SYNOPSIS
Objective
This study investigates maternal responsive parenting behaviors as a theorized buffer to the detrimental impact of maternal PTSD symptoms on young children’s depression and anxiety symptoms, disruptive behavior, and stress-related symptoms.
Design
A multi-ethnic sample of 242 trauma-exposed mothers and their preschool-aged children was assessed. Maternal responsive parenting behaviors were observed during standardized parent-child interactions. Maternal and child mental health symptoms were reported by mothers.
Results
Maternal PTSD symptoms were associated with their responsive parenting behaviors and predicted children’s mental health symptoms. Responsive parenting was inversely associated with children’s depression and stress-related symptoms. Moderation analyses revealed an interactive effect of maternal symptoms and responsive parenting on preschool children’s disruptive behavior and stress-related symptoms.
Conclusions
Responsive parenting behaviors can mitigate the ill effects of maternal PTSD symptoms. Nurturing relationships buffer the impact of maternal PTSD. Helping parents’ to sensitively respond to their young children’s distress can support positive outcomes in children.
Keywords: parenting, maternal mental health, posttraumatic stress, child mental health, early childhood
INTRODUCTION
Parental symptoms of PTSD are linked with increased risk for emotional distress and behavioral problems in their children, whether or not the child has also been exposed to trauma (for reviews, see Lambert, Holzer, & Hasbun, 2014; Leen-Feldner et al., 2013; Morris, Gabert-Quillen, & Delahanty, 2012; van Ee, Kleber, & Jongmans, 2016). Furthermore, when children of adults with PTSD are exposed to traumatic events, they are more likely to develop posttraumatic stress reactions themselves (Chemtob et al., 2010; Leen-Feldner et al., 2013).
However, not all children of parents with PTSD develop mental health symptoms, suggesting the existence of additional individual, environmental, and familial factors that may reduce this risk. This study investigates a possible buffer to the detrimental impact of maternal PTSD on young children’s functioning. We focus on a proximal and potentially modifiable feature of the family environment, maternal responsive parenting, among a diverse sample of trauma-exposed women and their children. Because there is multifinality in the effect of parental PTSD symptoms on children (Lambert et al., 2014), we examine a range of young children’s symptoms, including depression, anxiety, and stress-related symptoms as well as their disruptive behavior. We focus on young children because they may be especially vulnerable to disruptions in maternal functioning that can interfere with the attainment of key developmental tasks of early childhood (Goodman et al., 2010).
Parents who engage in responsive parenting are sensitive to their children’s needs, and respond appropriately, consistently, and contingently (Bornstein, Tamis-LeMonda, Hahn, & Haynes, 2008; Eshel, Daelmans, Carbral de Mello, & Martines, 2006). A large literature has documented direct associations between responsive parenting and positive psychosocial, cognitive, and behavioral outcomes (Eshel et al., 2006). Previous work has also demonstrated that responsive parenting can protect young children from a number of socioeconomic and maternal risks, but notably these studies rarely include violence exposure or maternal PTSD (Clark, Massey, Wiebe, Espy, & Wakschlag, in press; Ellis & Alisic, 2013; Katz, Stettler, & Gurtovenko, 2016; Shipman et al., 2007; Wakschlag & Hans, 1999; Wakschlag & Hans, 2002). Thus, how well these parenting behaviors may protect children from the intergenerational effects of their parents’ maltreatment experiences is less well understood.
PTSD and Parenting
Overall, the research examining associations between maternal PTSD and parenting is relatively sparse. Studies primarily focus on negative parenting styles and behaviors, and frequently rely on cross-sectional examinations and have shared method variance with reliance on maternal reports (Christie, Hamilton-Giachritsis, Alves-Costa, Tomlinson, & Halligan, 2019; van Ee et al., 2016). Within these limitations, the data provide fairly consistent evidence that maternal PTSD symptoms are associated with risk for increased aggressive, hostile, or inconsistent parenting behaviors (Christie et al., 2019; Van Ee, Kleber, & Mooren, 2012), more withdrawn or unavailable patterns of parent-child interaction (Schechter et al., 2010; van Ee et al., 2016), greater parenting stress (Christie et al., 2019), lower parenting satisfaction (Christie et al., 2019), and a tendency for mothers to view their children more negatively (van Ee et al., 2016).
Less attention has been paid to mothers with mental health problems who do not exhibit parenting deficits. These mothers are able to parent their children in a sensitive and responsive manner despite their own mental health challenges. Although it is theorized that symptoms of PTSD – especially behavioral avoidance and negative mood alterations – can interfere with the parent-child relationship (Creech & Misca, 2017), two recent reviews suggest that associations between PTSD and responsive parenting practices are somewhat inconsistent (Christie et al., 2019; van Ee et al., 2016). Although many studies have found that parents’ PTSD symptoms are associated with lower responsivity (e.g., Gewirtz, Polusny, DeGarmo, Khaylis, & Erbes, 2010; Schechter et al., 2010; Van Ee et al., 2012), others have found no association between PTSD and parental responsivity (Davis, Hanson, Zamir, Gewirtz, & DeGarmo, 2015; Samuelson, Wilson, Padron, Lee, & Gavron, 2017). This variability suggests that some parents are able to engage in sensitive and responsive interactions with their children, even in the face of their own trauma exposures and PTSD symptoms.
Responsive Parenting
Identifying parenting behaviors exhibited by mothers with PTSD that may be protective for their children has clear implications for the development of supportive interventions with parents experiencing PTSD symptoms. To this end, researchers have looked at sensitivity and responsiveness as potential buffers of the impact of parental mental health symptoms on children. The majority of this literature has examined this question among mothers with depression, finding that, indeed, a mother’s ability to respond to her children with warmth and sensitivity can serve as a protective factor for her children (Boyd & Waanders, 2013; Brennan, Le Brocque, & Hammen, 2003; Compas et al., 2010; Leckman-Westin, Cohen, & Stueve, 2009). However, to our knowledge, the potential buffering effect of responsive parenting has not been investigated among parents with PTSD. In fact, most studies of parenting among parents with PTSD have investigated direct effects (Christie et al., 2019; Creech & Misca, 2017) and, to a lesser degree, mediating pathways on children’s outcomes that typically involve negative parenting practices (Bryant et al., 2018; Greene, Chan, McCarthy, Wakschlag, & Briggs-Gowan, 2018). No studies that we are aware of have investigated the hypothesized moderating, protective effect of responsive parenting among parents with PTSD symptoms.
There is some emerging evidence to support the hypothesized protective effect of responsive parenting. Among female victims of intimate partner violence (IPV) and their toddler and preschool children, authoritative parenting and parent-child interactions characterized by low levels of negativity have been associated with children’s better psychosocial functioning and prosocial skills (Howell, Graham-Bermann, Czyz, & Lilly, 2010; Levendosky, Huth-Bocks, Shapiro, & Semel, 2003). Mothers in these studies exhibited high rates of depression and PTSD, and these psychological symptoms were also associated with children’s psychosocial functioning. Together, these studies provide important evidence that maternal psychological functioning and positive parenting may promote better outcomes for young children exposed to IPV. However, these studies did not statistically test whether positive parenting practices moderate the effects of maternal symptoms. Thus, an important next step is to determine whether positive parenting differentially buffers the effects of high versus low levels of maternal symptoms.
The Current Study
The goals of the current study were to investigate the use of responsive parenting practices by mothers of young children among a community sample of families experiencing high rates of poverty, maternal childhood maltreatment, and IPV exposure and to investigate the moderating effect of observed responsive parenting behaviors on the link between maternal PTSD symptoms and children’s stress-related, depressive, anxious, and disruptive behavior symptoms. Specifically, we hypothesized that children would be protected from the impact of maternal posttraumatic stress symptoms (i.e., have fewer symptoms) when their mothers were observed to engage in responsive parenting behaviors.
METHOD
Participants
The study utilizes a high-risk sample of families with young children (N = 497) participating in a longitudinal lab-based study in an urban region of the Midwest (Wakschlag et al, 2014). Participants in the lab-based study were recruited by stratified random sampling of a community-based survey sample of 1,857 3- to 5-year-olds in the Multidimensional Assessment of Preschoolers (MAPS) Study (for sampling details, see Nichols et al., 2015) and were restricted to children with no significant cognitive delays or neurocognitive conditions (e.g., Autism Spectrum Disorders) and English-speaking children and mothers. As the goal of the study was to investigate behavioral and environmental risks for psychopathology, families participating in laboratory visits were oversampled based on past-year intimate partner violence (IPV) or elevated child disruptive behavior.
The analytic sample for the current study consists of the subset of mothers who reported that they had experienced maltreatment during their childhood and/or intimate partner violence during their child’s lifetime and had complete data for all of the key study measures used in analyses (n=242). The analytic sample was evenly distributed by sex (48% boys) and diverse with respect to child’s ethnicity (51% African American, 32% Hispanic Latina, 16% European American, and 1% other). Half of the families (53%) were living on incomes below the poverty line, according to the ratio of income to need.
At the preschool laboratory visit, children’s M age was 4.6 years (SD =.83; range = 3.1–7.2). At this visit, mothers reported about IPV exposure and their PTSD and depressive symptoms, and maternal responsiveness was assessed in mother-child interactions. Child mental health data were collected by survey 6 months later (M child age = 5.44, SD = .88). Mean maternal age at the birth of the target child was 30.4 years (SD = 6.4; range = 18–47). Ninety-three percent of mothers were positive for having experienced childhood maltreatment (including physical abuse and neglect, emotional abuse and neglect, and sexual abuse). Twenty-nine percent of mothers reported experiencing physical IPV during the child’s lifetime; 22% of mothers had experienced both childhood trauma and physical IPV. Based on mothers’ report, 64% of the children had experienced at least one traumatic event; 17% had experienced 3 or more. This analytic sample was comparable to the excluded 255 families in terms of mother’s age and child’s age, gender, and ethnicity, ps > .10. A higher percentage of families lived below the poverty line (53% versus 44%) among the analytic sample as compared to the excluded families. Eighteen mothers (7%) who experienced trauma were lost to follow-up between the initial laboratory visit and the completion of the 6-month survey in which mothers’ provided the child mental health data and were therefore not included in the final analytic sample. These mothers did not differ from the analytic sample in terms of mother’s age, child’s age, PTSD symptoms, ethnicity or economic level (p > .05). However, there was a higher percentage of boys (78% versus 48%) among the families that did not complete the child symptom data, and on average the mothers responsive parenting scores were higher, compared to the analytic sample (M = 14.33 versus 12.60)
Procedures
Participants attended two laboratory visits that included maternal interviews and questionnaires to assess children’s mental health, family environment, and childrearing practices. Mothers were compensated for participation and transportation, and they provided informed consent. Study protocols were approved by two institutional review boards. Mandated child abuse and neglect reporting procedures were followed, with reports of suspected maltreatment made to Child Protective Services. All mothers were given parenting resource and referral information at the end of the visit, and additional consultative follow-up was provided for families in distress.
Mothers and children were videotaped during a standardized clinical observational paradigm designed to elicit variations in young children’s response to a range of contextual demands with the parent, including mildly stressful tasks designed to elicit frustration and/or disappointment (clean up a box of crayons, refrain from playing with enticing toys on a shelf, and complete a difficult puzzle) and opportunities to observe parental behaviors in the course of these interactions (Wakschlag et al., 2008). For further details about the tasks refer to Petitclerc et al (2015). The coding system used to assess parental behavior is described in the Measures section.
Measures
Instruments used to assess maternal and child symptoms are described below, and the descriptive statistics for each are included in Table 1. Recommended scoring guidelines were followed for each measure: when published norms were available, scores were converted to T-scores; for all other scales, composite scores were created such that each subscale contributed equally to the total. Sample items and detailed descriptions of these procedures are included below.
Table 1.
Bivariate associations and descriptive statistics for primary variables and demographic variables.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Child’s age (years) | ___ | .00 | −.03 | −.01 | −.02 | −.04 | −.12 | −.11 | −.14* | .06 | −.04 |
| 2. | Child’s gender | ___ | −.09 | .02 | .02 | .00 | .00 | .01 | .01 | −.09 | −.12 | |
| 3. | Mother’s age | ___ | −.37*** | −.17** | −.05 | .29*** | −.15* | −.17** | −.22** | .04 | ||
| 4. | Poverty | ___ | .23*** | .20** | −.26*** | .14* | .28*** | .17** | .08 | |||
| 5. | Maternal PTSD | ___ | .50*** | −.13* | .37*** | .29*** | .29*** | .23*** | ||||
| 6. | Maternal depression | ___ | −.18** | .39*** | .30*** | .25*** | .30*** | |||||
| 7. | Responsive parenting | ___ | −.19** | −.10 | −.34*** | −.03 | ||||||
| 8. | Child stress symptoms | ___ | .52*** | .62*** | .52*** | |||||||
| 9. | Child anxiety | ___ | .48*** | .52*** | ||||||||
| 10. | Child depression | ___ | .50*** | |||||||||
| 11. | Child disruptive behavior | ___ | ||||||||||
| M or % | 5.45 | 48% male | 30.40 | 53% poor | 27.91 | 48.07 | 12.60 | 47.94 | .49 | .18 | .08 | |
| SD | 0.88 | _ | 6.42 | _ | 11.76 | 9.33 | 3.41 | 11.27 | .33 | .26 | .94 | |
| Range | 3.8–8.3 | _ | 18–47 | _ | 17–82 | 37–76 | 1–20 | 40–110 | 0–1.78 | 0–1.44 | −1.5–3.6 |
p< .05.
p < .01.
p <.001.
Maternal Current Posttraumatic Stress Symptoms
PTSD Check List – Civilian version (PCL-C; Weathers, Litz, Herman, Huska, & Keane, 1993). Mothers rated how much symptoms related to their traumatic experiences had bothered them in the past month (0 = Not at All, 1 =A Little Bit, 2 = Moderately, 3 = Quite a Bit, 4 = Extremely). The 17 items are based closely on the DSM-IV (American Psychiatric Association, 2000) symptoms for PTSD (e.g., “In the past month, how much were you bothered by repeated, disturbing, memories, thoughts or images of a stressful experience from the past?”). A total PTSD symptom severity score was calculated as the sum of all 17 items (current sample α= 0.93).
Maternal Responsive Parenting
Parenting Clinical Observation Schedule (P-COS; Hill, Maskowitz, Danis, & Wakschlag, 2008). The P-COS assesses competent and problematic parenting behavior during the parent-child interaction paradigm. Mother-child interactions were coded by independent observers globally to capture parenting behaviors across the tasks, with ratings that integrate frequency and qualitative dimensions of parenting behavior to create a continuum of parenting behaviors. The Responsive Involvement domain includes assessments of 7 codes: scaffolding (e.g., putting a desired but prohibited toy out of reach), positive engagement (e.g., attends to the child in a manner that conveys pleasure in the shared experience, and remains engaged in the face of challenging situations), intensity and pervasiveness of maternal positive affect (as conveyed by maternal expression, tone, animation, and behavior), warm affection (physical behavior and verbal statements that are appropriate and not intrusive), labelling (e.g., use of an emotion word to label the feeling being communicated by the child’s behaviors), and responsiveness to the child’s emotions and behaviors (e.g., praise for good behavior or encouragement in the face of frustration). Ratings for each code were made on a 4-point scale from 0 (none) to 3 (high) that captures a continuum of competent to clinically concerning caregiver behavior and takes into account the appropriateness and effectiveness of the parental response to the child’s behavior and affect, and summed to create a total Responsive Involvement score (current sample α = .78). Twenty percent of videotapes were coded by a second coder to establish inter-rater reliability: Weighted kappas for individual items comprising the Responsive Involvement scale ranged from 0.48 to 0.78 and the ICC for the scale score was 0.81 (0.72–0.88).
Child Stress-Related Symptoms
Trauma Symptom Checklist for Young Children (TSCYC; Briere, 2005). The TSCYC is a norm-referenced measure of children’s trauma-related symptoms that is developmentally appropriate for use with young children. It can be used to assess trauma symptoms in normative and clinical populations (Wherry & Dunlop, 2017) and as such does not require a criterion event. In effect, it captures children’s stress reactivity, which may be related to trauma, but might also manifest in young children who have not experienced criterion events. For the current study, mothers rated their child’s arousal (e.g., “Being easily startled”), avoidance (e.g., “Not wanting to talk about something that happened to him/her”), and intrusion symptoms (e.g., “Bad dreams or nightmares”) on a 5-point scale ranging from Not true at all to Very often true. These were summed to create a total stress score and converted to a T-score using published norms (for the composite scale, current sample α = 0.85).
Child Depression and Anxiety Symptoms
Children’s depression and anxiety symptoms were assessed with the Separation Anxiety, General Anxiety, and Depression subscales of the Preschool version of the Infant-Toddler Social and Emotional Assessment (P-ITSEA; Briggs-Gowan & Carter, 2012). The P-ITSEA is an adaptation of an existing measure of young children’s social-emotional development that has well-established reliability and validity. Parents are asked to rate their children’s symptoms in the past month on a 3-point scale (Not True/Rarely, Somewhat True/Sometimes, or Very True/Often). The 9-item Depression subscale (α = 0.77) of the P-ITSEA was used to assess depression symptoms (e.g., “Looks unhappy or sad without any reason” and “Has less fun than other children”) and was created by using the mean of the items. The 5-item Separation Anxiety (e.g., “Cries or hangs onto parent when he or she tries to leave;” α = 0.67) and 10-item General Anxiety (e.g., “Seems nervous, tense, or fearful;” α = 0.72) subscales of the P-ITSEA were correlated, r(237) = .40, p < .001. The mean score of the two subscales was used to form a composite anxiety symptoms scale.
Child Disruptive Behavior
Multidimensional Assessment Profile of Disruptive Behavior (MAP-DB; Wakschlag et al., 2014). The MAP-DB is a parent-report dimensional questionnaire designed to capture normative to clinically concerning variation in young children’s disruptive behavior. Parents were asked to rate children’s disruptive behavior symptoms on the 25-item Aggression (e.g., “Gets into fights”), 22-item Noncompliance (e.g., “Argues when asked to do something”), 22-item Temper Loss (e.g., “Yells angrily at someone”), and 9-item Low Concern (e.g., “Enjoys making others mad”) subscales using a 6-point scale ranging from 0 (never) to 5 (many times each day). Scores were generated using item response theory methods, consistent with the original development and validation of the scales (Wakschlag et al., 2014). A composite disruptive behavior score was generated by taking the mean of the four scales. Internal consistency for the combined scale was excellent (α = .94).
Maternal Childhood Maltreatment Experiences
Eligibility for the analytic sample on the basis of childhood maltreatment was determined based on their reports on the Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998). The CTQ is a widely-used 28-item self-report inventory assessing five types of trauma experienced as a child and/or teenager: emotional, physical and sexual abuse, and emotional and physical neglect (e.g., “People in my family hit me so hard that it left me with bruises or marks.”). Each of these scales has 5 items that are rated on a 5-point scale according to their frequency (1 = never true to 5 = very often true) and summed to yield a total score for each type of trauma, ranging from 5 to 25, with higher scores indicating greater severity. To identify mothers with any history of childhood maltreatment, mothers scoring above the mild-moderate threshold in any category (>9 for emotional abuse, >8 for physical abuse, >6 for sexual abuse, >10 for emotional neglect, and > 10 for physical neglect) were considered positive for childhood maltreatment, following the recommended guidelines (Bernstein & Fink, 1998). The CTQ has acceptable convergent validity, test-retest reliability, and internal consistency in both clinical and community samples (Scher, Stein, Asmundson, McCreary, & Forde, 2001). Internal consistency was acceptable for all scales in the current sample (.70 to .94).
Maternal Physical IPV Experiences
Eligibility for the analytic sample on the basis of mothers’ partner violence experiences was assessed using the partner conflict section of the Family Socialization Interview – Revised (FSI-R; O’Dor et al., 2017, adapted from Dodge, Pettit & Bates, 1994), a semi-structured interview from the child’s birth to the present, with established reliability and validity. Physical violence victimization was coded based on descriptions of the severity and frequency of violent conflict between the mother and another adult that were witnessed (or potentially witnessed) by the child during his/her lifetime. Physical IPV was coded by independent raters on a five-point scale where 0 = no conflict, 1 = a single, moderate episode; 2 = repeated, moderate episodes; 3 = a single, severe episode; 4 = repeated, severe episodes; and 5 = severe episodes occurring weekly or more often. Videotaped interviews were coded by trained interviewers, with 20% reliability monitored throughout the coding process and bi-weekly consensus meetings to maintain reliability. This code has demonstrated acceptable inter-rater reliability (Weighted Kappas ranged from 0.80 to 1.0). In the current study, physical IPV scores >= 1 during the child’s lifetime were used to select the analytic sample.
Maternal Current Depressive Symptoms
Patient-Reported Outcomes Measurement Information System (PROMIS) Short Form – Depression (Pilkonis et al., 2011). Mothers completed this 8-item self-report that assesses negative mood, views of self, social cognition, and decreases in positive affect and engagement in the past 7 days on a 5-point scale (1 = Never, 2 = Rarely, 3 = Sometimes, 4 = Often, 5 =Always) (current sample α= 0.94). Sample items include, “I felt sad.” and “I felt helpless.” Raw scores were converted to T-scores, following recommended scoring guidelines (PROMIS, 2012).
Analytic Plan
All analyses were conducted using SPSS version 21. Descriptive statistics were calculated for all study variables and preliminary analyses examined inter-relations among study variables. Relations among study variables and child’s age, child’s gender, mother’s age, and poverty status (dichotomous) were investigated with Pearson correlations. A one-way analysis of variance (ANOVA) was conducted to evaluate the associations among primary study variables and the child’s ethnicity.
Multiple regression analyses were used to test the hypothesized moderating effect of responsive parenting behaviors on the specific links between maternal PTSD symptoms and children’s stress-related, depressive, anxious, and disruptive behavior symptoms in preschool. Prior to running the regression analyses, outcome variables were examined for normality by checking for significant levels of skewness and kurtosis. Children’s stress-related symptoms and children’s depression symptoms were identified to have significant skew (>2; West, Finch, & Curran, 1995) and therefore were either log- (stress-related symptoms) or square root- (depressive symptoms) transformed following the method of Tabachnik and Fidell (2007). Predictor and moderator variables were converted to z-scores and examined for outliers. Using the cut-off of +/−3.5, 1 outlier in the maternal PTSD variable was identified and reined in (i.e., assigned the value +3.5). In each model, demographic covariates associated with the outcome variable were entered in the first step; maternal PTSD symptoms were entered in the second step; observed responsive parenting behaviors were added in the third step; and the interaction term between the maternal parenting and mental health variables was added in the fourth step. Finally, because maternal PTSD and depressive symptoms were highly correlated, r(231) = .50, a supplemental set of regression models was examined in which maternal depressive symptoms were included as a covariate in Step 1. The purpose of these models was to evaluate whether the hypothesized buffering effects of responsiveness (i.e., PTSD x responsiveness interactions) were robust to the inclusion of this correlated and comparatively better understood risk factor.
RESULTS
Descriptive Statistics
The means, standard deviations, and bivariate associations of the primary study variables and key demographic variables are presented in Table 1. Children’s symptoms at preschool were strongly associated with maternal PTSD symptoms. Children’s stress-related and depression symptoms were associated with observed parenting behaviors, and children’s stress-related, anxious and depressive symptoms were associated with poverty, but disruptive behavior symptoms were not associated with either of these constructs. Observed parenting behaviors were associated with maternal PTSD and depressive symptoms. Not surprisingly, maternal PTSD and depressive symptoms were intercorrelated, as were children’s symptoms. Ratings of parenting behaviors did not vary among the mothers of African American, Hispanic/Latinx, and European American children when poverty was controlled, F(3,237) = 1.19, ns. Poverty, mothers’ age, and child’s age were controlled in the regression analyses.
Responsive Parenting as a Moderator of Maternal PTSD and Child Mental Health Symptoms
Multiple regression models were utilized to evaluate associations among maternal PTSD symptoms and maternal responsive parenting behaviors at the laboratory visit, and children’s mental health symptoms 6 months later (Table 2). Main effects were found for maternal PTSD symptoms on children’s depression, anxiety, disruptive, and stress-related symptoms (Step 2), controlling for child age, maternal age, and poverty in these models (βs ranging from .17 to .33, ps ranging from .009 to < .001, R2Δ ranging from .03 to .11). Controlling for maternal PTSD symptoms, a main effect was also found for maternal responsive parenting on children’s depression and stress-related symptoms, R2Δ= .07 and .02 respectively, but not for children’s anxious or disruptive symptoms (Step 3).
Table 2.
Multiple regression analyses examining associations of maternal health symptoms and responsive parenting on preschool child symptoms.
| Preschool Child Mental Health
Symptoms |
||||||||
|---|---|---|---|---|---|---|---|---|
| Depression (ITSEA) |
Anxiety (ITSEA) |
Disruptive
(MAPS-DB) |
Stress-Related Symptoms
(TSCYC) |
|||||
| Predictor | β | p | β | p | β | p | β | p |
| Step 1: Child’s age at preschool visit | .06 | .373 | −.14 | .026 | −.04 | .504 | −.09 | .161 |
| Mother’s age at baseline visit | −.13 | .046 | −.10 | .142 | −.02 | .805 | −.10 | .164 |
| Poverty | .14 | .034 | .22 | .001 | .09 | .216 | .10 | .125 |
| R2Δ = .06 | R2Δ = .09 | R2Δ = .01 | R2Δ = .03 | |||||
| Step 2: Maternal PTSD symptoms | .17 | .009 | .24 | <.001 | .23 | <.001 | .33 | <.001 |
| R2Δ = .03 | R2Δ = .05 | R2Δ = .05 | R2Δ = .11 | |||||
| Step 3: Responsive parenting | −.28 | <.001 | −.03 | .639 | .01 | .907 | −.14 | .030 |
| R2Δ = .07 | R2Δ = .00 | R2Δ = .00 | R2Δ = .02 | |||||
| Step 4: Maternal PTSD × responsive parenting | −.08 | .24 | .01 | .945 | −.16 | .026 | −.24 | <.001 |
| R2Δ = .005 | R2Δ = .00 | R2Δ = .02 | R2Δ = .05 | |||||
|
|
||||||||
| Total R2 | .16 | <.001 | .14 | <.001 | .08 | .003 | .20 | <.001 |
Note. In each step, only the predictor added into the model at that step is listed in the table; however, all previously entered predictors were included in subsequent steps.
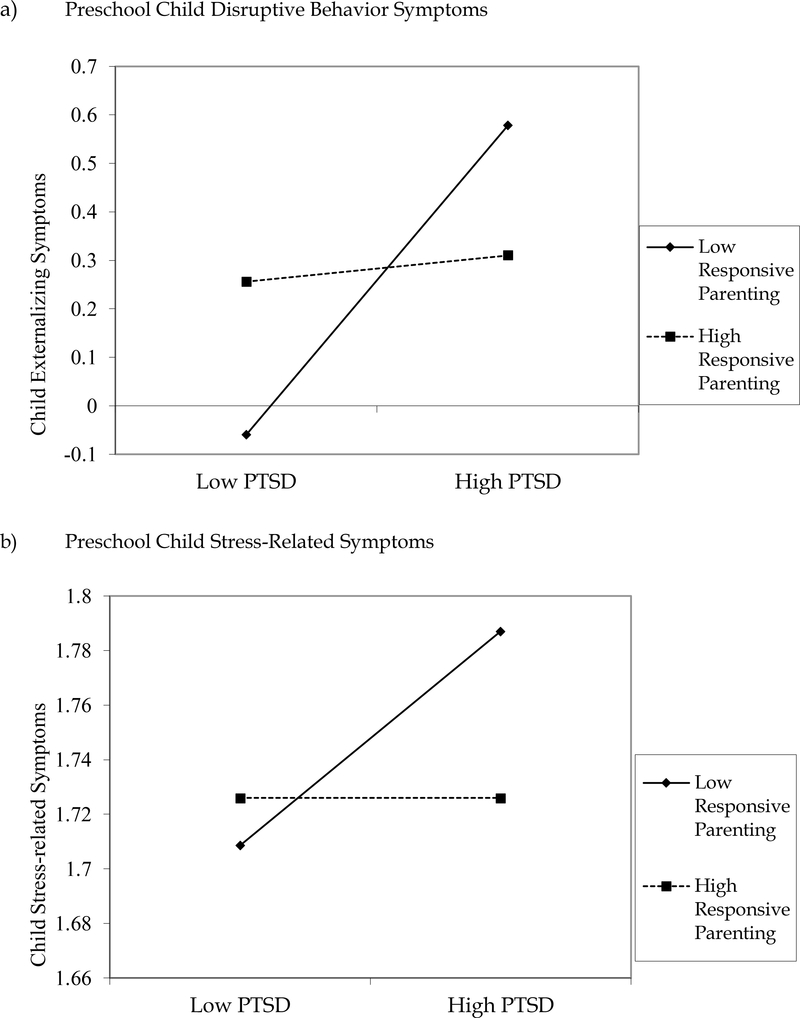
An interaction term was included in each model to test for moderation. The interaction between maternal PTSD symptoms and responsive parenting was significant for children’s disruptive behavior and stress-related symptoms (Step 4). Follow-up analyses of these interactions were conducted by plotting graphically the moderator (responsive parenting) at 1 SD above and below the M and examining the simple slopes (Figure 1). For disruptive behavior, there was no effect of maternal symptoms on child symptoms when responsive parenting was high, simple slope = 0.03, t = 0.27, ns. However, there was an effect of maternal symptoms on child symptoms when responsive parenting was low, simple slope = 0.32, t = 4.12, p < .001. Results were similar for stress-related symptoms, such that there was an effect of maternal symptoms on child symptoms only when responsive parenting was low, simple slope = 0.04, t = 6.48, p < .001.
Figure 1.
Interactions between maternal responsive parenting and maternal PTSD symptoms predicting (a) preschool child disruptive behavior symptoms and (b) preschool child stress-related symptoms. The moderator (responsive parenting) is plotted at +/− 1 SD. Simple slope of low responsive parenting is significant at p < .001 for both graphs
Because of the high correlation between maternal PTSD and depressive symptoms, and the well-documented deleterious effect of maternal depression on children’s mental health symptoms, a second set of multiple regression models was examined to determine whether the same pattern of interaction effects would be observed when maternal depression was included as a covariate in Step 1 of the model. Results of these analyses were largely the same as the results of the analyses without maternal depression in the model: Responsive parenting continued to moderate the association between maternal PTSD symptoms and children’s disruptive and stress-related symptoms and the interactions for child depression and anxiety remained non-significant (additional details available in Supplemental Material).
DISCUSSION
Strong evidence supports the negative impact of maternal PTSD on children’s mental health functioning among community and clinical samples (Chemtob et al., 2010; Lambert et al., 2014; Leen-Feldner et al., 2013). For this reason, we examined the potential for responsive parenting to buffer the risk associated with maternal PTSD in a sample of trauma-exposed mothers, half of whom were living below the poverty line, and their preschool-aged children. Among these mother-child dyads, mothers’ PTSD symptoms predicted the depression, anxiety, stress-related, and disruptive behavior symptoms of their preschool aged children, even after controlling for the influence of poverty on children’s symptoms. Mothers’ responsive parenting moderated this relation for children’s stress-related and disruptive behavior symptoms, such that there was only an association between maternal PTSD symptoms and children’s symptoms when responsive parenting was low.
The literature suggests that there is an increased risk for parents with PTSD to have difficulty engaging in responsive or positive parenting (van Ee et al., 2016). Consistent with these studies, in the current sample mothers’ PTSD symptoms were correlated with independent observers’ ratings of their responsive parenting behaviors. However, this association was relatively modest, r = .13, p< 05, suggesting that there was heterogeneity in women’s parenting behaviors along the spectrum of PTSD symptoms. Mothers reporting both high and low levels of PTSD symptoms were likely to be demonstrating high and low levels of responsivity. This study supports what others have also found – that there is variability among the parenting behaviors of mothers, even those who are dealing with adversity, trauma, or mental health symptoms (Graham-Bermann, Gruber, Howell, & Girz, 2009; Greeson et al., 2014; Letourneau, Fedick, & Willms, 2007; Wakschlag & Hans, 1999). Additional research is warranted to further explore the heterogeneity in parenting behaviors and identify the resilience factors that support engagement in responsive parenting among mothers with high levels of PTSD symptoms.
One possible resilience factor is emotion regulation; mothers who are responsive to their children’s needs in spite of their own emotional distress may possess greater emotion regulation skills. A review of the literature examining parenting and maternal emotional control concluded that higher maternal emotion regulation is associated with more positive parenting behaviors, lending credence to this supposition (Crandall, Deater-Deckard, & Riley, 2015). Likewise, a study by McCullough and colleagues (2017) found that mothers’ experiences of emotional maltreatment were associated with greater risk of emotionally unsupportive parenting only in the context of high emotion dysregulation. Thus, future studies might investigate whether emotion regulation serves as a mechanism in (mediates) the association between maternal PTSD and responsive parenting.
The current study examined responsive parenting as a potential buffer of the ill effects of maternal PTSD symptoms on children’s symptoms. Emotionally responsive parents attend to their children with warmth and affection and respond to negative child affect with behaviors that help their children to learn to regulate themselves, such as scaffolding, labeling, helping them to make sense of their experiences, and modeling strategies for young children to co-manage their negative affect. Results from this community sample suggest that these behaviors may offset some of the risks incurred by maternal psychopathology. That is, a mother’s ability to respond to her child with warmth and sensitivity, even while struggling with her own significant symptoms of PTSD, can serve as a protective factor for her young child.
Although maternal PTSD symptoms were universally associated with increased mental health symptoms in their young children, different patterns emerged for the direct and moderating associations among responsive parenting and each of the categories of children’s symptoms. These varied patterns suggest that there may be specificity to the protective effects of responsive parenting.
Intergenerational trauma exposure was high in this sample of mothers who had experienced trauma; nearly two-thirds of their preschool aged children had already experienced at least one traumatic event. Although when children of adults with PTSD are exposed to traumatic events they are more likely to develop posttraumatic stress reactions themselves, in this sample only children in the low responsive parenting group had elevated levels of stress-related symptoms. This finding suggests that maternal responsive parenting mitigated the added risk of maternal PTSD symptoms on children’s development of stress–related symptoms, thus serving as a protective factor (Rose, Holmbeck, Coakley, & Franks, 2004). The safety and security that these mothers provide their children when they respond sensitively to their children’s negative affect appears to support their children’s resilience to the ill effects of exposure to trauma, maternal PTSD symptoms, and other environmental stressors.
Responsive parenting also protected against the development of children’s disruptive behavior symptoms among children of mothers with high levels of PTSD symptoms. For these dyads, only low-responsive mothers had children at higher risk for disruptive behavior, which is consistent with prior work showing that it is the “double whammy” of exposure to adversity and an unresponsive parenting environment that jointly contribute to increased risk of disruptive behavior in offspring (Clark et al., in press; Wakschlag & Hans, 1999; Wakschlag & Hans, 2002; Wakschlag et al., 2011).
Maternal responsive parenting did not interact with maternal PTSD symptoms in the association with children’s depression and anxiety. Rather, there was a direct effect of responsive parenting on children’s depression, suggesting that having a mother who is emotionally responsive benefitted all children in the study. In contrast, there was no direct effect between responsive parenting and children’s anxious symptoms in this sample. This lack of association may be explained by prior work suggesting that highly responsive parenting may, in fact, be moderated by children’s fearful temperament (Kochanska, Aksan, & Joy, 2007). In fearful children, responsive parenting may be more likely to contribute to maladaptive behavior because it serves to reinforce the child’s anxious behavior and avoidance.
Maternal responsive parenting exhibited protective effects among this sample of trauma-exposed mothers and their children (93% of mothers experienced childhood trauma experiences, 29% of mothers experienced physical IPV during the child’s lifetime, and 64% of children had experienced at least one traumatic event). Much has been written about the potential intergenerational effect of parents’ traumatic experiences on offspring. The evidence is clear across a broad spectrum of survivors of violence – from survivors of war and genocide (Daud, Skoglund, & Rydelius, 2005; Field, Muong, & Sochanvimean, 2013; Yehuda, Schmeidler, Wainberg, Binder-Brynes, & Duvdevani, 1998), combat (Dekel & Goldblatt, 2008), IPV (Levendosky & Graham-Bermann, 2001; Zarling et al., 2013), and childhood maltreatment (Martinez-Torteya et al., 2014; Min, Singer, Minnes, Kim, & Short, 2012; Plant, Jones, Pariante, & Pawlby, 2017) – that children of violence-exposed parents are at increased risk for psychopathology, altered stress response, and impairment. Parents’ posttraumatic adjustment, including their ability to respond consistently and supportively to their children, may be an important factor to consider in their children’s outcomes. For example, the current findings are consistent with studies that have associated positive parenting with more resilient outcomes among young children in families with IPV (Greeson et al., 2014; Gustafsson, Cox, & Blair, 2012; Howell et al., 2010). This study expands this research by identifying a potential mechanism for this association. That is, our results suggest that responsive parenting may be associated with positive outcomes for children in trauma-exposed families because such parenting helps to protect young children against the ill effects of their mothers’ posttraumatic stress symptoms.
However, there is still much to be learned about how maternal PTSD symptoms interfere with children’s healthy development as well as how responsive parenting protects against these processes. Mothers who respond sensitively to their children’s needs provide an environment in which children feel safe and secure and learn the skills to manage their negative emotions. As previously noted, mothers who are emotionally regulated are likely better able to engage in these responsive behaviors. Simultaneously, they are also modeling their own affective control. Thus, the combination of emotion regulation and responsive parenting may be providing two potent means by which mothers socialize their children’s emotion regulation skills (Eisenberg, Cumberland, & Spinrad, 1998) and thereby protect children from developing their own psychopathology. These promising findings underscore the need for further research into these potential mechanisms.
Limitations
Our current analyses examined associations between maternal PTSD symptoms, responsive parenting, and children’s symptoms in a number of domains. We chose to focus on parenting because it is a potentially modifiable influence on children’s outcomes. However, there are alternative influences and explanations that must also be considered. First, we recognize that a complex array of factors can affect both children’s and mother’s symptoms and behaviors, many of which were not assessed in our study. These include, but are not limited to, children’s temperament and genetics, maternal and child emotion regulation, fathers and other family members, environmental stress, and social support. Second, the effects that we have identified may be bidirectional. That is, children can and do influence parents, just as parents influence children, and these effects interact over time (Davidov, Knafo-Noam, Serbin, & Moss, 2015). Indeed, transactions over time among children’s prosocial, internalizing, and externalizing symptoms and both positive and controlling parenting behaviors have been documented (Del Vecchio & Rhoades, 2010; Lansford et al., 2017; Milan & Carlone, 2018; Pastorelli et al., 2016; Pinquart, 2016). In the current sample, therefore, it is possible that children’s stress-related and disruptive behavior symptoms make it more difficult for some mothers with PTSD to regulate their emotions, and thus their ability to respond sensitively. Furthermore, the effects of child temperament, symptoms, and behavior may contribute to, or be particularly salient for parents with high levels of, parenting stress (Deater-Deckard, 1998), a relevant consideration for the current sample of highly stressed mothers which also might influence their ability to respond supportively to their children. Unfortunately, our data and design do not allow a fully longitudinal exploration of transactions among maternal PTSD, responsive parenting, and child symptoms. Although our current data do not support the testing of these more complex models, our results must be considered within the context of these alternative dynamics that are potentially at play.
Several additional limitations should also be noted. Our sample consisted solely of mothers; the impact of paternal psychopathology and parenting are likewise important influences on children’s outcomes and warrant inclusion in future studies. All of the maternal and child mental health symptoms are mother-reported via questionnaire and thus subject to bias, although it is worth noting that responsive parenting was assessed via observational coding of mother-child interactions. In addition, our sample consisted of a community sample of women at risk for PTSD; future exploration of these findings among a clinical sample of mothers who might be experiencing a higher level of PTSD symptoms is warranted to determine if responsive parenting continues to buffer the effects of more severe PTSD symptoms.
IMPLICATIONS FOR PRACTICE
There is growing recognition of the ability of nurturing and stable relationships to buffer the impact of childhood adversity, and in turn a number of child mental health intervention programs are focusing on increasing parents’ capacity to provide this support (Morris et al., 2017). But we must also recognize that many parents seeking mental health care for their children are experiencing poverty, high levels of stress, and frequently their own traumatic experiences, and as a result are also experiencing high rates of psychological distress (Swartz et al., 2005). Thus, addressing both the parent-child relationship as well as parental mental health within childhood mental health treatment approaches is warranted.
Fortunately, maternal sensitivity to a young child’s distress has been shown to be modifiable in treatment (Bernard, Simons, & Dozier, 2015; Brahm et al., 2016; Suchman et al., 2010; van IJzendoorn, Juffer, & Duyvesteyn, 1995). Dozier and colleagues, for example, have demonstrated that a short-term parenting intervention is effective in increasing maternal responsiveness to children’s cues of distress among Child Protective Service-referred mothers of children 4–6 years old (Bernard et al., 2015). Interventions focused on parental emotion socialization also provide evidence that mothers’ strategies for responding to children’s negative affect can be enhanced (Havighurst et al., 2015; Herbert, Harvey, Roberts, Wichowski, & Lugo-Candelas, 2013).
In addition, studies have documented that intervening with mothers to reduce their mental health symptoms can reduce children’s symptoms (Gunlicks & Weissman, 2008; Overbeek, De Schipper, Willemen, Lamers-Winkelman, & Schuengel, 2017). Overbeek et al. (2017), for example, found that decreases in parental mental health problems over the course of an intervention for IPV-exposed children and their parents were associated with decreases in children’s posttraumatic stress symptoms. Furthermore, these reductions in parental psychopathology mediated the association between nonspecific intervention factors during parent sessions – such as positive attention and inviting parents to share their parenting experiences – and children’s lower posttraumatic stress symptoms.
Together, these two bodies of literature and the current findings support a two-generation approach to children’s treatment (Shonkoff & Fisher, 2013) that both acknowledges and also addresses parents’ own mental health challenges, while supporting the development of responsive parenting, particularly the recognition of and sensitive response to young children’s emotional distress.
The results of the current study underscore the importance of recognizing the role of maternal mental health as a risk factor for children’s poor mental health outcomes and the ability of responsive parenting practices to mitigate its impact on young children. By helping parents become more affectively regulated, they may be better able to assist their children in using adaptive emotion regulation skills when distressed and thereby support resilient outcomes for their children.
Supplementary Material
Acknowledgements
The authors thank the reviewers for their comments on prior versions of this manuscript. The ideas and opinions expressed herein are those of the authors alone, and endorsement by the authors’ institutions and the National Institute of Mental Health is not intended and should not be inferred.
Funding
This work was supported by Grants R01MH090301, R01MH082830, and U01MH082830 from the National Institute of Mental Health. The MacArthur Health and Behavior Questionnaire was made available free of charge by the John D. and Catherine T. MacArthur Foundation Research Network on Psychopathology and Development (David J. Kupfer, Network Chair).
Footnotes
Conflict of Interest Disclosures
Each author signed a form for disclosure of potential conflicts of interest. No authors reported any financial or other conflicts of interest in relation to the work described.
Ethical Principles
The authors affirm having followed professional ethical guidelines in preparing this work. These guidelines include obtaining informed consent from human participants, maintaining ethical treatment and respect for the rights of human or animal participants, and ensuring the privacy of participants and their data, such as ensuring that individual participants cannot be identified in reported results or from publicly available original or archival data.
Role of the Funders/Sponsors
None of the funders or sponsors of this research had any role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Contributor Information
Carolyn A. Greene, Department of Psychiatry, University of Connecticut School of Medicine, 65 Kane Street, West Hartford, Connecticut 06119.
Kimberly J. McCarthy, University of Connecticut School of Medicine
Ryne Estabrook, University of Illinois at Chicago.
Lauren S. Wakschlag, Northwestern University
Margaret J. Briggs-Gowa, University of Connecticut School of Medicine
REFERENCES
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, D.C.: Author. [Google Scholar]
- Bernard K, Simons R, & Dozier M (2015). Effects of an attachment-based intervention on child protective services--referred mothers’ event-related potentials to children’s emotions. Child Development, 86(6), 1673–1684. doi: 10.1111/cdev.12418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, & Fink L (1998). Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Bornstein MH, Tamis-LeMonda CS, Hahn C-S, & Haynes OM (2008). Maternal responsiveness to young children at three ages: Longitudinal analysis of a multidimensional, modular, and specific parenting construct. Developmental Psychology, 44(3), 867–874. doi: 10.1037/0012-1649.44.3.867 [DOI] [PubMed] [Google Scholar]
- Boyd RC, & Waanders C (2013). Protective factors for depression among African American children of predominantly low-income mothers with depression. Journal of Child & Family Studies, 22(1), 85–95. doi: 10.1007/s10826-012-9588-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brahm P, Cortazar A, Fillol MP, Mingo MV, Vielma C, & Aranguiz MC (2016). Maternal sensitivity and mental health: does an early childhood intervention programme have an impact? Family Practice, 33(3), 226–232. [DOI] [PubMed] [Google Scholar]
- Brennan PA, Le Brocque R, & Hammen C (2003). Maternal Depression, Parent–Child Relationships, and Resilient Outcomes in Adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 42(12), 1469–1477. doi: 10.1097/00004583-200312000-00014 [DOI] [PubMed] [Google Scholar]
- Briere J (2005). Trauma Symptom Checklist for Young Children (TSCYC): Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc. [Google Scholar]
- Briggs-Gowan MJ, & Carter AS (2012). Manual for the Preschool ITSEA: Adaptation of the Infant-Toddler Social Emotional Assessment for Preschool-age Children. Farmington, CT: University of Connecticut and University of Massachusetts. [Google Scholar]
- Bryant RA, Edwards B, Creamer M, O’Donnell M, Forbes D, Felmingham KL, … Hadzi-Pavlovic D (2018). The effect of post-traumatic stress disorder on refugees’ parenting and their children’s mental health: a cohort study. Lancet Public Health, 3, e249–258. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, & Abramovitz R (2010). Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children’s behavior. Child Development, 81(4), 1129–1141. doi: 10.1111/j.1467-8624.2010.01458.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie H, Hamilton-Giachritsis C, Alves-Costa F, Tomlinson M, & Halligan SL (2019). The impact of parental posttraumatic stress disorder on parenting: a systematic review. European Journal of Psychotraumatology, 10(1), 1550345. doi: 10.1080/20008198.2018.1550345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark CAC, Massey S, Wiebe SA, Espy KA, & Wakschlag LS (in press). Does maternal responsiveness buffer prenatal tobacco exposure effects on young children’s behavioral disinhibition? Development & Psychopathology. doi: 10.1017/S0954579418000706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J, … Roberts L (2010). Coping and parenting: Mediators of 12-month outcomes of a family group cognitive-behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology, 78(5), 623–634. doi: 10.1037/a0020459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall A, Deater-Deckard K, & Riley AW (2015). Maternal emotion and cognitive control capacities and parenting: A conceptual framework. Developmental Review, 36, 105–126. doi: 10.1016/j.dr.2015.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creech SK, & Misca G (2017). Parenting with PTSD: A Review of Research on the Influence of PTSD on Parent-Child Functioning in Military and Veteran Families. Frontiers in Psychology, 8, 1101–1101. doi: 10.3389/fpsyg.2017.01101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daud A, Skoglund E, & Rydelius P-A (2005). Children in families of torture victims: transgenerational transmission of parents’ traumatic experiences to their children. International Journal of Social Welfare, 14(1), 23–32. doi: doi: 10.1111/j.1468-2397.2005.00336.x [DOI] [Google Scholar]
- Davidov M, Knafo-Noam A, Serbin LA, & Moss E (2015). The influential child: How children affect their environment and influence their own risk and resilience. Development and Psychopathology, 27(4pt1), 947–951. doi: 10.1017/S0954579415000619 [DOI] [PubMed] [Google Scholar]
- Davis L, Hanson SK, Zamir O, Gewirtz AH, & DeGarmo DS (2015). Associations of contextual risk and protective factors with fathers’ parenting practices in the postdeployment environment. Psychological Services, 12(3), 250–260. doi: 10.1037/ser0000038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deater-Deckard K (1998). Parenting Stress and Child Adjustment: Some Old Hypotheses and New Questions. Clinical Psychology: Science and Practice, 5(3), 314–332. doi: 10.1111/j.1468-2850.1998.tb00152.x [DOI] [Google Scholar]
- Dekel R, & Goldblatt H (2008). Is there intergenerational transmission of trauma? The case of combat veterans’ children. American Journal of Orthopsychiatry, 78(3), 281–289. doi: doi: 10.1037/a0013955 [DOI] [PubMed] [Google Scholar]
- Del Vecchio T, & Rhoades KA (2010). Bidirectional influences in mother-toddler dyads: An examination of the relative influence of mothers’ and children’s behaviors. Infant and Child Development, 19(5), 516–529. doi: 10.1002/icd.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, & Spinrad TL (1998). Parental Socialization of Emotion. Psychological Inquiry, 9(4), 241–273. doi: 10.1207/s15327965pli0904_1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BH, & Alisic E (2013). Maternal emotion coaching: A protective factor for traumatized children’s emotion regulation? Journal of Child and Adolescent Trauma, 6(2), 118–125. doi: 10.1080/19361521.2013.755651 [DOI] [Google Scholar]
- Eshel N, Daelmans B, Carbral de Mello M, & Martines J (2006). Responsive parenting: Interventions and outcomes. Bulletin of the World Health Organization, 84(12), 991–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field NP, Muong S, & Sochanvimean V (2013). Parental Styles in the Intergenerational Transmission of Trauma Stemming From the Khmer Rouge Regime in Cambodia. American Journal of Orthopsychiatry, 83(4), 483–494. doi: doi: 10.1111/ajop.12057 [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, & Erbes C, R. (2010). Posttraumatic stress symptoms among national guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology, 78(5), 599–610. doi: 10.1037/a0020571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham-Bermann SA, Gruber G, Howell KH, & Girz L (2009). Factors disriminating among profiles of resilience and psychopathology in children exposed to intimate partner violence (IPV). Child Abuse & Neglect, 33(648–660). doi: 10.1016/j.chiabu.2009.01.002 [DOI] [PubMed] [Google Scholar]
- Greene CA, Chan G, McCarthy KJ, Wakschlag LS, & Briggs-Gowan MJ (2018). Psychological and physical intimate partner violence and young children’s mental health: The role of maternal posttraumatic stress symptoms and parenting behaviors. Child Abuse & Neglect, 77, 168–179. doi: 10.1016/j.chiabu.2018.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeson MR, Kennedy AC, Bybee D, Beeble ML, Adams AE, & Sullivan C (2014). Beyond deficits: Intimate partner violence, maternal parenting, and child behavior over time. American Journal of Community Psychology, 54, 46–58. doi: 10.1007/s10464-014-9658-y [DOI] [PubMed] [Google Scholar]
- Gunlicks ML, & Weissman MM (2008). Change in child psychopathology with improvement in parental depression: A systematic review. Journal of the American Academy of Child & Adolescent Psychiatry, 47(4), 379–389. [DOI] [PubMed] [Google Scholar]
- Gustafsson HC, Cox MJ, & Blair C (2012). Maternal parenting as a mediator of the relationship between intimate partner violence and effortful control. Journal of Family Psychology, 26(1), 115–123. doi: 10.1037/a0026283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havighurst SS, Duncombe M, Frankling E, Holland K, Kehoe C, & Stargatt R (2015). An Emotion-Focused Early Intervention for Children with Emerging Conduct Problems. Journal of Abnormal Child Psychology, 43(4), 749–760. doi: 10.1007/s10802-014-9944-z [DOI] [PubMed] [Google Scholar]
- Herbert SD, Harvey EA, Roberts JL, Wichowski K, & Lugo-Candelas CI (2013). A randomized controlled trial of a parent training and emotion socialization program for families of hyperactive preschool-aged children. Behavior Therapy, 44, 302–316. [DOI] [PubMed] [Google Scholar]
- Hill C, Maskowitz K, Danis B, & Wakschlag LS (2008). Validation of a clinically sensitive, observational coding system for parenting behaviors: The parenting clinical observation schedule. Parenting, 8(2), 153–185. doi: 10.1080/15295190802045469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell KH, Graham-Bermann SA, Czyz E, & Lilly M (2010). Assessing resilience in preschool children exposed to intimate partner violence. Violence and Victims, 25(2), 150–164. doi: 10.1891/0886-6708.25.2.150 [DOI] [PubMed] [Google Scholar]
- Katz LF, Stettler N, & Gurtovenko K (2016). Traumatic stress symptoms in children exposed to intimate partner violence: The role of parent emotion socialization and children’s emotion regulation abilities. Social Development, 25(1), 47–65. doi: 10.1111/sode.12151 [DOI] [Google Scholar]
- Kochanska G, Aksan N, & Joy ME (2007). Children’s fearfulness as a moderator of parenting in early socialization: Two longitudinal studies. Developmental Psychology, 43(1), 222–237. doi: 10.1037/0012-1649.43.1.222 [DOI] [PubMed] [Google Scholar]
- Lambert JE, Holzer J, & Hasbun A (2014). Association between parents’ PTSD severity and children’s psychological distress: A meta-analysis. Journal of Traumatic Stress, 27(1), 1–9. doi: 10.1002/jts.21891 [DOI] [PubMed] [Google Scholar]
- Lansford JE, Cappa C, Putnick DL, Bornstein MH, Deater-Deckard K, & Bradley RH (2017). Change over time in parents’ beliefs about and reported use of corporal punishment in eight countries with and without legal bans. Child Abuse Negl, 71, 44–55. doi: 10.1016/j.chiabu.2016.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leckman-Westin E, Cohen PR, & Stueve A (2009). Maternal depression and mother-child interaction patterns: association with toddler problems and continuity of effects to late childhood. Journal of Child Psychology and Psychiatry, 50(9), 1176–1184. doi: 10.1111/j.1469-7610.2009.02083.x [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Knapp A, Bunaciu L, Blumenthal M, & Amstadter AB (2013). Offspring psychological and biological correlates of parental posttraumatic stress: Review of the literature and research agenda. Clinical Psychology Review, 33(8), 1106–1133. doi: 10.1016/j.cpr.2013.09.001 [DOI] [PubMed] [Google Scholar]
- Letourneau NL, Fedick CB, & Willms JD (2007). Mothering and domestic violence: A longitudinal analysis. Jounral of Family Violence, 22, 649–659. doi: 10.1007/s10896-007-9099-6 [DOI] [Google Scholar]
- Levendosky AA, & Graham-Bermann SA (2001). Parenting in battered women: The effects of domestic violence on women and their children. Journal of Family Violence, 16(2), 171–192. [Google Scholar]
- Levendosky AA, Huth-Bocks AC, Shapiro DL, & Semel M, A. (2003). The impact of domestic violence on the maternal-child relationship and preschool-age children’s functioning. Journal of Family Psychology, 17(3), 275–287. doi: 10.1037/0893-3200.17.3.275 [DOI] [PubMed] [Google Scholar]
- Martinez-Torteya C, Dayton CJ, Beeghly M, Seng JS, McGinnis E, Broderick A, … Muzik M (2014). Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment. Development and Psychopathology, 26(2), 379–392. doi: 10.1017/s0954579414000017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough C, Han Z, & Morelen D (2017). he Moderating Effects of Maternal Age at Childbirth and Emotion Dysregulation on the Intergenerational Continuity of Emotionally Unsupportive Parenting Behaviors.. Journal of Family Issues, 38(7), 948–971. doi: 10.1177/0192513X15597290 [DOI] [Google Scholar]
- Milan S, & Carlone C (2018). A two-way street: Mothers’ and adolescent daughters’ depression and PTSD symptoms jointly predict dyadic behaviors. Journal of Family Psychology, 32(8), 1097–1108. doi: 10.1037/fam0000467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Singer LT, Minnes S, Kim H, & Short E (2012). Mediating Links Between Maternal Childhood Trauma and Preadolescent Behavioral Adjustment. Journal of Interpersonal Violence, 28(4), 831–851. doi: 10.1177/0886260512455868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Gabert-Quillen C, & Delahanty D (2012). The association between parent PTSD/Depression symptoms and child PTSD symptoms: A meta-analysis. Journal of Pediatric Psychology, 37, 1076–1088. [DOI] [PubMed] [Google Scholar]
- Morris AS, Robinson LR, Hays-Grudo J, Claussen AH, Hartwig SA, & Treat AE (2017). Targeting Parenting in Early Childhood: A Public Health Approach to Improve Outcomes for Children Living in Poverty. Child development, 88(2), 388–397. doi: 10.1111/cdev.12743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols SR, Briggs-Gowan MJ, Estabrook R, Burns JL, Kestler J, Berman G, … Wakschlag LS (2015). Punishment insensitivity in early childhood: A developmental, dimensional approach. Journal of Abnormal Child Psychology, 43(6), 1011–1023. doi: 10.1007/s10802-014-9950-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dor SL, Grasso DJ, Forbes D, Bates JE, McCarthy K, Wakschlag LS, & Briggs-Gowan MJ (2017). The Family Socialization Interview-Revised (FSI-R): a Comprehensive Assessment of Parental Disciplinary Behaviors. Prevention Science, 18(3), 292–304. doi: 10.1007/s11121-016-0707-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overbeek MM, De Schipper JC, Willemen AM, Lamers-Winkelman F, & Schuengel C (2017). Mediators and Treatment Factors in Intervention for Children Exposed to Interparental Violence. Journal of Clinical Child and Adolescent Psychology, 46(3), 411–427. doi: 10.1080/15374416.2015.1012720 [DOI] [PubMed] [Google Scholar]
- Pastorelli C, Lansford JE, Luengo Kanacri BP, Malone PS, Di Giunta L, Bacchini D, … Sorbring E (2016). Positive parenting and children’s prosocial behavior in eight countries. Journal of Child Psychology and Psychiatry, 57(7), 824–834. doi: 10.1111/jcpp.12477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petitclerc A, Briggs‐Gowan MJ, Estabrook R, Burns JL, Anderson EL, McCarthy KJ, & Wakschlag LS (2015). Contextual variation in young children’s observed disruptive behavior on the DB‐DOS: Implications for early identification. Journal of Child Psychology and Psychiatry, 56(9), 1008–1016. doi: 10.1111/jcpp.12430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & Group PC (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS): depression, anxiety, and anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M (2016). Associations of parenting dimensions and styles with internalizing symptoms in children and adolescents: A meta-analysis. Marriage & Family Review, 1–28. doi: 10.1080/01494929.2016.1247761 [DOI] [Google Scholar]
- Plant DT, Jones FW, Pariante CM, & Pawlby S (2017). Association between maternal childhood trauma and offspring childhood psychopathology: Mediation analysis from the ALSPAC cohort. The British Journal of Psychiatry, 211(3), 144–150. doi: 10.1192/bjp.bp.117.198721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PROMIS. (2012). PROMIS Depression Scoring Manual Retrieved 7/20/2018, 2018, from http://www.healthmeasures.net/promis-scoring-manuals
- Rose BM, Holmbeck GN, Coakley RM, & Franks EA (2004). Mediator and moderator effects in developmental and behavioral pediatric research. Developmental and Behavioral Pediatrics, 25(1), 58–67. doi: 0196-206X/00/2501-0058 [DOI] [PubMed] [Google Scholar]
- Samuelson KW, Wilson CK, Padron E, Lee S, & Gavron L (2017). Maternal PTSD and Children’s Adjustment: Parenting Stress and Emotional Availability as Proposed Mediators. Journal of Clinical Psychology, 73(6), 693–706. doi: 10.1002/jclp.22369 [DOI] [PubMed] [Google Scholar]
- Schechter DS, Willheim E, Hinojosa C, Scholfield-Kleinman K, Turner JB, McCaw J, … Myers MM (2010). Subjective and objective measures of parent-child relationship dysfunction, child separation distress, and joint attention. Psychiatry, 73(2), 130–144. doi: 10.1521/psyc.2010.73.2.130 [DOI] [PubMed] [Google Scholar]
- Shipman KL, Schneider R, Fitzgerald MM, Sims C, Swisher L, & Edwards A (2007). Maternal Emotion Socialization in Maltreating and Non-maltreating Families: Implications for Children’s Emotion Regulation. Social Development, 16(2), 268–285. doi: 10.1111/j.1467-9507.2007.00384.x [DOI] [Google Scholar]
- Shonkoff JP, & Fisher PA (2013). Rethinking evidence-based practice and two-generation programs to create the future of early childhood policy. Development & Psychopathology, 25, 1635–1653. doi: 10.1017/S0954579413000813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, DeCoste C, Castiglioni N, McMahon TJ, Rounsaville B, & Mayes L (2010). The Mothers and Toddlers Program, an attachment-based parenting intervention for substance using women: Post-treatment results from a randomized clinical pilot. Attachment & Human Development, 12(5), 483–504. doi: 10.1080/14616734.2010.501983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Shear MK, Wren FJ, Greeno CG, Sales E, Sullivan BK, & Ludewig DP (2005). Depression and Anxiety Among Mothers Who Bring Their Children to a Pediatric Mental Health Clinic. Psychiatric Services, 56(9), 1077–1083. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2007). Using multivariate statistics. Boston: Pearson Education, Inc. [Google Scholar]
- van Ee E, Kleber R, & Jongmans MJ (2016). Relational patterns between caregivers with PTSD and their nonexposed children: A review. Trauma, Violence & Abuse, 17(2), 186–203. doi: 10.1177/1524838015584355 [DOI] [PubMed] [Google Scholar]
- Van Ee E, Kleber R, & Mooren TTM (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent-child interaction, and child development. Infant Mental Health Journal, 33(5), 459–468. doi: 10.1002/imhj.21324 [DOI] [PubMed] [Google Scholar]
- van Ijzendoorn MH, Juffer F, & Duyvesteyn MGC (1995). Breaking the intergenerational cycle of insecure attachment: A review of the effects of attachment-based interventions on maternal sensitivity and infant security. Journal of Child Psychology and Psychiatry, 36(2), 225–248. doi: 10.1111/j.1469-7610.1995.tb01822.x [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, Briggs-Gowan MJ, Choi SW, Nichols SR, Kestler J, Burns JL, … Henry D (2014). Advancing a multidimensional, developmental spectrum approach to preschool disruptive behavior. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 82–96. doi: 10.1016/j.jaac.2013.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, & Hans SL (1999). Relation to maternal responsiveness during infancy to the development of behavior problems in high risk youths. Developmental Psychology, 37, 569–579. doi: 10.1037/0012-1649.35.2.569 [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, & Hans SL (2002). Maternal smoking during pregnancy and conduct problems in high-risk youth: A developmental framework. Development and Psychopathology, 14(2), 351–369. doi: 10.1017/s0954579402002092 [DOI] [PubMed] [Google Scholar]
- Wakschlag LS, Henry DB, Blair RJ, Dukic V, Burns J, & Pickett KE (2011). Unpacking the association: Individual differences in the relation of prenatal exposure to cigarettes and disrtuptive behavior phenotypes. Neurotoxicology and Teratology, 33(1), 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Hill C, Carter AS, Danis B, Egger HL, Keenan K, … Briggs-Gowan MJ (2008). Observational Assessment of Preschool Disruptive Behavior, Part I: reliability of the Disruptive Behavior Diagnostic Observation Schedule (DB-DOS). J Am Acad Child Adolesc Psychiatry, 47(6), 622–631. doi: 10.1097/CHI.0b013e31816c5bdb [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD checklist: reliability, validity, & diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- West SG, Finch JF, & Curran PJ (1995). Structural equation models with nonnormal variables: Problems and remedies. In Hoyle RH (Ed.), Structural equation modeling: Concepts, issues, and applications (pp. 56–75). Newbery Park, CA: Sage. [Google Scholar]
- Yehuda R, Schmeidler J, Wainberg M, Binder-Brynes K, & Duvdevani T (1998). Vulnerability to Posttraumatic Stress Disorder in Adult Offspring of Holocaust Survivors. American journal of Psychiatry, 155(9), 1163–1171. doi: 10.1176/ajp.155.9.1163 [DOI] [PubMed] [Google Scholar]
- Zarling AL, Taber-Thomas S, Murray A, Knuston JF, Lawrence E, Valles N-L, … Bank L (2013). Internalizing and externalizing symptoms in young children exposed to intimate partner violence: Examining intervening processes. Journal of Family Psychology, 27(6), 945–955. doi: 10.1037/a0034804 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.