale, PTSD couples reported greater difficulties in child rearing than did comparisons (Means = 54.4 vs. 47.9, SEs = 1.55, 1.41), F(1,42) = 9.67, p = .003, η2p = .19.
Table 2.
Couple Mean Standardized Scores and Differences Between PTSD and Comparison Groups
| MSI-R Subscale | PTSD Mean (SE) |
COMPARISON Mean (SE) |
F(1, 59) | η2p |
|---|---|---|---|---|
| Affective Communication (AFC) | 57.5a (1.29) | 46.2c (1.37) | 37.44** | .36 |
| Problem Solving Communication (PSC) | 58.3a (1.37) | 49.0c (1.41) | 35.22** | .36 |
| Aggression (AGG) | 55.3ab (1.22) | 47.8c (1.18) | 20.72** | .24 |
| Time Together (TTO) | 53.5b (1.56) | 45.9c (1.51) | 17.79** | .22 |
| Disagreement about Finances (FIN) | 56.1a (1.46) | 46.9c (1.51) | 20.52** | .26 |
| Sexual Dissatisfaction (SEX) | 51.2b (1.47) | 44.3c (1.45) | 11.76* | .16 |
Note. Means with different subscripts differ across scales and between groups, p < .05.
p < .002.
p < .001. PTSD = posttraumatic stress disorder; MSI-R = Marital Satisfaction Inventory – Revised.
Figure 1.
Means (SEs) for Veterans’ and Partners’ Scores on the MSI-R Scales. Affective Communication (AFC), Problem-Solving Communication (PSC), Aggression (AGG), Time Together (TTO), Disagreement about Finances (FIN), and Sexual Dissatisfaction (SEX) Scale‘s.
Note. AFC = Affective Communication; PSC = Problem-Solving Communication; AGG = Aggression; TTO = Time Together; FIN = Disagreement about Finances; SEX = Sexual Dissatisfaction.
The percentage of scores in good, intermediate, and problematic MSI-R ranges for each area, and comparisons between PTSD and comparison group couples, are presented in Table 3. Generally, a substantial majority of PTSD Veterans and partners reported problems of intermediate or clear clinical concern, significantly more so than comparison couples. The one exception, conflicts regarding child rearing, may be due to the smaller sample size.
Table 3.
Percentage of Veterans and Partners Scoring in the Good, Intermediate, and Problematic Range, and Chi-square for Differences Between PTSD and Comparison Groups
| Veterans | Partners | |||
|---|---|---|---|---|
| Affective Communication | PTSD | Comparison | PTSD | Comparison |
| Good | 6.2 | 78.8 | 21.9 | 78.1 |
| Intermediate | 59.4 | 15.1 | 37.5 | 12.5 |
| Problematic | 34.4 | 6.1 | 40.6 | 9.4 |
| Χ2 (2) = 36.0, p <.001 | Χ2 (2) = 20.4, p <.001 | |||
| Problem Solving Communication | ||||
| Good | 18.8 | 69.7 | 18.8 | 69.7 |
| Intermediate | 34.4 | 21.2 | 28.1 | 27.3 |
| Problematic | 46.8 | 9.1 | 53.1 | 3.0 |
| Χ2 (2) = 18.8, p <.001 | Χ2 (2) = 24.2, p <.001 | |||
| Aggression | ||||
| Good | 25.0 | 63.6 | 25.0 | 78.8 |
| Intermediate | 53.1 | 18.2 | 46.9 | 18.2 |
| Problematic | 21.9 | 18.2 | 28.1 | 3.0 |
| Χ2 (2) = 11.2, p = .004 | Χ2 (2) = 19.8, p <.001 | |||
| Time Together | ||||
| Good | 28.1 | 63.6 | 31.2 | 69.7 |
| Intermediate | 40.6 | 30.3 | 34.4 | 24.2 |
| Problematic | 31.3 | 6.1 | 34.4 | 6.1 |
| Χ2 (2) = 10.5, p = .005 | Χ2 (2) = 11.8, p = .003 | |||
| Disagreement about Finances | ||||
| Good | 25.0 | 75.0 | 32.3 | 71.0 |
| Intermediate | 34.4 | 15.6 | 35.4 | 25.8 |
| Problematic | 40.6 | 9.4 | 32.3 | 3.2 |
| Χ2 (2) = 16.5, p <.001 | Χ2 (2) = 12.3, p = .002 | |||
| Sexual Dissatisfaction | ||||
| Good | 37.5 | 72.7 | 40.6 | 78.8 |
| Intermediate | 43.8 | 18.2 | 37.5 | 18.2 |
| Problematic | 18.7 | 9.1 | 21.9 | 3.0 |
| Χ2 (2) = 8.2, p = .017 | Χ2 (2) = 10.8, p = .004 | |||
| Conflict over Child Rearing | ||||
| Good | 34.5 | 62.5 | 25.0 | 62.5 |
| Intermediate | 47.8 | 29.2 | 55.0 | 33.3 |
| Problematic | 17.4 | 8.3 | 20.0 | 4.2 |
| Χ2 (2) = 3.67, p = .16 | Χ2 (2) = 6.97, p = .03 | |||
Couple Agreement on Problems
The correlation of Veterans’ and partners’ continuous GDS scores was r(64) = .71, p < .001; the ordinal correlation between their GDS categories (i.e., good, intermediate, problematic) was ρ(64) = .64, p < .001. For the continuous problem area scores, correlations between Veterans and partners were as follows: AFC, r(64) = .56, p < .01; PSC, r(64) = .62, p < .01; AGG, r(64) = .34, p < .01, TTO, r(64) = .66, p < .01, FIN, r(64) = .66, p < .01, SEX, r(64) = .50, p < .01; CCR, r(44) = .41, p < .01. For the categorical problem scores, the correlations were: AFC, ρ(64) = .52, p < .01; PSC, ρ(64) = .62, p < .01; AGG, ρ(64) = .32, p < .01; TTO, ρ(64) = .58, p < .01, FIN, ρ(64) = .62, p < .01; SEX, ρ(64) = .60, p < .01, and CCR, ρ(44) = .35, p < .05. PTSD and comparison group couples did not differ on these levels of agreement. Thus, Veterans and partners generally agreed on presence and severity of overall distress and specific problems.
Discussion
In a substantial body of previous research, Posttraumatic Stress Disorder (PTSD) is associated with lower levels of general romantic relationship quality and elevated reports of aggressive conflict and intimate partner violence (Lambert et al., 2012; Taft et al., 2011). Studies of other relationship content areas indicate that Veterans with PTSD and their partners also report a wide variety of specific couple problems. However, examination of associations with continuous measures of relationship quality make it difficult to determine the clinical significance or implications of these effects, especially when investigations rely upon research measures of relationship quality that lack adequate normative information. Standardized, well-normed assessments of overall relationship quality and multiple problem areas could provide information about more precisely defined clinically significant concerns for these couples.
In a previous report from this sample using continuous relationship quality scores, Veterans with PTSD and their partners reported higher general relationship distress, lower general affection and warmth, and higher general conflict relative to comparisons (Caska et al., 2014). The present results extend those findings and other research on PTSD and intimate relationships in Veterans by providing preliminary evidence of a much higher frequency of clinically significant relationship distress and higher levels of clear difficulties in several specific relationship domains, using a well-validated and standardized measure with considerable normative information (Snyder, 1997) and multi-modal diagnostic assessment of PTSD.
For overall couple distress, PTSD couples were several times more likely than comparison couples to score in the clearly problematic range for the MSI-R global distress norms and for the marital discord taxon (Whisman et al., 2008). In terms of effect sizes and scale elevations for specific problems, difficulties in affective and problem-solving communication are perhaps the most noteworthy, followed closely by aggressive behavior, disagreements about finances, and dissatisfaction surrounding leisure time together. Consistent with prior studies (LaMotte et al., 2015; Nunnink, Goldwaser, Afari, Nievergelt, & Baker, 2010), Veterans with PTSD and their partners also reported greater sexual dissatisfaction, although this was a somewhat less pronounced problem. For couples with children, the PTSD group reported greater conflicts over child rearing than did comparisons, which is consistent with prior research documenting greater parenting stress among couples who have experienced trauma (Gewirtz, Polusny, DeGarmo, Khaylis, & Erbes, 2010). In analyses of categories of problem severity, PTSD was generally associated with considerably higher prevalence of scores in the intermediate and clearly problematic range. Thus, PTSD couples reported pronounced difficulties for general distress and across a broad range of relationship domains, a conclusion strengthened by the multi-method documentation of clinically meaningful levels of PTSD severity, use of a well-validated and standardized measure of relationship functioning, and an examination of the frequency with which Veterans and their partners reported clinically elevated levels of distress.
There are several factors that may account for PTSD couples experiencing greater difficulties in these multiple domains, including interactions between factors at the level of PTSD, the relationship, and other emotional and behavioral health factors of each individual partner (Campbell & Renshaw, 2018). Nelson Goff and Smith’s Couples Adaptation to Traumatic Stress Model (2005) highlights the interactions among acute and chronic factors of the trauma survivor and their partner, individual predisposing factors and coping resources, and multiple aspects of couple functioning. These complex interactions explain generally why couples present with more clinically significant distress. Prior research documenting that emotional numbing, avoidance, and hyperarousal symptoms, in particular, are associated with greater difficulties in affective expression and communication, with emotional and physical intimacy, and with parenting stress (Campbell & Renshaw, 2018) further supports our findings of clinically significant distress in these areas.
Patterns of difficulties were quite similar for Veterans and their partners, and correlations between spouse reports suggested agreement in their views, which may bode well for couple therapy (Biesen & Doss, 2013). There was less agreement on reports of difficulties with aggression and child rearing. The low correlation for AGG scores is somewhat ambiguous, as the respondents are asked to report on the other partners’ behavior. Hence, a low correlation could reflect aggressive behavior limited to one partner. However, low agreement between Veterans and their partners has been found in parallel ratings of their own and the other partners’ aggressive behavior (e.g., LaMotte, Taft, Reardon, & Miller, 2014). The use of the MSI-R in couple assessments could be useful by providing not only well-normed information about the presence of specific couple difficulties, but patterns of couple (dis)agreement, as well.
Limitations and Qualifications
There are important limitations of these findings. The generalizability is limited by the small, mostly Caucasian sample of heterosexual couples consisting of male Veterans with female partners. Moreover, there may be self-selection biases in the Veterans who present to the VAMC for care and who attend post-deployment workshops, where participants were recruited, which could further limit generalizability to the larger population of Veteran couples. These limitations underscore the importance of replications with larger and more diverse samples. The results suggest a considerably elevated prevalence of clinically significant relationship discord in PTSD couples, but the very small sample renders this as a preliminary estimate of difficulties in the OEF/OIF population. Also, the cross-sectional design precludes interpretations regarding causal associations of PTSD with couple difficulties, although PTSD predicts subsequent couple difficulties (Erbes, Meis, Polusny, Compton, & Wadsworth, 2012; Fredman et al., 2016).
The self-report nature of the MSI-R is also a limitation, as respondents may not be fully willing or able to describe relationships accurately. However, behavioral assessments of marital conflict discussions in this sample provide converging evidence of dysfunction in the PTSD couples (Caska et al., 2014). By including Veterans with PTSD who had typical comorbid psychological problems (Pietrzak et al., 2011), couple type differences might reflect other conditions, as opposed to PTSD, specifically. However, it is important to emphasize that the close conceptual and empirical ties between PTSD and several such factors (e.g., depression, anger, aggressiveness) suggest that efforts to disentangle overlapping risks for relationship difficulties will be challenging and potentially misleading (Campbell & Renshaw, 2018).
Importantly, although these preliminary results suggest the value of standardized couple assessments in PTSD, direct tests of their incremental validity and utility are needed (Hunsley & Meyer, 2003). Finally, the length of the MSI-R might preclude its use in some applications, such as larger scale efforts to determine the prevalence of clinically significant relationship difficulties among Veterans with PTSD or in screening. However, a 10-item measure derived from the MSI-R items has a strong association with discordant versus non-discordant marital taxon status (Whisman, Snyder, & Beach, 2009).
Conclusions and Implications
These limitations notwithstanding, the present findings suggest that a well-normed and standardized relationship assessment device replicates prior research on overall relationship distress and specific couple problems associated with PTSD. Importantly, because of the availability of norms (Snyder, 1997) and empirically established cutoffs for membership in a qualitatively distinct marital discord group (Whisman et al., 2008), this measure has additional advantages in identifying both overall distress levels and a broad range of specific problems that may fall within the range of clinical concern. With the limitations of the small and select sample appropriately emphasized, these preliminary findings suggest that in the well-established general association between PTSD and couple functioning (Lambert et al., 2012; Taft et al., 2011), diagnosed PTSD may be associated with clinically significant relationship distress in a majority of couples and may reflect notable difficulties across a broad range of relationship problems. Fortunately, Veterans and their partners generally agree about the presence and severity of such concerns. If these results are replicated and extended in more representative samples and with direct tests of assessment utility, current approaches to clinical care for Veterans with PTSD and their partners could be augmented by appropriate standardized screening and assessment of general couple distress and of multiple domains of relationship functioning.
For individual couples, using standardized measures routinely could increase the likelihood that clinically significant relationship distress is accurately identified, in terms of severity and manifestations across multiple relationship domains. Many VAMCs aim to provide a range of family services, from brief consultation and workshops, to more intensive couple and family therapies. Accurately assessing clinical severity and domains of relationship distress could assist in triaging couples to the most appropriate clinical services and in developing treatment goals. More routine use of screening versions of these assessments (e.g., Whisman et al., 2009) could also guide policy decisions about resource allocation by providing accurate estimates of the prevalence of significant couple issues among Veterans with PTSD. Finally, the use of such measures is consistent with the VA Central Office’s national initiative to implement measurement-based care as a routine standard of practice within mental health treatment (U.S. Department of Veterans Affairs, 2016).
Well-normed inventories such as the MSI-R may be useful, especially in the context of integrative couple assessments, providing feedback on relationship functioning, and prioritizing treatment goals (Snyder, Heyman, & Haynes, 2005). Of course, levels of distress falling below established norms and cutoffs for significant concern might still warrant attention. However, these results suggest that clearly problematic couple functioning is considerably more common in PTSD. Again, pending replication and extension, these results not only support the more routine consideration of couple issues in PTSD but also support the emphasis that current couple interventions for this population (Monson et al., 2012) place on affective and problem-solving communication, reduction of aggressive behavior and conflicts about finances and parenting, and enhancement of sexual functioning and leisure time.
Public Significance Statement.
This study highlights the potential benefit of using standardized measures of relationship functioning to assess the relationship satisfaction of Veterans with PTSD and their partners. This allows clinicians and researchers to compare the degree of relationship distress against a large database of couples, and published normative data, to more specifically describe the clinical severity of relationship problems in Veteran couples and to better identify couples in need of services. Additionally, this study advances prior research by using a standardized, normed, measure to document that Iraq and Afghanistan Veterans with PTSD and their partners experience relationship distress that falls within a high range of clinical severity, across several different areas of relationship functioning, and as compared to couples where the Veteran does not have PTSD or any other mental health diagnosis.
Acknowledgments
The research reported in this article was supported in part by National Institute of Mental Health Grant 1F31MH091915-01A1.
Contributor Information
Catherine M. Caska-Wallace, Mental Health Service, VA Puget Sound Health Care System – Seattle Division and Department of Psychiatry and Behavioral Sciences, University of Washington
Timothy W. Smith, Department of Psychology, University of Utah
Keith D. Renshaw, Department of Psychology, George Mason University
Steven N. Allen, PTSD Clinical Team, VA Salt Lake City Health Care Team
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th edition). Washington, DC: American Psychiatric Association. [Google Scholar]
- Balderrama-Durbin C, Cigrang JA, Osborne LJ, Snyder DK, Talcott GW, Slep AMS, ... & Sonnek S (2015). Coming home: A prospective study of family reintegration following deployment to a war zone. Psychological Services, 12, 213–221. doi: 10.1037/ser0000020. [DOI] [PubMed] [Google Scholar]
- Beach SRH, Fincham FD, Amir N, & Leonard KE (2005). The taxometrics of marriage: Is marital discord categorical? Journal of Family Psychology, 19, 276–285. doi: 10.1037/0893-3200.19.2.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernhardson CS (1975). Type I error rates when multiple comparisons follow a significant F test in AVOVA. Biometrics, 31, 229–232. doi: 10.1007/bf02105408 [DOI] [Google Scholar]
- Berz JB, Taft CT, Watkins LE, & Monson CM (2008). Associations between PTSD symptoms and parenting satisfaction in a female veteran sample. Journal of Psychological Trauma, 7, 37–45. doi: 10.1080/19322880802125969 [DOI] [Google Scholar]
- Biesen JN, & Doss BD (2013). Couple’s agreement on presenting problems predicts engagement and outcomes in problem-focused couple therapy. Journal of Family Psychology, 27, 658–663. doi: 10.1037/a0033422 [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8, 75–90. doi: 10.1007/BF02105408 [DOI] [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, & Hoge CW (2008). Validating the Primary Care Posttraumatic Stress Disorder Screen and the Posttraumatic Stress Disorder Checklist with soldiers returning from combat. Journal of Consulting and Clinical Psychology, 76, 272–281. doi: 10.1037/0022-006x.76.2.272 [DOI] [PubMed] [Google Scholar]
- Campbell SB, & Renshaw KD (2018). Posttraumatic stress disorder and relationship functioning: A comprehensive review and organizational framework. Clinical Psychology Review, 65, 152–162. doi: 10.1016/j.cpr.2018.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caska CM, Smith TW, Renshaw KD, Allen SN, Uchino BN, Birmingham W, & Carlisle M (2014). Posttraumatic stress disorder and responses to couple conflict: Implications for cardiovascular risk. Health Psychology, 33, 1273–1280. doi: 10.1037/hea0000133 [DOI] [PubMed] [Google Scholar]
- Erbes CR, Meis LA, Polusny MA, Compton JS, & Wadsworth SM (2012). An examination of PTSD symptoms and relationship functioning in U.S. soldiers of the Iraq war over time. Journal of Traumatic Stress, 25, 187–190. doi: 10.1002/jts.21689. [DOI] [PubMed] [Google Scholar]
- First MB, & Gibbon M (2004). The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). In Hilsenroth MJ & Segal DL (Eds.), Comprehensive handbook of psychological assessment, Vol. 2: Personality assessment (pp. 134–143). Hoboken, NJ: John Wiley & Sons Inc. [Google Scholar]
- Fredman SJ, Beck JG, Shnaider P, Le Y, Pukay-Martin ND, Pentel KZ, & Monson CM (2016). Longitudinal associations between PTSD symptoms and dyadic conflict communication following severe motor vehicle accident. Behavior Therapy, 48, 235–246. doi: 10.1016/j.beth.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, & Erbes CR (2010). Posttraumatic stress symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of consulting and clinical psychology, 78(5), 599. doi: 10.1037/a0020571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrick SS, Dicke A, & Hendrick C (1998). The relationship assessment scale. Journal of social and personal relationships, 15(1), 137–142. doi: 10.1177/0265407598151009 [DOI] [Google Scholar]
- Herrington RL, Mitchell AE, Castellani AM, Joseph JI, Snyder DK, & Gleaves DH (2008). Assessing disharmony and disaffection in intimate relationships: Revision of the Marital Satisfaction Inventory factor scales. Psychological Assessment, 20, 341–350. doi: 10.1037/a0013759 [DOI] [PubMed] [Google Scholar]
- Hunsley J, & Meyer GJ (2003). The incremental validity of psychological testing and assessment: Conceptual, methodological, and statistical issues. Psychological Assessment, 15, 446–455. doi: 10.1037/1040-3590.15.4.446 [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Conybeare D, Phelps L, Hunt S, Holmes HA, Felker B, Klevens M, & McFall ME (2007). Anger, hostility, and aggression among Iraq and Afghanistan war Veterans reporting PTSD and subthreshold PTSD. Journal of Traumatic Stress, 20, 945–954. doi: 10.1002/jts.20258 [DOI] [PubMed] [Google Scholar]
- Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, & Weiss DS (1992). Problems in families of male Vietnam veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 60(6), 916–926. doi: 10.1037/0022-006X.60.6.916 [DOI] [PubMed] [Google Scholar]
- Keane TM, Street AE, & Stafford J (2004). The Assessment of Military-Related PTSD. In Wilson JP & Keane TM (Eds.), Assessing psychological trauma and PTSD (2nd ed.). (pp. 262–285). New York, NY: Guilford Press. [Google Scholar]
- Kenny DA, Kashy DA, & Cook WL (2006). Dyadic data analysis. New York, NY: Guilford. [Google Scholar]
- Lambert JE, Engh R, Hasbun A, & Holzer J (2012). Impact of Posttraumatic Stress Disorder on the relationship quality and psychological distress of intimate partners: A meta-analytic review. Journal of Family Psychology, 26, 729–737. doi: 10.1037/a0029341 [DOI] [PubMed] [Google Scholar]
- LaMotte AD, Taft CT, Reardon AF, & Miller MW (2014). Agreement between veteran and partner reports of intimate partner aggression. Psychological Assessment, 26, 1369–1374. doi: 10.1037/pas0000018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMotte AD, Taft CT, Reardon AF & Miller MW (2015). Veterans’ PTSD symptoms and their partners’ desired changes in key relationship domains. Psychological Trauma: Theory, Research, Practice, and Policy, 7, 479–484. doi: 10.1037/tra0000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin Y, Greene T, & Solomon Z (2016). PTSD symptoms and marital adjustment among ex-POWs’ wives. Journal of Family Psychology, 30, 72–81. doi: 10.1037/fam0000170. [DOI] [PubMed] [Google Scholar]
- Meis L, Barry R, Kehle S, Erbes C, & Polusny M (2010). Relationship adjustment, PTSD symptoms, and treatment utilization among coupled National Guard soldiers deployed to Iraq. Journal of Family Psychology, 24, 560–567. doi: 10.1037/a0020925. [DOI] [PubMed] [Google Scholar]
- Monson CM, Fredman SJ, Macdonald A, Pukay-Martin ND, Resick PA, & Schnurr PP (2012). Effect of Cognitive-Behavioral Couple Therapy for PTSD: A randomized controlled trial. Journal of the American Medical Association, 308, 700–709. doi: 10.1001/jama.2012.9307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson Goff BS, & Smith DB (2005). Systemic traumatic stress: The couple adaptation to traumatic stress model. Journal of Marital and Family Therapy, 31, 145–157. doi: 10.1111/j.1752-0606.2005.tb01552.x [DOI] [PubMed] [Google Scholar]
- Nunnink SE, Goldwaser G, Afari N, Nievergett CM, & Baker DG (2010). The role of emotional numbing in sexual functioning among Veterans of the Iraq and Afghanistan wars. Military Medicine, 175, 424–428. doi: 10.7205/MILMED-D-09-00085 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25, 456–465. doi: 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, & Marmar CR (2009). Trends and risk factors for mental health diagnoses among Iraq and Afghanistan Veterans using Department of Veterans Affairs health care, 2002–2008. American Journal of Public Health, 99, 1651–1658. doi: 10.2105/AJPH.2008.150284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder DK (1997). Marital Satisfaction Inventory, Revised (MSI-R). Los Angeles: Western Psychological Services. [PubMed] [Google Scholar]
- Snyder DK, Heyman RE, & Haynes SN (2005). Evidence-based approaches to assessing couple distress. Psychological Assessment, 17, 288–307. doi: 10.1037/1040-3590.17.3.288 [DOI] [PubMed] [Google Scholar]
- Solomon Z, Dekel R, & Zerach G (2008). The relationships between posttraumatic stress symptom clusters and marital intimacy among war veterans. Journal of Family Psychology, 22, 659–666. doi: 10.1037/a0013596 [DOI] [PubMed] [Google Scholar]
- Spanier GB (1976). Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and Family, 38, 15–28. doi: 10.2307/350547 [DOI] [Google Scholar]
- Spasojevic J, Heffer RW, & Snyder DK (2000). Effects of posttraumatic stress and acculturation on marital functioning in Bosnian refugee couples. Journal of Traumatic Stress, 13, 205–217. doi: 10.1023/A:1007750410122 [DOI] [PubMed] [Google Scholar]
- Straus MA (1979). Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family, 41, 75–88. doi: 10.2307/351733 [DOI] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, & Monson CM (2011). Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology, 79, 22–33. doi: 10.1037/a0022196 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. (2016, May). Measurement Based Care (MBC) in Mental Health Initiative. Washington, D.C.: Author. Retrieved from https://www.mirecc.va.gov/visn4/docs/MBCinMHInitiative.pdf. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the annual meeting of the International Society for Traumatic Stress Studies, San Antonio, TX, San Antonio, TX. [Google Scholar]
- Weathers FW, Ruscio AM, & Keane TM (1999). Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment, 11, 124–133. doi: 10.1037/1040-3590.11.2.124 [DOI] [Google Scholar]
- Whisman MA, Beach SRH, & Snyder DK (2008). Is marital discord taxonic and can taxonic status be assessed reliably? Results from a national, representative sample of married couples. Journal of Consulting and Clinical Psychology, 76, 745–755. doi: 10.1037/0022-006X.76.5.745 [DOI] [PubMed] [Google Scholar]
- Whisman MA, Snyder DK, & Beach SRH (2009). Screening for marital and relationship discord. Journal of Family Psychology, 23, 247–254. doi: 10.1037/a0014476 [DOI] [PubMed] [Google Scholar]