Abstract
Disrupted sleep and nocturnal wakefulness are evidence-based risk factors for suicidal thoughts and behaviors. We present a suicide attempt following a rapid increase in nocturnal wakefulness. This case illustrates how nocturnal wakefulness may drive suicide risk through circadian misalignment.
Citation:
Tubbs AS, Harrison-Monroe P, Fernandez F-X, Perlis ML, Grandner MA. When reason sleeps: attempted suicide during the circadian night. J Clin Sleep Med. 2020;16(10):1809–1810.
Keywords: suicide, nocturnal wakefulness, suicidal attempt, sleep
INTRODUCTION
Disrupted sleep is an evidence-based risk factor for suicide,1 and treatment of insomnia may reduce suicide risk.2,3 Emerging evidence indicates nocturnal wakefulness also operates as a suicide risk factor, possibly through misalignment of circadian rhythms. After adjusting for population wakefulness, the incidence of completed suicide is highest at night4 regardless of month or method.5 Nighttime wakefulness predicts next-day suicidal ideation,6 and reducing nocturnal wakefulness may reduce suicidal thinking in at-risk populations.7 To highlight this issue, we present a suicide attempt following a rapid increase in nocturnal wakefulness. Informed consent was obtained for this report.
REPORT OF CASE
The patient is a 29-year-old Caucasian male with a history of prior suicide attempt, post-traumatic stress disorder, and a diagnosis of schizoaffective disorder within the past 10 years enrolled in a first-episode psychosis treatment program. Psychotherapeutic services included individual and group cognitive behavioral therapy for psychosis, along with a prescription for olanzapine, which had increased to 20 mg over the past month. Benztropine (1 mg) was added due to increased arm and leg movements that were interfering with sleep. In supplemental services, the patient was also participating in weekly cognitive behavioral therapy for insomnia (CBT-I) sessions with sleep/wake monitoring via actigraphy (Actiwatch Spectrum Plus; Philips Respironics, Murrysville, PA). The primary CBT-I approach employed was stimulus control as there was concern that sleep restriction could exacerbate his psychotic symptoms. At the time of the attempt, the patient was spending excess time in bed coping with distressing hallucinations; consequently, therapy involved constructing an alternative location for coping and reserving the bed for sleep alone. The patient was additionally waiting for evaluation by sleep medicine for obstructive sleep apnea and restless leg syndrome.
Eighteen days prior to the attempt (day −18), the patient’s grandfather died unexpectedly, and the patient relapsed on alcohol and cannabis in the direct aftermath. When the patient was seen in clinic on day −14, he reported no auditory or visual hallucinations, had not used alcohol or cannabis since his grandfather’s death, and was only struggling with difficulty sleeping. On objective measures, his Insomnia Severity Index score was 20, his Patient Health Questionnaire–9 score was 7, and his Generalized Anxiety Disorder–7 Questionnaire score was 6.
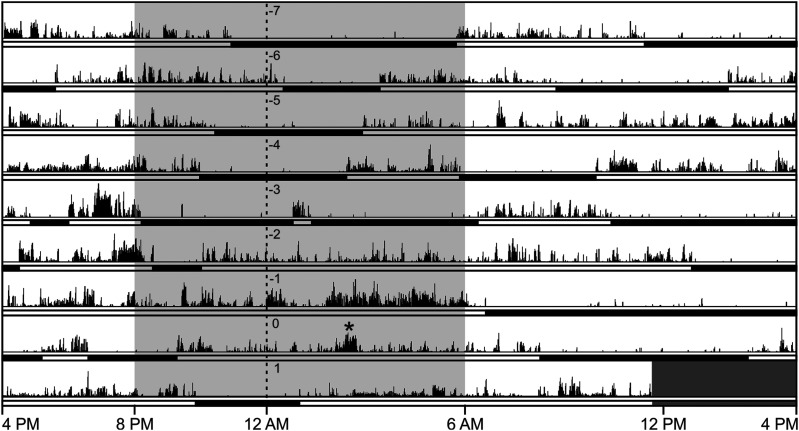
Over the next 2 weeks, the patient dramatically increased daytime sleeping (6:00 am–8:00 pm). Two days prior to the suicide attempt, he began sleeping exclusively during the day—which included 10.5 hours of sleep just prior to the attempt—and began experiencing intrusive visual hallucinations of himself hanging to death that felt compulsory in nature. He then attempted suicide by fashioning a noose out of blankets and hanging himself between 2:00 and 3:00 am (day 0; Figure 1). The attempt failed when the patient could not fit the noose over his head. He then abandoned the effort.
Figure 1. The timing of sleep and attempted suicide.
The actogram for the week preceding the suicide attempt (*). Sleep is indicated by black horizontal bars, and activity is indicated by vertical black lines.
The patient reported the attempt to his psychiatrist in the clinic the next day. He felt hopeless and disillusioned about his symptoms and prognosis and reported that the increased dosage of olanzapine (20 mg) was sedating him to the point that he could not function. Consequently, he was only taking it twice per week, rather than nightly as prescribed. He additionally reported he had not used alcohol or cannabis since his grandfather died. The attending psychiatrist concluded that the patient’s exacerbated psychotic and depressive symptoms required in-patient treatment, and the patient subsequently agreed to be hospitalized in an in-patient psychiatric unit.
DISCUSSION
Suicide is a complex phenomenon built on distal and proximal risk factors. In this case study, the patient’s history of severe mental illness and prior suicide attempt was compounded by personal loss, recent substance abuse, medication noncompliance, intrusive hallucinations, and severe sleep disturbance. However, the objective sleep data (measured via actigraphy) highlight how the link between suicide risk and sleep disturbance may be a matter of timing, not duration. First, the sudden shift in sleep organization resulted in wakefulness when the patient was most vulnerable to poor decision making and affect regulation.8 This shift represents a severe circadian misalignment, which likely contributed to the suicide attempt in agreement with preliminary findings that circadian dysregulation is associated with suicidal ideation.9 Moreover, while inconsistent use of olanzapine certainly increased the patient’s likelihood of breakthrough psychosis, hallucinations follow a daily pattern10 and the patient’s circadian dysregulation may have exacerbated or even precipitated these symptoms. Finally, the suicide attempt followed a 10.5-hour period of objectively measured sleep, which eliminates sleep deprivation as a potential contributing factor. Ultimately, this case illustrates how disrupted sleep timing may increase vulnerability to suicide and emphasizes the need for further research to explore the underlying neurobiological mechanisms linking sleep, nocturnal wakefulness, and suicide risk.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. Work for this study was performed at the University of Arizona. M.A.G. reports he has received grants from Jazz Pharmaceuticals, the National Institutes of Health, Nexalin Technology, and Kemin Foods. He has performed consulting activities for Fitbit, Natrol, Casper, Curaegis, Thrive, Pharmavite, SPV, NightFood, and Merck. The above-mentioned conflicts are unrelated to the topic of this paper. The other authors report no conflicts of interest.
REFERENCES
- 1.Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17(3):554. 10.1007/s11920-015-0554-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pigeon WR, Funderburk JS, Cross W, Bishop TM, Crean HF. Brief CBT for insomnia delivered in primary care to patients endorsing suicidal ideation: a proof-of-concept randomized clinical trial. Transl Behav Med. 2019;9(6):1169–1177. 10.1093/tbm/ibz108 [DOI] [PubMed] [Google Scholar]
- 3.McCall WV, Benca RM, Rosenquist PB, et al. Reducing Suicidal Ideation Through Insomnia Treatment (REST-IT): a randomized clinical trial. Am J Psychiatry. 2019;176(11):957–965. 10.1176/appi.ajp.2019.19030267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perlis ML, Grandner MA, Brown GK, et al. Nocturnal wakefulness as a previously unrecognized risk factor for suicide. J Clin Psychiatry. 2016;77(6):e726–e733. 10.4088/JCP.15m10131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tubbs AS, Perlis ML, Basner M, et al. Relationship of nocturnal wakefulness to suicide risk across months and methods of suicide. J Clin Psychiatry. 2020;81(2):19m12964. 10.4088/JCP.19m12964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ballard ED, Vande Voort JL, Bernert RA, et al. Nocturnal wakefulness is associated with next-day suicidal ideation in major depressive disorder and bipolar disorder. J Clin Psychiatry. 2016;77(6):825–831. 10.4088/JCP.15m09943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vande Voort JL, Ballard ED, Luckenbaugh DA, et al. Antisuicidal response following ketamine infusion is associated with decreased nighttime wakefulness in major depressive disorder and bipolar disorder. J Clin Psychiatry. 2017;78(8):1068–1074. 10.4088/JCP.15m10440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perlis ML, Grandner MA, Chakravorty S, Bernert RA, Brown GK, Thase ME. Suicide and sleep: is it a bad thing to be awake when reason sleeps? Sleep Med Rev. 2016;29:101–107. 10.1016/j.smrv.2015.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rumble ME, McCall WV, Dickson DA, Krystal AD, Rosenquist PB, Benca RM. An exploratory analysis of the association of circadian rhythm dysregulation and insomnia with suicidal ideation over the course of treatment in individuals with depression, insomnia, and suicidal ideation. J Clin Sleep Med. 2020;16(8):1311–1319. 10.5664/jcsm.8508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koizumi T, Suzuki T, Pillai NS, et al. Circadian patterns of hallucinatory experiences in patients with schizophrenia: potentials for chrono-pharmacology. J Psychiatr Res. 2019;117:1–6. 10.1016/j.jpsychires.2019.06.019 [DOI] [PubMed] [Google Scholar]