Abstract
STUDY QUESTION
How is the semen quality of sexually active men following recovery from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection?
SUMMARY ANSWER
Twenty-five percent of the men with recent SARS-Cov-2 infections and proven healing were oligo-crypto-azoospermic, despite the absence of virus RNA in semen.
WHAT IS KNOWN ALREADY
The presence of SARS-CoV-2 in human semen and its role in virus contagion and semen quality after recovery from coronavirus disease 2019 (COVID-19) is still unclear. So far, studies evaluating semen quality and the occurrence of SARS-CoV-2 in semen of infected or proven recovered men are scarce and included a limited number of participants.
STUDY DESIGN, SIZE, DURATION
A prospective cross-sectional study on 43 sexually active men who were known to have recovered from SARS-CoV2 was performed. Four biological fluid samples, namely saliva, pre-ejaculation urine, semen, and post-ejaculation urine, were tested for the SARS-CoV-2 genome. Female partners were retested if any specimen was found to be SARS-CoV-2 positive. Routine semen analysis and quantification of semen leukocytes and interleukin-8 (IL-8) levels were performed.
PARTICIPANTS/MATERIALS, SETTING, METHODS
Questionnaires including International Index of Erectile Function and Male Sexual Health Questionnaire Short Form were administered to all subjects. The occurrence of virus RNA was evaluated in all the biological fluids collected by RT-PCR. Semen parameters were evaluated according to the World Health Organization manual edition V. Semen IL-8 levels were evaluated by a two-step ELISA method.
MAIN RESULTS AND THE ROLE OF CHANCE
After recovery from COVID-19, 25% of the men studied were oligo-crypto-azoospermic. Of the 11 men with semen impairment, 8 were azoospermic and 3 were oligospermic. A total of 33 patients (76.7%) showed pathological levels of IL-8 in semen. Oligo-crypto-azoospermia was significantly related to COVID-19 severity (P < 0.001). Three patients (7%) tested positive for at least one sample (one saliva; one pre-ejaculation urine; one semen and one post-ejaculation urine), so the next day new nasopharyngeal swabs were collected. The results from these three patients and their partners were all negative for SARS-CoV-2.
LIMITATIONS, REASONS FOR CAUTION
Although crypto-azoospermia was found in a high percentage of men who had recovered from COVID-19, clearly exceeding the percentage found in the general population, the previous semen quality of these men was unknown nor is it known whether a recovery of testicular function was occurring. The low number of enrolled patients may limit the statistical power of study.
WIDER IMPLICATIONS OF THE FINDINGS
SARS-CoV-2 can be detected in saliva, urine, and semen in a small percentage of men who recovered from COVID-19. One-quarter of men who recovered from COVID-19 demonstrated oligo-crypto-azoospermia indicating that an assessment of semen quality should be recommended for men of reproductive age who are affected by COVID-19.
STUDY FUNDING/COMPETING INTEREST(S)
None.
TRIAL REGISTRATION NUMBER
N/A.
Keywords: COVID-19, coronavirus disease 2019, semen, oligo-crypto-azoospermia, fertility, sexual transmission, SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
Introduction
The world is currently experiencing the outbreak of coronavirus disease (COVID-19) infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The virus exhibits a strong infectivity with a low virulence compared to previous coronavirus strains, and a higher fatality rate in men than in women (COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU), 2020). Widespread contact tracing followed by hospital isolation or quarantine is recommended to contain the outbreak (Swerdlow and Finelli, 2020).
Human-to-human transmission of SARS-CoV-2 usually occurs within households, including relatives and friends who are in intimate contact with symptomatic or incubating patients (Pan et al., 2020). In some patients, blood samples showed positive RT-PCR test results, suggesting that infection may be occasionally systemic (Wang et al., 2020). Respiratory droplets and physical contact of contaminated surfaces are the confirmed transmission modality of SARS-CoV-2 (Rothe et al., 2020), even if the virus has also been detected in saliva (To et al., 2020), teardrops, urine, and stool (Peng et al., 2020).
The occurrence of viral genomes in semen of infected men, previously not identified as being sexually transmitted, has been reported for Ebola and Zika (Feldmann, 2018). The high expression of angiotensin-converting enzyme (ACE) and transmembrane serine protease 2 (TMPRSS2) in somatic and germ cells of the testis suggests that SARS-CoV-2 virus may localize in the gonad (Wang and Xu, 2020). A recent study (Rastrelli et al., 2020) demonstrated the development of hypergonadotrophic hypogonadism in patients with active COVID-19 infection, suggesting an impairment of Leydig cell function, although whether this impairment is related to localization of the virus in the testis is unknown. However, in view of the essential role played by testosterone in spermatogenesis (Smith and Walker, 2014), alterations of semen quality in patients with COVID-19 can be hypothesized. In addition, semen parameters may be compromised by the inflammatory condition occurring in men with COVID-19.
Few studies have evaluated the presence of the virus in human semen. Paoli et al. reported the absence of SARS-CoV-2 RNA in semen and urine samples 13 days after COVID-19 diagnosis and 4 days after the second negative nasopharyngeal (NP) swab in a single patient who tested positive for SARS-CoV-2 through a NP-swab (PaoLi et al., 2020). Li et al. (2020) demonstrated that the semen of six patients tested positive for SARS-CoV-2, with four of these patients at the acute stage of infection and two at 2 and 3 days after clinical recovery, respectively. Pan et al. (2020) did not find viral RNA in any of 34 semen samples from males with active infection. Similarly, Song et al. (2020) demonstrated no detectable SARS-CoV-2 RNA in semen samples collected from 12 patients during the recovery phase: after 1–16 days from the second negative NP swab and 14–42 days after acute infection (Song et al., 2020). Only two studies (Guo et al., 2020; Ma et al., 2020) evaluated semen quality in a small cohort of men during infection or in the recovery phase of COVID-19.
In the present study, we investigated the direct (RNA) presence of SARS-CoV-2 in saliva, urine, and semen; evaluated semen parameters; and investigated semen IL-8 levels as a surrogate marker of the male genital tract inflammatory condition (Lotti et al., 2011) of 43 sexually active men with laboratory evidence of recovery from COVID-19.
Materials and methods
Study population and design
This prospective cohort study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. All male patients with SARS-CoV-2 infection, confirmed using molecular methods on respiratory specimens, were identified. Sexually active men aged 18–65 years with proven recovery from SARS-CoV2 infection (two consecutive negative NP-swabs for SARS-CoV2 RNA) were eligible for the study (World Health Organization, 2020). Men without sexual activity or with ejaculatory disorders, being treated with prostatic surgery or alpha-blockers and those with an inability to express informed consent were excluded from the study. All the partners of the enrolled patients were tested for SARS-CoV-2 positivity (NP swabs) at the time of the original diagnosis of the men and retested according to National Health Care System criteria until NP-swab double negativity, as suggested by World Health Organization (WHO) on clinical management of COVID-19 (WHO, 2020).
Moreover, if one or more specimens collected from the patients enrolled during the study were positive, partners were retested.
Ethics
The study was carried out with the approval of the local Ethics Committee (Rif: CEAVC17104) and registered on clinicaltrial.gov (Rif: NCT04446169), in compliance with the Declaration of Helsinki. All enrolled men provided written informed consent.
Clinical data and specimen collection
Clinical data included patient demographics, comorbidities, medications, hospitalization time and features (including intensive care need), and laboratory tests and treatments (including oxygen therapy). Moreover, patients were asked to fill out questionnaires, including International Index of Erectile Function (IIEF-5) and Male Sexual Health Questionnaire Short Form (MSHQ-SF), in order to assess a comprehensive urological, sexual and reproductive anamnesis. Data on COVID-19 status were recorded for patients’ partners.
Four biological fluid samples (saliva, pre-ejaculation urine, sperm obtained with masturbation, and first fraction post-ejaculation urine) were collected in four sterile jars to be tested for SARS-CoV-2. After liquefaction of semen and assessment of volume, semen samples were divided into two aliquots, one for evaluation of the presence of SARS-CoV-2 virus by RT-PCR and one for semen analysis.
Detection of SARS-CoV-2 in biological specimens
All samples were processed on the same day as collection or stored at −80°C until further analysis. Nucleic acids from samples were extracted with the Microlab Nimbus IVD system (Seegene Inc, Seoul, South Korea) using the Starmag Universal Cartridge and amplified with the multiplex RT-PCR Allplex™ 2019-nCoV assay (Seegene Inc), targeting RdrP, E and N genes, according to the manufacturers’ instructions.
Semen analysis and IL-8 evaluation
Semen analysis was carried out according to WHO guidelines (WHO, 2010). Quantification of leukocytes in semen was performed by counting the number of round cells per milliliter using an improved Neubauer hemocytometer and evaluating the percentage of leukocytes and immature germ cells after May-Grunwald staining of the sample.
For IL-8 evaluation, semen plasma aliquots were stored frozen and IL-8 levels were quantified by conventional two-step ELISA using a human IL-8 ELISA kit (BD Bioscience, San Diego, CA, USA), according to the manufacturer’s instructions.
Statistics
Patients were divided into different groups for comparisons according to hospitalization, intensity of treatment, and semen parameters. Differences were tested with Independent Sample Student’s t-test, Mann–Whitney u-test, and univariate analysis of variance (ANOVA) for continuous variables, and with χ2 and Fisher’s Exact Test for categorical variables according to sample size. A logistic regression was carried out including significant factors to better define the risk of sexual transmission and to identify the main determinants of impairment of semen quality. A value of P < 0.05 was considered to be significant. All statistical analyses were performed using IBM SPSS version 20.0 (SPSS Inc, Chicago, IL, USA).
Results
Patient characteristics and clinical features
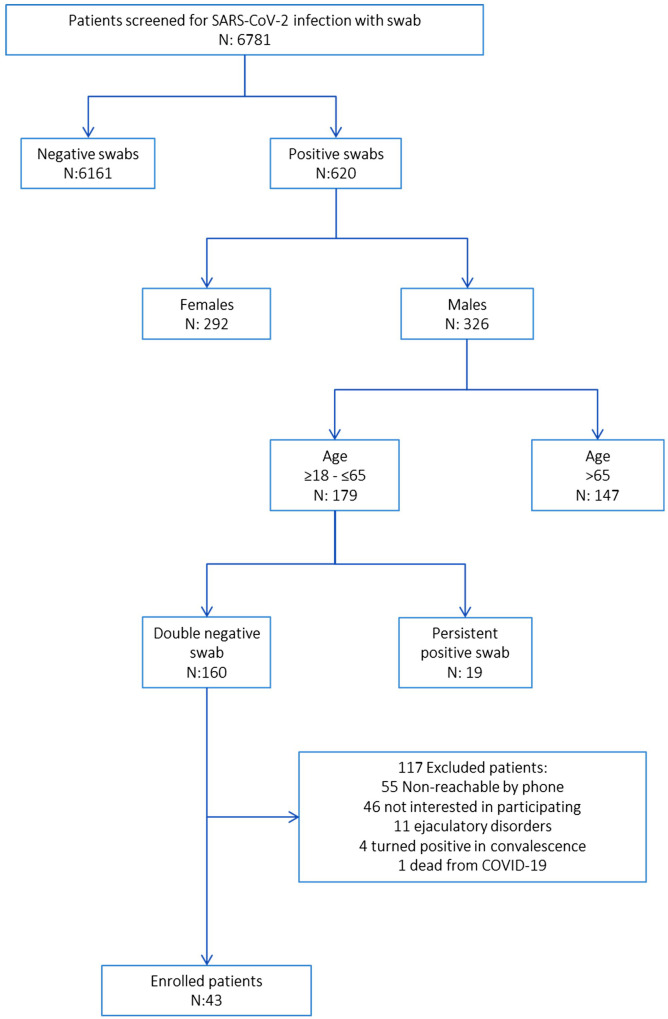
From 326 male patients with a positive NP-swab, 179 were between 18 and 65 years of age and were eligible for inclusion, among these, 43 agreed to participate in the study (Fig. 1). All enrolled patients previously affected by COVID-19 had a negative result from at least two consecutive NP swabs before sample collection. Clinical features, including urological and andrological medical history, are summarized in Table I.
Figure 1.
Flowchart of screening, eligibility, and the inclusion process for the study sample of men who recovered from COVID-19. Age is in years. CODIV-19: coronavirus disease 2019, SARS-CoV-2: severe acute respiratory syndrome coronavirus.
Table I.
Comparison of clinical, social, and uro-andrological characteristics of the study sample (N = 43) stratified by clinical management of COVID-19.
| Nonhospitalized (N = 12; 27.9%) | Hospitalized (without ICU) (N = 26; 60.5%) | ICU (N = 5; 11.6%) | P valuea | ||
|---|---|---|---|---|---|
| DEMOGRAPHICS | |||||
| Age (years) (median, IQR) | 44 (33–49) | 52 (48–58) | 59 (56–59) | 0.003 | |
| BMI (kg/m2) (median, IQR) | 26.1 (23.7–27.9) | 26.9 (23.6–31.0) | 27.4 (26.3–28.7) | 0.380 | |
| Smoking status | Never (n, %) | 9 (75.0%) | 22 (84.6%) | 4 (80.0%) | 0.850 |
| Current (n, %) | 2 (16.7%) | 1 (3.8%) | 0 (0.0%) | 0.157 | |
| Former (n, %) | 1 (8.3%) | 3 (11.5%) | 1 (20.0%) | 0.401 | |
| Period between last negative oropharyngeal swab and sample collection (days) (median, IQR) | 30 (23–39) | 37 (26–49) | 24 (23–32) | 0.558 | |
| ANDROLOGICAL FEATURES | |||||
| Previous orchitis/genital infection (n, %) | 2 (16.7%) | 3 (11.5%) | 0 (0.0%) | 0.814 | |
| Previous parotitis (n, %) | 4 (33.3%) | 3 (11.5%) | 1 (20.0%) | 0.209 | |
| Previous surgically treated varicocele (n, %) | 2 (16.7%) | 2 (7.7%) | 0 (0.0%) | 0.747 | |
| IIEF-5b (median, IQR) | 25 (24–25) | 24 (21–25) | 22 (22–23) | 0.389 | |
| MSHQc erection scale (1–4) (median, IQR) | 19 (17–20) | 19 (17–20) | 19 (17–20) | 0.487 | |
| MSHQc ejaculation scale (5–12) (median, IQR) | 37 (33–38) | 36 (35–38) | 34 (32–39) | 0.165 | |
| MSHQc satisfaction scale (13–18) (median, IQR) | 25 (23–25) | 26 (24–30) | 28 (26–29) | 0.433 | |
| MSHQc sexual activity (19) (median, IQR) | 3 (2–4) | 3 (2–4) | 4 (3–5) | 0.554 | |
| MSHQc sexual activity (20, 21) (median, IQR) | 8 (6–8) | 8 (7–8) | 8 (8–8) | 0.179 | |
| MSHQc sexual desire (22–25) (median, IQR) | 16 (14–16) | 16 (16–17) | 17 (15–18) | 0.353 | |
Calculated using Chi Quadro or Fischer test for categorical variables or ANOVA test for continuous variables.
International Index of Erectile Function Questionnaire.
Male Sexual Health Questionnaire.
COVID-19: coronavirus disease 2019; IQR: interquartile range, ICU: intensive care unit.
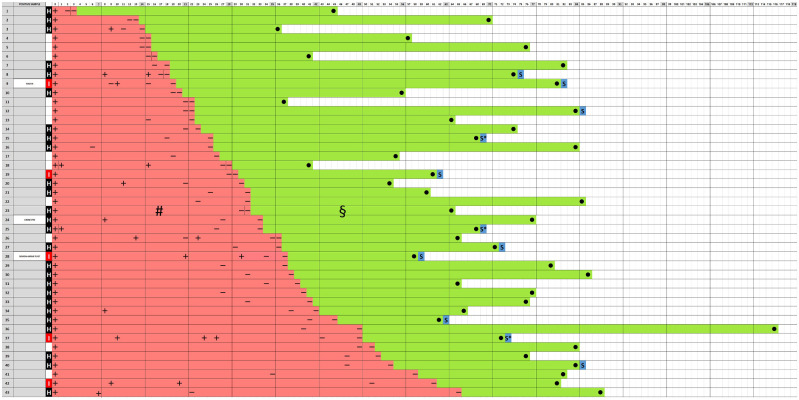
Timelines from the first positive NP swab to sample collection are reported in Fig. 2. In particular, median proven healing time (time from first positive to second consecutive negative NP-swab) was 31 days (range: 3–65), whereas median SARS-CoV-2-free time (time between second negative NP-swab and sample collection) was 35 days (r: 24–43).
Figure 2.
Timeline in days of the period between the first positive nasopharyngeal swab for COVID-19 and sample collection. Urine pre: urine collected before semen collection; urine post: urine collected after semen collection. Timeline (days) from first positive nasopharyngeal swab for COVID-19 and the sample collection for each patient. In the first column, the origin of the samples is reported. White box: not hospitalized patient; ‘H’: patient hospitalized in medicine units; ‘I’: patient hospitalized in intensive care unit. Red squares indicate the period between the first positive nasopharyngeal swab for COVID-19 and the second negative nasopharyngeal swab, while the green ones represent the period between the second negative nasopharyngeal swab and the date of sample collection. The symbols ‘+’ and ‘−’ indicate a positive or a negative nasopharyngeal swab result for SARS-CoV-2 RNA. ‘S’: azoospermic; ‘S*’: oligospermic; ●: sample collection time; #: median proven healing time: 31 days (range 3–65); §: median SARS-CoV-2-free time: 35 days (range: 24–43).
Twelve patients (27.9%) were not hospitalized, 26 (60.5%) were hospitalized in internal medicine unit, and 5 (11.6%) were admitted to intensive care unit (Table II). Overall 19 patients (44.2%) did not require oxygen therapy, 10 (23.2%) were treated with low flow O2 therapy, whereas 14 (32.6%) necessitated high flow/invasive O2 therapy.
Table II.
Comparison of relationship and parental status of the study sample (N = 43) stratified by clinical management of COVID-19.
| Nonhospitalized (N = 12; 27.9%) | Hospitalized (without ICU) (N = 26; 60.5%) | ICU (N = 5; 11.6%) | P valuea | ||||
|---|---|---|---|---|---|---|---|
| RELATIONSHIPS AND PARENTHOOD | |||||||
| Long-term female partner (n, %) | 11 (91.7%) | 22 (84.6%) | 4 (80.0%) | 0.838 | |||
| Long-term partner | Past COVID-19 infection at time of partner diagnosis (n, %) | 5 (45.5%) | 8 (34.8%) | 1 (20.0%) | 0.714 | ||
| Positive for COVID-19 at enrollment (n, %) | 2 (18.2%) | 2 (9.0%) | 0 | 0.710 | |||
| Patients without children | 5 (41.6%) | 5 (19.2%) | 1 (20.0%) | 0.152 | |||
| Number of children (median, IQR) | 2 (0–2) | 2 (1–2) | 1 (1–1) | 0.472 | |||
| Number of sexual relationships during the last 3 months | None (n, %) | 2 (16.7%) | 6 (23.1%) | 1 (20.0%) | 0.979 | ||
| 1–4 per month (n, %) | 9 (75.0%) | 16 (61.5%) | 3 (60.0%) | 0.648 | |||
| 4–8 per month (n, %) | 1 (8.3%) | 3 (11.5%) | 1 (20.0%) | 0.635 | |||
| >8 per month (n, %) | 0 (0.0%) | 1 (3.9%) | 0 (0.0%) | 0.958 | |||
| Problems having a baby (n, %) | 3 (25.0%) | 4 (16.0%) | 1 (20.0%) | 0.851 | |||
| Abortion by the long-term partner (n, %) | 3 (25.0%) | 6 (23.1%) | 0 (0.0%) | 0.447 | |||
Calculated using Chi Quadro or Fischer test for categorical variables or ANOVA test for continuous variables.
The sexual habits of enrolled men are reported in Table II. Six patients (13.9%) were without a fixed partner, while 37 (86.1%) had a stable relationship. Fourteen out of 37 stable female partners (37.8%) presented a positive NP swab for SARS-CoV-2 at the time of partner diagnosis (Table II) and four were positive at the time of enrollment of men, with two subsequent negative results for the two NP swabs performed according to National guidelines (WHO, 2020). Five of the 11 stable partners of nonhospitalized (45.5%), 8 of the 22 of the hospitalized men (34.8%) and one of the four stable partners of men requiring intensive care support (20%) tested positive at the time of partner diagnosis.
Twenty-nine male patients with a stable partner (78.4%) did not use condom: 10 of these female partners (34.5%) had a positive NP swab. In this subpopulation of stable partners having sex without condom, multivariate analysis did not show a difference in the number of sexual intercourse events per month between female partners with positive versus negative NP swab (median: 5 vs. 4, P = 0.470; data not shown).
SARS-CoV-2 detection in collected specimens
A total of 170 samples collected from 43 enrolled patients were tested by RT-PCR, namely saliva, urine sample collected before ejaculation, and semen and urine sample collected after ejaculation. Two samples from two different patients yielded inconclusive results. Forty patients (93%) were negative for SARS-CoV-2 RNA in any tested sample. Three patients (7%) tested positive in at least one sample: one (patient A) in saliva (collected 62 days after the second negative swab), which was positive for all target genes; one (patient B) in pre-ejaculation urines (44 days after the second negative swab), which were positive only for the N-gene (Threshold Cycle (Ct)= 37.04); one (patient C) in semen, where all target genes were detected, and in post-ejaculation urines where only the E- and N-genes were detected (Ct = 34.99 and 37.16, respectively) (21 days after the second negative swab). Patients A and C needed intensive care support during COVID-19 infection. These three patients and their partners were retested for SARS-CoV-2 RNA with NP-swabs and all samples tested negative.
Patient A was rehospitalized for sepsis resulting from bacterial infection and was treated with antibiotics, with subsequent healing. Patient B was asymptomatic, with no signs or symptoms of recurrence of COVID-19 and decided independently to undergo self-quarantine. Patient C reported having unprotected oral, vaginal, and anal sex with his stable partner after recovering from COVID-19. Therefore, they were further investigated using a urethral swab (patient) and pharyngeal, vaginal, and rectal swabs (partner): all samples tested negative.
Semen parameters
Data for parental and fertility status of the included patients are reported in Table II. Five of the 12 (41.6%) nonhospitalized, 5 of the 26 (19.2%) of the hospitalized and one of the five men (20%) requiring intensive care support had no children, with no significant difference between groups (P = 0.152).
Semen analysis demonstrated that eight patients (18.6%) were azoospermic and three were oligospermic with less than 2 million/mL (7.0%) spermatozoa: overall, 25.6% of patients were oligo-crypto-azoospermic. The occurrence of azoospermia was highly related to the severity of the illness: the condition was found in four out of five patients admitted to the intensive care unit, in three of the 26 hospitalized in the medicine department and only in one among the 12 nonhospitalized (P < 0.001). No relation was found between occurrence of azoospermia and severity of oxygen therapy (P = 0.417). Semen parameters are reported in Table III.
Table III.
Comparison of semen analysis of the study sample (N = 43) stratified by clinical management of COVID-19.
| Nonhospitalized (N = 12; 27.9%) | Hospitalized (without ICU) (N = 26; 60.5%) | ICU (N = 5; 11.6%) | P valuea | ||||
|---|---|---|---|---|---|---|---|
| SEMEN ANALYSIS | |||||||
| Collected semen volume (mL) (median, IQR) | 2.5 (1.5–3.5) | 2.0 (0.8–2.5) | 1.5 (1–2) | 0.778 | |||
| Total sperm number (millions) (median, IQR) | 133.25 (50.5–244.1) | 38.1 (5.5–123.8) | 0.0 (0.0–7.0) | 0.021 | |||
| Sperm concentration (millions/mL) (median, IQR) | 65.8 (23.8–71.0) | 17.8 (5.5–70.0) | 0.0 (0.0–3.5) | 0.215 | |||
| Progressive motility (%) (median, IQR) | 36.0 (26.0–58.0) | 25.0 (12.0–42.0) | 27.0 (27.0–27.0) | 0.154 | |||
| Time from collection to analysisb (minutes) (median, IQR) | 210 (168–270) | 240 (180–300) | 340 (120–270) | 0.558 | |||
| Vitality (live sperm, %) (median, IQR) | 59 (47–81) | 49 (31–67) | 0 (0–9) | 0.003 | |||
| Sperm morphology (%) (median, IQR) | 2 (2–5) | 3 (1–4) | 0 (0–0) | 0.332 | |||
| pH (median, IQR) | 7.6 (7.4–7.6) | 7.3 (7.2–7.6) | 7.6 (7.6–7.6) | 0.598 | |||
| Leucocytes (106/mL) (median, IQR) | 0.0 (0.0–0.24) | 0.0 (0.0–0.1) | 0.3 (0.1–1.7) | 0.324 | |||
| Interleukin-8 (ng/mL) (median, IQR) | 6 (3–10) | 7 (5–11) | 37 (13–78) | <0.001 | |||
Calculated using Chi Quadro or Fischer test for categorical variables or ANOVA test for continuous variables.
Time needed to carry the samples to laboratory.
The presence of leukocytes in semen was found in 16 patients (37.2%) and their occurrence was higher in men admitted to the intensive care unit as compared to non-hospitalized patients or those admitted to the medicine department, but was not related to the intensity of oxygen therapy (36.8% in men without O2 vs. 30.0% with low flow O2 and 42.9% with high flow/invasive O2).
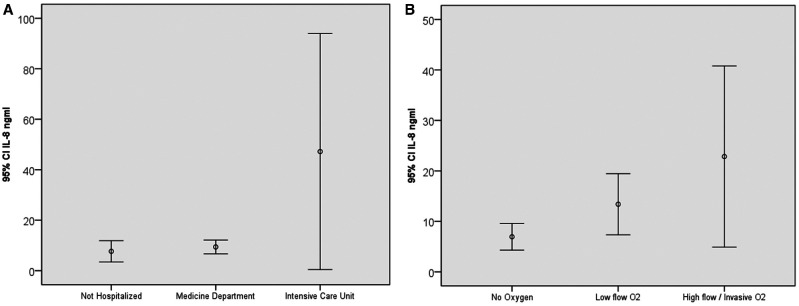
Thirty-three patients (76.7%) showed pathological levels of semen IL-8 (sIL-8) (i.e., >3.8 ng/mL) (Hofny et al., 2011): among them, 7 out of 12, (58.3%) were not hospitalized during the illness, 21 of 26 (80.8%) were hospitalized in the medicine department, and 5 (100.0%) were admitted to the intensive care unit (P = 0.142) (Fig. 3A). Pathological levels of sIL-8 were related to the severity of oxygen therapy (r = 0.356; P = 0.050). As shown in Fig. 3B, high levels of sIL-8 were found in 12 out of 19 (63.2%) men without oxygen therapy, 9 out of 10 (90.0%) with low flow O2-therapy and 12 out of 14 (85.7%) necessitating high flow/invasive O2 therapy.
Figure 3.
The 95% CIs for mean interleukin-8 concentration in semen of the enrolled patients (N = 43). Data were stratified by clinical management (not hospitalized N = 12, medicine department N = 26, intensive care unit N = 5) (A) and need of oxygen support (no oxygen N = 19, low flow O2 N = 10, high flow O2 N = 14) (B) for COVID-19. The time of collection is shown in Fig. 2. IL-8: interleukin-8. aCalculated using ANOVA test. Low flow O2 Therapy includes nasal cannula, simple face mask, and partial rebreather mask. High flow oxygen/invasive O2 includes trans tracheal catheters, venturi mask, aerosol mask, tracheostomy collars, non-rebreathing mask with reservoir and one way valve and high humidity face tents.
In univariate analysis, age, hospitalization and sIL-8 were all significant items for azoospermia (Supplementary Table SI). In multivariate analysis, hospitalization (not recovered vs. hospitalized vs. intensive care unit) was the main determinant of crypto-azoospermia (P = 0.039) (data not shown).
Discussion
In our sample, the age range was from 30 to 64 years. This study demonstrates that young and sexually active men with proven recovery from COVID-19 have a significant risk of developing oligo-crypto-azoospermia.
Prolonged viral shedding from the nasopharynx in convalescent patients, up to at least 3 weeks after recovery from symptoms, has been previously reported (Young et al., 2020). According to the European Centre for Disease Prevention and Control (ECDC) we considered as healed from SARS-CoV-2 infection those men with two upper respiratory tract samples that were negative for SARS-CoV-2 RNA, and showing clinical resolution of symptoms (https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-Discharge-criteria.pdf). However, in our population, one patient died from COVID-19 after clinical relapse and four tested positive again for SARS-CoV-2 infection by NP swab during the screening phase (from March 2020 to May 2020). Moreover, three men presented with persistence of SARS-COV-2 RNA in biological fluids 3–9 weeks after double negative NP swabs.
The occurrence of the virus in saliva, urine, and semen of asymptomatic patients several weeks after double negative NP swabs was demonstrated in a very small percentage of men in our cohort; nevertheless previous studies (Guo et al., 2020; Ma et al., 2020; Pan et al., 2020) did not report occurrence of virus in semen of healed patients or in their recovery phase. Interestingly, none of the partners of these three newly positive patients tested positive for SARS-CoV-2 including the patient with a positive test result for semen. Overall, these studies suggest that the occurrence of virus in semen is a rare event. Further studies will be required to determine the risk of SARS-CoV-2 transmission by sexual intercourse.
The occurrence in the male reproductive system, in particular testis, has been described for several viral strains. The HIV and mumps virus might lead to male infertility as a result of direct damage to the testicular structure (Masarani et al., 2006; Garolla et al., 2013). Abnormal sperm parameters have been observed in other viral infections such as herpes simplex virus, hepatitis virus B, or hepatitis virus C (Garolla et al., 2013). Recent findings seem to support an influence of SARS-CoV-2 infection on male sex hormones, with an increase in plasma levels of LH and a marked decrease in testosterone and FSH (Ma et al., 2020).
In our study, we found that one out of four (11/43, 25.5%) of COVID-19 healed patients were oligo-crypto-azoospermic, a percentage clearly exceeding that reported for the general population (about 1% for azoospermia, Jarow et al., 1989; 3% for oligozoospermia, Ombelet et al., 2009). Interestingly, all azoospermic patients reported a previous unimpaired fertility status (five had one child, two had two children, and one had three children), and only one out of three oligo-crypto-azoospermic men reported no parenthood (while the other two each had two children). Occurrence of azoospermia could be related to antibiotics or other drugs used for the treatment of patients during COVID-19. Indeed, antibiotics, antiviral drugs, chloroquine, corticosteroids, and immunomodulators might affect male fertility status (Semet et al., 2017). However, a contribution to impairment of testicular function from SARS-COV-2 infection cannot be excluded, considering that, on average, the time from recovery was around 30 days, which is below the length of a complete cycle of human spermatogenesis. The virus may localize in the testis owing to the elevated expression of ACE and TMPRSS2 in the organ, and COVID-19 patients with active infection show low testosterone levels (Rastrelli et al., 2020; Wang et al., 2020). Moreover, although antibiotics have long been suspected of contributing to male infertility (Semet et al., 2017), limited data support this hypothesis (Samplaski and Nangia, 2015). Semen quality could also be affected by febrile illness, even if limited data are currently available. In particular, semen concentration was significantly influenced by fever occurring during the meiosis and postmeiotic period, with a mean decrease of 32.6% and 35%, respectively (Carlsen et al., 2003). Moreover, a large variation in sperm concentration was observed, and semen recovery was obtained almost 60 days after temperature normalization (MacLeod, 1951). In our cohort of patients, one crypto-azoospermic semen was analyzed 4 weeks after temperature normalization and one oligospermic after 6 weeks, while the other nine oligo-crypto-azoospermic patients were tested at least 8 weeks after COVID-19 clinical healing. Moreover, 8 out of 11 men with semen impairment were crypto-azoospermics and three were oligospermics. Thus, the impact of fever on semen quality seems negligible.
Furthermore, the virus can have direct (viral replication and dissemination in the testis) and indirect (fever and immunopathology) effects on testicular function (Carlsen et al., 2003). Leukocytospermia is associated with male accessory gland infection (MAGI). However, the pathophysiology of leukocytes in semen is unclear and the diagnostic significance is still debated (Grande et al., 2018). New seminal biomarkers, including some cytokines, have been reported as the most promising putative markers of infection (Grande et al., 2018). IL-8 is a chemokine involved in several inflammatory diseases, comprising inflammation of the prostate, seminal vesicles, and epididymis (Penna et al., 2007; Lotti and et al., 2012; Lotti and Maggi, 2013). Therefore, IL-8 has been proposed as a specific marker for silent MAGI (Lotti et al., 2011). The high levels of sIL-8 found in a high percentage of our patients support the persistence of an inflammatory condition within the male genitourinary tract (Penna et al., 2007) after healing. In addition, reanimation treatments (e.g., invasive ventilation, administration of sedative drugs, specific organ support therapy) and body distress can affect testicular function (Vishvkarma and Rajender, 2020). Clearly, in order to understand whether these men can recover from poor testicular function, they should be reassessed at least 3 months after complete healing from COVID-19.
Our study has some limitations. First, the number of enrolled patients (43) may limit the statistical power of our study regarding the cause-effect relationship between COVID-19 infection, semen quality, and sexual transmission. However, ours is the largest among studies published to date reporting on semen quality and occurrence of virus genome in the semen of sexually active men who were previously infected and who recovered from COVID-19 (12 patients in Ma et al., 2020; 23 in Guo et al., 2020). Another limitation of our study is that semen quality before infection of the men that demonstrated severe oligo-crypto-azoospermia after COVID-19 was not known. However, all patients who were crypto-azoospermic had previously had children.
The strength of our study is that that the SARS-CoV-2 genome has been analyzed in four different biological samples, from different anatomical sites, collected simultaneously. Finally, the study was performed over a short time frame, and in a single center: this allows us to minimize biases related to virus modifications or analytic procedures.
Conclusion
The SARS-CoV-2 genome can be detected in biological fluids such as saliva, urine, and semen in a small percentage of sexually active men who have recovered from COVID-19. Even if our evidence suggests that the risk of SARS-CoV-2 sexual transmission after recovery in stable partners seems negligible, caution should be taken when managing the semen of healed COVID-19 patients during assisted reproduction and cryopreservation.
Most importantly, one-quarter of men who recovered from COVID-19 demonstrated oligo-crypto-azoospermia and signs of male genital tract inflammation, strictly related to disease severity. Therefore, our study suggests that COVID-19 patients of reproductive age should undergo a careful follow up for reproductive function and semen parameters.
Supplementary data
Supplementary data are available at Human Reproduction online.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Authors’ roles
Conception and Design: M.G., S.S., E.B., F.A., M.M., L.V., A.B. and G.M.R. Acquisition of data: A.M., A.P., R.N., C.B., A.L. and L.G. Analysis and interpretation of data: A.S., M.G., E.B., S.M., S.M., S.D. and S.D. Drafting the manuscript: M.G. and A.S. Critical revision of the manuscript: all the Authors. Statistical analysis: S.M., M.G., E.B. and S.P. Administrative, technical or material support: A.A., S.P., F.L. and M.C. Supervision: S.G. Ethical approval: S.M. and C.Z.
Funding
None.
Conflict of interest
None.
Supplementary Material
References
- Carlsen E, Andersson AM, Petersen JH, Skakkebaek NE.. History of febrile illness and variation in semen quality. Hum Reprod 2003;18:2089–2092. [DOI] [PubMed] [Google Scholar]
- COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU); https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (1 October 2020, date last accessed).
- Feldmann H. Virus in semen and the risk of sexual transmission. N Engl J Med 2018;378:1440–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garolla A, Pizzol D, Bertoldo A, Menegazzo M, Barzon L, Foresta C.. Sperm viral infection and male infertility: focus on HBV, HCV, HIV, HPV, HSV, HCMV, and AAV. J Reprod Immunol 2013;100:20–29. [DOI] [PubMed] [Google Scholar]
- Grande G, Milardi D, Baroni S, Luca G, Pontecorvi A.. Identification of seminal markers of male accessory gland inflammation: from molecules to proteome. Am J Reprod Immunol 2018;80:e12992. [DOI] [PubMed] [Google Scholar]
- Guo L, Zhao S, Li W, Wang Y, Li L, Jiang S, Ren W, Yuan Q, Zhang F, Kong F. et al. Absence of SARS-CoV-2 in semen of a COVID-19 patient cohort. Andrology 2020;29:10.1111/andr.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofny ERM, Ali MEM, Taha EA, Nafeh HM, Samir Sayed D, Abdel-Azeem HG, Abdou EF, Kamal GM, Mostafa T.. Semen and hormonal parameters in men with chronic hepatitis C infection. Fertil Steril 2011;95:2557–2559. [DOI] [PubMed] [Google Scholar]
- Jarow JP, Espeland MA, Lipshultz LI.. Evaluation of the azoospermic patient. J Urol 1989;142:62–65. [DOI] [PubMed] [Google Scholar]
- Li D, Jin M, Bao P, Zhao W, Zhang S.. Clinical characteristics and results of semen tests among men with coronavirus disease 2019. JAMA Netw Open 2020;3:e208292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotti F, Corona G, Mancini M, Filimberti E, Degli Innocenti S, Colpi GM, Baldi E, Noci I, Forti G, Adorini L. et al. Ultrasonographic and clinical correlates of seminal plasma interleukin-8 levels in patients attending an andrology clinic for infertility. Int J Androl 2011;34:600–613. [DOI] [PubMed] [Google Scholar]
- Lotti F, Maggi M.. Interleukin 8 and the male genital tract. J Reprod Immunol 2013;100:54–65. [DOI] [PubMed] [Google Scholar]
- Lotti F, Tamburrino L, Marchiani S, Muratori M, Corona G, Fino MG, Degl'Innocenti S, Forti G, Maggi M, Baldi E. et al. Semen apoptotic M540 body levels correlate with testis abnormalities: a study in a cohort of infertile subjects. Hum Reprod 2012;27:3393–3402. [DOI] [PubMed] [Google Scholar]
- MacLeod J. Effect of chickenpox and of pneumonia on semen quality. Fertil Steril 1951;2:523–533. [DOI] [PubMed] [Google Scholar]
- Ma L, Xie W, Li D. et al. Effect of SARS-CoV-2 infection upon male gonadal function: a single center-based study. 2020. medRxiv 2020.03.21.20037267. [Google Scholar]
- Masarani M, Wazait H, Dinneen M.. Mumps orchitis. J R Soc Med 2006;99:573–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ombelet W, Bosmans E, Cox A, Janssen M, Mestdagh G, Nijs M.. In search for the general population’s semen profile: the study of sperm parameters in partners of women with chronic anovulation. Facts Views Vis Obgyn 2009;1:18–26. [PMC free article] [PubMed] [Google Scholar]
- Pan X, Chen D, Xia Y, Wu X, Li T, Ou X, Zhou L, Liu J.. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis 2020;20:410–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paoli D, Pallotti F, Colangelo S. et al. Study of SARS-CoV-2 in semen and urine samples of a volunteer with positive naso-pharyngeal swab. J Endocrinol Invest 2020;43:1819–1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng L, Liu J, Xu W, Luo Q, Deng K, Lin B. et al. Novel coronavirus can be detected in urine, blood, anal swabs and NP-swabs samples. medRxiv. 2020:2020.02.21. 2020. 10.1101/2020.02.21.20026179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penna G, Mondaini N, Amuchastegui S, Degli Innocenti S, Carini M, Giubilei G, Fibbi B, Colli E, Maggi M, Adorini L. et al. Seminal plasma cytokines and chemokines in prostate inflammation: interleukin 8 as a predictive biomarker in chronic prostatitis/chronic pelvic pain syndrome and benign prostatic hyperplasia. Eur Urol 2007;51:524–533. [DOI] [PubMed] [Google Scholar]
- Rastrelli G, Di Stasi V, Inglese F. et al. Low testosterone levels predict clinical adverse outcomes in SARS-CoV-2 pneumonia patients [published online ahead of print, 2020 May 20]. Andrology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, Guggemos W. et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020;382:970–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samplaski MK, Nangia AK.. Adverse effects of common medications on male fertility. Nat Rev Urol 2015;12:401–413. [DOI] [PubMed] [Google Scholar]
- Semet M, Paci M, Saïas-Magnan J, Metzler-Guillemain C, Boissier R, Lejeune H, Perrin J.. The impact of drugs on male fertility: a review. Andrology 2017;5:640–663. [DOI] [PubMed] [Google Scholar]
- Smith LB, Walker WH.. The regulation of spermatogenesis by androgens. Semin Cell Dev Biol 2014;30:2–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song C, Wang Y, Li W, Hu B, Chen G, Xia P, Wang W, Li C, Diao F, Hu Z. et al. Absence of 2019 novel coronavirus in semen and testes of COVID-19 patients. Biol Reprod 2020;103:4–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swerdlow DL, Finelli L.. Preparation for possible sustained transmission of 2019 novel coronavirus: lessons from previous epidemics. JAMA 2020;323:1129–1130. [DOI] [PubMed] [Google Scholar]
- To KK, Tsang OT, Chik-Yan Yip C. et al. Consistent detection of 2019 novel coronavirus in saliva [published online ahead of print, 2020 Feb 12]. Clin Infect Dis 2020;ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vishvkarma R, Rajender S.. Could SARS-CoV-2 affect male fertility? Andrologia 2020;52:e13712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Xu Y, Gao R. et al. Detection of SARS-CoV-2 in different types of clinical specimens [published online ahead of print, 2020 Mar 11]. JAMA 2020;323:1843–1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Xu X.. scRNA‐seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS CoV‐2 infection in spermatogonia, Leydig and Sertoli cells. Cells 2020;9:920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. Cambridge, UK: Cambridge University Press, 2010. [Google Scholar]
- World Health Organization (WHO). Clinical management of COVID-19 (Interim Guidance) https://www.who.int/publicationsdetail/clinical-management-of-covid-19 (27 May 2020).
- Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, Ng O-T, Marimuthu K, Ang LW, Mak TM, for the Singapore 2019 Novel Coronavirus Outbreak Research Team et al. Epidemiologic features and clinical course of patients infected with SARS CoV-2 in Singapore. JAMA 2020;323:1488–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.