Abstract
Background
The World Health Organization declared coronavirus disease 2019 (COVID-19) a global pandemic on 11 March 2020. We report a patient with acute myocardial infarction (AMI) who presented late due to fears of contracting COVID-19.
Case summary
A 65-year-old man with a history of hypertension presented late to the emergency department (ED) with AMI. He gave a 2-month history of exertional angina but avoided seeking medical consult due to fears of contracting COVID-19. On the day of admission, he had 4 h of severe chest pain before presenting to the ED. He was hypotensive and tachycardic on arrival. Electrocardiogram showed inferolateral ST-elevation myocardial infarction. Chest radiograph revealed widened superior mediastinum and bedside echocardiogram revealed inferoseptal and inferolateral hypokinesia with features of cardiac tamponade. An urgent computed tomography aortogram showed possible left ventricular (LV) wall perforation with resulting haemopericardium and cardiac tamponade. Subsequent coronary angiogram showed 100% occlusion of mid left circumflex artery and a contained LV wall rupture was confirmed with LV ventriculogram. He was transferred to a tertiary centre and underwent successful emergency surgical repair.
Discussion
Our index case demonstrates the impact of the COVID-19 pandemic on health seeking behaviour due to fears of contracting COVID-19 and the ensuing impact of delayed medical intervention. Cardiologists worldwide are seeing an alarming rate of rare complications of AMI in patients who present late. Physicians need to be aware of this phenomenon and have an active role to play in public education.
Keywords: Acute coronary syndrome, Case report, COVID-19, Mechanical complication
Learning points
Physicians should:
Have an awareness of the impact of coronavirus disease 2019 on patients’ health seeking behaviour.
Adopt a low threshold of clinical suspicion for rare mechanical complications of acute myocardial infarction as a result of delayed presentation.
Introduction
Viral pneumonia outbreaks caused by severe acute respiratory syndrome coronavirus 2 which originated from Wuhan, China in December 2019 has escalated to become a global pandemic. As of 18 October 2020, there have been more than 39 million confirmed cases of coronavirus disease 2019 (COVID-19) and more than 1 million deaths reported.1
The COVID-19 pandemic has impacted healthcare delivery worldwide. Many countries have reported a significant decline, of up to 40%, in acute myocardial infarction (AMI)-related hospitalizations during this pandemic with an alarming pattern of delayed myocardial infarction (MI) presentations and their associated cardiac complications.2,3 Another recent study4 has shown that patients were more likely to die from AMI when compared with pre-pandemic times.
It is postulated that hospital admissions3 for acute coronary syndrome (ACS) have reduced significantly during the pandemic due to the perception that the hospital is a high-risk place to contract COVID-19 infection.
Diagnosis and treatment of ACS, especially ST-elevation myocardial infarction (STEMI) start from the point of first medical contact. Ischaemic time duration is a major determinant of infarct size and survival in patients with STEMI. Hence, prompt activation of emergency medical services leading to early recognition and treatment is crucial to reduce the mortality and morbidity related to ACS.5 We report a patient with ACS who presented late during the COVID-19 pandemic due to medical care avoidance behaviour. He did not have any signs and symptoms of COVID-19 and was diagnosed to have left ventricular (LV) posterolateral wall contained rupture and underwent a successful emergency surgical repair.
Timeline
| Timeline | Event |
|---|---|
| 2 months before admission |
|
| 3 days before admission |
|
| On admission |
|
| 0.5 h after admission |
|
| 1 h after admission |
|
| 1–2 h after admission |
|
| 4 h after admission |
|
| Day 12 |
|
| Day 20 |
|
| 4 months after (follow-up) |
|
Case presentation
A 65-year-old man with a known history of hypertension presented to the emergency department (ED) with a 3-day history of chest pain with the worst onset of chest pain occurring just few hours before admission. On further questioning, patient had experienced exertional angina for 2 months prior to ED visit. He had deliberately avoided medical consultation due to fear of contracting COVID-19 from hospital visit.
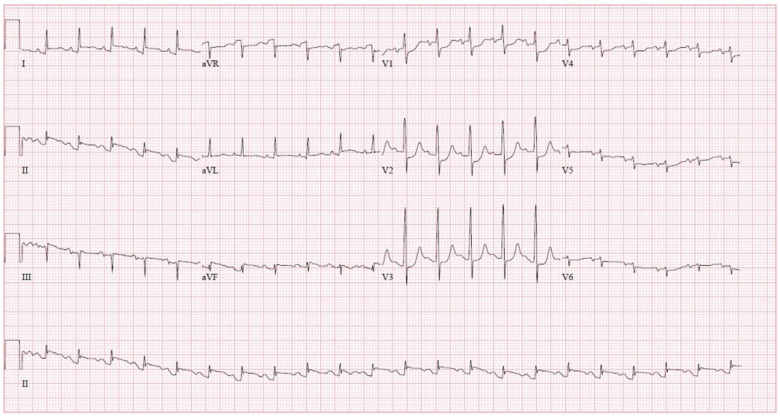
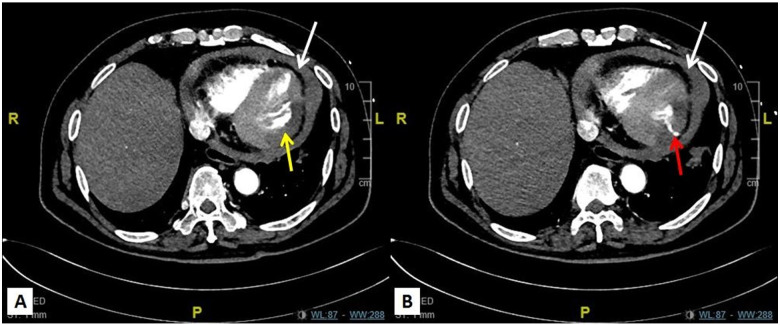
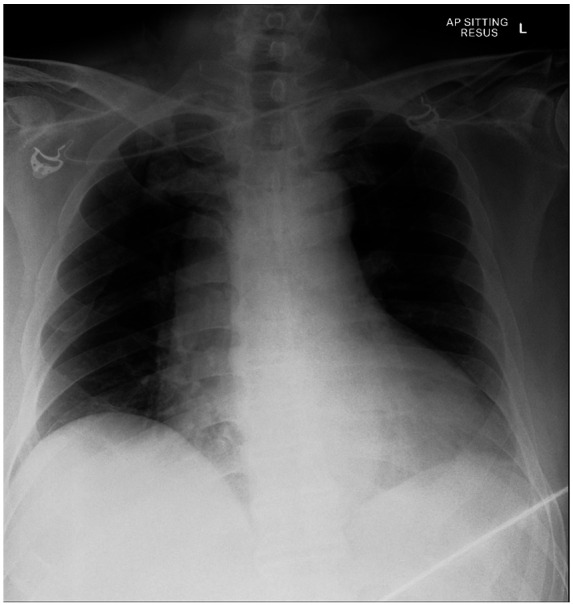
On arrival at the ED, his blood pressure was 93/72 mmHg with heart rate of 120 beats per minute. He had a low grade fever of 37.9°C. On examination, there were reduced air entry in bilateral lung bases. Heart sounds were dual with no audible murmurs. There were no radio-radial or radio-femoral delays. Electrocardiogram showed ST-elevation in the inferolateral leads (Figure 1) and high-sensitivity troponin level was elevated at 13 852 ng/L (normal value 18 ng/L). Chest X-ray showed widened superior mediastinum (Figure 2). Transthoracic echocardiogram revealed hypokinesia in the inferoseptal and inferolateral walls with moderately depressed LV ejection fraction of 40%. A moderate size global pericardial effusion was seen with right atrial collapse (Video 1) and plethoric inferior vena cava. He remained hypotensive in the ED despite intravenous fluid challenge and was started on intravenous noradrenaline. Urgent computed tomography aortogram was performed to rule out aortic dissection. This showed contrast leakage at posterolateral LV free wall suggesting possible perforation of the LV wall resulting in haemopericardium and cardiac tamponade (Figure 3A and B).
Figure 1.
Electrocardiogram showing inferolateral ST-elevation myocardial infarction.
Figure 2.
Chest radiograph showing widened superior mediastinum.
Figure 3.
Computed tomography aortogram showing hypoenhancement of the posteroinferior wall of the left ventricle suggesting possible myocardial infarction (A, yellow arrow). There was a transmural linear track of contrast seen extending from the lumen to the left ventricular wall raising concern for possible perforation of left ventricular wall (B, red arrow). Moderate haemopericardium seen with mild compression of right ventricle in keeping with cardiac tamponade (white arrow).
The working diagnosis was a delayed presentation of inferoposterior MI with LV wall rupture and cardiac tamponade. Coronary angiogram showed 100% occlusion of the mid left circumflex artery (Video 2). Left ventriculogram (LVgram) showed a small LV pseudoaneurysm (LVP) likely from a contained LV wall rupture (Video 3). An intra-aortic balloon pump was inserted for haemodynamic support. He was immediately transferred to a tertiary centre with cardiothoracic surgery services for emergency surgical repair and drainage of the cardiac tamponade. Operative findings revealed extensive posterolateral infarct of LV wall and a ruptured site covered in fibrin and clots with minimal oozing. This was repaired successfully with a bovine pericardial patch (Figure 4). His condition stabilised post-operatively and he was discharged from hospital on Day 20. He remained clinically well and asymptomatic at 4 months of follow-up.
Figure 4.
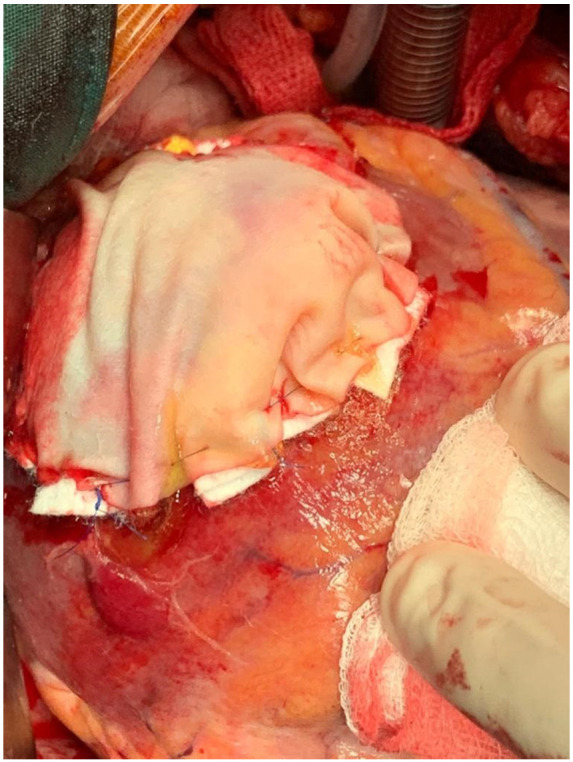
Intraoperative picture of posterolateral left ventricular wall ruptured site covered with bovine pericardial patch.
Discussion
We described a patient with STEMI who presented late with mechanical complication of MI. LVP6–8 forms when there is a contained rupture of the left ventricle by adherent pericardium, thrombus or scar tissue. LVP can be clinically silent in 12% of patients and the most common symptoms at presentation9 include dyspnoea, chest pain, and congestive heart failure.
The most common aetiology of LVPs is MI. It is however a rare complication of MI, with a reported incidence of 0.2–0.3%. Inferior MI accounts for twice as many cases of LVPs compared to anterior MI. This finding is consistent with the most common reported location of LVPs which are the posterior, lateral, apical or inferior surface of LV wall. LVPs are best diagnosed with LVgram during coronary angiography, which is crucial for planning of subsequent surgical intervention. Untreated LVPs are prone to rupture with the reported risk as high as 30–45%. The mortality rate for conservative management of LVPs is 50%. Therefore, early surgical intervention10 is highly recommended.
COVID-19 was declared a pandemic by the World Health Organization on 11 March 2020 and has imposed an enormous strain on healthcare systems worldwide.11 Decreased utilization of healthcare services for acute conditions by non-COVID-19 patients have also been reported and attributed to the public’s concerns about contracting the virus.
Our index case demonstrates the psychological impact of COVID-19 pandemic on health seeking behaviour in our local population. Access to healthcare requires both the availability of services as well as the patient’s ability to recognize their need for medical attention. Patient’s unconfirmed beliefs about the mode of transmission of disease, perceived severity and susceptibility of illness have contributed to medical avoidance behaviour.12 In this particular case, the patient’s preconceived fear of acquiring COVID-19 resulted in significant delay in seeking medical attention for his life-threatening condition.
This is consistent with a recent paper from Hong Kong13 which reported significant delay in time from symptom onset to first medical contact (median time of 318 min) during the COVID-19 pandemic compared to the time before pandemic (median time of 82.5 min during office hour and 91.5 min during non-office hours). Although some patients with ACS presented late as demonstrated by our index case, there is a greater concern for those do not seek medical help at all.
These patients will likely suffer unnecessary morbidity and mortality without proper ACS management. Cardiologists worldwide are seeing an alarming increase in rare complications14 of untreated ACS which include ventricular septal defects from transmural infarcts, papillary muscle rupture, LV aneurysm, and thrombus. A recent publication15 from Lombardy, Italy reported 58% increase in the number of out-of-hospital cardiac arrests in the first 40 days of the COVID-19 pandemic compared to 2019. It may not be possible to differentiate between the cardiac arrests caused by complications of COVID-19 and those that are a result of hospital avoidance but the authors estimate that COVID-19 accounts for 77.4% of the increase.
Hence, proper public education by healthcare providers worldwide through traditional media channels/social media is extremely crucial in ensuring individuals with symptoms suggestive of ACS seek prompt medical evaluation and timely medical intervention.
In conclusion, our index case demonstrates the impact of COVID-19 pandemic on health seeking behaviour of patients and the ensuing collateral damage. Physicians worldwide need to be aware of this phenomenon and be more vigilant. A high index of clinical suspicion is needed to look for mechanical complications of AMI especially for those who presented late and haemodynamically unstable.
Lead author biography

Dr Joo Hor Tan graduated from University of Edinburgh in 2013. He obtained her Masters of Medicine and MRCP (UK) in 2016. He completed his internal medicine residency training in 2019 and is currently a second year senior resident in Department of Cardiology, Tan Tock Seng Hospital.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Supplementary Material
Acknowledgements
The authors wish to thank Dr Kang Giap Swee (senior consultant) and Dr Qian Qi (senior resident) from Department of Cardiac, Thoracic & Vascular Surgery from National University Hospital, Singapore for the emergency surgical support and image acquisition.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Funding: None declared.
Conflict of interest: None declared.
References
- 1.World Health Organization. Coronavirus Disease (COVID-2019) Situation Reports 12/10/2020. who.int/docs/default-source/coronaviruse/situation-reports/20201012-weekly-epi-update-9.pdf (14 October 2020).
- 2.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A. et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med 2020;383:88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah KTang DIbrahim FGhosh BBhatti SAkhabue Eet al. . Surge in delayed myocardial infarction presentations. JACC Case Rep 2020;2:1642–1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gluckman TJ, Wilson MA, Chiu ST, Penny BW, Chepuri VB, Waggoner JW. et al. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol 2020;e203629.doi:10.1001/jamacardio.2020.3629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholz KH, Maier SKG, Maier LS, Lengenfelder B, Jacobshagen C, Jung J. et al. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: Results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J 2018;39:1065–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dachman AH, Spindola-Franco H, Solomon N.. Left ventricular pseudoaneurysm. Its recognition and significance. JAMA 1981;246:1951–1953. [PubMed] [Google Scholar]
- 7.Frances C, Romero A, Grady D.. Left ventricular pseudoaneurysm. J Am Coll Cardiol 1998;32:557–561. [DOI] [PubMed] [Google Scholar]
- 8.Csapo K, Voith L, Szuk T, Edes I, Kereiakes DJ.. Postinfarction left ventricular pseudoaneurysm. Clin Cardiol 1997;20:898–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeo TC, Malouf JF, Oh JK, Seward JB.. Clinical profile and outcome in 52 patients with cardiac pseudoaneurysm. Ann Intern Med 1998;128:299–305. [DOI] [PubMed] [Google Scholar]
- 10.Atik FA, Navia JL, Vega PR, Gonzalez-Stawinski GV, Alster JM, Gillinov AM. et al. Surgical treatment of postinfarction left ventricular pseudoaneurysm. Ann Thorac Surg 2007;83:526–531. [DOI] [PubMed] [Google Scholar]
- 11.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kannan VD, Veazie PJ.. Predictors of avoiding medical care and reasons for avoidance behavior. Med Care 2014;52:336–345. [DOI] [PubMed] [Google Scholar]
- 13.Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M. et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020;13:e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moroni F, Gramegna M, Ajello S. et al. Collateral damage: medical care avoidance behavior among patients with acute coronary syndrome during the COVID-19 pandemic. JACC Case Rep 2020;2:1625–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R. et al. Out-of-hospital cardiac arrest during the COVID-19 outbreak in Italy. N Engl J Med 2020;383:496–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.